Abstract
Aim:
This article describes and discusses the Swedish UngDOK interview and its psychometric properties.
Method:
The study is based on empirical data from 1633 intake interviews collected by 15 units in ten cities and focused primarily on the two central sections of intake form: alcohol and drug use and mental health. The statistical analyses concern internal consistency, test–retest reliability, discriminant validity and internal non-response.
Results:
The reliability of AUDIT-C and the mental health domain was good with regard to both internal consistency and test–retest. The test–retest values were generally satisfactory, except for frequency of drug use and association with peers who use drugs. The discriminant validity shows that the interview clearly distinguishes adolescents with more profound problems from a group with milder problems and that a minor degree of inconsistency and non-response bias may occur in empirical material based upon self-reported information.
Conclusion:
The study showed that the psychometric properties of the UngDOK interview are generally satisfactory and may be regarded as a valuable option for practices engaged in treating adolescents with substance-use problems.
Keywords: adolescents, structured interview, substance abuse, UngDOK, validation
Specialist outpatient care for adolescents with substance-use problems has increased in scope, and the percentage of adolescents identified as needing treatment for substance misuse in Sweden has risen in the last decade (Swedish Government Official Reports, 2011). UngDOK is a semi-structured interview method developed specifically for adolescents with various forms of alcohol and drug problems. The primary purpose of the interview is to identify the young person’s problems, needs and current situation to enable relevant assessment and choice of appropriate intervention. The information derived may also constitute a basis for follow-up and local evaluation of interventions and outcomes; further, it makes a contribution to research. This study reports a validation of the UngDOK interview method.
The UngDOK interview was developed in 2003 within the framework of a collaboration project among outpatient “Maria clinics” for adolescents and young adults with substance-use problems in Stockholm, Göteborg and Malmö. The clinics provide various forms of treatment for alcohol and drug abuse as well as counselling and support for adolescents and/or their families. The average treatment duration is 4–6 months. The clinics offer psychosocial and medical assessment related to the abuse of alcohol and drugs, drug tests, individual or family therapy and manual-based treatment programmes. The staff groups include social workers, nurses, psychologists and doctors.
Some of the clinics had no systematic documentation of their clients, while others used forms they had designed themselves or interview methods designed for adults with substance-use problems. A central aspect was that the interview should be brief and easily administered to make it more appropriate for adolescents presenting for outpatient care. It was also intended to provide treatment support and a basis for describing the target groups of the clinics (Richert, 2007).
UngDOK was revised and further developed jointly by practitioners and researchers in 2012. “Trestad 2” was a renewed partnership among the three large cities, whose main objective was to reduce cannabis use among adolescents. The project began in 2012 and ran through 2015 within the framework of the national Alcohol, Narcotics, Doping and Tobacco Strategy (Swedish Ministry of Health and Social Affairs, 2013). One of the projects within Trestad 2 aimed at developing UngDOK and designing models to continuously follow up the treatment outcomes of Maria clinics and to identify and track trends in the three cities concerning drug use and the psychosocial situations of adolescents who seek care.
A fundamental priority for the clinics is that both adolescents and therapists should perceive the UngDOK interview as clinically meaningful. It should also be useful in the direct treatment process with respect to needs assessment, treatment planning and follow-up. The interview should be perceived as a conversation between the therapist and the adolescent, which is accomplished by means that include seeking subjective perceptions and asking several open-ended questions. A further ambition is to maintain the limit on the number of interview questions; that is, the interview should not be too comprehensive or difficult to administer and should be linguistically adapted to adolescents. A structured interview aimed at adolescents with substance-use problems must also meet theoretical and methodological standards.
The further development of the UngDOK interview began with a review of the literature related to the design of identification, assessment and follow-up instruments for adolescents with substance-use problems. An empirical test of the previous intake and discharge forms was also performed; a descriptive analysis of the target group was carried out, followed by a comparative analysis of information derived from more than 600 adolescents who had begun and completed a treatment episode. The results supported the development project. Representatives of the participating clinics and researchers held several workshops where they arrived jointly at suggestions for relevant life domains and specific variables.
Acceptance of the newly developed UngDOK interview by therapists and adolescents was studied in the spring of 2013 using a Swedish version of a questionnaire based on a model designed by researchers in Switzerland (Suppiger et al., 2009). A total of 31 adolescents and 31 therapists answered the survey after the intake interview. The results showed that the adolescents generally had a high degree of acceptance for the form and content of the interview and found it relevant. Therapists had a somewhat lower degree of acceptance, especially with regard to the scope of the form and the time required to conduct the interview. This resulted in revised intake and discharge forms as well as in a newly designed follow-up form and manual (Anderberg & Dahlberg, 2016b). The revised forms were implemented at the Maria clinics, and several studies based on the new UngDOK interview have since been carried out (Almazidou et al., 2014; Anderberg et al., 2015; Anderberg & Dahlberg, 2014, 2015, 2016a; Dahlberg & Anderberg, 2015; Ekberg, Fonseca, Anderberg, & Dahlberg, 2016).
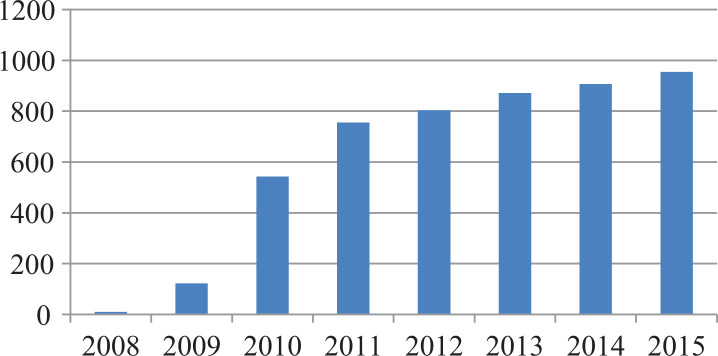
At present, UngDOK is used in ten cities by 15 outpatient units, most of which are Maria clinics. The documentation system is administered jointly by the Institute for the Development of Knowledge and Methods in the Treatment of Drug Abuse (IKM) at Linnaeus University (Swedish Government Official Reports, 2011) and the clinics in Stockholm, Göteborg and Malmö. The histogram below (Figure 1) illustrates the use and spread of the method during 2008–2015. As shown on the chart, there has been a continuous increase, with nearly 1000 intake interviews conducted in 2015.
Figure 1.
Reported numbers of adolescents interviewed at intake using UngDOK, 2008–2015.
For information collected by a structured interview to be useful as a basis for individual assessment, organisational improvement and various forms of evaluations or studies, however, the interview method must be of sufficient quality in terms of validity and reliability. The latest Swedish guidelines for substance abuse treatment, which now include recommendations related to adolescents with substance-use problems, emphasise that it is essential that the approaches and methods used by therapists and researchers in the field are of good quality and meet scientific standards (Swedish National Board of Health and Welfare, 2015). Accordingly, to be considered valid, a method needs to be investigated as the object of scientific studies concerning its relevance and quality.
The aim of this article is to describe and discuss the Swedish UngDOK interview and its psychometric properties with regard to internal consistency, test–retest reliability, discriminant validity and internal non-response.
Previous research
The following review of the literature on the design of identification, assessment and follow-up instruments for adolescents with substance-use problems has identified some important theoretical and research-related aspects, which have to some extent been integrated into the structured interview UngDOK. Comparisons were also made with other interview methods used for this target group, such as ADAD (Adolescent Drug Abuse Diagnosis – Friedman & Utada, 1989; Söderholm Carpelan & Hermodsson, 2004), DOK (Documentation of Clients – Jenner & Segraeus, 1996), T-ASI (Teen Addiction Severity Index – Brodey et al., 2005; Kaminer, Bukstein, & Tarter, 1991) and C-ASI (Comprehensive Addiction Severity Index – Meyers, McLellan, Jaeger, & Pettinati, 1995). The UngDOK interview also harmonises with the key variables recommended in TDI (Treatment Demand Indicators – EMCDDA, 2013) to facilitate comparisons with treatment data from other European countries.
Theories on risk and protective factors are now well established in the field of preventive and therapeutic interventions targeting adolescents at risk of developing various types of psychosocial problems (Hawkins, Catalano, & Miller, 1992; Stone, Becker, Huber, & Catalano, 2012). The risk and protective factors may increase or reduce, respectively, the risk of unfavourable developments and future problems in the form of mental illness, substance misuse and crime. They are stated in relation to four main levels: the individual and his or her peers, family, school and community. The fundamental principle in treatment of substance abuse, for example, is to reduce the risk factors present in the individual while reinforcing the protective factors. If these conditions can be influenced during the treatment episode, there is potential for positive development (Fleming, Catalano, Haggerty, & Abbott, 2010; Shekhtmeyster, Sharkey, & You, 2011).
Another theory in treatment with adolescents is the Risk–Need–Responsivity model (Andreassen, 2003; Andrews, Bonta, & Hoge, 1990). The risk principle refers to the level of treatment needing to be adjusted to the level of risk; that is, adolescents who demonstrate high risk of continued development of misuse patterns need more comprehensive and intensive therapeutic interventions compared with adolescents at lower risk. The need principle implies that therapeutic work should focus on risk factors amenable to influence within the specific life domains observed in the adolescent. The responsivity principle notes that treatment must be matched to the adolescent’s individual character traits and learning capacity in order to generate a good working alliance and an optimal outcome. The development of UngDOK was guided by these theoretical precepts.
Adolescents with substance-use problems are a heterogeneous group. It is therefore important that a structured interview or assessment instrument clearly distinguishes between adolescents who are experimenting with drugs and those who have more pronounced and serious misuse problems (Dilbaz & Hendriks, 2006; Meyers et al., 1995; Winters, 2003).
As alcohol and drug problems are both multifaceted and multifactorial, structured interviews and assessment instruments designed for adolescents with substance-use problems need to be multidimensional and to cover several significant life domains to enable relevant needs assessment (Winters & Stinchfield, 1995). However, too extensive an interview can affect both its usefulness and validity (Brodey et al., 2005; Winters, 2003; Winters & Kaminer, 2008). A personal interview with adolescents is to be preferred, based on the knowledge that, when completing surveys or self-assessment forms, adolescents can give answers that are vague and difficult to interpret. It is also important that questions and response options are adapted to the language used by adolescents as well as to their (possibly limited) reading and writing ability (Meyers et al., 1995).
The time frame of the questions is also highly pertinent to the assessment of problems and needs with regard to, for example, drug use and mental health. For this reason, a combination of past and present circumstances is required. Interview methods aimed at adolescents commonly contain questions that cover the last 30 days, a three-month and a lifetime perspective (Meyers et al., 1995).
Investigating the reliability and validity of adolescents’ self-reported information about their drug and alcohol use can be challenging. Some adolescents do not perceive their drug use to be a problem and therefore see no reason to report their actual use (Buchan, Dennis, Tims, & Diamond, 2002; Winters, 2003). It may, for example, be problematic to elicit reliable answers in an interview situation involving adolescents who are the subject of legal proceedings or are poorly motivated to participate in an interview (Buchan et al., 2002; Meyers et al., 1995; Winters, 2003). Parental involvement in the interview may also negatively affect the reliability of the information provided by adolescents (Burleson & Kaminer, 2006; Winters, 2003). There are also test–retest studies that show that adolescents’ drug use may increase gradually between the first and the second interview (Winters, Stinchfield, Henly, & Schwartz, 1991).
Studies have shown generally good internal consistency and very good inter-rater reliability for the Swedish ADAD interview, which is primarily used by the state compulsory care system for adolescents. However, the agreement between adolescent and interviewer severity ratings is weak, and differences in composite scores are small between a normal population group and a clinical group with profound psychosocial problems (Börjesson, Armelius, & Ostgård-Ybrandt, 2007). Predictive reliability with regard to problem development for both normal and clinical groups is low to moderate in the ADAD interview (Börjesson & Ybrandt, 2012). In spite of these identified limitations, several studies show generally good reliability and validity with regard to adolescent drug use, for example, through good agreement between self-reported information and urine tests (Buchan et al., 2002; Burleson & Kaminer, 2006; Kaminer, 2008; Winters, 2003; Winters et al., 1991).
Method
Sample
The study is based on empirical data from intake interviews collected by 15 units in ten cities between 1 January 2013 and 30 June 2015. One of the units is an inpatient detoxification clinic, and the others are outpatient clinics for adolescents with various forms of substance-use problems. The completed UngDOK interviews were transferred to a database via the treatment units that participate in the documentation system and included information on a total of 1821 unique individuals reported during the stated period. Incomplete interviews (44) and information based on file material (144) were eliminated, leaving a total of 1633 interviews. This sample was used to test internal consistency and to analyse non-response bias. Based on this material, 43 individuals were also identified who had been the subject of two interviews within a three-month period, which constituted a subsample for analysing test–retest reliability. The sample for testing discriminant validity was made up of 164 inpatients from the detoxification clinic and the remaining 1469 outpatients.
The sample consisted of 1633 respondents aged 12–27 years (mean 17.3, SD 2.1); 28% were females. In about 8% of the cases, the adolescent’s parents were present at the interview. The main form of living status during the last three months for 79% of the adolescents was with their parents. About 70% attended secondary school or high school, and 17% reported an impaired ability to read and write. Cannabis was the most common primary drug (75%), followed by alcohol (14%) and other narcotic substances (11%). Eighteen per cent had previously been treated for drug problems, while a smaller proportion (5%) had previously been treated for alcohol problems.
Material
The primary target group for the UngDOK interview is adolescents and young adults aged 13–25 years who come into contact with care and treatment for substance-use problems. The interview contains questions within the following life domains which are consistent with the domains recommended in previous research (Meyers et al., 1999): housing and financial support; occupation; alcohol, drug and tobacco use; treatment history; criminality; childhood; exposure to violence; family and relationships; physical health and mental health. In addition to these, there are sections for administrative and sociodemographic information and information on treatment episodes, as well as a section with concluding open-ended questions.
Questions of both an objective and subjective nature are asked within each life domain, that is, concerning factual circumstances that can usually be verified as well as more individual perceptions or estimations of the adolescent’s need for change. Three time frames are used throughout the interview; “the last 30 days” and “the last three months” before intake, and “lifetime” in some questions. The intake interview contains a total of 75 questions and takes about 45 minutes to administer. The UngDOK interview also generates a text summary that can be fed back to the adolescent and used as a basis for assessment and treatment planning.
The study focused primarily on the two central sections of the intake form: alcohol and drug use and mental health. In the first section, the following nine variables were tested: alcohol use was measured with a revised version of the AUDIT-C, called AUDIT-CR, where item three was a question on how often the respondents consumed 4 (girls) or 5 (boys) drinks on the same occasion (see Reinert & Allen, 2007; Swedish Ministry of Health and Social Affairs, 2013); primary and secondary drug; usual route of administration of the primary and secondary drug and frequency of use of the primary and secondary drug in the last three months. Twenty-two variables were included for mental health with regard to the occurrence of psychological distress over the adolescent’s lifetime and for the last 30 days. These included sleep disturbances, depression, anxiety, concentration difficulties, aggressive behaviour, suicidal thoughts, suicide attempts, hallucinations, medication for psychological disorders, eating disorders and self-harming behaviour. Other variables tested included nicotine use, being arrested by the police, living conditions, main occupation and main income for the last three months and a risk factor index in which nine items were summarised: placement in foster care/residential home; problems in the childhood environment related to economic vulnerability, substance abuse, mental health and violence/abuse; parental separation; and three variables of physical, psychological and sexual victimisation.
The interviews were conducted by treating professionals at each clinic after informed consent had been obtained from the adolescent and in accordance with a manual. Only de-identified data, with no connection to personal data, were used in this study.
Analysis
In addition to the mere description of the sample, data were analysed in four steps. First, for summary indices, internal consistency (Cronbach’s alpha) was calculated for the full sample. Second, for a small subsample with repeated data collections within three months, test–retest reliability was calculated. In items with categorical data, Cohen’s kappa was employed, and for continuous data Pearson correlations were used. A frequently used classification of the level of agreement for kappa was provided by Landis and Koch (1977): less than 0, poor; 0.00–0.20, slight; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, substantial; and 0.81–1.00, almost perfect. Third, as a means to describe the discriminant validity of the instrument, inpatients were compared to outpatients with respect to alcohol use and psychological distress, assuming that inpatients generally have a higher risk load. Finally, a subgroup analysis was carried out to extract a profile of respondents who showed high rates of non-response. This was done with a CHAID analysis (Chi-square Automatic Interaction Detection; Kass, 1980). CHAID is a stepwise procedure where a decision tree is built on the basis of data. When using categorical binary outcome data, as in this case, the first step is to find a cut-off for an independent variable that best discriminates (on the basis of the chi-square value) between outcomes in the dependent variable. Next, the procedure is repeated for each node in the tree until a pre-specified stopping criterion is met. The stopping criterion in this case was when the Bonferroni-adjusted p-value dropped below 0.05. This rather uncommon method has several advantages, as it can include data on all measurement levels, describe complex interactions and include several (potential) independent variables (Kass, 1980).
Results
Internal consistency
Alcohol use was measured with AUDIT-CR and yields a Cronbach’s alpha of 0.77 (see Table 1). The summary measure of lifetime psychological distress comprises 11 items, previously described in the methods, and the measure of current psychological distress contains the same 11 items but referring to the state over the last 30 days. The internal consistency for these indices is 0.82 and 0.76, respectively. A summary measure of risk factors comprises nine items. This index is satisfactory with regard to internal consistency, 0.71.
Table 1.
Internal consistency and test–retest reliability for different domains of UngDOK.
| Internal consistency (N = 1633) | Test–retest (N = 43) (rxx or Cohen’s kappa) | |
|---|---|---|
| AUDIT-CR | 0.77 | rxx = 0.71 |
| Psychological distress (lifetime) | 0.82 | rxx = 0.37 |
| Psychological distress (last 30 days) | 0.76 | (not relevant) |
| Risk factor index | 0.71 | rxx = 0.83 |
| Living conditions (last three months) | – | Kappa = 0.56 |
| Main occupation (last three months) | – | Kappa = 0.52 |
| Main income (last three months) | – | Kappa = 0.57 |
| Primary drug | – | Kappa = 0.63 |
| Usual route of administration (oral, smoking, etc.) | – | Kappa = 0.54 |
| Frequency of use of primary drug (last three months) | – | Kappa = 0.13 |
| Secondary drug | – | Kappa = 0.34 |
| Usual route of administration (oral, smoking, etc.) | – | Kappa = 0.35 |
| Frequency of use of secondary drug (last three months) | – | Kappa = 0.22 |
| Nicotine use | – | Kappa = 0.45 |
| Arrested by police (number of occasions) | – | rxx = 0.55 |
| Association with drug-abusing peers | – | Kappa = 0.23 |
| Association with criminal peers | – | Kappa = 0.32 |
Test–retest reliability
The test–retest reliability is satisfactory (i.e., > 0.70) for the AUDIT-CR (rxx = 0.71; CI95% = 0.54–0.85; SE = 0.08) and the risk factor index (rxx = 0.83; CI95% = 0.71–0.92; SE = 0.05), but the test–retest reliability for the scale measuring lifetime psychological distress is low (rxx = 0.37; CI95% = 0–0.72; SE = 0.19) similar to the reported number of police arrests (rxx = 0.55; CI95% = 0.06–0.95; SE = 0.26), see Table 1. Cohen’s kappa is acceptable for most of the items between t1 and t2 (from 0.34 to 0.83). However, some exceptions are the measure of frequency of use of the primary and secondary drug (0.13 and 0.22, respectively), and association with drug-abusing peers (0.23). The 30-day measure of psychological distress covers a shorter time span than the other items, and since it is not possible to differentiate between actual change and item reliability, this value is not presented.
Discriminant validity
Out of the 1633 informants, 164 were inpatients and 1469 outpatients. Inpatients and outpatients were compared with respect to relevant factors in UngDOK, assuming that inpatients generally have a higher risk load and more severe life conditions. As shown in Table 2, inpatients have a higher level of hazardous use of alcohol (5.60 versus 4.67 points), higher levels of psychological distress, more frequent consumption of their primary drug and a significantly different route of administration of the drugs.
Table 2.
Differences between inpatients and outpatients regarding alcohol consumption, psychological distress and frequency of use of the primary drug.
| Outpatients N = 1469 | Inpatients N = 164 | Significance | |
|---|---|---|---|
| AUDIT-CR | 4.67 (2.56) | 5.60 (2.77) | t (1367) = −4.11; p < 0.001 |
| Psychological distress (lifetime) | 3.81 (2.87) | 6.29 (2.46) | t (1519) = −10.42; p < 0.001 |
| Psychological distress (last 30 days) | 2.30 (2.12) | 4.84 (2.31) | t (1515) = −14.12; p < 0.001 |
| Primary drug use, last 30 days (%) No use Occasional use 1 day/w or less 2–3 times/w 4–6 times/w Daily | 52.6 19.1 8.2 9.3 4.6 6.0 | 6.8 6.8 7.4 17.9 16.0 45.1 | Chi-square (5) = 342.77; p < 0.001 |
| Primary drug use, last three months (%) No use Occasional use 1 day/w or less 2–3 times/w 4–6 times/w Daily | 15.5 30.2 13.6 17.7 8.8 14.2 | 4.3 6.2 5.6 18.5 16.7 48.8 | Chi-square (5) = 158.17; p < 0.001 |
| Usual route of administration (%) Oral Nasal Smoking Injecting | 21.3 1.6 76.9 0.2 | 17.8 11.0 69.9 1.2 | Chi-square (3) = 56.85; p < 0.001 |
Inconsistencies and non-response patterns
Finally, a focus was placed on inconsistent answers and patterns of non-response items. One such inconsistency is that 3.6% (N = 54) of interviewees report more psychiatric symptoms over the last 30 days than cumulatively over their lifetime. Another such inconsistency is that ten adolescents who state never drinking, simultaneously reported occasional binge drinking.
Next, to explore which subgroup was most prone to non-response, a two-step procedure was followed. First, we calculated the number of missing answers for each individual for the three alcohol questions, and for all 22 questions in psychological symptoms. Next, a CHAID analysis was carried out to extract the configuration that best discriminated between subjects who completed the interview with no missing data in these items (about 79%) and individuals with non-response in any of these items (about 21%).
Three variables entered into the model predicting the non-response bias: self-reported inability to read and write, age and whether a parent was present at the interview (see Table 3). Three other variables are not included because they did not predict dropout: gender, adoption and the source of referral. In the group of subjects with missing data for the question on reading and writing disability, only 33% complete the alcohol and psychological distress questions. This can be compared to a configuration of reporting no reading/writing disabilities, an age above 16 years and no parent present at the interview (84.3% completers).
Table 3.
Summary of CHAID analysis using partial non-response as dependent variable (n = 1633).
| Node configuration | Cases completers/missing | Completers | |
|---|---|---|---|
| Split 1a | 1: RWD = No | N = 1052/269 | 79.6% |
| 2: RWD = Yes | N = 224/52 | 81.2% | |
| 3: RWD = No response | N = 12/24 | 33.3% | |
| Split 2b | 4: RWD = No & age < 14 years | N = 39/31 | 55.7% |
| 5: RWD = No & age = 14–16 years | N = 355/107 | 76.8% | |
| 6: RWD = No & age > 16 years | N = 658/131 | 83.4% | |
| Split 3c | 7: RWD = No & age > 16 years & parent not present at interview | N = 642/120 | 84.3% |
| 8: RWD = No & age > 16 years & parent present at interview | N = 16/11 | 59.3% |
CHAID = Chi-square Automatic Interaction Detection; RWD = Reading and writing disability.
aChi-square = 46.13; df = 2; adjusted p < 0.001. bChi-square = 33.81; df = 2; adjusted p < 0.001. cChi-square = 11.76; df = 1; adjusted p < 0.005.
Discussion
The aim of this study was to investigate and analyse the reliability and validity of the UngDOK interview. The results showed that the psychometric properties of the interview are generally satisfactory, but also indicate some weaknesses. The reliability of AUDIT-CR was good with regard to both internal consistency and test–retest. Good internal consistency was also achieved for the mental health domain, but the test–retest values for lifetime psychological distress were somewhat poorer, possibly because respondents frequently referred to ongoing problems in these questions, a notion that is supported by the high correlation between lifetime distress and distress over the last 30 days. Consequently, this measure should not be regarded as a stable feature, and the 30-day measure of psychological distress is probably a more adequate time frame. However, questions about psychological distress of various kinds previously in life may have clinical value.
The test–retest values were generally satisfactory, except for frequency of drug use and association with peers who use drugs. The frequency of drug use is unstable, and the low consistency of this measure over time could be attributed to actual changes in consumption habits rather than low reliability.
The discriminant validity shows that the UngDOK interview clearly distinguishes adolescents with more profound problems from a group with milder problems in relation to risky consumption of alcohol, drug use and the incidence of psychological distress (see Dilbaz & Hendriks, 2006; Meyers et al., 1995; Winters, 2003).
The results show that a minor degree of inconsistency and non-response bias may occur in empirical material based upon self-reported information. The three variables that predict the non-response pattern are reading and writing difficulties, age and parental presence at the interview. That parental involvement at the interview is one of the factors that affect non-response is not surprising (see Burleson & Kaminer, 2006; Winters, 2003). This is an important clinical statement, because the involvement of parents and other family members may be an important aspect with regard to the completion and outcome of treatment. It is also possible that the non-response could be related to therapists who choose not to ask certain sensitive issues.
Practitioners and researchers jointly contributed knowledge and experience to the development of the UngDOK interview. A practice-based development process may entail both obstacles and opportunities, but may also make it clear that most of the standards imposed on an interview method are relevant to both parties. Through significant risk and protective factors having been incorporated into the intake form, these circumstances can be identified and taken into account during the treatment episode, which may lead to a higher degree of clinical relevance and a favourable development for the adolescent (Andreassen, 2003; Andrews et al., 1990; Fleming et al., 2010; Shekhtmeyster et al., 2011).
Because the variables are based on both theory and empirical knowledge, the input derived from the interview method can be used by both practitioners and researchers for purposes including describing the target group, tracking trends and tendencies, following up interventions or engaging in the development of methods.
Adolescents who present for treatment for substance-use problems are a heterogeneous group, which imposes particular demands on the discriminative capacity of an interview method. It must distinguish between adolescents who are experimenting with drugs and those who have more pronounced and serious misuse problems (Dilbaz & Hendriks, 2006; Meyers et al., 1995; Winters, 2003). This implies, for example, that problematic use of alcohol is also an important aspect to identify in order to arrive at a more in-depth understanding of the scope and severity of the use even when cannabis is the primary drug.
Because the target group is characterised by heterogeneity, the interview needs to be multidimensional and to cover several significant life domains to enable relevant needs assessment (Winters & Stinchfield, 1995). Another aspect that can be related to reliability and validity is that the questions and response options are designed in a concrete and comprehensible manner; that is, that they have been adapted to the language used by adolescents and to their reading and writing ability (Meyers et al., 1995).
The UngDOK interview may be regarded as a valuable option for practices engaged in treating adolescents with substance-use problems. The interview was developed for this specific target group and is perceived as useful by practitioners. This probably explains why the method has become relatively widespread and frequently used in Sweden in such a short time. Overall, it can be confirmed that the validation performed shows that the interview method has satisfactory psychometric properties but the potential value of UngDOK depends on its capability to capture the most relevant information about the adolescents, its capability to identify adolescents with specific needs and its value as a treatment planning instrument, and by the extent to which the interview is implemented at clinics aimed at the target group.
Footnotes
Declaration of conflicting interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Contributor Information
Mikael Dahlberg, Linnaeus University, Sweden.
Mats Anderberg, Linnaeus University, Sweden.
Peter Wennberg, Stockholm University, Sweden; Karolinska Institutet, Sweden.
References
- Almazidou M., Anderberg M., Borg M., Dahlberg M., Kainulainen K., Nilsson I.…Williamsson O. (2014). Maria-mottagningarna i Stockholm, Göteborg och Malmö. Ungdomar i öppenvård år 2013 [The Maria clinics in Stockholm, Göteborg and Malmö. Adolescents in outpatient care 2013]. Göteborg, Sweden: Trestad; 2. [Google Scholar]
- Anderberg M., Borg M., Dahlberg M., Davidsson C., Holmstedt A., Kainulainen K.…Williamsson O. (2015). Lokal uppföljning av ungdomar med missbruksproblem vid Maria-mottagningarna i Stockholm, Göteborg och Malmö [Local follow-up of adolescents with substance abuse problems at the Maria clinics in Stockholm, Göteborg and Malmö]. Göteborg, Sweden: Trestad; 2. [Google Scholar]
- Anderberg M., Dahlberg M. (2014). Ungdomar med missbruksproblem – en deskriptiv studie av Maria-mottagningarna i Stockholm, Göteborg och Malmö [Adolescents with substance abuse problems – a descriptive study of the Maria clinics in Stockholm, Göteborg and Malmö]. Socialmedicinsk Tidskrift, 91(4), 348–359. [Google Scholar]
- Anderberg M., Dahlberg M. (2015). Riskfylld alkoholanvändning hos ungdomar med cannabisproblem [Hazardous alcohol consumption among adolescents with cannabis use problems]. Socialmedicinsk Tidskrift, 92(4), 484–494. [Google Scholar]
- Anderberg M., Dahlberg M. (2016. a). Experiences of victimization among adolescents with substance abuse disorders in Sweden. Scandinavian Journal of Child and Adolescent Psychiatry and Psychology, 4(3), 123–131. [Google Scholar]
- Anderberg M., Dahlberg M. (2016. b). UngDOK. Manual för intervjuformulären 2016 [UngDOK. A manual for the interview forms 2016]. Växjö, Sweden: IKM, Linnaeus University. [Google Scholar]
- Andreassen T. (2003). Institutionsbehandling av ungdomar. Vad säger forskningen? [Residential treatment of adolescents. What does the research suggest?]. Stockholm, Sweden: Swedish National Board of Institutional Care and Förlagshuset Gothia AB. [Google Scholar]
- Andrews D. A., Bonta J., Hoge R. D. (1990). Classification for effective rehabilitation. Criminal Justice and Behavior, 17(1), 19–52. [Google Scholar]
- Brodey B. B., Rosen C. S., Winters K. C., Brodey I. S., Sheetz B. M., Steinfeld R. R., Kaminer Y. (2005). Conversion and validation of the Teen Addiction Severity Index (T-ASI) for internet and automated telephone self-report administration. Psychology of Addictive Behaviors, 19(1), 54–61. [DOI] [PubMed] [Google Scholar]
- Börjesson J., Armelius B.-Å., Ostgård-Ybrandt H. (2007). The psychometric properties of the Swedish version of the Adolescent Drug Abuse Diagnosis (ADAD). Nordic Journal of Psychiatry, 61(3), 225–232. [DOI] [PubMed] [Google Scholar]
- Börjesson J., Ybrandt H. (2012). Concurrent and predictive validity of the Adolescent Drug Abuse Diagnosis (ADAD). The Open Psychology Journal, 5, 31–37. [Google Scholar]
- Buchan B. J., Dennis M. L., Tims F. M., Diamond G. S. (2002). Cannabis use: Consistency and validity of self-report, on-site urine testing and laboratory testing. Addiction, 97(Suppl. 1), 98–108. [DOI] [PubMed] [Google Scholar]
- Burleson J. A., Kaminer Y. (2006). Adolescent alcohol and marijuana use: Concordance among objective-, self-, and collateral-reports. Journal of Child & Adolescent Substance Abuse, 16(1), 53–68. [Google Scholar]
- Dilbaz N., Hendriks V. (2006). Screening and assessment In Group Pompidou. (Eds.), Young people and drugs: Care and treatment (pp. 75–79). Strasbourg, France: Council of Europe. Co-operation Group to Combat Drug Abuse and Illicit Trafficking in Drugs (Pompidou Group). [Google Scholar]
- Ekberg M., Fonseca L., Anderberg M., Dahlberg M. (2016). Ungdomar med missbruksproblem och deras uppfattning om skolproblem [Adolescents with substance abuse problems and their perception of school problems]. Nordic Studies in Education, 36(4), 266–278. [Google Scholar]
- EMCDDA. (2013). Treatment Demand Indicator (TDI). Standard protocol 3.0 guidelines for reporting data on people entering drug treatment in European countries. Lisbon, Portugal: European Monitoring Centre for Drugs and Drug Addiction (EMCDDA; ). [Google Scholar]
- Fleming C. F., Catalano R. F., Haggerty K. P., Abbott R. D. (2010). Relationships between level and change in family, school, and peer factors during two periods of adolescence and problem behavior at age 19. Journal of Youth and Adolescence, 39(6), 670–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman A. S., Utada A. (1989). A method for diagnosing and planning the treatment of adolescent drug abusers: The Adolescent Drug Abuse Diagnosis (ADAD) instrument. Journal of Drug Education, 19(4), 285–312. [DOI] [PubMed] [Google Scholar]
- Hawkins J. D., Catalano R. F., Miller J. Y. (1992). Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin, 112(1), 64–105. [DOI] [PubMed] [Google Scholar]
- Jenner H., Segraeus V. (1996). Att utveckla missbrukarvård genom dokumentation: Beskrivning av DOK-projektet [Documentation as a useful tool in the care and treatment of drug abusers: A presentation of the DOK project]. Nordisk Alkoholtidskrift, 13(3), 150–159. [Google Scholar]
- Kaminer Y. (2008). The teen Addiction Severity Index around the globe: The Tower of Babel revisited. Substance Abuse, 29(3), 89–94. [DOI] [PubMed] [Google Scholar]
- Kaminer Y., Bukstein O., Tarter R. E. (1991). The teen Addiction Severity Index: Rationale and reliability. The International Journal of the Addictions, 26(2), 219–226. [DOI] [PubMed] [Google Scholar]
- Kass G. V. (1980). An exploratory technique for investigating large quantities of categorical data. Applied Statistics, 29(2), 119–127. [Google Scholar]
- Landis J. R., Koch G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. [PubMed] [Google Scholar]
- Meyers K. Hagan T. A. Zanis D. Webb A. Frantz J. King-Kurtz S.…McLellan T., (1999). Critical issues in adolescent substance use assessment. Drug and Alcohol Dependence, 55(3), 235–246. [DOI] [PubMed] [Google Scholar]
- Meyers K., McLellan T., Jaeger J. L., Pettinati H. M. (1995). The development of the Comprehensive Addiction Severity Index for Adolescents (CASI-A). An interview for assessing multiple problems of adolescents. Journal of Substance Abuse Treatment, 12(3), 181–193. [DOI] [PubMed] [Google Scholar]
- Reinert D. F., Allen J. P. (2007). The alcohol use disorders identification test: An update of research findings. Alcoholism: Clinical and Experimental Research, 31(2), 185–199. [DOI] [PubMed] [Google Scholar]
- Richert T. (2007). Unga missbrukare i Stockholm, Göteborg och Malmö – En deskriptiv och jämförande studie av sex öppenvårdsmottagningar och deras besökare [Young substance abusers in Stockholm, Göteborg and Malmö – a descriptive and comparative study of six outpatient clinics and their visitors]. Stockholm, Sweden: Mobilisering mot narkotika. [Google Scholar]
- Shekhtmeyster Z., Sharkey J., You S. (2011). The influence of multiple ecological assets on substance use patterns of diverse adolescents. School Psychology Review, 40(3), 386–404. [Google Scholar]
- Söderholm Carpelan K., Hermodsson A. (2004). ADAD och utvecklingen av ett dokumentationssystem för ungdomar [ADAD and the development of a documentation system for adolescents]. Nordisk sosialt arbeid, 24(2), 110–123. [Google Scholar]
- Stone A. L., Becker L. G., Huber A. M., Catalano R. F. (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors, 37(7), 747–775. [DOI] [PubMed] [Google Scholar]
- Suppiger A., In-Albon T., Hendriksen S., Hermann E., Margraf J., Schneider S. (2009). Acceptance of structured diagnostic interviews for mental disorders in clinical practice and research settings. Behavior Therapy, 40(3), 272–279. [DOI] [PubMed] [Google Scholar]
- Swedish Government Official Reports. (2011). Bättre insatser vid missbruk och beroende. Individen, kunskapen och ansvaret [Better interventions in addiction and dependence. The individual, the knowledge and the responsibility]. Swedish Government Official Reports 2011:35 Stockholm, Sweden: Fritzes. [Google Scholar]
- Swedish Ministry of Health and Social Affairs. (2013). Åtgärdsprogram för alkohol-, narkotika-, dopnings- och tobakspolitiken 2013 [Action programme for alcohol, drugs, doping and tobacco policy in 2013]. Stockholm, Sweden: Ministry of Health and Social Affairs. [Google Scholar]
- Swedish National Board of Health and Welfare. (2015). Nationella riktlinjer för vård och stöd vid missbruk och beroende. Stöd för styrning och ledning [National guidelines for treatment and support for addiction and dependence. Support for governance and management]. Stockholm, Sweden: National Board of Health and Welfare. [Google Scholar]
- Winters K. C. (2003). Assessment of alcohol and other drug use behaviors among adolescents In Allen J. P., Wilson V. B. (Eds.), Assessing alcohol problems: A guide for clinicians and researchers (2nd ed, pp. 101–123). Bethesda, MD: National Institutes of Health (NIDA; ). [Google Scholar]
- Winters K. C., Kaminer Y. (2008). Screening and assessing adolescent substance use disorders in clinical populations. Journal of the American Academy of Child and Adolescent Psychiatry, 47(7), 740–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters K. C., Stinchfield R. D. (1995). Current issues and future needs in the assessment of adolescent drug abuse In Rahdert E., Czechowicz D. (Eds.), Adolescent drug abuse: Clinical assessment and therapeutic interventions (pp. 146–171). NIDA Research Monograph 156 Rockville, MD: National Institute on Drug Abuse. [PubMed] [Google Scholar]
- Winters K. C., Stinchfield R. D., Henly G. A., Schwartz R. H. (1991). Validity of adolescent self-report of alcohol and other drug involvement. The International Journal of the Addictions, 25(11), 1379–1395. [DOI] [PubMed] [Google Scholar]