Abstract
Introduction:
As the global climate changes, heat waves are having a disproportionate impact on seniors and other socially vulnerable groups. In order to mitigate the threats of extreme heat, it is critical to develop and promote resources for coping during these events. A better understanding of the role of risk perceptions and the factors that influence them is needed in order to improve public responses to threatening events, particularly among seniors.
Methods:
This mixed-methods study examined risk perceptions and coping practices in seniors using qualitative interviews (n = 15) and a survey (n = 244) of seniors across Waterloo Region, Ontario.
Results:
Seniors showed relatively accurate risk tracking as indicated by the link between measures of actual risk and perception of personal risk. While vulnerability to heat is often believed to be associated with inaccurate perceptions of risk, within our sample, vulnerability appears more strongly related to social location and access to resources. Participants described social connections as important resources for resilience, but the stigma surrounding vulnerability, and other social norms, as barriers to seeking support.
Conclusion:
The positive relationship between participants’ risk perceptions and actual risk for negative consequences of extreme heat was an important finding, given that problems of emergency preparedness and risk reduction are often framed as issues of awareness of risk, rather than social location and inequality. Along with increased public resources for coping with extreme heat, communicating about resources, fostering social connections and reducing stigma may be important leverage points for increasing the resiliency of seniors to heat waves.
Keywords: climate change, heat waves, seniors, health promotion
Highlights
Mitigating the risks of increasing extreme heat events for seniors requires the development and promotion of public resources for coping during these events.
The lack of response to public efforts to mitigate these risks has previously been framed in terms of inaccurate risk perceptions.
Vulnerability to heat has been associated with inaccurate perceptions of risk; however, seniors in our sample showed relatively accurate risk perceptions, and vulnerability appears more strongly related to social location and access to resources.
Improving communication about available resources, building social connections and reducing social stigma and inequality can help promote better resilience among seniors during heat waves.
Introduction
Recent climate models predict that extreme weather events will increase in frequency and intensity over the next several decades,1-4 leading to significant consequences for human health.5 An increase in heat waves is particularly concerning, given the correlations among increasing global ambient temperature, increases in extreme heat events (also known as heat waves) and heat-related mortality risk. Studies have found a nonlinear association between hospitalization rates and episodic heat waves, with increased temperatures contributing to a seven-fold rise in hospital admission rates.6 The severity of heat waves is greater in cities, because of the urban heat island effect,7 and has become increasingly salient following the heatrelated deaths of over 700 people in Chicago during a heat wave in 19958 and 70 000 Europeans in 2003.9
Studies have also begun to demonstrate that heat-related illnesses and deaths disproportionately affect individuals from lower socioeconomic backgrounds,3,10 those who live alone11 and those living in areas with higher crime rates or substandard housing,2,12 suggesting that heat waves have impacts that are both socially and spatially differentiated.2,13 Seniors (those aged 65 years and older) are at higher risk for the negative consequences of heat, including hospitalization for heat-related illnesses such as heat exhaustion, heat stroke and heat syncope.6 They are also at greater risk for hospitalization for complications of pre-existing conditions and increased mortality rates during heat waves,2,6,14 a risk that is further amplified by the presence of the additional heat-related illnesses listed above.2,14 While seniors are at particular risk from the negative consequences of heat, there are only a few studies that have examined the effects of heat on this population.14-16 Given demographic trends indicating an aging population in Canada and around the world,15 a better understanding of heat mortality prevention strategies among this specific group is urgently needed.2,6,10,17
Consequently, public health departments are beginning to use more comprehensive approaches to reduce community-dwelling seniors’ vulnerability to heat waves, such as revamping infrastructure, increasing knowledge of risks and improving protective measures and response systems.4 However, many current heat-health campaigns throughout Canada and abroad report a disconnect between the communication strategies used and the behaviour performed.3,14,18-21 Others have reported little consensus on which communication styles are best for communicating an effective and impactful heat wave plan.22 Seniors’ subjective experiences of heat waves are critical to enhancing adaptive capacity,10,13,19,22,23 and changing self-perceptions of risk remains key to preventive action.1,2,19 However, only a few studies have looked at risk perceptions in relation to extreme weather, and to heat waves more specifically, among older adults.9,23,24 Enhancing our understanding of these perceptions may contribute to the development of more efficient, effective and better-tailored heat-health communication strategies,2,3,9,18 bolstering the information processing and behavioural strategies of seniors living in community or in supportive housing, and those who support them.23,25
Our current understanding of risk perceptions stems mostly from scholarship examining other forms of extreme weather (such as hurricanes or flooding).1,26 Lower risk perceptions have been linked to less effective coping strategies,21,27 whereas increased risk perceptions have been positively associated with more favourable adaptation attitudes.27,28 Those who are more aware of their own constraints are more likely to react appropriately to environmental warnings.2 Factors influencing risk perception include personal experiences of extreme weather,27-30 political dispositions, 30-32 gender,1,3 attitudes and beliefs about climate change33 and sense of selfefficacy to adapt as needed.31 Proximity to structural resources and social networks, or the lack thereof, can also amplify or dampen perceptions of risk.24,3-35
According to the few studies on seniors’ risk perceptions of heat waves, many seniors do not consider themselves to be at a “vulnerable” age,11,22 and consequently see themselves as at a lower risk than others. 1,14,21,36 In the event of heat waves, many seniors exaggerate the effectiveness of preventive measures used or deny their actual level of risk.14 Others may experience cognitive dissonance because of alternative belief systems (e.g. need to be self-reliant) or may underestimate the risks due to their limited understanding of the issues at hand.35-37
While existing research offers some initial insights, the social and contextual circumstances that inform seniors’ inadequate perceptions of the risks of heat waves and their consequent shortfalls in adaptive capacity remain largely unknown. With several researchers and public health advocates calling for further examination of this issue,2,10,14 we sought to add to the existent literature by exploring and predicting factors that contribute to the risk perceptions and coping practices and resources used by seniors in Waterloo Region, Ontario. The objectives of this study were to (1) understand seniors’ current perceptions of the risks of extreme heat, (2) identify factors that contribute to risk and risk perception, (3) explore how to improve risk perceptions and resilience to extreme heat, and (4) contribute to public policy and planning to reduce seniors’ vulnerability to heat waves.
Methods
For this project, we took a communitybased, participatory approach, using mixed methods and a sequential exploratory design to gain a deeper understanding of how seniors perceive, experience and cope with heat waves. Our approach was influenced by dominant theories of risk perception and planned behaviour, including Edelstein’s risk personality,38 which generally suggest that an individual’s evaluation of possible outcomes and their attitudes toward prescribed behaviours that affect these outcomes can predict their intentions and behaviour,38,39 but also by more recent critiques of these theories’ emphasis on internal factors and lack of attention to the broader social and environmental context.40
The project had a community focus, building on the results of a previous study exploring the impacts of a changing climate on homeless people in Waterloo Region that identified seniors as a group at particular risk, and on the partnerships created through that study. An advisory committee (consisting of representatives from local agencies serving seniors, providing housing and overseeing public planning and policy) was formed to provide input on the study design and to oversee the data collection, analysis and dissemination of results. Two local seniors who were active in their community were also hired as peer researchers and participated in the study design, data collection and analysis and dissemination of results.
The Regional Municipality of Waterloo is a mid-sized municipality that includes three cities and several rural townships in Canada, where climate models are predicting increased heat waves within the next several decades. With the support and interest of local organizations, we sought to develop research that could inform local planning and policy, with the potential to be generalized to other regions.
The study included two data collection phases: an exploratory phase consisting of 15 qualitative interviews with Waterloo Region residents aged 65 and older, and a broader quantitative survey informed by the exploratory phase. We used a combination of snowball sampling and convenience sampling, working with community partners to connect with a sample of participants likely to have important and informative experiences while also conducting broader public outreach at public events such as weekly farmers’ markets and community dinners. Exceptions to the age requirement were made for participants recommended by our community partners who had experiences that were unique or difficult to capture (such as street-involved and low-income seniors and newcomers to Canada). This allowed one interview participant, aged 51, and three survey participants, aged between 52 and 64, with important lived experiences to participate.
Ethical considerations
The Research Ethics Board at Wilfrid Laurier University approved all study procedures (REB#4482) including recruitment, data collection, storage and dissemination processes. We obtained informed consent from all interview and survey participants. The research assistants and peer researchers also participated in team interview training, which included a discussion of research ethics and confidentiality.
Qualitative interviews
In the initial interview phase, seniors were invited to participate in a brief screening questionnaire to determine their eligibility to participate in the study, and to assess demographic factors to improve the representativeness of our sample. We invited eligible participants to participate in an interview covering topics such as experiences of extreme weather, perceptions of current weather and broader climate, perceived risks of heat waves for themselves and other seniors and strategies for coping with extreme heat. In order to increase the quality of content in terms of both academic interest and participant expertise and shared experiences, interviews were conducted in person by pairs of research team members, each including one research staff member and one peer researcher. This allowed conversations to be guided by not only the interview guide and research expertise, but also by the insight and experiences of our senior peer researchers. The interviews were digitally recorded, anonymized and transcribed word for word. Interviews lasted approximately 60 to 90 minutes, and were conducted at locations of the participants’ choosing.
Quantitative survey
The questionnaire for the second phase of this sequential design study was developed by the research team and community advisory group based on factors identified in the literature on seniors and heat waves, a measure of risk perception developed for emergency responses to threats of terrorism40 and key themes from the qualitative interviews. Topics covered by the survey included demographic information (using questions based on those in the Canadian census form), risk factors, access to resources, perceptions of risk, protective behaviours, use of resources and perceptions of gaps in resources for seniors. The initial questionnaire was drafted by the research team, then reviewed to enhance content validity by additional researchers with expertise in climate change and risk perception and community advisors with experience working with seniors. Our research team adapted the survey questions based on the feedback from these expert reviewers to develop the final questionnaire. The survey was distributed online via email, in person at community events and through community partner agencies, both in person and by mail.
Analyses
Qualitative interviews were digitally recorded and transcribed verbatim by a research assistant from the project team. A second research assistant reviewed a sample of transcripts in order to ensure accuracy. The team conducted an initial, inductive thematic analysis of the interviews, in which two research assistants reviewed each transcript and noted major relevant themes and categories (clusters of themes). These themes were then organized into a coding framework, which was further refined to develop a coding scheme through discussion with the project team (including the two peer researchers). Once a final coding scheme was agreed upon, all transcripts were coded by at least two research team members independently, applying the final coding scheme to all transcripts. The coded transcripts were entered into a database using NVivo qualitative analysis software, version 11 (QSR International Americas Inc., Burlington, MA, USA), which was used to generate summaries of the major themes from the interviews. The research team used these summaries to highlight key results, summarize responses to our central research questions and note other important trends in the interviews. We presented the final overarching categories and themes to the community advisory board to allow for their input and to collaboratively develop the presentation of the final results.
Quantitative survey responses were entered into a Microsoft Access form using forced responses to ensure accurate data entry. We then analyzed the quantitative data using R version 3.0 (R Core Team, Vienna, Austria). We computed means or frequencies for all study variables. We further analyzed survey responses for Pearson’s r or Spearman’s rho correlations between various individual-level variables such as demographic characteristics and risk awareness, and factors contributing to risk in seniors in our sample. We developed two risk indices to assess objective risk using the clusters of factors within the survey associated with specific types of risk. For example, health risk, representing the likelihood of negative health effects in extreme heat, included two factors: (a) the presence of health conditions that are negatively impacted by heat, and (b) having previously experienced heat exhaustion or other heat-related illness. Adaptability risk, representing the ability to cope during extreme heat, included knowledge and behaviour factors: (a) knowing the symptoms of heat exhaustion; (b) being aware of heat warnings; (c) using or accessing resources during heat waves; and (d) demographic factors such as income level, living alone, and housing— including ventilation and air conditioning.
Results
While the qualitative and quantitative components and initial analyses in this study were conducted sequentially, in our final analyses we considered results across datasets to triangulate a more complete picture of seniors’ risk and resilience. In this report, the results are discussed simultaneously by theme in order to triangulate them and for ease of understanding.
Sample
Recruitment for this study proved challenging, particularly for the qualitative component, as many seniors seemed to lack interest in talking about the subject of heat waves or climate change in general. Political orientation and beliefs about climate change also influenced people’s willingness to participate in this study. In total, fifteen participants completed qualitative interviews between August 2014 and September 2015, and 244 participants completed the survey questionnaire between April 2016 and September 2016.
Of our fifteen interview participants, five (33.3%) identified as male and ten (66.7%) identified as female. They ranged in age from 51 to 84 years, with a mean age of 71.7 (SD 9.6). Nine participants lived alone (60%), while the other six lived with a partner or with other family members (30%). Four participants were born outside of Canada (26.7%). Four participants (26.7%) also identified as visible minorities, with two participants identifying as East Asian, one as First Nations and one as Latino, and the rest identifying as Caucasian and/or Canadian (73.3%). Two participants (13.3%) identified as people living with disabilities.
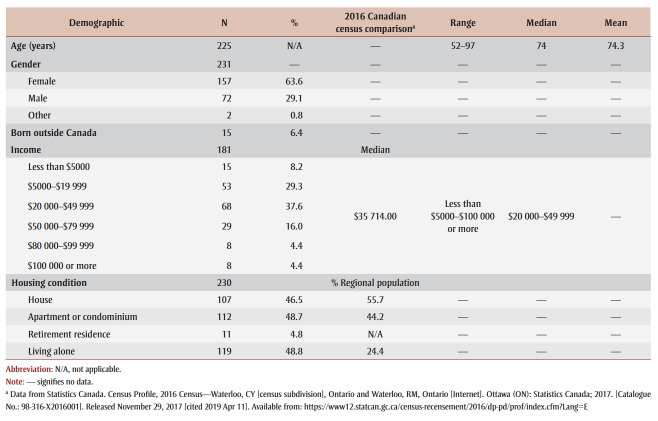
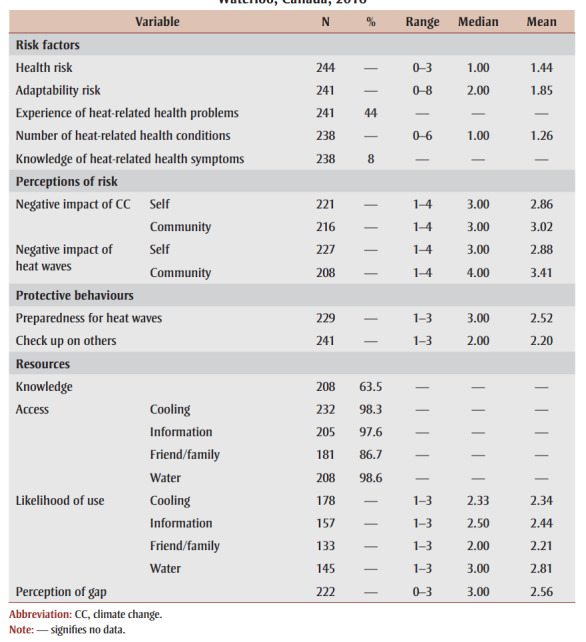
Survey participant demographics are summarized in Table 1, along with local comparison data from Canada’s 2016 Census. Participant demographics are summarized in Table 2.
Table 1. Demographic characteristics of respondents to survey on seniors’ awareness of heat wave risks, Waterloo, Canada, 2016, compared to local census data.
Table 2. Summary of results of survey on seniors’ awareness of heat wave risks, Waterloo, Canada, 2016.
 |
General awareness
Overall, participants reported being aware that weather was changing, and characterized the weather in Waterloo Region as unpredictable. Since we received mixed responses to climate change terminology in our introductory conversations and interviews, we chose to frame our conversations in the context of extreme weather and heat and to avoid broader climate questions unless participants raised the topic themselves. Many participants felt unqualified to make broader predictions about climate, choosing only to comment on immediate weather experiences and experiences from their past.
I have tracked this in my mind for the last 20 years because I grew up on the farm and I know our seasons. You had spring ... you had summer … you had fall. You had winter and spring. On the farm you are dependent on the weather for getting crops in and planting crops. I just know that the weather has changed a lot. (Ellen)
Among the survey participants, there was considerable variation in perceived negative influences of climate change. As participants’ perception of negative impacts of climate change increased, so did their perceived risk for people in Waterloo Region (r = .614, p < .001).
Risk profile
To better understand the process by which environmental stressors such as extreme heat result in negative psychological consequences, Michael Edelstein proposed the formulation of a risk personality.38 A risk personality describes the defining characteristics of the specific environmental stressor as it may be experienced by people living in a certain proximity to the stressor.38 This is important because the psychological impacts are caused by an interaction of the characteristics of the environmental stressor and the way individuals appraise that risk and cope with its impacts. This framework focusses on three key factors that contribute to how a person evaluates risk: cause, consequence and controllability. In this section, key themes and results that emerged from our analyses are presented within this framework.
Causes
In assessing risk, people assess the causal attributes of the environmental stressor, such as its origins, its temporal and geographical boundaries and its nature.36 In Waterloo Region, seniors considered not only heat waves in isolation, but also increased heat and other extreme weather as a component of global climate change more broadly.
When asked to reflect on their perceptions of how weather has or has not changed over time, many interview participants believed that weather patterns had changed, but were reluctant to draw conclusions about overall trends. They frequently described the weather as unpredictable, and often felt unqualified to make predictions for future weather.
We are definitely not getting the weather that we did get 10 even 15 years ago. The whole change of weather, the whole atmosphere has changed. I think it has. Like you are not getting the same good weather. It’s either good or it has completely gone the opposite direction. It is completely measurable. The smogginess. The sun, you don’t get as much sun anymore. It is dull and dreary. Maybe it is because I am getting older, I don’t know ... (Sanaa)
Participants had a mixed response to climate change terminology, with some supporting and having knowledge of global climate change and its causes, and others not believing there was a broader global pattern, or that changes to climate were natural long-term patterns.
It’s been more changeable than before I think ... yeah. I am very aware of climate change ... I even went on a march to Toronto a few weeks ago … (Leslie)
Experiences with extreme heat were mediated by personal factors such as age, health and resources. Some participants were very aware of heat waves and their effects on their own well-being, while others did not notice any effects or found increased heat easy to deal with.
Consequences
The second factor contributing to risk perceptions is the potential consequences of the environmental stressor.38 This includes the known impacts on the environment and the physical and psychological wellbeing of the people experiencing the stressor. Participants in this study had varied experiences with extreme heat and its consequences, as well as varied perceptions of the potential consequences of extreme heat and sense of personal preparedness to cope with extreme heat.
Interview participants who lived with health conditions such as heart disease or respiratory conditions often reported being aware of the effects of increased heat on their well-being, and took measures to cope and protect themselves during heat waves. Participants mentioned impacts on both their physical and mental well-being:
I am slower, I move slower. Sometimes just moving horribly slow. My knees hurt sometimes, you know? I do not, like, my body doesn’t like it, and I don’t like it. I don’t think well. There’s a distract ... It’s a distraction for me because my body doesn’t want it. It’s a huge distraction for me. (Philip)
… I don’t like heat waves, I can’t stand them. I am cranky and I can’t tolerate BS from people when it’s, it’s overheated. So I stay where I can get angry with ’em. I stay home ... (Sanaa)
Several interview participants reported specific instances when they became aware of previously unknown risks, often due to a personal experience of overheating, whether their own or that of a loved one:
And I said I could sleep in the family room, it’s no big deal. Well, my son came over to check up on me around 7 p.m., and I thought that I was warm—I felt warm, but I guess I looked worse than I felt. He said “That’s it, you’re coming to my house—pack your bag. This is ridiculous! I mean, look at you, your face is as red as that cup.” So anyway he packed me up and we went over to his place. It wasn’t until we got to his place did we realize how hot I really was. (Eleanor)
While some participants who had experiences with heat-related health consequences were aware of the impact of heat on their health, in general, participants’ awareness of the health consequences of heat and the symptoms of heat-related illness was relatively low. When asked to select the symptoms of heat exhaustion or heat stroke from a checklist, only 8.4% of our survey participants correctly identified all eight symptoms, and fewer than half of the participants (46.2%) correctly identified six out of eight symptoms.
Waterloo Region is typically cold and snowy in the winter, which often lasts almost six months. Thus, for residents of this area, heat is connected with summer and generally perceived as something positive. This was also true for the participants of this study. Some participants distinguished summer heat (which they liked) from the high humidity during heat waves that bothered them more:
No, again, I don’t do a whole lot of complaining about the weather, ’cause the only time I do a lot of complaining, like I said, is in the summer when it is humid like this and that really irritates me. (Maria)
Risk assessment
In this study, participants were asked about both their perceptions of their own vulnerability to extreme heat, and the objective factors that influenced their risk. In order to better understand the relationship between perceived and actual risk, we created two indices representing actual assessments of risk: health risk and adaptability risk. Health risk represented the influence of health conditions affected by heat and previous heat-related illness. Adaptability risk represented factors and resources that affect the likelihood of coping well with extreme heat, including knowledge of heat-related illness, awareness of heat alerts, access to emergency resources and support, having air conditioning or good ventilation at home, living alone, likelihood of using available resources, and income.
Overall, seniors showed some degree of accurate risk tracking as indicated by the link between our assessment of actual risk and their perception of their own risk. Those with higher actual health risk did perceive higher personal risk of negative impacts of extreme heat (r = .443, p < .001). Those with higher adaptability risk (i.e. less awareness and access to resources) also perceived a higher degree of personal risk of negative impacts of extreme heat (r = .184, p = .006).
While vulnerability to heat is often thought to be related to inaccurate perceptions of risk, within our sample, vulnerability to extreme heat appears more strongly related to social location and access to resources. Income was one key factor, as perceptions of higher risk of negative consequences of heat were correlated with lower income (r = −.198, p = .004), with the level of perceived risk decreasing as income increased. Type of housing was a contributor to perceived risk, with 61.9% of those at high risk living in apartments as opposed to houses (38.1%). In general, the fewer the resources participants felt were available to them, the higher their perceived risk of negative impacts of extreme heat (r = .288, p < .001).
Controllability
The perceived controllability of a stressor is a final important assessment that affects people’s risk perceptions and response. One way to control negative outcomes is to prepare for them in advance in order to mitigate or avoid negative impacts. We asked our survey participants to rate their general sense of preparedness for extreme heat, as well as their access to specific coping resources. Overall, 50% of participants felt they were well prepared to cope with extreme heat. In terms of specific resources to help cope with heat, 98.7% of participants expected to see some sort of warning in the news if there were an extreme heat event, 97.6% reported having access to information about the weather and coping strategies, 98.3% had access to at least one way of cooling themselves (e.g. air conditioning, fans), 98% had access to extra bottled water at home and 86.7% had friends or family members nearby whom they could ask for help.
Based on the broad availability of resources, seniors in our sample did not appear to be a group at particularly high overall risk. However, many of the same demographic factors that affected their actual risk and perceived personal risk of the negative impacts of extreme heat also predicted their perceptions of controllability and preparedness. Fifty percent of participants who felt they were not very well prepared (either completely unprepared or somewhat prepared) for extreme heat lived alone, with 62.5% of those who felt completely unprepared living alone, and 65.2% of those who felt “only somewhat prepared” living alone.
A total of 56.3% of those who lived alone felt unprepared or only somewhat prepared to cope with extreme heat, compared to 32.5% of those living with a partner, 38.9% of those living with family or 25% living with other older adults. This suggests that social connectedness may play an important role in preparedness and risk mitigation. Furthermore, while 86.7% of participants reported that they had friends or family members they could ask for assistance, only 50% of those who had support reported that they would be very likely to use it.
Some participants suggested that social stigma, perception of personal control and beliefs about individual responsibility may be factors influencing seniors’ willingness to ask for help. Many spoke of the need to take personal responsibility for their well-being:
… taking some responsibility … I can stay in if it is not urgent for me to stay out. I can just stay in with AC and do some other things like reading or some hobbies and stuff rather than complain because that is just going to make you hotter and affect your disposition so I am trying that way myself not to. (Florence)
… take responsibility. If it’s hot, don’t stand there in the sun and say “Oh my goodness, it is hot.” (Mark)
A common theme in the interviews was the need to simply accept and put up with difficult or uncomfortable conditions:
I mean in the wintertime if it’s misty and smoggy and crappy, well ok you don’t want to go outside, I understand that, but have some nice weather so you can go out and enjoy the cold here. Suck it up buttercup, you know? (Sophie)
Finally, another element that may make seniors reluctant to ask for help may be a fear of being perceived as vulnerable, which could lead to a loss of independence.
Resilience
Another survey finding was that many seniors took time to check in on friends, family and neighbours during extreme heat, with 43.2% being somewhat likely to check on others, 38.2% very likely, and only 18.7% not at all likely to do so (data not shown). This is noteworthy, given the low likelihood that participants in this sample would ask friends or family for help, as well as the finding that individual knowledge of the symptoms of heatstroke was low and that those who were less likely to ask a friend or family member for help were likely to be at higher adaptability risk (r = −.282, p = .001).
Building resilience
Participants in this study had many helpful suggestions for ways to increase awareness of the risks of extreme heat and for resources that could support or build resilience. Seniors reported that heat warnings did not always reach them, and that there was a lack of information about local resources, such as cooling centres. They identified doctors, pharmacists, community centres and local news as trusted sources of information that could be used to disseminate this information further. Participants also noted that the majority of seniors learned to rate temperatures using the Fahrenheit scale, and that weather reports using Celsius were not as accessible to them.
Discussion
Risk awareness is an important component of building resilience to extreme heat, particularly in vulnerable populations. In this study, we set out to assess risk awareness, risk perceptions and preparedness for extreme heat among seniors in Waterloo Region. Researchers around the world have called for investigations of seniors’ risk perceptions and coping practices during extreme heat; however, risk perceptions may not actually be the key to understanding seniors’ risk and resilience.2,10,14 We found that the seniors in our sample had a realistic overall assessment of their personal risks during heat waves. However, not all seniors in our sample were at equal risk, and not all seniors had equal or sufficient access to resources to protect themselves during extreme heat events. Seniors who perceived themselves to be at lower risk of negative consequences of extreme heat tended to have better health and access to more resources, while those who had concrete risk factors, such as pre-existing health conditions, lack of social support and lower income, tended to be aware of their elevated risks. Furthermore, stigma and social norms may have prevented some seniors who do have access to protective resources from making use of them.
The positive relationship between participants’ risk perceptions and actual risk for negative consequences of extreme heat was an important finding, given that problems of emergency preparedness and risk reduction are often framed as issues of awareness of risk.1,3,5,14,21,34,35 Our participants appeared to have accurate assessments of their own risks. However, there were significant differences in the demographic factors associated with the risks of extreme heat. Participants who were lower income, lived alone or had existing health conditions were at increased risk, and were relatively more aware of these risks, but their awareness did not necessarily lead to a reduction in their vulnerability.
Reducing vulnerability
Many risk mitigation initiatives focus on informing seniors of their risk and encouraging them to take personal actions to reduce it. This was reflected in participants’ comments about the personal responsibility to be aware of their wellbeing, to push through discomfort and to take action on their self-care. Knowledge and self-care are important components of risk mitigation, and our results show that participants could be better informed about the symptoms of heat-related illness and resources in their community to help them take care of their health. However, many participants in this study reported that they were unlikely to make use of community resources or ask for help during a heat wave, and some suggested that social stigma, perceptions of personal responsibility, and fear of being perceived as vulnerable may be barriers to seniors’ use of resources to stay healthy during heat waves. Risk factors such as social isolation, lack of social support and lack of access to cooling and other protective resources also played important roles in risk, and are more difficult for seniors to change for themselves.
Knowledge of risks and resources
Seniors in this sample had gaps in their knowledge of the symptoms of heat-related illnesses, and were open to receiving more information about the risks of heat and resources for coping. Having information that is directly relevant to seniors, particularly those with specific risk factors, disseminated through trusted sources such as community nurses, general practitioners and family doctors, local clinics, pharmacists and community centres could increase the accessibility, relevance and trustworthiness of heat-related resources to seniors. Finding out which local media outlets seniors favour, through community consultation and by ensuring that heat alerts and resources are disseminated through the best channels, could also increase the likelihood of important heatrelated information reaching seniors.
Communication
Using language that is relevant, accessible and engaging for seniors is critical for the uptake of information.22,34 Since many seniors in our sample learned the Imperial system before Canada switched to the metric system, communicating weather alerts in both Celsius and Fahrenheit degrees could help seniors recognize when the temperature puts them at risk. Avoiding technical, scientific language, referring to weather rather than climate and referencing the experience of humidity rather than heat are also recommended findings. Using strength-based language and avoiding language that may be disempowering or socially stigmatized is also important for supporting seniors’ independence and sense of agency.22,37 This could include avoiding the use of climate change terminology in broader alerts or preparedness resources, and avoiding terms that seniors may dislike or do not identify with, such as “vulnerable” or “elderly.” Community consultation and stakeholder engagement is a vital tool for learning best practices for communication with local seniors.
Access to resources
While many seniors in our study felt they had the resources they needed to stay well during a heat wave, those who were socially isolated or living on low incomes often felt unprepared. Broader social determinants of health such as livable incomes and social support are important to address over the long-term,41 but there are more immediate things that can be done to support seniors whose social location puts them at additional risk. Ensuring there are community resources such as cooling centres or other air-conditioned spaces available throughout the region, and that these sites are well-communicated and accessible by local transit could support seniors who do not have air conditioning or access to other spaces to stay cool. Water fountains or temporary water stations can also be helpful for anyone who cannot stay indoors during a heat wave, along with public washrooms, as many seniors mentioned avoiding drinking water out of fear they may not be able to access a washroom away from home.
Social networks
A lack of social connections and the stigma surrounding accessing support are important barriers to resilience that were identified by our participants. Many seniors did not have access to emergency resources, and others who did have access to additional support stated they were unlikely to ask for help. However, many seniors in our study and other research have reported supporting other seniors or people who may be at risk by sharing information and checking on them during heat waves.22 This peer support could be a helpful and empowering tool to leverage to increase seniors’ resilience to extreme heat. For instance, the San Jose Buddies Program42 and the Netherlands Red Cross43 local branches have established peer volunteer networks where seniors check on their peers, help with errands and provide assistance during heat waves and other emergencies. Implementing similar systems in Ontario could help improve social connections among seniors, increase knowledge among both low- and highresource seniors, and help de-stigmatize their access to social support. To support these goals, it is critical to effectively engage stakeholders and include local community-based organizations. It is also important to understand the relative strengths and weaknesses of social networks for seniors, and to establish volunteer- based programs.
Strengths and limitations
Recruitment was a challenge throughout this study, and while our community partners were extremely helpful in recruiting participants from their networks, this may have contributed to a skewed sample. One particular strength of this study was our partnerships with community organizations, which allowed us to recruit participants for both the interview and survey components who had experiences, risks and resources relevant to our research, including low-income seniors, seniors with disabilities, senior community leaders and newcomers. The majority of our participants were women, and while gender-based analyses have revealed important differences in the ways men and women cope with heat,44 our unbalanced sample did not allow for reasonable comparison. Our participants were predominantly white and Canadian-born, which, while representative of previous generations in Waterloo Region, does not represent the area’s current overall diverse cultural and linguistic groups. Our sample was also skewed in terms of income, with clusters at the high and low end of the income spectrum, which made it challenging to accurately assess the contribution of demographic factors to vulnerability across a broad spectrum of seniors’ experiences. People’s perspectives on climate change and controllability of risk also influenced their willingness to participate, with many of the seniors we spoke to declining to participate because they did not believe in climate change or were not worried because they had air conditioning. Finally, our sample was geographically limited to seniors in Waterloo Region. However, because the municipality includes three cities as well as a number of rural townships, it is representative of many other districts within the province. While this regional focus may limit the generalizability of our results, the data we collected were relevant and useful for local planners and community, social service and public health organizations, and may be particularly useful to other nearby communities. Consequently, we believe that most of our findings are transferable beyond this region.
Conclusion
Unlike previous studies indicating that the dangers posed to seniors by environmental stressors such as heat waves are heightened by seniors’ inaccurate perceptions of the risk to themselves and by their lack of response to risk, our study showed that Waterloo Region seniors’ assessments of their risks from heat waves were relatively realistic. Instead, both their actual risk and their resilience were impacted more by social location and coping resources. Even in those with higher incomes, greater social support and better housing, resilience tends to depend heavily on the availability of coping resources such as air conditioning and running water. During prolonged heat waves, those resources could temporarily become unavailable because of power outages or freshwater sources. Communication about community resources, such as cooling centres and emergency water access, could help seniors better prepare in the event of a prolonged extreme heat wave.
More generally, different communication strategies may be used for those who have access to appropriate resources and those who do not. This targeted approach would avoid the quick dismissal of the public health communication as irrelevant by those with resources, and the feeling that they are being blamed for their lack of resources by those without them. Realizing that seniors are capable and active partners in the response to heat waves will help prevent them from feeling like vulnerable individuals who have lost their ability to deal with such challenges. Peer-based approaches seem to be highly suitable for this purpose; peer support not only de-stigmatizes the act of asking for help, it is likely to increase the efficacy of information about risks by increasing openness on the part of seniors who attend to this information not only for themselves, but also to offer support to others.
Acknowledgements
This study was funded through an Insight Development Grant from the Social Sciences and Humanities Research Council.
This project would not have been possible without the help of our peer researchers, Chris Hodnett and Susan Gow, and without the support of our Community Advisory Group.
Conflicts of interest
The authors have no conflict of interest to report.
Authors’ contributions and statement
AE contributed to project design, participated in qualitative and quantitative data collection and analysis, and led the drafting and revision of the paper. BD contributed to project design, participated in quantitative data collection and qualitative and quantitative analysis, and contributed to the drafting and revision of the paper. BH contributed to recruitment strategy, qualitative data collection, qualitative and quantitative analysis, and to the drafting and revision of the paper. MR coled project conceptualization and design, co-supervised qualitative and quantitative data collection and analysis, and contributed to drafting and revision of the paper. AW co-led project conceptualization and design, co-supervised qualitative and quantitative data collection and analysis, and contributed to drafting and revision of the paper.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
References
- Akompab D, Bi P, Williams S, Grant J, Walker IA, Augoustinos M, et al. Heat waves and climate change: applying the health belief model to identify predictors of risk perception and adaptive behaviours in Adelaide, Australia. Int J Environ Res Public Health. 2013;10((6)):2164–84. doi: 10.3390/ijerph10062164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolitho A, Miller F, et al. Heat as emergency, heat as chronic stress: policy and institutional responses to vulnerability to extreme heat. Local Environ. 2017;22((6)):682–98. [Google Scholar]
- Lane K, Wheeler K, Charles-Guzman K, et al, et al. Extreme heat awareness and protective behaviors in New York City. J Urban Health. 2014;91((3)):403–14. doi: 10.1007/s11524-013-9850-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minister of Health. Ottawa(ON): 2011. Extreme heat events guidelines: technical guide for health care workers. [Google Scholar]
- Syal SS, Wilson RS, Crawford JM, Lutz J, et al. Climate change and human health – what influences the adoption of adaptation programming in the United States public health system. Mitig Adapt Strateg Glob Change. 2011;16((8)):911–24. [Google Scholar]
- Liss A, Wu R, Chui KK, Naumova EN, et al. Heat-related hospitalizations in older adults: an amplified effect of the first seasonal heatwave. Sci Rep. 2017 doi: 10.1038/srep39581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beniston M, et al. Future extreme events in European climate: an exploration of regional climate projections. Clim Change. 2007:71–95. [Google Scholar]
- Semenza JC, Rubin CH, Falter KH, et al, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335((2)):84–90. doi: 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- Robine J, Roy S, et al, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. crvi. 2008;331((2)):171–8. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- Zografos C, Anguelovski I, Grigorova M, et al. When exposure to climate change is not enough: exploring heatwave adaptive capacity of a multi-ethnic, low-income urban community in Australia. Urban Clim. 2016 [Google Scholar]
- Wolf J, Adger WN, Lorenzoni I, Abrahamson V, Raine R, et al. Social capital, individual responses to heat waves and climate change adaptation: an empirical study of two UK cities. Glob Environ Change. 2010:44–52. [Google Scholar]
- Loughnan M, Nicholls N, Tapper NJ, et al. Mapping heat health risks in urban areas. Int J Popul Res. :518687–52. [Google Scholar]
- Wilhelmi OV, Hayden MH, et al. Connecting people and place: a new framework for reducing urban vulnerability to extreme heat. Environ Res Lett. 2010;5((1)):14021–52. [Google Scholar]
- Bittner MI, el U, et al. Perceptions of heatwave risks to health: results of a qualitative interview study with older people and their carers in Freiburg, Germany. Psychosoc Med. 2012 doi: 10.3205/psm000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- re E, Payette H, Gaudreau P, Morais JA, Shatenstein B, reux M, et al. Risk and protective factors for heat-related events among older adults of Southern Quebec (Canada) Can J Public Health. 2016;107((3)):e258–e265. doi: 10.17269/CJPH.107.5599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. Ottawa(ON): Estimates of population, by age group and sex for July 1, Canada, provinces and territories, annual (Table 17-10-0005-01) [Internet] Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501. [Google Scholar]
- Bi P, Williams S, Loughnan M, et al, et al. The effects of extreme heat on human mortality and morbidity in Australia: implications for public health. Asia Pac J Public Health. 2011;23((2 Suppl)) doi: 10.1177/1010539510391644. [DOI] [PubMed] [Google Scholar]
- Milan BF, Creutzig F, et al. Reducing urban heat wave risk in the 21st century. Curr Opin Environ Sustain. 2015:221–31. [Google Scholar]
- Hine DW, Phillips WJ, Cooksey RW, Watt SE, et al. Preaching to different choirs: how to motivate dismissive, uncommitted and alarmed audiences to adapt to climate change. Glob Environ Change. 2016:1–11. [Google Scholar]
- Pfaff R, et al. Disarming the “silent killer”: reducing the vulnerability of Toronto’s elderly to extreme heat [master’s thesis] [Lund (Sweden)]: Lund University; 2016. 2016 Available from: http://lup.lub.lu.se/luur/download?func=downloadFile&recordOId=8879088&fileOId=8879090. [Google Scholar]
- Semenza JC, Hall DE, Wilson DJ, Bontempo BD, Sailor DJ, George LA, et al. Public perception of climate change: voluntary mitigation and barriers to behavior change. Am J Prev Med. 2008:479–87. doi: 10.1016/j.amepre.2008.08.020. [DOI] [PubMed] [Google Scholar]
- Abrahamson V, Wolf J, Lorenzoni I, et al, et al. Perceptions of heatwave risks to health: interview-based study of older people in London and Norwich, UK. Perceptions of heatwave risks to health: interview-based study of older people in London and Norwich, UK. J Public Health (Oxf) 2009;31((1)):119–26. doi: 10.1093/pubmed/fdn102. [DOI] [PubMed] [Google Scholar]
- Akompab DA, et al. Population health and climate change: public perceptions, attitudes and adaptation to heat waves in Adelaide, Australia [online doctoral dissertation] Akompab DA. 2013 Available from: https://digital.library.adelaide.edu.au/dspace/bitstream/2440/99892/2/02whole.pdf. [Google Scholar]
- Bickerstaff K, et al. Risk perception research: socio-cultural perspectives on the public experience of air pollution. Environ Int. 2004;30((6)):827–40. doi: 10.1016/j.envint.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Itkonen JV, et al. Social ties and concern for global warming. Clim Change. 2015;132((2)):173–92. [Google Scholar]
- Takahashi B, Burnham M, Hartman C, Sopchak AR, Selfa T, et al. Climate change perceptions of NY state farmers: the role of risk perceptions and adaptive capacity. Environ Manag. :58(6):946–57. doi: 10.1007/s00267-016-0742-y. [DOI] [PubMed] [Google Scholar]
- Smoyer KE, et al. Putting risk in its place: methodological considerations for investigating extreme event health risk. Soc Sci Med. 1998;47((11)):1809–24. doi: 10.1016/s0277-9536(98)00237-8. [DOI] [PubMed] [Google Scholar]
- Carlton JS, Mase AS, Knutson CL, et al, et al. The effects of extreme drought on climate change beliefs, risk perceptions, and adaptation attitudes. Clim Change. 2016;135((2)):211–26. [Google Scholar]
- Chauvin B, Hermand D, Mullet E, et al. Risk perception and personality facets. Risk Anal. 2007;27((1)):171–85. doi: 10.1111/j.1539-6924.2006.00867.x. [DOI] [PubMed] [Google Scholar]
- Gifford R, et al. The dragons of inaction: psychological barriers that limit climate change mitigation and adaptation. Am Psychol. 2011;66((4)):290–302. doi: 10.1037/a0023566. [DOI] [PubMed] [Google Scholar]
- McCright AM, Dunlap RE, Pyatt ST, et al. Political ideology and views about climate change in the European Union. Environ Politics. 2016;25((2)):338–58. [Google Scholar]
- Hidalgo MC, Pisano I, et al. Determinants of risk perception and willingness to tackle climate change. PsyEcology. 2010;1((1)):105–12. [Google Scholar]
- Douglas M, Wildavsky AB, et al. University of California Press. Berkeley(CA): 1982. Risk and culture: an essay on the selection of technical and environmental dangers. [Google Scholar]
- Brody SD, Zahran S, Vedlitz A, Grover H, et al. Examining the relationship between physical vulnerability and public perceptions of global climate change in the United States. Environ Behav. 2008;40((1)):72–95. [Google Scholar]
- Sheridan SC, et al. A survey of public perception and response to heat warnings across four North American cities: an evaluation of municipal effectiveness. Int J Biometeorol. 2007;52((1)):3–15. doi: 10.1007/s00484-006-0052-9. [DOI] [PubMed] [Google Scholar]
- Sara LM, Jameson S, Pfeffer K, Baud I, et al. Risk perception: the social construction of spatial knowledge about climate change-related scenarios in Lima. Habitat Int. 2016;54((2)):136–49. [Google Scholar]
- Vaughan E, et al. Contemporary perspectives on risk perceptions, health-protective behaviors, and control of emerging infectious diseases. Int J Behav Med. 2011;18((2)):83–7. doi: 10.1007/s12529-011-9160-y. [DOI] [PubMed] [Google Scholar]
- Edelstein M, nd ed, et al. Westview Press. Boulder(CO): 2004. Contaminated communities: coping with residential toxic exposure. [Google Scholar]
- Becker JS, Paton D, Johnston DM, Ronan KR, et al. A model of household preparedness for earthquakes: how individuals make meaning of earthquake information and how this influences preparedness. Nat Hazard. 2012:107–37. [Google Scholar]
- Gibson S, Lemyre L, Lee JE, et al. Predicting emergency response intentions among the Canadian public in the context of terrorism threats: examining sociodemographics and the mediating role of risk perception. Hum Ecol Risk Assess. 2015;21((1)):205–26. [Google Scholar]
- Mikkonen J, Raphael D, et al. York University School of Health Policy and Management. Toronto(ON): 2006. Social determinants of health: the Canadian facts. Available from: http://www.thecanadianfacts.org/ [Google Scholar]
- ‘Buddy system’ for heat waves [Internet] City of San Jose. Available from: http://www.midtownresidents.org/pan/ep/info/heatwave.doc. [Google Scholar]
- International Federation of Red Cross and Red Crescent Societies. Geneva(CH): Netherlands Red Cross innovation program for heat waves [Internet] Available from: http://www.climatecentre.org/downloads/File/articles/Netherlands%20heat%20wave%20campaign.pdf. [Google Scholar]
- Steen Y, Ntarladima A, Grobbee R, Karssenberg D, Vaartjes I, et al. Sex differences in mortality after heat waves: are elderly women at higher risk. Int Arch Occup Environ Health. 2019;92((1)):37–48. doi: 10.1007/s00420-018-1360-1. [DOI] [PubMed] [Google Scholar]