Abstract
Aim:
The purpose of this qualitative study was to investigate the effects experienced by users of a novel psychoactive substance, the benzodiazepine flubromazolam, by analysing users’ own accounts on the Swedish forum Flashback.org.
Method:
A thematic analysis of anonymous self-reports published on the forum was performed and generated five general themes describing effects and experiences by flubromazolam users.
Results:
The themes which emerged were: Onset and duration, Desired effects, Adverse effects and addiction, Loss of control, General estimations and evaluations. The main reported characteristics of flubromazolam were heavy hypnotic and sedative effects, long-lasting amnesiac effects and the rapid development of tolerance. Flubromazolam was also anxiolytic and acted as a muscle relaxant for many users. Some users experienced euphoria or intense wellbeing. Other prominent characteristics were loss of control (leading to poor choices and actions, with unpleasant consequences) and long-lasting, often severe withdrawals. There were also serious incidents where users had been admitted to hospital, acute psychiatric treatment or taken into custody by the police.
Conclusion:
Flubromazolam appears to be a highly addictive and precarious benzodiazepine with many, possibly severe, side effects. The substance is generally described as very potent and with long-lasting effects. Memory loss and loss of control are common adverse effects, and withdrawals appear to be severe for many users.
Keywords: addiction, benzodiazepine, drug discussion forum, flubromazolam, harm reduction, novel psychoactive substance, NPS
Novel psychoactive substances (NPS) are readily available on the internet. In the past five years there has been a steep rise in available psychoactive substances, and currently 560 new drugs are being monitored by the European Monitoring Centre for Drugs and Drug Addiction. In 2015, 100 new substances were identified, and five of these were benzodiazepines (EMCDDA, 2016a).
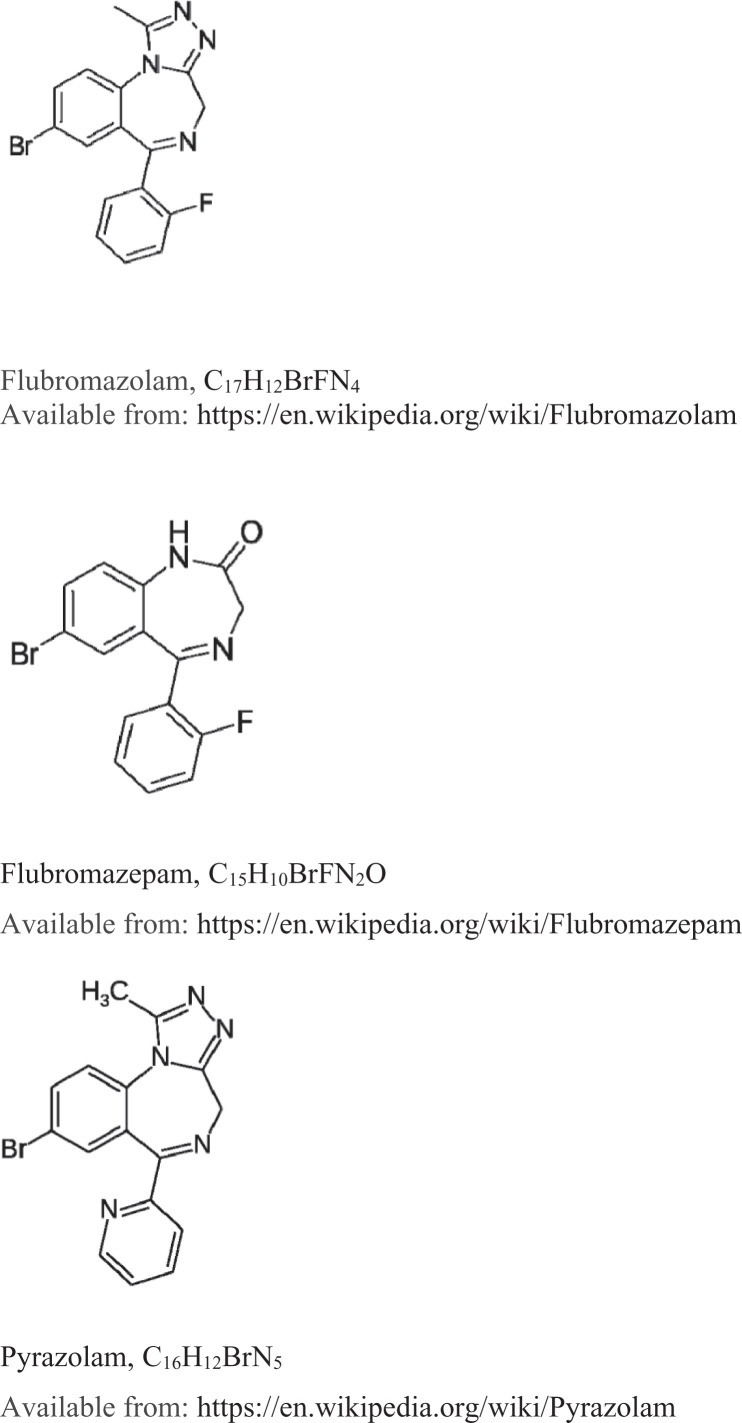
Misuse of NPS benzodiazepines has been identified as an increasing problem among drug users (e.g., Høiseth, Skogstad Tuv, & Karinen, 2016; Moosmann, King, & Auwärter, 2015). In our study, the focus is one such novel benzodiazepine, flubromazolam, which is chemically similar to, for example, flubromazepam and pyrazolam (See Figure 1). Such substances have been connected with toxic reactions and severe acute poisonings (Łukasik-Głębocka et al., 2016; Swedish Prosecution Authority, 2016).
Figure 1.
The chemical structure of the three novel psychoactive benzodiazepines: flubromazolam, flubromazepam and pyrazolam
In Sweden flubromazepam and pyrazolam were classified as narcotic substances in April 2014, and were joined by flubromazolam in June 2015 (Medical Products Agency, 2015). At the time of the data gathering for our study, flubromazolam was still legally available. The Swedish Drug Users Union issued early warnings in 2014 on their website regarding flubromazolam, encouraging drug users to refrain from using it (and rather choose other, better-known substances) in order to prevent unnecessary harm or fatalities. Based on these warnings, together with indications that flubromazolam had gained increased popularity and was frequently discussed on the Swedish forum Flashback.org, we chose flubromazolam as the subject for our study.
In 2015, flubromazolam was classified as a narcotic substance in Switzerland (Der Bundesrat Switzerland, 2015). In the United Kingdom, the Psychoactive Substances Act has made it illegal to produce, supply or consume flubromazolam (Psychoactive Substances Act, 2016). Still, flubromazolam continues to occupy a legal grey area in many parts of the world. A simple Google search in November 2016 with the words “buy flubromazolam” revealed several online vendors offering the substance for worldwide delivery.
Pharmaceutical benzodiazepines, on the other hand, are prescribed in clinical practice for a wide variety of psychiatric and neurological conditions, primarily for anxiety and insomnia. Muscle spasms, epilepsy and detoxification from alcohol and other substances are other common clinical uses for these benzodiazepines (Hollister, Müller-Oerlinghausen, Rickels, & Shader, 1993). There is a range of benzodiazepines, all acting as central nervous system (CNS) depressants by a positive allosteric modulation of the GABAA receptor complex, which is among the most abundant in the CNS (EMCDDA, 2015; Jones, Mogali, & Comer, 2012).
The relatively high therapeutic index of most pharmaceutical benzodiazepines purports that they are relatively safe, but their use still presents several, and sometimes severe, side effects and clinical issues such as dependence, rebound anxiety, memory impairment and withdrawal syndromes (Dell’osso & Lader, 2013; Uzun, Kozumplik, Jakovljević, & Sedić, 2010).
The misuse of (medically prescribed) benzodiazepines has been identified as a concern among several groups in the population (EMCDDA, 2015). Benzodiazepines are rarely fatal if ingested singularly but will potentiate CNS depression caused by co-ingested substances like opioids (Bateman, 2012) or alcohol. A diverse population of polydrug users of various subgroups commonly use benzodiazepines to extend or balance the effects of other drugs (Darke, 1994; Darke, Ross, & Cohen, 1994; Kurtz, Surratt, Levi-Minzi, & Mooss, 2011; Ross, Darke, & Hall, 1997). Subsequently, there is a substantial user base that might have interest in the often cheaper and more readily available NPS benzodiazepines.
Considering that research studies are scarce for most NPS, it can be hard to assess their toxicity, addiction potential or general effects profile. To produce a better understanding of the effects and possible harms of newly emerging substances in the rapidly evolving drug market, internet drug discussion forums and users’ own accounts of their experiences have proven to be a valuable source for surprisingly accurate early research data on NPS when other research studies are not available (Kjellgren, Henningsson, & Soussan, 2013; Soussan & Kjellgren, 2014a, 2014b, 2016). The value of using public internet drug discussion fora as a general platform for drug research has also been capitalised on by several researchers (Røed-Bilgrei, 2016; Rönkä & Katainen, 2017).
The aim of this qualitative study was to investigate the effects experienced by users of the NPS benzodiazepine flubromazolam by systematic analysis of the users’ own accounts in the Swedish discussion forum Flashback.org.
Method
Data collection
The raw data for our study consisted of anonymous self-reports published by users of flubromazolam. All reports were extracted from a discussion in the public domain of the Flashback.org internet forum. This is the largest Swedish internet-based discussion forum, with over a million registered users and covering a wide range of topics. We made use of a discussion on flubromazolam, with 1588 posts between 22 August 2014 and the date of the data collection, 11 February 2015. The discussion had 122 participants (individual user aliases). As the data were collected when flubromazolam was still unclassified, a new search on the Flashback.org forum was performed six months after classification to reference how discussions were affected by the new legal status.
Analysis
The data were prepared and analysed using the steps of inductive thematic analysis according to Braun and Clarke (2006). Thematic analysis is a widely used method for identifying, analysing, interpreting and reporting recurring patterns in qualitative data. The data for the present study were coded and categorised by computer-assisted content analysis using research software QSR NVivo 11. Our focus for this study was to recognise themes at an explicit level rather than on implicit or interpretative levels. The analysis carefully followed the checklist of criteria for good thematic analysis (Braun & Clarke, 2006) to ensure a consistent analysis with as little preconceptualisation as possible. To check for verification and consistency, the results were continually matched with the original dataset throughout the process.
The analysis resulted in 773 coded elements (CE), which were then assorted in 79 categories, and as a final step, related to five general themes: Onset and duration, Desired effects, Adverse effects and addiction, Loss of control, and General estimations and evaluations.
Ethical considerations
This study was based on freely available data in the public domain. There was no interaction with the users, and no user profile or login on the Flashback.org forum was created to obtain the data. The information available was therefore considered to be an observation of public behaviour online, in compliance with the ethical guidelines and recommendations provided by SACHRP (2013). In order to protect the confidentiality of the users, no aliases, URLs, names or identifiable data have been stored or presented in the article. All quotations have been translated from Swedish and slightly altered to prevent backtracking.
Results
The five themes resulting from the thematic analysis are presented below together with some illustrative quotations.
Onset and duration
User descriptions regarding onset and duration time of flubromazolam, and how different methods of administration were utilised to modulate onset, duration time and some characteristics of the effects, are outlined in this theme.
Onset time was generally described as quite long, but some users characterised flubromazolam as acting rapidly. Onset time appears to vary individually from only 10 minutes to several hours, also depending on dosage and method of administration. Not all users mentioned how they administered the drug, but oral use of flubromazolam, in pill form, was the most common route described.
Examples of effective rectal, nasal, sublingual and intravenous administration, as well as inhalation (smoking and vaporisation) were described by the flubromazolam users. Smoking, nasal, rectal and intravenous administration were generally depicted as shorter acting, with faster onset compared to the more common route of oral administration. Intravenous administration was reported to give a “rush” not experienced by any other way of administration: “I have tried all the usual benzodiazepines. But flubromazolam is the only one that actually was something for me. It’s no heroin or amphetamine, but ‘shooting’ it sure gives a decent rush”. The faster acting routes of administration were frequently utilised by flubromazolam users aiming to get “high” or “wasted”, and not commonly used by the “self-medicating” users.
Generally, flubromazolam was said to be a long-lasting benzodiazepine with lingering (side) effects for up to several days, even from a single use: “I ingested a high dose on Friday. More or less asleep until Sunday, and was still under the influence when waking up”. Some users described immediate anxiolytic effects but some attained rather more of the anxiolytic effects on the day following ingestion: “Flubromazolam had the best effect when I used maximum 1 mg before bedtime. Then I woke up in a nice relaxed and anxiety-free state that lasted throughout the following day”. For a few, the long-lasting and lingering effects were described as desirable, while for others this characteristic of flubromazolam was not sought after, or was perceived as unpleasant, leading to a discontinuation of use.
Desired effects
This theme summarises effects of flubromazolam that were enjoyed and desired by users. Most commonly, users of flubromazolam appreciated the heavy sleep-inducing effects. Self-medicating for various ailments was described as an incentive to use flubromazolam; the controlling of anxiety, nervousness, panic attacks and social unease was felt to be facilitated by flubromazolam. Occasional reports also described how flubromazolam was used to cope with, or to break, manic episodes. A few users reported increased energy levels and a pleasurable lessening of inhibition as desired effects.
The sedative effects were praised by many users with insomnia. To have a full night’s sleep with pleasant dreams and not to wake up several times a night was described as a highly appreciated effect: “I haven’t slept for more than 1.5 hours at a time the last two years. I’m so happy and relieved to finally do so”. Overall relaxation of body (muscle relaxation) and mind was also commonly mentioned as a pleasant and desired effect: “The pills were superb. Gave me deep relaxation in my body, and released me from my anxiety. I feel like a new person!” Other users mentioned an overall, and for some, intense, feeling of wellbeing or even euphoria. Occasionally some users also described a heightening of musical appreciation.
Quite a few users described a numbing intoxication, phrased as being “wasted”, or “woolly”, as the main incentives for using flubromazolam: “I’m going to try this substance to find out if it’ll be nice for some dopey chilling out”.
While most users reported heavy sedative and hypnotic effects, there were also examples of users who described increased energy and power of initiative, facilitating daily chores or work. A few users expressed how the effects made them feel “chattier” and more open to engage in social situations. But while a lowering of inhibitions was a common effect, the heavy sedative and hypnotic effects meant that very few users were using flubromazolam to facilitate social situations.
Adverse effects and addiction
Flubromazolam users described a wide range of serious adverse effects, both physical and psychological. The addictive potentiality, and increased tolerance with prolonged and often severe withdrawals, were reported as typical pitfalls of this substance. Many users also described various degrees of cognitive impairment, from slight confusion or problems with writing to not being able to walk or talk at all.
While most users seemed to appreciate the long-lasting and heavy sleep-inducing qualities of flubromazolam, others were dismayed by waking up a day (or more) later with no recollection of ever falling asleep. A few users described unpleasant dreams and others reported much worse sleeping problems after discontinuation of use. Sleeping paralysis was mentioned as one example of the negative effects experienced after discontinuation of flubromazolam use.
Flubromazolam was described by many as producing worse and longer withdrawals than any other benzodiazepines. Symptoms of withdrawals ranged from muscle aches, chills, sleeping disorders and panic attacks to dissociative symptoms, perceptual distortions, severe anxiety, cramping, vomiting and seizures. Depending on length of use and dosage, the withdrawals were said to last from a couple of days to over a month:
It was a tortuous comedown, with shivering, anxiety, pain and vomiting. I was sort of back to normal after 20 days // Terrible withdrawals. One week of use causes similar symptoms as months of using another benzodiazepine.
Most users agreed on the rapid onset of tolerance effects of flubromazolam. Some reported multiplying the dose already after just a week’s use, by even as much as 30 times the original dose to achieve the desired effects. However, this seemed more the case for those users whose main purpose was to get “high” or “wasted” and who therefore used high doses. “Self-medicating” users would typically retain the same low dosage successfully over longer periods of time to facilitate sleeping or handle anxiety: “I’ve been using flubromazolam for insomnia for 3–4 months and didn’t need to up the dosage”.
A worsening of anxiety both during and after flubromazolam use was also mentioned. Difficult anxiety and discomfort could occur even after a single use. A few users described depressive effects and found themselves rather sad and tearful more than anything else from this substance. Several users also described feelings of emotional coldness toward others after using flubromazolam.
Several physical side effects were also described. Palpitations, pain and sharp twinges around the heart, as well as gastrointestinal problems were cited as acute side effects. Impotence and loss of libido were occasionally also given as possible side effects. Visual distortions during use or comedown were quite commonly described. One person reported experiencing temporary blindness in one eye in the days after use: “My body was unruly the day after use; my legs were like rubber, I stumbled and was blind in my right eye, so it was more or less impossible to read anything”.
Loss of control
A combination of effects or adverse effects of flubromazolam sometimes resulted in a more or less total loss of personal control and discernment, in worst cases leading to harm of self or others. These adverse effects were so qualitatively distinctive and prevalently described throughout the data that they were categorised as a theme of their own.
Flubromazolam was characterised as a very sedating and hypnotic substance, sometimes inducing sleep or somnambulistic states for several days. Memory loss seemed to be a highly pronounced effect for most users and, together with an impaired self-assessment capability, this sometimes developed into a more or less total loss of control: “My friends apparently had come over to visit, which I don’t remember at all. They didn’t even realize I was totally wasted. The autopilot is really good at doing his job, the poor bastard”.
Several flubromazolam users described an urge to ingest more of the substance while under the influence, which in combination with memory loss and lowered inhibitions led users to ingest more of the substance than originally intended. They would typically describe “coming to their senses” the next day, or several days later, to find an unexpected amount of pills missing.
One user was planning to let a friend (who was not using) hold on to his supply of flubromazolam when trying the substance out again, so as to prevent ingesting more than intended while affected:
I flushed most of them down the toilet, I don’t trust myself to refrain from using them, I’m scared to get hooked on flubromazolam // A craving for more, you feel great but you want to feel even better.
Several users said that they had ended up in emergency clinics or acute psychiatric treatment, sometimes after losing control and ingesting higher doses of flubromazolam than intended: “I took a total of 1 mg and went to bed. I woke up 48 hours later and 100 mg of flubromazolam was gone. Eight of these hours were apparently spent at the police station”.
Another aspect of losing personal control and discernment, described by several users, was a tendency to start shoplifting under the influence of flubromazolam, even when they had never before been involved in this kind of behaviour: “Damn, I went and stole a fillet of pork and fried it whole. I never shoplifted before” // “You go shopping, or shoplifting, I actually don’t know what the fuck I did. Completely unnecessary stuff as well”. A few, apparently regretful, flubromazolam users also reported aggressiveness or hostile acts committed under the influence.
General estimations and evaluations
This theme summarises the various general evaluations and assessments by the users to review their experiences and characterise flubromazolam. Flubromazolam was generally described as having very strong effects and being a very potent, and by many as being a highly precarious benzodiazepine. The effects were often compared to those of flunitrazepam (Rohypnol), but most seemed to agree that flubromazolam is more potent and has longer and worse withdrawals. Some reviews were also based on either disappointment over the lack of or undesirability of effects.
Overall, many users were happy with the potency and effects profile, but those describing no or very weak effects were also relatively prevalent. Disappointment and unfulfilled expectations may stem from users not experiencing any anxiolytic effects or not attaining the long-lasting deep sleep sought by many. Other users were disappointed by the lack of any particular wellbeing or euphoric effect that they were expecting. Generally flubromazolam was described as heavily sleep-inducing, and to numerous users the sedating effects were too pronounced for them to enjoy or use this substance as anything else but a sleeping aid:
Disappointed not to get any happy phase, or if that occurs, you fall asleep before you feel it.
I only get very tired, I’m disappointed!
I don’t find this substance gives any euphoria of feel-good effects. I.e. nothing for recreational use.
To combat the sedative effects a few users suggested mixing flubromazolam with a CNS stimulant drug.
Flubromazolam was also characterised as very unpredictable and hard to dose correctly. Some users explained their contradictive views on flubromazolam as due to the varying quality of different batches from different vendors. Some suspected that they had been sold a completely different substance: “My mental state became really strange from one batch and I sought medical treatment, same thing happened to my girlfriend”. Among those who used flubromazolam in pill form, many reported that the pills were of too high dosage (reliable data on the exact dosage of various batches was not given by the users).
The unpleasant effects were quite often predominant in the evaluation of flubromazolam. Many users said they were frightened of the strong (“zombifying”) effects and did not want to use it again:
I tried 2 mg, and did not come out from the haze until several days later. I’m shocked, you literally turn into a zombie on this drug at that dosage. I flushed the rest in the toilet; I’m scared to ever try this one again.
Most commonly, users expressed fear of the possible heavy withdrawals and loss of personal control or discernment, leading to potentially harmful behaviour under the influence of flubromazolam:
I get extremely emotionally cold on flubromazolam. I was on it for a couple of months and didn’t realize how I behaved toward others. I was confronted by friends and I realised that I was experiencing memory loss for weeks and that the months prior had all been very foggy. Flubromazolam has made me afraid for myself.
Several warnings were issued by the users regarding this substance. Some were calling for caution, to use low doses and stay at home, while others discouraged anyone to try this substance altogether:
Everybody should be careful with flubromazolam. My friend didn’t follow my instructions to only use a quarter of the red ones. Now he’s home again from the hospital, one experience richer. I never use more than that, often even less. And I do this only once a week to get a deep sleep for 9–10 hours.
Several users stressed that flubromazolam should be used in low doses to be useful (i.e., for sleeping disorders, anxiety) or manageable, and to minimise tolerance build-up and side effects like memory loss or heavy withdrawals. Mixing flubromazolam with alcohol was strongly discouraged, as this combination was described to lead to memory loss and loss of control.
One user summarised vividly the slippery slope of the effects flubromazolam can have on behaviour: “The first day you pass out, the second day you shoplift, the third day you’re carrying a knife”.
Discussion
The aim of this study has been to outline effects experienced by users of the NPS benzodiazepine flubromazolam as described on the Swedish internet forum Flashback.org. Computer-assisted thematic analysis was performed on data from a discussion with posts by 122 individual user aliases, which yielded 79 categories that were further related to five general themes: Onset and duration, Desired effects, Adverse effects and addiction, Loss of control, and General estimations and evaluations.
The results give an estimation of effects and adverse effects caused by flubromazolam. These findings indicate a typical profile of high affinity for the GABAA receptor complex, as would be expected from a CNS depressant benzodiazepine (Uzun et al., 2010).
Flubromazolam was categorised by most users as a highly potent benzodiazepine, somewhat similar to flunitrazepam (Rohypnol), but generally stronger, longer lasting and with worse and lengthier withdrawals. The main characteristics of flubromazolam included heavy hypnotic and sedative effects, long-lasting amnesiac effects (that could cover several days and in some cases even weeks) and the rapid development of tolerance. Flubromazolam was also reported to be anxiolytic and acted as a muscle relaxant. Some users also experienced euphoria or intense wellbeing.
Other prominent reported characteristics were loss of control (leading to poor choices and actions, with unpleasant consequences). Serious incidents where users were admitted to hospital, acute psychiatric treatment or taken into custody by the police were also described. The long-lasting withdrawals were frequently cited as more severe than withdrawals from other benzodiazepines.
The loss of control reported by flubromazolam users is something far more than the often sought after lessening of control or loosening of inhibitions, which can in fact be a desired effect from using drugs. A complex combination of different effects, or adverse effects, of flubromazolam appears at times to result in a more or less total loss of personal control and discernment, which may have dire consequences. Several flubromazolam users described the loss of control as a severe effect temporarily impairing the core characteristics and morals or conscience of the intoxicated person, rendering the user more or less incapable to assess how their actions affected themselves or others, but still fully capable of acting on impulses and desires. This was reported as very negative and frightening, and sometimes as leading to various forms of criminal or harmful behaviour. Based on the present data, no causal link can be established between the pharmacological properties of flubromazolam and the specific criminal behaviours described in the results; however, the participants attribute such behaviour to effects of flubromazolam. Also, the connection between misuse of hypnotic benzodiazepines in general and various forms of criminal behaviour is already known and has been described by others (e.g., Boles & Miotto, 2003).
For many users the addictive potential of flubromazolam seems to assert itself quite immediately, as the intoxicating effects (before any abstinence effects set in) were reported to generate an immediate craving for more of the substance. These properties, combined with the loss of control and discernment, and together with prolonged and heavy withdrawals, render this substance a very likely candidate for problematic use. Also, flubromazolam has a relatively high pharmacological potency (Huppertz et al., 2015), which makes it harder to accurately dose and thereby increases the prospect of potential overdosing. Some users in our study described ending up in police custody or emergency clinics or seeking acute psychiatric treatment after overdosing or having a bad reaction to flubromazolam. According to a previous case study, a 27-year-old male was admitted to hospital (intensive care) in a deep coma with acute respiratory failure and hypotension about 19 hours after ingesting not more than 3 mg of flubromazolam (Łukasik-Głębocka et al., 2016). This case study and the overall characterisation given by the flubromazolam users in our study indicate a narrower safety ratio than with most medically prescribed benzodiazepines.
Overall, the users’ perceptions of this substance were somewhat contradictory. A relatively large group felt flubromazolam was not enjoyable or helping with their particular affliction. Some found it terrible, “zombifying” and said it was insidious to use. Other users expressed how they enjoyed, or were helped by flubromazolam, over longer periods of time without experiencing deterring adverse effects.
A few, describing themselves as experienced users of benzodiazepines, maintained that this substance in many ways was “worse” than other benzodiazepines, and issued strong warnings to other potential users of the Flashback.org forum: “I have used ‘benzo’ for 15 years but one week of flubromazolam literally almost cost me my life”. In contrast, there were also some users contesting these admonitions and alarming views of flubromazolam, stating that the many warnings and bad experiences from this substance mainly were due to users not understanding the potency and using dosages that were far too high. These users made the argument that very high dosage and lengthy use of most benzodiazepines would cause comparable side effects and equally severe withdrawals. There were also several examples of flubromazolam users stating that they had “successfully” used very low doses for specific self-medication purposes, over longer periods of time, without any serious side effects or increased tolerance: “If you get totally wasted by 0.25 mg, maybe, just maybe you shouldn’t have 1 mg the next time? Sigh.! I used 0.25 mg for a few weeks and didn’t notice any adverse effects during or after use”.
In our view, the reported severe adverse effects are most likely a consequence of both reckless misuse and the pharmacological properties of flubromazolam. The strength and dosage of various batches is possibly also a factor to consider. A relationship between dosage and incentives to use (i.e., recreational, self-medication or compulsive) was suggested in the many accounts of loss of control and severe withdrawal, but we could not entirely elucidate this connection. As we have no reliable data either on the strength and quality of different batches, or on the exact amounts ingested by the users, there is no real basis for accurately evaluating this relationship. However, it seems to be that none, or very few, of those using low dosages for self-medication purposes experienced the “slippery slope” effects on personal behaviour.
Although some users attested to achieving expedient relief or enjoyment from this substance, the discussions were usually not characterised by drug-romantic content or recruiting new users. There was rather more focus on reciprocal harm reduction and information exchange. Alongside the many dire warnings not to use this substance at all, many posts were quite nuanced and advocated a highly cautious approach with flubromazolam to avoid tolerance, addiction or any of the common side effects. Usual recommendations advised not to use flubromazolam more than a couple of times a week and in very low doses. Discussions on safety, dosage and information exchange regarding different vendors and batches of flubromazolam contributed to the harm-reduction content. Similar observations on the characteristics of drug discussions have been made in previous studies of drug discussion forums (e.g., Soussan & Kjellgren, 2014a, 2014b).
While harm reduction is not a stated objective of the Flashback.org forum, it is nevertheless a part of the forum’s drug discussions and the reciprocal knowledge-producing process in general. Duxbury (2015) mentions how drug discussion forum boards are organised by substance, or substance group, and how this generates discourses in relation to a specific type of drug. Although the discourse of the flubromazolam reports was possibly not as systematically and meticulously investigating as some drug forum discussions can be, our impression was that the “citizen science” aspects of the flubromazolam reports incorporated important and crucial elements that can contribute to a relevant harm-reduction perspective.
We can only speculate on the particular demographics of the Swedish Flashback.org forum and on the specific group using and discussing flubromazolam. What we do know is that Sweden is particularly interesting in a drug policy perspective, as mortality from drug use is the second highest in the EU (EMCDDA, 2016b), despite a relatively low overall drug consumption and a long tradition of restrictive drug policies (EMCDDA, 2016c). Mortality from NPS drugs is also on the rise in Sweden (National Board of Health and Welfare, 2016). Sweden has recently begun to officially incorporate some harm-reduction approaches, but drug use is still criminalised and often “taboo” to discuss, which naturally influences official discourse. In this situation, anonymous drug discussion forums possibly cater to an increased need among Swedish drug users to communicate openly and freely on various drug uses and to share information.
We cannot guarantee how well the forum discourse represents offline flubromazolam users. Although, since flubromazolam is mainly sold and discussed on the internet and most likely has its main user base among the internet-using population, there may not be a substantial user base outside this environment.
As several flubromazolam users were motivated by various self-medicating purposes, the reality of flubromazolam (and other NPS benzodiazepines) should be considered by healthcare providers to avoid dangerous interactions when prescribing medications. In addition, prescribing physicians should be attentive to the fact that certain patients sometimes turn to precarious NPS substances if they do not receive effective treatment. As described in previous studies, the incentive of “substance displacement” – when users are turning to precarious NPS as a substitute for medication or better known substances – is an important consideration both for policy makers and medical personnel (Andersson & Kjellgren, 2016).
Even though flubromazolam is now a classified narcotic substance in many parts of the world, there are reasons to believe it can often go undetected in standard drug tests. Some flubromazolam users from the Flashback.org forum attested to being subjected to drug testing while using flubromazolam, and the substance did not show up in standard tests for benzodiazepines. According to Huppertz et al. (2015), the high potency of flubromazolam normally implicates a very low blood concentration, making it difficult to detect and identify in biological samples.
The discussion on Flashback.org used for this study was revisited six months after the Swedish classification of flubromazolam. There were considerably fewer posts and decreased interest in flubromazolam after classification. In the six months prior to classification the discussion had over 1100 posts on flubromazolam, whereas the post count during the six months after classification was just below 100. There is, however, no reason to believe that the general interest in “designer” benzodiazepines is, or will be, lessening: interest rather shifts to ever new, and possibly even more precarious, substances not yet classified.
Limitations
The accuracy of individual reports cannot be guaranteed. Since the supply chain of NPS is not regulated by any supervisory authority nor subjected to any regulatory protocol and monitoring of the manufacturing process, users do not always know what substance they are ingesting. Information on dosage was sometimes ill defined or missing. Additionally, the amount and quality of active substance can vary between batches. Therefore, we were not able to entirely elucidate the connection between dosage and effects. The basis for this study implies that it was not possible to rule out other substances being used together with flubromazolam. Furthermore, the users’ varying tolerance also implies a great impact on subjective effects, and a study based exclusively on participants with no pre-developed tolerance to flubromazolam or other benzodiazepines could have generated a slightly different result.
Despite the limitations of this study, we find no reason to believe that the described overall effects profile of flubromazolam is not generalisable. Certainly, there could be particulars in the reports and subjective experiences of flubromazolam that are culturally specific for the Swedish demographic or the specific users of the Flashback.org forum, but as a whole the effects described are consistent with what is previously known of benzodiazepines in general and flubromazolam in particular.
Conclusions
Flubromazolam appears to be a highly addictive and precarious benzodiazepine with many, possibly severe, side effects. The substance is generally described as very potent and long-lasting. Memory loss and loss of control are common adverse effects, and withdrawals seem to be very severe for many users. Serious incidents were reported where users had overdosed or experienced other adverse reactions, and consequently were subjected to emergency care or sought acute psychiatric assistance. Other users had been taken into police custody during memory loss or loss of control of personal behaviour.
Medical personnel should observe flubromazolam and similar analogue NPS benzodiazepines to avoid possibly harmful interaction effects when medications are prescribed to patients with an ongoing NPS benzodiazepine use. Also, prescribing physicians need be aware that certain patients may turn to precarious NPS benzodiazepines if they do not receive effective medication. Our study also showed how drug discussion forums are used to endorse harm reduction through warnings and guidelines on safer drug use.
Acknowledgements
The authors wish to acknowledge the Public Health Agency of Sweden and the county council of Värmland, which supported the present study with unrestricted grants. Also thanks to Mona Jonsson for valuable help with data gathering.
Footnotes
Declaration of conflicting interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Public Health Agency of Sweden and the county council of Värmland, Sweden.
Contributor Information
Martin Andersson, Karlstad University, Sweden.
Anette Kjellgren, Karlstad University, Sweden.
References
- Andersson M., Kjellgren A. (2016). Aspects of substance displacement: From illicit drugs to novel psychoactive substances. Journal of Addiction Research and Therapy, 7(3), 1000283. doi:10.4172/2155-6105.1000283 [Google Scholar]
- Bateman D. N. (2012). Benzodiazepines. Medicine, 40(3), 111 doi:10.1016/j.mpmed.2011.12.004 [Google Scholar]
- Boles S. M., Miotto K. (2003). Substance abuse and violence: A review of the literature. Aggression and Violent Behavior, 8(2), 155–174. doi:10.1016/S1359-1789(01)00057-X [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. [Google Scholar]
- Darke S. (1994). The use of benzodiazepines among injecting drug users. Drug and Alcohol Review, 13(1), 63–69. doi:10.1080/09595239400185741 [DOI] [PubMed] [Google Scholar]
- Darke S., Ross J., Cohen J. (1994). The use of benzodiazepines among regular amphetamine users. Addiction, 89(12), 1683–1690. doi:10.1111/j.1360-0443.1994.tb03769.x [DOI] [PubMed] [Google Scholar]
- Dell’osso B., Lader M. (2013). Do benzodiazepines still deserve a major role in the treatment of psychiatric disorders? A critical reappraisal. European Psychiatry, 28(1), 7–20. doi:10.1016/j.eurpsy.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Der Bundesrat Switzerland. (2015). Verordnung des EDI über die Verzeichnisse der Betäubungsmittel, psychotropen Stoffe, Vorläuferstoffe und Hilfschemikalien [Regulation of the EDI on the directories of Psychotropic drugs, precursors, and auxiliary chemicals]. Retrieved from https://www.admin.ch/opc/de/classified-compilation/20101220/index.html
- Duxbury S. W. (2015). Information creation on online drug forums: How drug use becomes moral on the margins of science. Current Sociology. Advance online publication. doi:10.1177/0011392115596055 [Google Scholar]
- EMCDDA, European Monitoring Centre for Drugs and Drug Addiction. (2015). The misuse of benzodiazepines among high-risk opioid users in Europe. Retrieved from http://www.emcdda.europa.eu/topics/pods/benzodiazepines
- EMCDDA, European Monitoring Centre for Drugs and Drug Addiction. (2016. a). EU drug markets report: Strategic overview 2016. Retrieved from http://www.emcdda.europa.eu/system/files/publications/2374/TD0416161ENN_1.PDF
- EMCDDA, European Monitoring Centre for Drugs and Drug Addiction. (2016. b). Europeisk narkotika rapport; trender och utveckling 2016 [European drug report; trends and developments in 2016]. Retrieved from http://www.emcdda.europa.eu/system/files/publications/2637/TDAT16001SVN.pdf
- EMCDDA, European Monitoring Centre for Drugs and Drug Addiction. (2016. c). ESPAD report 2015: Results from the European school survey project on alcohol and other drugs. Retrieved from http://www.espad.org/sites/espad.org/files/ESPAD_report_2015.pdf
- Hollister L. E., Müller-Oerlinghausen B., Rickels K., Shader R. I. (1993). Clinical uses of benzodiazepines. J Clin Psychopharmacol, 13(6), 1S–169 S. doi:10.1097/00004714-199312001-00001 [PubMed] [Google Scholar]
- Høiseth G., Skogstad Tuv S., Karinen R. (2016). Blood concentrations of new designer benzodiazepines in forensic cases. Forensic Science International, 268, 35–38. doi:10.1016/j.forsciint.2016.09.006 [DOI] [PubMed] [Google Scholar]
- Huppertz L. M., Bisel P., Westphal F., Franz F., Auwärter V., Moosmann B. (2015). Characterization of the four designer benzodiazepines clonazolam, deschloroetizolam, flubromazolam, and meclonazepam, and identification of their in vitro metabolites. Forensic Toxicology, 33(2), 388–395. [Google Scholar]
- Jones J. D., Mogali S., Comer S. D. (2012). Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug and Alcohol Dependence, 125(1–2), 8–18. doi:10.1016/j.drugalcdep.2012.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjellgren A., Henningsson H., Soussan C. (2013). Fascination and social togetherness: Discussions about spice smoking on a Swedish internet forum. Substance Abuse: Research and Treatment, 27(7), 191–198. doi:10.4137/SART.S13323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz S. P., Surratt H. L., Levi-Minzi M. A., Mooss A. (2011). Benzodiazepine dependence among multidrug users in the club scene. Drug and Alcohol Dependence, 119(1–2), 99–105. doi:10.1016/j.drugalcdep.2011.05.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Łukasik-Głębocka M., Sommerfeld K., Teżyk A., Zielińska-Psuja B., Panieński P., Żaba C. (2016). Flubromazolam: A new life-threatening designer benzodiazepine. Clinical Toxicology, 54(1), 66–68. doi:10.3109/15563650.2015.1112907 [DOI] [PubMed] [Google Scholar]
- Medical Products Agency. (2015). 16 nya ämnen narkotikaklassas [16 new substances classified]. Retrieved from https://lakemedelsverket.se/Alla-nyheter/NYHETER-2015/16-nya-amnen-narkotikaklassas
- Moosmann B., King L. A., Auwärter V. (2015). Designer benzodiazepines: A new challenge. World Psychiatry, 14(2), 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Board of Health and Welfare. (2016). Narkotikarelaterade dödsfall [Drug-related deaths]. Retrieved from http://www.socialstyrelsen.se/publikationer2016/2016-2-32
- Psychoactive Substances Act. (2016). Retrieved from http://www.legislation.gov.uk/ukpga/2016/2/contents/enacted
- Røed-Bilgrei O. (2016). From “herbal highs” to the “heroin of cannabis”: Exploring the evolving discourse on synthetic cannabinoid use in a Norwegian internet drug forum. International Journal of Drug Policy, 29(3), 1–8. doi:10.1016/j.drugpo.2016.01.011 [DOI] [PubMed] [Google Scholar]
- Rönkä S., Katainen A. (2017). Non-medical use of prescription drugs among illicit drug users: A case study on an online drug forum. International Journal of Drug Policy, 39(1), 62–68. doi:10.1016/j.drugpo.2016.08.013 [DOI] [PubMed] [Google Scholar]
- Ross J., Darke S., Hall W. (1997). Transitions between routes of benzodiazepine administration among heroin users in Sydney. Addiction, 92, 697–705. doi:10.1111/j.1360-0443.1997.tb02936.x [PubMed] [Google Scholar]
- SACHRP, Secretary’s Advisory Committee on Human Research Protections. (2013). Considerations and recommendations concerning internet research and human subjects research regulations. Washington, DC: US Department of Health and Human Services. [Google Scholar]
- Soussan C., Kjellgren A. (2014. a). The flip side of “spice”: The adverse effects of synthetic cannabinoids as discussed on a Swedish internet forum. Nordic Studies on Alcohol and Drugs, 31(2), 207–220. doi:10.2478/nsad-2014-0016 [Google Scholar]
- Soussan C., Kjellgren A. (2014. b). Harm reduction and knowledge exchange: A qualitative analysis of drug-related internet discussion forums. Harm Reduction Journal, 11(25). doi:10.1186/1477-7517-11-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soussan C., Kjellgren A. (2016). The users of novel psychoactive substances: Online survey about the characteristics, attitudes and motivations. International Journal of Drug Policy, 32, 77–84. doi:10.1016/j.drugpo.2016.03.007 [DOI] [PubMed] [Google Scholar]
- Swedish Prosecution Authority. (2016). Narkotika – Preparatbeskrivning [Narcotics: Description of substances]. Stockholm, Sweden: Utvecklingscentrum; Retrieved from https://www.aklagare.se/globalassets/dokument/rattspromemorior/rattspm-2016-1.pdf [Google Scholar]
- Uzun S., Kozumplik O., Jakovljević M., Sedić B. (2010). Side effects of treatment with benzodiazepines. Psychiatria Danubina, 22(1), 90–93. [PubMed] [Google Scholar]