Highlights
-
•
The COVID-19 outbreak has led to an unprecedented crisis in Spain
-
•
This paper examines the spread of COVID-19 and the policies and technologies used
-
•
A stringent confinement, paired with substantial reduction in mobility showed positive epidemiological results
Keywords: COVID-19, Spain, Policy and technology
Abstract
Background
The COVID-19 outbreak has led to an unprecedented crisis in Spain. After Italy, the spread of the virus was quick, and Spain became the second epicenter in Europe by number of cases and deceased. To tackle the outbreak and contain the spread, the Spanish authorities undertook exceptional measures based on a generalized lockdown by which the majority of the economic activity ceased for several weeks.
Objectives
The goal of this paper is to examine the spread of COVID-19 in Spain from February to May 2020, as well as the public policies and technologies used to contain the evolution of the pandemic. In particular it aims to assess the effectivity of the policies applied within the different autonomous communities. Cases are presented until August as well as the main changes in containment and mitigation measures.
Methods
Data was collected from various official sources, including government reports, press releases and datasets provided by national and international level institutions.
Results
We show that the main measure to contain the spread of the pandemic was a stringent confinement policy enforced through fines. It resulted in a substantial reduction in the mobility and the economic activity. At a regional level, the negative consequences of the crisis affected differently across regions.
Introduction
The COVID-19 outbreak has led to an unprecedented crisis in Spain. After Italy, the spread of the virus was quick, and Spain became the second epicenter in Europe by number of cases and deceased. Although the first case diagnosed with COVID-19 was registered at the end of January, the Spanish health authorities did not undertake measures until one month later, moment when a systematic and exponential increase in registered cases and deceases was observed. To tackle the outbreak and contain the spread, the management of public health policies were centralized within the Ministry of Health and the authorities undertook exceptional measures based on a generalized lockdown by which the majority of the economic activity ceased for several weeks.
In this paper we describe and analyze the spread of COVID-19 in Spain and the policies and technologies used through the course of the unfolding of the pandemic. Our focus consists of assessing the patterns within regional departments, Autonomous Communities (AC), to understand how the pandemic evolved across different parts of the country. This question is particularly relevant for the Spanish case given the highly decentralized nature of the health system where AC manage most public health policies and are provided with different health resources. These different resource allocations across AC prior to the crisis could have been key determinants to understand the spread and impact of the virus throughout different parts of the country.
We exploit official sources of epidemiological information a to assess the trends across AC. In particular, we study several indicators that include: registered cases, recovered, deceased, hospitalizations, ICU cases by age and gender and comorbidity patterns. Further, we pay special attention to the outcomes of the different policies and technologies. In particular, we evaluate the effectiveness of lockdown measures by comparing the evolution of a stringency index during the different stages of the pandemic and mobility.
The rest of the paper is structured as follows. Section 2 provides an overview of Spain and its health care system. Section 3 describes the main epidemiological trends. Section 4 presents the series of policies put in place. Section 5 outlines the health system response. Section 6 shows some economic and financial spillovers of the virus. Section 7 concludes. At the end of the document the references can be found.
Country description
In 2019, Spain's population was 47 million people, distributed among the 17 AC that further divide into provinces.
The health system is organized via a national health system typology, Sistema Nacional de Salud (in Spanish), and provides universal healthcare through 13,122 primary care facilities of General Practitioners (GP), and 466 hospitals [1]. AC are the main managers of the health system coordinating the provider networks and purchasing resources. Further, the Ministry of Health, dependent on central government, mainly acts in stewardship and coordination with the AC through the Interterritorial Council of the National Health Service.
Table 1 contains an overview of the demographics and health system characteristics of Spain, which we use as aid in contextualizing the epidemiological trends of COVID-19 and changes in health resources.
Table 1.
Country and Health system overview.
| Spain | OECD | |
|---|---|---|
| Total population*,’ | 47,026,208 | 1,301,969,697 |
| Population density+ | 92.9 | |
| Life expectancy | 83.4 | 80.7 |
| Old age dependency ratio | 0.293 | 0.264 |
| Share of the population >65 years old | 19.29 | 17.204 |
| People living with two of more chronic conditions | ||
| 15–64 | 21.3 | 24.1 |
| 65+ | 62.3 | 58.1 |
| Total | 30.0 | 31.3 |
| Diabetes I and II prevalence | 7.2 | 6.4 |
| Health care expenditure as% of GDP | 8.9 | 8.8 |
| Health care expenditure per capita ($) | 3,428 | 3,994 |
| Practicing doctors per 1,000 pop | 4.0 | 3.5 |
| Share of different categories of doctors (GP, other general, Specialists, other docs) | ||
| GP | 19.6 | 23.4 |
| Other general | 7.8 | |
| Specialists | 65.3 | 64.6 |
| Other docs | 15.1 | 4.3 |
| Practicing nurses per 1,000 pop | 5.7 | 8.8 |
| Beds per population | 3.0 | 4.7 |
| Beds in residential long-term care facilities (per 1,000 population above 65)# | 44.1 | 43.1 |
Spain's life expectancy (83.4) is the highest amongst the European countries and it is well above the average of OECD nations (80.7). As an ageing country, the share of population over 65 exceeds other OECD countries (19.3 vs 17.2) as well as the old age dependency ratio1 (0.293 vs 0.264). Alongside this longevity, Spain presents a significant rate of morbidity having a 62.3% of older than 65 with two or more chronic conditions and a 7.2% of diabetes prevalence (also higher than the 6.4 average in OECD countries).
In a universal system, free at the point of use,2 the funding of the health system plays a key role. As a result of the 2008 financial crisis, over the period 2008–17 the health budget shrank [2]. These reductions resulted in decreases from 73.9% to 70.8% of the average participation in funding of the portion related to government compulsory schemes. At the same time, private expenditure on health, especially out of pocket spending rose, reaching 23.6% currently. The existing proportion of health expenditure as a fraction of the GDP (8.9%) is around OECD numbers (8.8%), and higher than in 2008 (8.3%), while per capita healthcare expenditure of 3,428 USD (PPP) in 2018, was below the OECD average of 3,994.
In terms of health and long-term care resources such as doctors, nurses and beds per 1,000 population, Spain falls above OECD levels – especially regarding nurses and hospital beds. Concerning long term care resources, despite not ranking among the top countries, Spain has more beds in long term care residences than Italy (18.6), and falls slightly above OECD average (43.1).
Table 2 shows the differences in health resources across the AC. Andalucía is the biggest AC by population whilst the autonomous city of Melilla presents the highest population density. Other big AC by population are Madrid and Cataluña. Cataluña, is also on top regarding number of hospitals and beds but not in the number ICU beds, key to treat COVID-19 severe patients, or primary care facilities important for tracking early cases.
Table 2.
Sociodemographic and health system resources per AC, number per 100.000 population.
| Autonomous Communities (AC) | Population | Density (population/km2) | Hospitals | Beds | ICU beds | Primary care facilities | Intensive care doctors | Primary Care doctors | Nurses | Elderly care facilities | Elderly care placements |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Andalucia | 8,414,240 | 96.1 | 0.6 | 169.4 | 8.7 | 18.0 | 4.5 | 94.1 | 538.0 | 8.0 | 445.6 |
| Aragon | 1,319,291 | 27.6 | 1.6 | 320.9 | 12.6 | 74.6 | 7.5 | 122.5 | 675.4 | 21.1 | 1,396.5 |
| Asturias | 1,022,800 | 96.5 | 1.2 | 294.3 | 9.1 | 20.9 | 6.0 | 105.7 | 718.6 | 18.5 | 1,203.9 |
| Baleares | 1,149,460 | 230.3 | 1.0 | 197.3 | 10.8 | 14.1 | 5.6 | 73.1 | 553.8 | 5.3 | 444.6 |
| Canarias | 2,153,389 | 289.2 | 0.7 | 208.1 | 11.0 | 12.1 | 5.1 | 96.3 | 647.1 | 4.6 | 309.6 |
| Cantabria | 581,078 | 109.2 | 0.9 | 238.2 | 6.9 | 28.6 | 3.1 | 95.9 | 813.1 | 6.0 | 431.3 |
| Castilla La Mancha | 2,032,863 | 25.5 | 0.8 | 316.2 | 8.3 | 64.5 | 5.2 | 85.0 | 581.7 | 23.3 | 871.0 |
| Castilla Leon | 2,399,548 | 25.6 | 0.8 | 187.0 | 8.3 | 163.1 | 4.4 | 132.1 | 739.8 | 28.7 | 1,768.9 |
| Cataluña | 7,675,217 | 239.0 | 2.0 | 329.2 | 8.5 | 16.3 | 5.5 | 89.6 | 713.5 | 13.1 | 807.5 |
| Ceuta | 84,777 | 4,238.9 | 2.4 | 401.1 | 14.2 | 8.3 | 13.0 | 121.5 | 690.0 | 3.5 | 257.1 |
| C. Valenciana | 5,003,769 | 215.2 | 0.8 | 199.4 | 11.0 | 17.0 | 4.1 | 78.3 | 568.8 | 6.6 | 189.4 |
| Extremadura | 1,067,710 | 25.6 | 1.1 | 308.6 | 9.6 | 49.3 | 4.7 | 132.4 | 750.0 | 24.8 | 977.9 |
| Galicia | 2,699,499 | 91.3 | 0.7 | 281.5 | 9.7 | 17.3 | 3.7 | 85.2 | 537.7 | 11.9 | 667.5 |
| Madrid | 6,663,394 | 830.0 | 0.6 | 192.6 | 12.0 | 6.4 | 3.9 | 77.4 | 791.2 | 6.4 | 731.9 |
| Melilla* | 86,487 | 7,207.3 | – | – | 8.1 | – | – | – | 681.0 | 2.3 | 313.3 |
| Murcia | 1,493,898 | 132.0 | 1.1 | 226.7 | 8.2 | 17.7 | 5.9 | 85.7 | 442.1 | 3.9 | 347.5 |
| Navarra | 654,214 | 63.0 | 0.9 | 221.5 | 9.9 | 44.2 | 5.8 | 82.2 | 1,036.1 | 11.9 | 939.9 |
| Pais Vasco | 2,207,776 | 305.2 | 1.1 | 269.5 | 8.1 | 14.5 | 4.1 | 97.5 | 751.6 | 16.9 | 573.7 |
| La Rioja | 316,798 | 62.8 | 1.9 | 303.3 | 9.2 | 61.2 | 3.2 | 99.1 | 635.1 | 10.1 | 1,012.9 |
The COVID-19 outbreak has modified the existing decentralized organization of health system. Since the declaration of the State of Alarm (14th of March), the main tasks and policies to tackle the crisis were temporarily centralized around the Ministry of Health. These included centralized purchase of necessary goods and services in order to meet three main purposes (according to the Ministry): reinforcement of the AC purchasing processes, allocation of resources among the population and professionals and organization of the production at national and international level. Only once the outbreak was under control, its effects and the State of Alarm concluded (21st of June). This implied that the AC, at different speeds regained their competences in health.
COVID-19 trends
Overview of data availability and data transparency
The Ministry of Health is the authority that sets and manages the protocol for reporting information related to COVID-19. Using a notification form, the AC report to two bodies under the Ministry of Health: The National Center of Epidemiology (Centro Nacional de Epidemiologia, CNE) and the Center for Coordination of Alerts and Sanitary Emergencies (Centro de Coordinación de Alertas y Emergencias Sanitarias, CCAE).
Another key institution, in charge of the management and release of the epidemiological information is the Charles III Institute of Health (Instituto de Salud Carlos III, ISCIII). The ISCIII, gathers the information through the National Network of Epidemiological Surveillance (RENAVE). The ISCIII is the official source of information and we will use it in the paper.
Until May, the ISCIII released daily information at regional level regarding confirmed cases (through different testing methods), hospitalizations as well as referrals to Intensive Care Units (ICU), deceased and recovered cases. Since then, and currently, daily data only on daily cases is being released, and is available to download in an interactive website [3]. Further the ISCIII elaborates reports with relevant breakdowns of the information (i.e. demographic, clinical and epidemiological risk history characteristics).
Two main caveats in the data must be mentioned. First, in the initial stages of the pandemic, there was misalignment in the criteria applied by ACs to classify new and hospitalized cases. Since the 15th of April, a unified criterion was implemented to account for the number of confirmed cases. These criteria included positive cases under different testing methods (e.g. PCR and Antibodies tests) [4]. Second, data since the 20th of May is under review, and since then the same information as before hasn't been released. For this reason, we use information until May to capture the complete range of epidemiological indicators, while we update the data until August, capturing daily cases (the currently available information).
There are other types of information available that are relevant for the purposes of this paper. In particular, information on existing health resources, reported by the Ministry of Health and information on new measures to mitigate the contagion.
COVID-19 numbers in Spain
Cases, deceased and recovered
The first confirmed case of COVID-19 in Spain was reported on the 31st of January. It was an imported case corresponding to a German tourist visiting the island of La Gomera (Canarias). After a month the number of confirmed cases increased to 100.
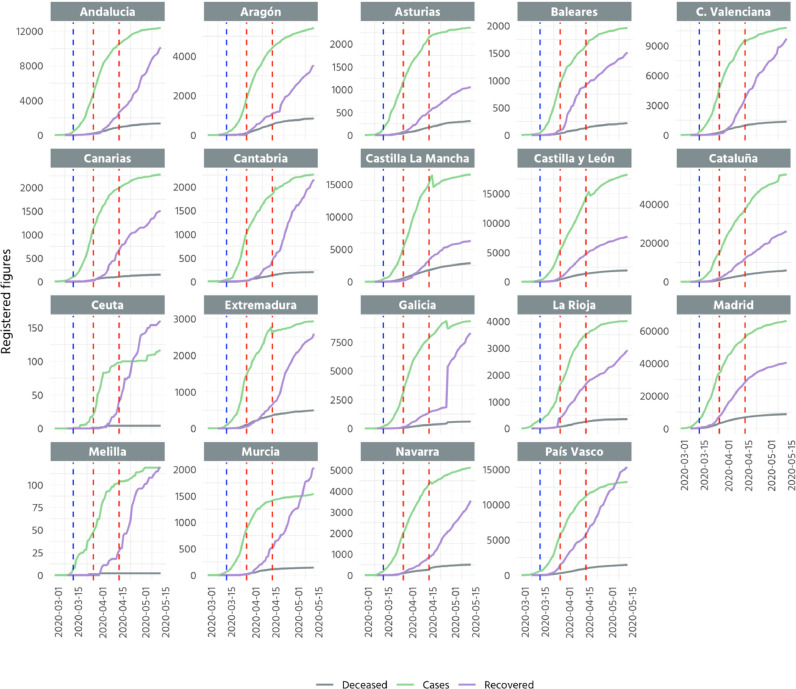
Fig. 1 presents the trends of registered cases, recovered and deceased amongst the different AC. After reaching 100 cases, all AC experienced an exponential growth. The top AC with higher cumulative figures were Madrid and Cataluña registering a more than 100,000 cases together. Further, in mid-April the majority of AC commenced to flatten the curved of registered cases. Yet, some regions such as Murcia or Ceuta flattened the curve faster than other regions such as Cataluña, Castilla-Leon or Castilla-La-Mancha. Finally, there are some ACs where the number of recovered exceeds the number of cases. This group of regions includes Ceuta, Murcia and Pais Vasco.
Fig. 1.
Cumulative cases, deceased and recovered (regions)
Note: Blue (first) dotted line indicates 15–03 (start of lockdown), red (second and third, respectively) dotted lines indicate 01–04 (close of non-essential activities) and 15–04 (lifting of restriction of non-essential activities). The data compiled correspond to the cumulative cases up to 15th of May.6 Deaths are recorded as a person that has tested positive to COVID-19 and has passed away. Cases correspond to those with positive PCR tests. Confirmed cases do not come from the sum of hospitalized, recovered and deceased, as they are not mutually exclusive. Deceased and recovered could have been hospitalized and therefore be in the two groups. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
[3].
Seroprevalence study [5] detected initially that around 5% of the Spanish population had antibodies, with a variability among regions and provinces ranging from 0.4% to 14%. This would mean that around 2.3 million individuals got the virus, while official numbers (subject to underestimations due to testing criteria and the nature of the illness where people can be asymptomatic, among others) are around 350,000 (August).
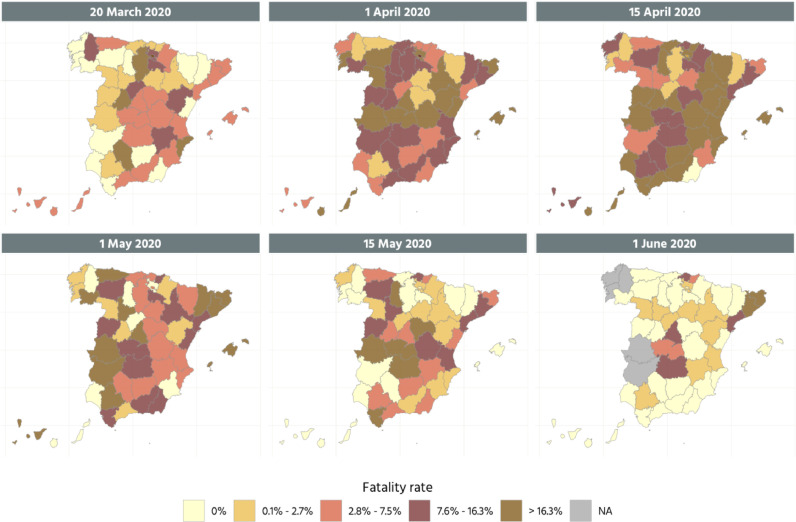
Fatality rates
Fig. 2 presents several snapshots of the fatality rates during the outbreak at province level. These data are released independently by different regional governments and collected by Montera24.3 The data used for the calculation of fatality rates are also affected by the change in the methodology mentioned above so are updated to the last record available before the change in the methodology. During the first half of April fatality rates reached their peak affecting several provinces located in the east of the country. A month after the worse parts belonged to provinces from AC of Cataluña, Extremadura, Asturias, Castilla-Leon and Madrid. Indeed, deaths in the peak of the pandemic have been proved to be significantly above (around twice) the reported by the Ministry of Health compared to deaths registered in the Daily Mortality Monitoring System [6] and those informed by the National Institute of Statistics [7], compared to the same dates in the previous year.
Fig. 2.
Fatality rates over time (provinces)
Note: Fatality rates are represented by quintiles and calculated as the proportion of deceases among registered cases. Figures are not cumulative and refer to each date in the panels instead. A zero fatality rate on that day means no deaths were recorded. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
[39].
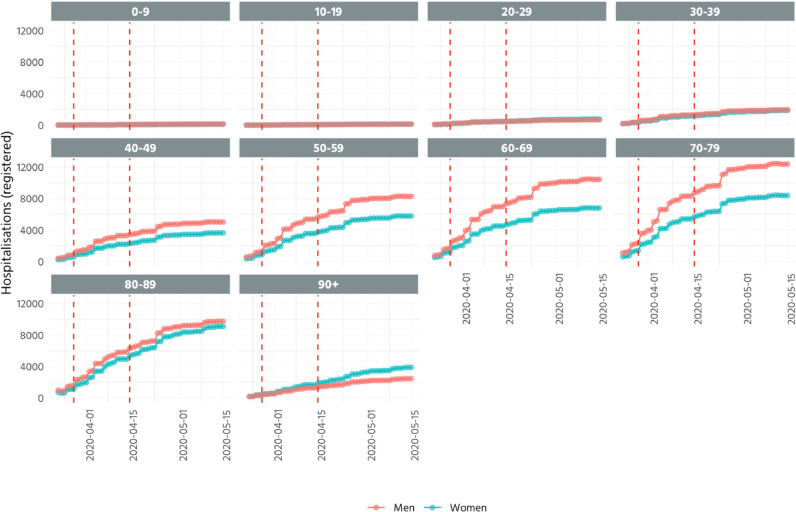
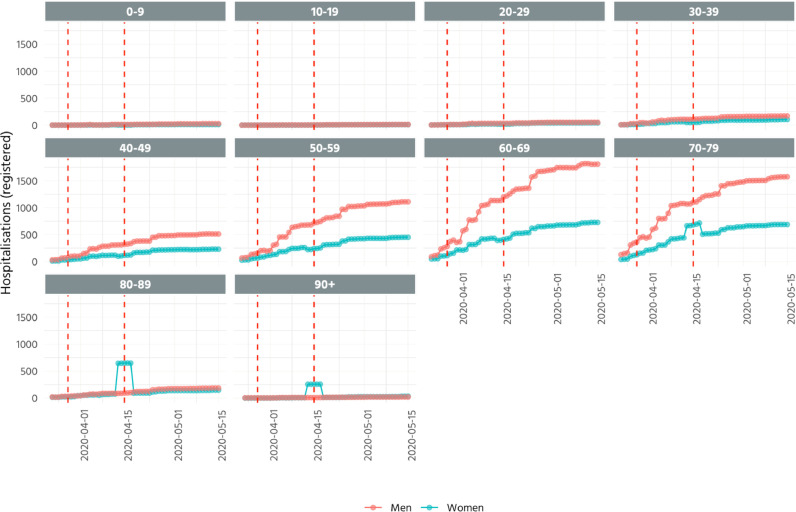
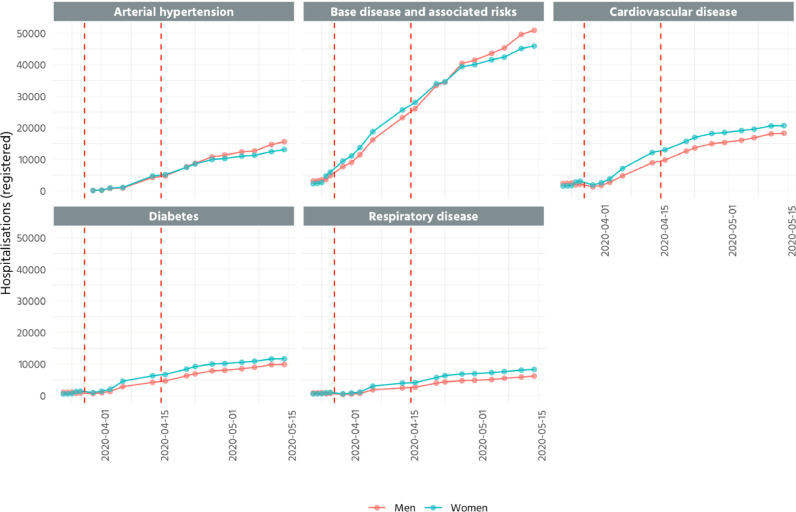
Hospitalisations and ICU referrals
The cases of hospitalisations and referrals to ICU have spread differently between different age ranges. As shown by Figs. 3 and 4 , the most affected groups have been individuals older than 60 years old which have been classified as risky population. In addition, especially in patients within the former age range, there has been a significant gender gap in hospitalisations where men have shown higher number of hospitalisations and ICU referrals. Interestingly the trends remain in parallel between genders for individuals younger than 40 years old.
Fig. 3.
Hospitalisations by age groups and gender (cumulative)
Note: Red dotted lines indicate 01–04 (close of non-essential activities) and 15–04 (lifting of restriction of non-essential activities).
[40].
Fig. 4.
ICU referrals by age groups and gender (cumulative)
Note: Red dotted lines indicate 01–04 (close of non-essential activities) and 15–04 (lifting of restriction of non-essential activities).
[40].
The epidemiologic information concerning diseases that may be related to COVID-19 is presented at aggregate level without differentiation between AC in Fig. 5 . Despite registering a lower number of hospitalisations, women registered a higher of daily cases than men in several diseases that included cardiovascular, diabetes and respiratory. Yet, trends across genders are fairly similar. Amongst all diseases, the base disease and associated risk is the comorbidity that presents more registered cases.
Fig. 5.
Hospitalisations by type of disease (cumulative)
Note: Red dotted lines indicate 01–04 (close of non-essential activities) and 15–04 (lifting of restriction of non-essential activities).
[40].
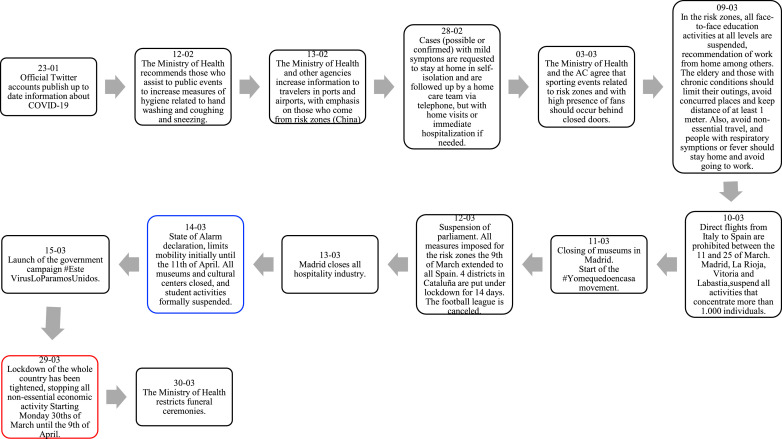
Policy road map
To address the spread of the virus, typically countries will put in place measures to contain and mitigate the spread and also, to address the consequences of those policies on the economy. As the first wave of the pandemic has passed, it is necessary to cover two parts of the policies, their phase in, and their phase out.
Mitigation and containing policies
Phase in of restrictions
After WHO's notification of the existence of COVID-19, Spain was quick to follow the advised instructions of the international organism in terms of epidemiological protocols and spread of information to the public. Press releases showed a confident approach by the authorities but also, a non-alarming one. An example is a press note from the 23rd of January arguing for reduced risk as Spain had no close links to the epicenter in China (Wuhan had no directs flights to from Spain, or China not being a frequented vacation destination).
Fig. 6 describes the full timeline of policies implemented to contain the spread of the virus. Until the middle of February, only minor measures where implemented, and at the end of the month, the government opted to inform those with symptoms to stay home (28–02). Some regional restriction where put in place after. Since then, activities, gathering, sporting events started their suspension. The 9th of March, schools and universities were closed when community outbreak was declared, following the 10th of March, a flight ban to Italy was imposed.
Fig. 6.
Policy interventions in February and March to contain the spread of the virus until phase-out of restrictions
Note: in blue the start of lockdown, in red the closure of nonessential activities, and in green the end of lockdown. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
[12] on the dates of press notes.
It was only on the 14th of March, when 7,658 cases had been recorded and 285 reported deaths, Spain declared the State of Alarm, limiting all people movement, with exception of grocery shopping, pharmacy and others. This came nearly a week after Italy imposed a nationwide lockdown (the 9th of March), but at a comparable number of cases (7,985), and around 3 times less deaths (724). Despite this, cases continued an upward trend, and tightening of the lockdown was issued on the 29th of March, where all non-essential activities where stopped.
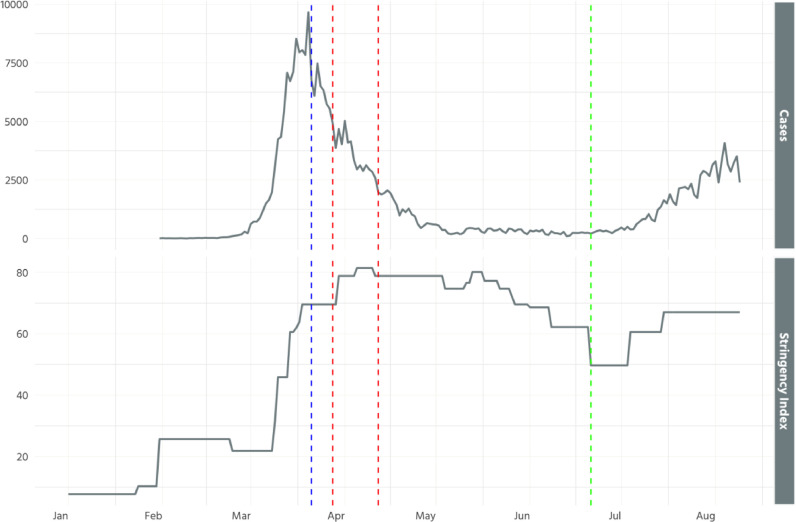
To assess the efficacy of the measures, Fig. 7 shows the containment measure stringency index [8], which captures eight policy indicators on containment and closure policies (e.g. school closures and restrictions in movement) compared to the daily new cases (until August). It is observed how the measures started to grow in terms of containment while the pandemic was unraveling and stayed at its maximum from the start of April. In consequence, cases declined, and have remained low for May and June. It has become evident that after the Spanish bumpy start, the restrictive measures that moved fast into extreme draconian ones paid the dividends.
Fig. 7.
Stringency index and daily cases (rolling 7-day average).
Note: Stringency Index represents a measure of containment. Blue (first) dotted line indicates start of lockdown (15th March), red (second and third) dotted lines indicate the closure of non-essential activities (1st-14th April). Green (fourth) dotted line represents the official end of lockdown (21st June). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Several determinants can be related to the success of the measures, aside the broadness of the containment measures. Two other key ones relate to the enforcement of the measure and their outcomes (e.g. mobility).
Regarding the first, the State of Alarm allowed punishable measures to be imposed, with fines ranging between €601 and up to €10,400. The Ministry of Internal Affairs (25th of April) informed that 741,407 fines had been issued since [9]. Moreover, as in other countries, drones have been operated by police forces to monitor the measures imposed (e.g. lockdown) and to inform individuals out in public about hygiene measures.
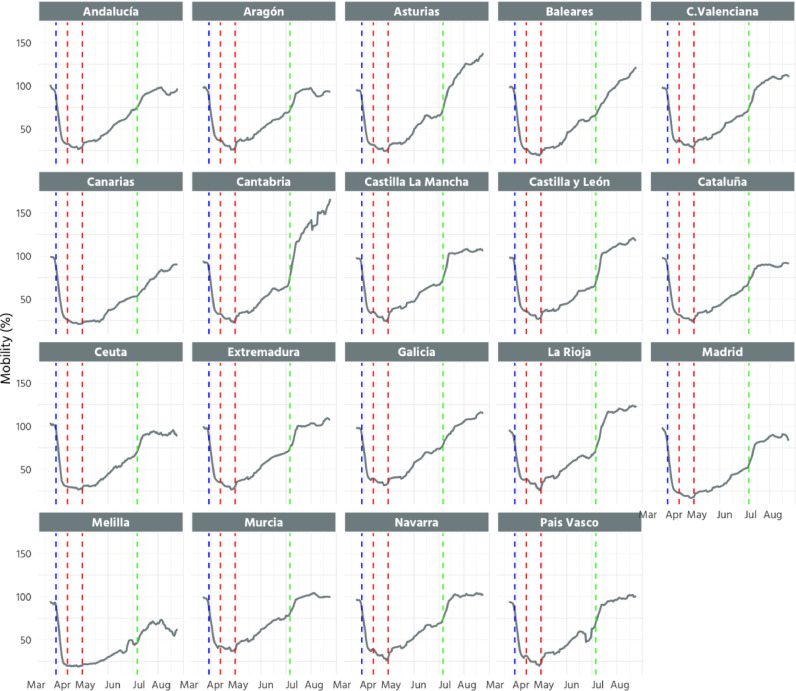
This further reflects on the mobility of the Spanish population. Fig. 8 plots the percentage of mobility of the population per AC respect to the reference period 14–20 February. It can be observed how mobility was significantly reduced during the first week of the State of Alarm, and was kept low during the lockdown period.
Fig. 8.
Mobility per AC
Note: Rolling 7-day average of the mobility in each AC. The percentage of mobility corresponds to that with respect to the reference period 14–20 February. Blue (first) dotted line indicates start of lockdown (15-03), red (second and third) dotted lines indicate the closure of non-essential activities (1st-14th April). Green (fourth) dotted line represents the official end of lockdown (21-06). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
[41].
Regional effects of the lockdown have been highlighted in Amuedo-Dorantes and co-authors [10], which show that regions that where at early stages of the contagion and were affected early on by confinement measures, reduced mortality rates. On the same basis, Orea and Álvarez [11]) using a spatial econometric approach simulate different scenarios to assess the effectiveness of the lockdown measures. Their results suggest that the lockdown reduced the COVID-19 cases in about 80% especially in provinces close to the outbreaks. Also, they conclude that the effectiveness of the lockdown could have improved by 12.8% if the measures would have been implemented a week before.
Phase out of restrictions
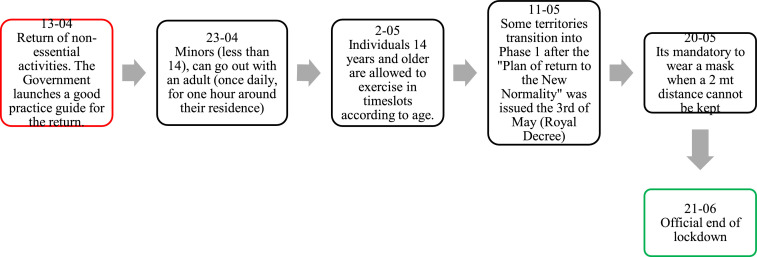
The reduced number in daily cases among others implied that gradually the country phased out the restrictions (see Fig. 9 ). As of Monday, 13th of April, working restrictions to non-essential workers were lifted, and thousands [12] of workers returned to work, while citizens were still obliged to stay home until the 26th of April. Two further policies were put in place: first, allowing minors (younger than 14) to go outside, and second, in different timeslots, for those 14 years and older to exercise outside.
Fig. 9.
Policy interventions to contain the spread of the virus starting with the phase out of restrictions
[12] on the dates of press notes.
The government has since agreed on a “Plan of return to the New Normality”. Different to how the State of Alarm happened, applicable for the whole of Spain, this plan would occur per AC in a process of co-governance with the Ministry of Health. Some criteria was put out by the Ministry of Health, but also, due to the fact that the government is in minority, political pressures from the AC played an important role. The plan established 4 phases: Phase 0 (State of Alarm) and 3 additional phases (Phase 1: family and friends reunions of up to 10 people; Phase 2: 15 people: Phase 3: mobility between provinces of the same AC), which differ in terms of the activities that are allowed in each. Schools remain closed until September, while some students can voluntarily go to school. Only when each AC reaches Phase 3, competences in health, temporarily in hands of the Ministry of Health, are returned to the AC. Currently, all AC are under no lockdown, while as of the increase in cases, clubs, bars and other will close back up.
When measures started to be consistently at lower levels, cases have started to slowly go up, and have now increased quite significantly to levels of April. Moreover, mobility has increased substantially, and currently, probably due to the summer period, it is higher than in the reference period. This correlates too with the increases in cases observed.
Policies aimed at containing the economic impact
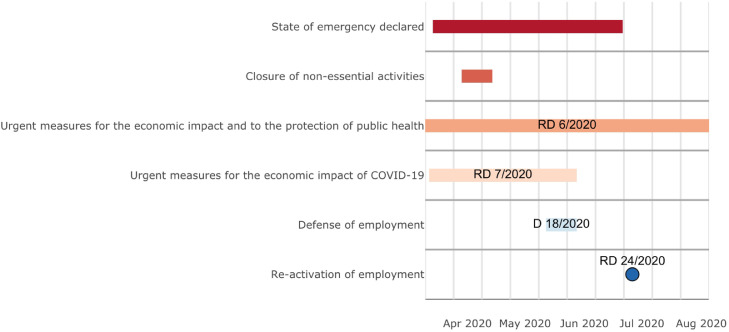
Shutting down the economy, has meant that the government, to reduce the catastrophic impacts in businesses and individuals in terms of finances, have implemented several policies to push money into the country. Legally, this have been published through several Royal Decrees (RD). Fig. 10 shows the timeline of the four main decrees that aimed at addressing the economic impact of COVID-19, and the two main restrictions imposed: declaration of the state of alarm and the closure of non-essential activities.
Fig. 10.
Main economic policies.
On the 10th of March (Royal Decree 6/2020), the first decree with economic measures was published. One of the main measures aimed at individuals who worked in the public administration, and where in isolation, to opt for Temporary Incapacity, similar to the Work Accidents. Additionally, measures related to mortgages where enacted.
On the 12th of March, the Royal Decree 7/2020 (further revised on the 18th, 28th of March and 28th of May) assigned 18,225 million euros to mitigate the economic impact of COVID-19. The package assigned funds to reinforce the health system (1,000 million euros for the Ministry of Health through the contingency fund, for extraordinary expenses; advance of 2,800 million euros for payments to the accounts of the AC to reinforce the availability of resources for the health system); to support families (25 million euros for specific resources to the AC, to guarantee food to kids in vulnerable situation and affected by the closing of schools); and to businesses (flexibility in the postponement of tax paying for 6 months, with bonification on the interest rate - Independent workers and SME-, injecting up to 14,000 million euros of liquidity). Additionally, measures for the tourism sector where enacted. The 18th of March, the economic stimulus supplemented with 300 million euros the budget of the Ministry of Social Rights and 2030 Agenda. Additionally, water and energy supply would be guaranteed for vulnerable users, as well as flexibility in mortgage payments, among other related dispositions. Moreover, 29.65 million euros where assigned for scientific research of COVID-19 (for ISCIII and CSIC).
The Decree 18/2020 expanded measures related to an unemployment figure, Temporary Employment Regulation known as ERTE, to protect employment, ranging from an extension of this measure due to major circumstances, and allowing those with ERTE to not contribute to social security. Additionally, and not strictly related to COVID-19 but highly influenced, was the implementation of the Minimum Vital Income (June).
The Royal Decree 24/2020, aimed at reactivating employment, protecting autonomous work and the competitiveness of the industrial sector.
Health care and health response and the use of technology
To address the needs associated to COVID-19, Spain had to unravel an extraordinary response in regard to its health system, putting to the forefront technology interventions. The pandemic, has also had spillover effects on non-COVID-19 related health care and health problems which are necessary to address to comprehend the full picture of the efforts and impacts.
Changes in the supply and demand of COVID-19 related resources
Initially, Spain was not equipped to deal with the rapid surge in cases. As mentioned, not only the organization of the system (e.g. decentralized), had to be modified, but the delivery of care (e.g. telemedicine), and its capacity had to be increased significantly in all major areas. This ranged from testing (availability of PCR and Rapid Tests, as well as labs to analyze them), beds (in existing and new facilities, and of different levels of severity – general ward and ICU), ventilators, medical staff to personal protective equipment (PPE).
Two main changes with respect to the delivery of care occurred: a move towards telemedicine, and the use of phone-apps to provide information about the illness. First, several private initiatives towards telemedicine, in the form of apps and in supplementary insurance plans added this type of consults and experienced a growth of their use [13]. Public use of telemedicine has been locally promoted, for example, the “HAZLO” project, for the Cardiac Rehabilitation Unit of the Ramón and Cajal University Hospital (ISCIII and Ramon y Cajal University Hospital) is a good example, while other types of consultations in the public system have been done through phone calls. Second, the severity of the spread required information and services to alleviate calls to emergency rooms. Phone apps where a key tool to provide information, self-diagnostic and monitoring of symptoms (e.g. apps like “StopCOVID19” in Cataluña, “Coronamadrid app” for Madrid or “Asistencia COVID-19″ in Canarias, Cantabria, Castilla-la Mancha, Extremadura, and Asturias). In the Pais Vasco, “COVID19.EUS”, aimed additionally at prevention, follow up to possible cases in their homes, and analysis of the concentration of cases.
Capacity of the system was quickly upscaled. One area of specific importance was testing. As the emergency unraveled, to contain the spread testing had to be increased and testing criteria evolved. Testing widely has become the cornerstone of the health policy specially, to be able to lift restrictions. To achieve that objective, the country has increased labs available and processing capacity and purchased significant amount of materials. A key actor in this regard, dependent on the Ministry of Health, is the National Center of Microbiology (Centro Nacional de Microbiología), which has assessed testing facilities and performed testing analysis. A key component has been the use of technology. Specifically, the use of robots (currently, 4) in different institutions to automatize testing. This has been paired with the purchase of swabs (PCRs) and antibodies tests that have been distributed. Table 3 shows the testing criteria. In can be observed that a reduction of the initial restrictions in place occurred over time.
Table 3.
Changes in testing criteria for COVID-19.
| 25-02-20 | Recommended to individuals who have symptoms, and that in the past 14 days have been in one of the risk zones (China, South Korea, Japan, Singapore, Iran, and 4 regions in Italy - Lombardy, Veneto, Piamonte and Emilia Romagna). Additionally, testing can be performed to those patients with severe respiratory symptoms, and that every other cause has been ruled out. |
| 18-03-20 | Person with a clinical case of acute respiratory infection that is hospitalized or that complies with clinical criteria to be admitted to other hospital; person with a clinical case of acute respiratory infection of various of any severity and that belongs to the following groups a) sanitary worker, b) other social services. The diagnostic test can be performed to a person in vulnerable situation with a clinical case of acute respiratory infection independent of the severity after individual clinical evaluation. Rapid test, nevertheless, can be performed to a broader population, vulnerable groups and persons with home isolation with symptoms. |
| 07-04-20 | Rapid antibody tests: They can be performed to symptomatic patients, moderate or severe in hospitals, or mild symptoms in the extra hospital, fundamentally in the residences of elderly and sociosanitary centers. |
Source: [12].
Despite there being no publicly available records of the number of daily tests being performed up to the 23rd of April, information released in press conferences by government authorities have stated that the number of tests went from 30,000 (15th of March) to 355,000 (22nd of March), stating an estimated capacity of the country to perform between 15,000 to 20,000 daily tests. Until the 6th of August, a total 7,472,031 tests had been performed (PCR: 4,983,935, Rapid Test: 2,143,910, Other for Antibodies: 344,186). Processing capacity was increased significantly through accreditation of new facilities and the automatization of testing. Indeed, the 2nd of May, 54 labs where validated to perform PCR tests, an increase of 41 from the 13 institutions that where performing tests on 13th of April [14].4 This has set the processing capacity to around 47,000 daily PCR tests.
Since reporting started, on the 13th of April, the median days from symptoms to diagnostics was 5 days (29 range), while on the report of the 15th of July, this number had reduced to 3 ([1–5] range). Nevertheless, regions vary in their testing agility, as outlier is Melilla, with 15 days, and a range of 3–26, until the 30th of July, while this value dropped to 4 on the 6th of August [3].
With respect to tracing, the task has been given to the AC and a protocol has been elaborated by the Ministry of Health on that regard. As the regions have the autonomy to decide their tracing strategy, there is variation in the way they do so. A notable case that has been criticized is Madrid, that hired a private company to do the tracing [15]. Tracing, as of the first report (15th July), managed to reach 1 (0–3) close contact. Until the 6th of August, the mean number of close contacts traced was 4 ([1–5] range). Again, there is variance between the regions, as the highest median number of contacts identified per case in Canarias is 9 ([3-30] range), while the lowest is Castilla La Mancha with 1 (0–3 range) (6th August) [3].
Provisional hospitals had to be opened. Notable cases are IFEMA (Feria de Madrid) (21st March) that could have accommodated, if necessary, up to 5,000 beds (and up to 800 ICU beds) although it had a maximum of about 1,200 simultaneous patients; and in Cataluña, Fira de Barcelona, which opened ready to admit 300 patients although potentially they could have been increased to 1,000.
Before the 29th of March, ICU beds totaled 4,405 [1]. As observed in Table 4 , where the new ICU and total beds are presented, an increase of 72% has been experienced to a total of 7,577 as of March 29th. Despite some of the AC, previous to the virus, having the highest regional number of ICU beds (e.g. Madrid, 704), the sharp increase in cases saturated the capacity. The AC that increased in the greatest percentage its ICU capacity was País Vasco (207.3%), followed by Murcia (192.7%), and Madrid and Cataluña (145% and 115.6%, respectively).
Table 4.
New beds (as of 29th of March) and total current beds per 100,000 population.
| Autonomous Community | New beds (29 march)(*,+) | Total+ | % Increase |
|---|---|---|---|
| Andalucía | 3.5 | 12.2 | 40.3% |
| Aragón | 10.9 | 21.1 | 106.7% |
| Asturias | 5.6 | 14.7 | 61.3% |
| Navarra | 8.4 | 18.3 | 84.6% |
| Canarias | 8.0 | 19.0 | 72.6% |
| Cantabria | 0.0 | 6.9 | 0.0% |
| Castilla y León | 5.5 | 13.8 | 66.0% |
| Castilla-la Mancha | 0.0 | 8 | 0.0% |
| Cataluña | 9.8 | 18.3 | 115.6% |
| C. Valenciana | 4.4 | 15.4 | 39.9% |
| Extremadura | -0.7 | 8.9 | −6.9% |
| Galicia | 0.4 | 10.2 | 4.2% |
| Baleares | 4.3 | 15.1 | 39.5% |
| La Rioja-Ceuta-Melilla | 8.3 | 11.3 | 61.8% |
| Madrid | 13.9 | 25.9 | 145.0% |
| País Vasco | 16.8 | 24.9 | 207.3% |
| Murcia | 15.9 | 24.1 | 192.7% |
| Total | 7.2 | 16.1 | 72.0% |
A key resource to treat serious patients are ventilators (invasive and non-invasive types). There is no data regarding pre-COVID-19 availability of ventilators to offer relevant comparisons. Nevertheless, since data has been made public (30th of March), an increasing number of ventilators have been added to the health system (at that time, 696 additional ventilators (640 non-invasive, 56 invasive)). To the 21st of April, this number had increased by 3.6 times to 3,200 (2,200 non-invasive, 1,000 invasive) [12],5 and to the 19th of May, total numbers doubled to 6,779 (an addition of 3,085 invasive and 494 non-invasive ventilators). This was made possible through local manufacturing (Hersill and SEAT companies) and different purchasing agreements in the international markets.
Personal protective equipment (PPE) became a key resource to provide the necessary safety conditions for the medical staff to treat COVID-19 patients. Shortages have been deemed one of the main reasons for the number of medical staff infected in Spain. Indeed, numbers nearly tripled in 5 days at the early stages of the pandemic (22nd of March to 27th of March), from 3,475 to 9,444 [16], [17], reaching 26,672 on the 14th of April. Since the 30th of April, a report is elaborated by the ISCIII provides in depth analysis of the infections among the medical staff [18]. Taking the proportion of reported stuff over reported total infections, the number of infected staff since the first report to the latest have evolved as 30,095, 31,971, 36,449 to 38,280 (14 of May).
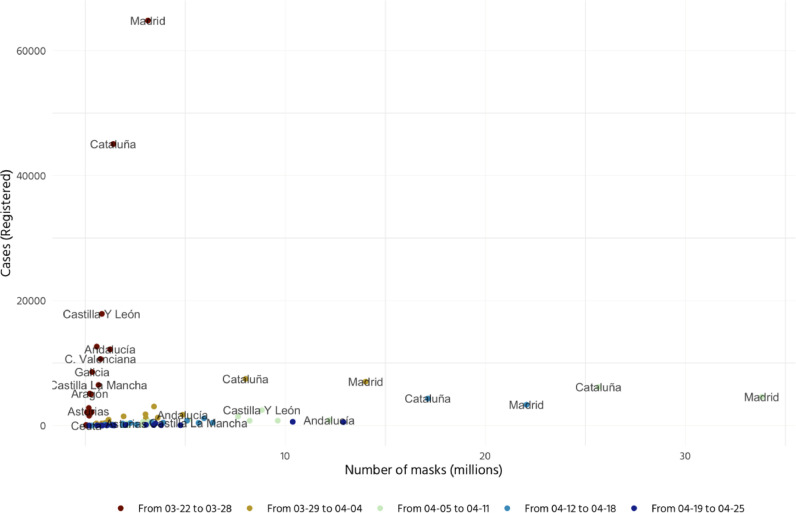
In an effort to increase work safety, the country had to significantly increase the delivery of PPE across AC. By means of centralized purchasing the distribution of PPE was under criteria based on epidemiological data and the population size of the AC. Fig. 11 . shows the relationship between the number of cases registered and the distribution of PPE weekly over a period of month. Madrid and Cataluña registered the highest number of cases and were also the top AC by number of PPE distributed (having each an accumulated amount of 86 and 62.5 million respectively). In general, all AC experience the highest increase in PPE distributed during the week from the 29th of March to the 4th of April. After this week the amount of received per AC decreased. As of 19th of May, a new system was implemented combining the petition of the AC and the Ministry of Health to allocate a “reservoir amount” of masks. This figure excludes purchases that may be carried out by AC individually.
Fig. 11.
Delivered masks to AC weekly and daily cases (10-03 to 20-04).
Note: There is missing information between the 20th and before the 19th of May. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
[12].
To deal with the human resource shortages that COVID-19 infection of medical staff and the general spread of the virus put in the system, a series of conditions previously in place related to contracting of medical staff, retirement, resident doctors, and graduation of health professionals had to be relaxed. The Ministry of Health informed that to the 2nd of April, it had increased the available for-hire health professionals to an extra 80,000. The second group of measures has consisted of cross-regional hiring process of health professionals from regions with less demand of COVID cases to regions with higher levels of demand as for example Madrid or Cataluña.
Changes in the supply and demand of non-COVID-19 related health care and health
The outbreak and focus on COVID-19 has resulted in a quick transformation in healthcare processes and structures that have produced spillover effects on the delivery of other medical service, and health aspects. One important aspect is related to waiting times. Latest reports (December 2019) [19], demonstrated an increase before and due to the pandemic effect on shifting the focus to treat COVID-19 patients, they will suffer an increase. One specifically critical health service relates to transplants. The National Transplant Organization has released information stating that there has been a 82% decrease in donors and 85% decrease in transplants compared to the same period of the previous year [20]. There is also record of a decreased participation in mandatory immunization programs during the first months of the pandemic [21]. In short, many non-urgent health services were avoided by the population or postponed by the health services during the pandemic and will have to catch up when possible.
In addition, other types of measures were implemented. Pané-Mena and Pascual [22] list three types of measures implemented on specialist services that included coordination and crisis management measures, support measures refocusing some services exclusively to COVID-19 related cases and referring other series to other centers and logistic measures based on tackling with the lack of devices and materials to provide a suitable healthcare.
Economic and financial fluctuation
The economy of Spain has suffered increased hardship due to the pandemic. GDP has contracted by −18.5 in the second quarter of 2020, and is currently in technical recession [23], falling close to the worst projections by the Spanish bank, between 16% and 21.8% [24].
Moreover, the IBEX-35 stock, has decreased significantly since January, with the lowest value being registered after the declaration of the State of Alarm (Fig. 12 ). Since then, the evolution has been positive, while still below levels of mid-February. The most significant increase was produced when the announcement of the credit loans for the tourist sector was made in mid-June [25], as this sector represents an important part of the Spanish economy, that in 2019 accounted for 12.3% of the GDP, and 2.62 million jobs [26].
Fig. 12.
Ibex-35 trends January - August 2020.
Note: Blue (first) dotted line indicates start of lockdown (15th March), red (second and third) dotted lines indicate the closure of non-essential activities (1st-14th April). Green (fourth) dotted line represents the official end of lockdown (21st June).
[43].
Unemployment rates in Spain have gone up to 15.33% in the second quarter of 2020 from 13.78% in the last quarter of 2019 [27]. In spite of this negative evolution, the unemployment rate is still much lower than in the first quarter of 2013, during the earlier economic crisis, when it reached the peak of 26.94%. However, this number does not consider those workers that have been subject to the temporary regulation of employment “ERTE” (suspension of work or reduction in hours). At the same time, in the last months, the labor market has changed drastically, as full time job placements have gone down 17.7 percentage points [23]. As a result, the affiliation to social security decreased in the month of July in the amount of −747,657 individuals (most of them men, 53%) [28].
Whether the economic impact of the pandemic is as large as estimated or even greater, will depend on the speed at which economic activity returns to normal, and on the existence of a possible resurgence or second wave that would requiere shutting down the economy again, before a preventive vaccine or cure for COVID-19 becomes available.
Concluding remarks
Spain was one of the first countries to be hardly hit by COVID-19 in terms of cases and deaths. Data shows that the country overcome the peak of the spread and intensity of the virus, greatly aided by the very stringent confinement policies that lasted for nearly 2 months, aided by strict enforcement which implied fines reached all-time peak, and resulted in a significant decrease of mobility.
Having been an early epicenter, it struck the health system by surprise. The virus showed that the health system was not ready to confront a strain of this magnitude. Nevertheless, the country managed to be quick in changing the necessary health system structures and increasing its resources to deal with the surge in cases. This encompassed from re-arranging the decentralized health system to a temporarily higher degree of centralization, to the significant roll out of PPE, beds, and medical staff to confront the emergency while it was unravelling.
Despite the measures to tackle with COVID-19 have been centralized by the Ministry of Health and implemented homogeneously across the country, we have shown that the pandemic has had a different impact across Spanish regions and provinces. This situation has led to a relaxation of lockdown measures on a case-by-case basis. Under this system, in order to lift mobility restrictions, AC have been required to submit bi-weekly reports to the Health Ministry to assess the suitability of their epidemic situation and more particularly their incidence rates. In some cases, provinces within the same AC showed different degrees of severity associated with the incidence rates. For instance, this was the case of Castilla-Leon where some of its provinces closer to Madrid (e.g. Ávila, Segovia), took longer to increase their mobility compared to other provinces of the same AC located more to the north.
The current debate in terms of public health consists of how to design measures to contain the new wave of cases that are arising in different AC. These measures need to promote the primary care delivered in General Practices. Primary care plays a core role in prevention and detection of early cases. To enhance the quality of their delivery it is necessary to improve the set of resources available in the current GP premises as well as incentivize the promotion of GP staff. Further, they need to increase their capacity to conduct tests. To this extent, there has been a generalized increase of tests in all AC.
Another key area to address public health measures consists of the redefinition in the organization of long-term care services. Two thirds of COVID registered deceased in Spain occurred in a care home [29]. These figures show deficiencies in the provision of long-term care under an epidemic crisis. To this extent, the implementation of coordinated protocols with a common framework as well as measures to increase the integration between long-term and primary care, may be two main elements to consider.
Author Statements
Funding
None
Declaration of Competing Interest
None declared
Ethical approval
Not required
Footnotes
Cumulative cases cannot be deduced that the difference between one day and the next day are new cases, as some could be cases recovered from previous dates. 15th of May was the last day with information on recovered cases. Updates on public data have not been reported since the 22nd of May.
Ratio between those in working age (15-64) with respect to those 65 and above
There are some exceptions such as pharmaceuticals.
See https://lab.montera34.com/covid19/ for details.
News on the mentioned date
Press releases by the Ministry of Health on the mentioned date.
References
- 1.Ministerio de Sanidad, Consumo y Bienestar Social. Estadística de Centros Sanitarios de Atención Especializada. [Online]; 2017. Available from:https://www.mscbs.gob.es/estadisticas/microdatos.do.
- 2.Bernal-Delgado E., García-Armesto S., Oliva J., Sánchez Martínez F., Repullo J., Peña- Longobardo L., et al. Spain: health system review.; 2018. [PubMed]
- 3.Instituto de Salud Carlos III. Situación de COVID-19 en España. [Online]; 2020. Available from:https://covid19.isciii.es.
- 4.Ministerio de Sanidad, Consumo y Servicios Sociales. Actualizacion. Enfermedad por coronavirus (COVID-19).; 2020.
- 5.Ministerio de Sanidad. La inmunidad de la población española experimenta un leve incremento con una tasa del 5,21% en la segunda ronda del ENE-Covid19. [Online]; 2020. Available from:https://www.mscbs.gob.es/gabinete/notasPrensa.do?id=4950.
- 6.Sistema de Monitoreo de la Mortalidad Diaria. Mortalidad por todas las causas. [Online]; 2020. Available from:https://momo.isciii.es/public/momo/dashboard/momo_dashboard.html#nacional.
- 7.INE. Estadística experimental - Estimación de Defunciones Semanales durante el brote de COVID-19 (EDeS). [Online]; 2020. Available from:https://www.ine.es/prensa/experimental_edes.pdf.
- 8.Hale T., Webster S., Petherick A., Phillips T., Kira B. Blavatnik School of Government; 2020. Oxford COVID-19 government response tracker.https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker [Online]Available from. [DOI] [PubMed] [Google Scholar]
- 9.El Pais. Tantas multas propuestas en el confinamiento como impuestas en 4 años de la Ley Mordaza. [Online]; 2020. Available from: https://elpais.com/espana/2020-04-25/tantas-multas-propuestas-en-el-confinamiento-como-impuestas-en-cuatro-anos-de-ley-mordaza.html.
- 10.Amuedo-Dorantes C., Borra C., Rivera-Garrido N., Sevilla A. Discussion Paper Series; IZA.: 2020. Timing is everything when fighting a pandemic: COVID-19 mortality in spain. [Google Scholar]
- 11.Orea L., Alvarez I. How effective has the Spanish lockdown been to battle COVID-19? A Spatial analysis of the coronavirus propagation across provinces. Documento de trabajo. 2020 doi: 10.1002/hec.4437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ministerio de Sanidad CySS. Notas de Prensa. [Online]; 2020. Available from:https://www.mscbs.gob.es/gabinete/notasPrensa.do.
- 13.El Pais. El coronavirus impulsa la telemedicina en España. [Online]; 2020. Available from:https://cincodias.elpais.com/cincodias/2020/04/21/companias/1587487221_998649.html.
- 14.Instituto de Salud Carlos III. Noticias. [Online]; 2020. Available from:https://www.isciii.es/Noticias/Noticias/Paginas/default.aspx.
- 15.LeoNoticias. [Online]; 2020. Available from:https://www.leonoticias.com/sociedad/salud/madrid-adjudica-empresa-privada-rastreadores-covid-20200811092550-ntrc.html?ref=https%3A%2F%2Fwww.google.com%2F.
- 16.El Pais. El 12% de los contagiados por coronavirus son trabajadores sanitarios. https://elpais.com/sociedad/2020-03-22/espana-registra-28572-casos-de-coronavirus-y-1725-muertes.html. 2020.
- 17.El Mundo. https://www.elmundo.es/ciencia-y-salud/salud/2020/03/27/5e7d9513fdddff8c088b4570.html. 2020.
- 18.RENAVE; CNE; CNM (ISCIII). Informe sobre la situación de COVID-19 en personal sanitario en España. 07-05-2020.; 2020.
- 19.Ministerio de Sanidad Sistema de Información Sobre Listas de Espera en el Sistema Nacional de Salud. Situación a 31 de diciembre de. 2019;2019 [Google Scholar]
- 20.Organización Nacional de Transplantes. COVID-19: impacto en la actividad de donación y transplantes. [Online]; 2020. Available from:http://www.ont.es/infesp/Paginas/Impacto_tx.aspx.
- 21.Comité Asesor de Vacunas. COVID-19 caida de las vacunaciones. [Online]; 2020. Available from:https://vacunasaep.org/sites/vacunasaep.org/files/covid-19-caida-de-las-vacunaciones-sei-seip-aep_24abr2020b.pdf.
- 22.Pané O., Pascual J. El desafio de la COVID-19 para la atencióon especializada. In: Abellán J., Campillo C., editors. Economia de la salud (y más) de la COVID-19. AES; 2020. [Google Scholar]
- 23.INE Contabilidad nacional trimestral de España: principales agregados CNTR (Avance) Primer trimestre. 2020;2020 https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736164439&menu=ultiDatos&idp=1254735576581 [Online]Available from. [Google Scholar]
- 24.Banco de España. Macroeconomic Projections for the Spanish Economy (2020-2022): the Banco de Españas contribution to the Eurosystems JUne 2020 Joint Forecasting Exercise. [Online]; 2020. Available from:https://www.bde.es/f/webbde/SES/AnalisisEconomico/AnalisisEconomico/ProyeccionesMacroeconomicas/ficheros/be08062020-proye.pdf.
- 25.El Pais. El plan de Sanchez para ayudar al turismo se basa en créditos a empresas. [Online]; 2020. Available from:https://elpais.com/economia/2020-06-18/el-gobierno-anuncia-un-plan-de-ayuda-al-turismo-con-mas-de-4250-millones.html.
- 26.INE. Cuenta satélite del turismo de España. 2016-2018. [Online]; 2019. Available from:https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=estadistica_C&cid=1254736169169&menu=ultiDatos&idp=1254735576863.
- 27.INE Encuesta de población activa. EPA. Primer trimestre. 2020;2020 [Online] Available from: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176918&menu=ultiDatos&idp=1254735976595. [Google Scholar]
- 28.MITRAMISS. [Online]; 2020. Available from:http://www.mitramiss.gob.es.
- 29.RTVE. Sanidad estima en 27.359 los fallecimientos en residencias durante la epidemia, más de dos tercios con coronavirus. [Online]; 2020. Available from: https://www.rtve.es/noticias/20200707/sanidad-estima-27359-fallecimientos-residencias-durante-epidemia-mas-dos-tercios-coronavirus/2026023.shtml.
- 30.INE. Población por comunidades y ciudades autónomas. [Online]; 2020. Available from:https://www.ine.es/jaxiT3/Datos.htm?t=2915#!tabs-tabla.
- 31.OECD. Demography and Population data. [Online]; 2018. Available from:https://stats.oecd.org/Index.aspx?DataSetCode=EDU_DEM.
- 32.INE. Extensión superficial de las COmunidades Autónomas y Provincias, por zonas altimétricas. [Online]; 1994. Available from:https://www.ine.es/inebaseweb/pdfDispacher.do?td=154090&L=0.
- 33.OECD. Health at a Glance 2019: OECD Indicators. Paris: 2019.
- 34.OECD. Long-Term Care Resources and Utilisation: beds in residential long-term care facilities. [Online]; 2018. Available from: https://stats.oecd.org/Index.aspx?QueryId=30142.
- 35.INE. Población residente en España. [Online]; 2020. Available from:https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176951&menu=ultiDatos&idp=1254735572981.
- 36.Universidad de las Palmas de Gran Canaria. Estimacion de la Oferta y Demanda de Medicos Especialistas España 2018-2030.; 2018.
- 37.INE. N° de Enfermeros por Comunidades, Ciudades autónomas y Provincias de colegiación, situación laboral y sexo. [Online]; 2018. Available from:https://www.ine.es/jaxi/Datos.htm?path=/t15/p416/a2018/l0/&file=s08004.px#!tabs-tabla.
- 38.Ministerio de Economia y Competitividad. Mapa de recursos sociales y sanitarios. [Online]; 2015. Available from:http://envejecimiento.csic.es/recursos/residencias/index.htm.
- 39.esCOVIDdata. [Online]; 2020. Available from:https://github.com/montera34/escovid19data.
- 40.RENAVE; CNE; CNM (ISCIII). Informe. Situación de COVID-19 en España a [fecha]; 2020.
- 41.MITMA. Movilidad Autonómica Viajeros-km. [Online]; 2020. Available from:https://www.mitma.gob.es/ministerio/covid-19/evolucion-movilidad-big-data/movilidad-ccaa.
- 42.El Confidencial. El mapa de la ocupación de las UCI. https://www.elconfidencial.com/espana/2020-03-29/coronavirus-covid-19-camas-uci-hospitales_2523031/. 2020Mar 29.
- 43.Bolsa de Madrid. Precios Historicos IBEX35. [Online]; 2020. Available from:https://www.bolsamadrid.es/esp/aspx/Indices/InfHistorica.aspx?grupo=IBEX.