Abstract
Prior research has shown that acute subjective psychedelic effects are associated with both spontaneous and intended changes in depression and anxiety. Psychedelics are also theorized to produce increases in psychological flexibility, which could explain decreases in depression and anxiety following a psychedelic experience. Therefore, the present cross-sectional survey study sought to examine whether psychological flexibility mediated the relationship between acute psychedelic experiences and spontaneous or intended changes in depression and anxiety among a large international sample of people who reported having used a psychedelic (n=985; male=71.6%; Caucasian/white=84.1%; Mage=32.2, SD=12.6). A regression analysis showed that acute effects (i.e., mystical and insightful effects) were significantly associated with decreases in depression/anxiety following a psychedelic experience. A path analysis revealed that, while controlling for age and sex, increases in psychological flexibility fully mediated the effect of mystical and insightful experiences on decreases in depression and anxiety following a psychedelic experience. This suggests that psychological flexibility may be an important mediator of the therapeutic effects of psychedelic drugs. Future prospective experimental studies should examine the effect of psychedelic drug administration on psychological flexibility in order to gain a better understanding of the psychological processes that predict therapeutic effects of psychedelics.
Keywords: psychedelics, hallucinogens, mechanism, psychological flexibility, depression, anxiety
Introduction
Depression and anxiety disorders are common mental health problems (Steel et al., 2013). Global lifetime prevalence of depression and anxiety are approximately 10% and 13%, respectively (Steel et al., 2013; Bandelow & Michaelis, 2015). The public health burden of depression and anxiety includes occupational impairment (Birnbaum et al., 2010), and increases the risk for chronic physical conditions such as cardiovascular disease (Katon, 2011; Niles et al., 2015). Given high prevalence rates and the substantial public health and personal burden of these mental health conditions, numerous interventions have been developed, which include combinations of psychotherapy and pharmacotherapy (Cuijpers et al., 2014; Otto & Hearon, 2016) . Despite evidence supporting the use of these interventions, many people do not have access to these treatments (Collins et al., 2004), and many people who have access will not experience symptom relief despite intervention (Collimore & rector, 2014; Coull & Morris, 2011; Hofmann et al., 2012; Sinyor, Schaffeer & Levitt, 2010; Koen & Stein, 2011), highlighting the need for more treatment options.
One emerging area of research has examined the psychotherapeutic action of psychedelic compounds (e.g., psilocybin, LSD, ayahuasca, 5-MeO-DMT) administered in clinical trials (Carhart-Harris, et al., 2016; Johnson & Griffiths, 2017; Palhano-Fontes et al., 2018; dos Santos et al., 2016) and used in naturalistic settings (Johnson et al., 2017; Davis et al., 2018; Davis et al., 2019). These substances act primarily as agonists of serotonin (e.g., 5-HT1A/2A/C) receptors and often produce profound changes in sensory perceptions, mood, cognitions, and behavior (Araújo et al., 2015; Carhart-Harris et al., 2011; Stroud et al., 2017; Carhart-Harris et al., 2017; dos Santos et al., 2016). For example, recent studies examining psychedelics administered as an adjunct to psychotherapy have demonstrated efficacy in decreasing symptoms of anxiety and depression (Johnson & Griffiths, 2017; Carhart-Harris et al., 2017; Ross et al., 2016; Griffiths et al., 2016, dos Santos et al., 2016). Published reports also show that decreases in depression and anxiety occur following naturalistic psychedelic use in ceremonial and recreational contexts (Davis et al., 2018; Davis et al., 2019; Santos et al., 2007; Uthaug, et al., 2018). Although more work is needed to fully understand the mechanisms of therapeutic action, the beneficial effects of these substances appear to be associated with the intensity of certain types of acute psychedelic effects (e.g., mystical-type phenomena, psychological insight) during these experiences in both healthy (Griffiths et al., 2008, 2011; Barrett et al., 2015) and clinical (Ross et al., 2016; Griffiths et al., 2016; Griffiths et al., 2008; Griffiths et al., 2011; Roseman, Nutt, & Carhart-Harris, 2018; Davis et al., 2018; Garcia-Romeu et al., 2019) populations. Potential mediators of psychedelic effects on therapeutic outcomes have been suggested, including changes in the entropy of brain network connectivity (Carhart-Harris et al., 2014), the importance of awe/ego dissolution (Hendricks, 2018; Preller & Vollenweider, 2018); and the possible role of changes in psychological flexibility following a psychedelic experience (Sabucedo, 2017; Kuypers et al., 2016; Walsh & Thiessen, 2018).
Psychological flexibility is described as an essential set of processes that help people manage stressors and engage in adaptive behaviors that promote values-driven action (Gloster, Meyer, & Lieb, 2017). Psychological flexibility is a transdiagnostic construct wherein people are thought to have the capacity to develop skills recognizing and adapting to various contextual demands, shift their mindset or behaviors during individual and social experiences, maintain balance across important life domains, and learn to be open to, aware of, and committed to behaviors that are congruent with their values (Kashdan & Rottenberg, 2010). According to this model, well-being is supported by fully contacting the present moment as a conscious human being and changing or persisting in a values-driven behavior regardless of what is present in each moment (Hayes, Stroshal, & Wilson, 2012). Conversely, dysfunctions in mental health, including depression and anxiety disorders (Kashdan & Rottenberg, 2010), are theorized to be the result of reduced psychological flexibility (or psychological inflexibility).
Psychological interventions have been developed using this theoretical framework (e.g., Acceptance and Commitment Therapy (ACT); Hayes et al., 2006), which attempt to increase psychological flexibility via six interconnected processes (i.e., acceptance, defusion, being present, self-as-context, determining direction for behavior change, and using techniques to facilitate change; Twohig & Levin, 2017). Meta-analyses have shown moderate to strong effects in favor of ACT interventions (compared to control conditions: waitlist, psychological placebo, and treatment as usual) in decreasing anxiety and depression symptoms (A-Tjak et al., 2015; Hacker, Stone, & MacBeth, 2016), and evidence shows that the positive outcomes of this intervention are mediated by increases in psychological flexibility (Twohig & Levin, 2017; French, Moghaddam, & Shroder, 2017). If psychedelic experiences promote increases in psychological flexibility, then such increases could be mediating the antidepressive and anxiolytic effects observed in clinical trials (Johnson & Griffiths, 2017; Carhart-Harris et al., 2017; Ross et al., 2016; Griffiths et al., 2016, dos Santos et al., 2016) and the associations found in naturalistic psychedelic use (Davis et al., 2018; Davis et al., 2019; Santos et al., 2007; Uthaug, et al., 2018). This relationship could also justify a psychotherapeutic approach to psychedelic-assisted therapy that focuses on processes of change with the psychological flexibility model.
The present cross-sectional survey study sought to examine psychological flexibility as a potential mediator of acute psychedelic experiences on changes in anxiety/depression. Prior research has shown that acute psychedelic effects are associated with reductions in depression and anxiety (Griffiths et al., 2016; Ross et al., 2016; Davis et al, 2019), that psychedelic effects are associated with changes in psychological flexibility (Kuypers et al., 2016), and that increases in psychological flexibility are associated with positive depression and anxiety outcomes (Twohig & Levin, 2017). Therefore, in a regression model we expect to find (Hypothesis 1: H1) acute psychedelic effects (mystical and insight effects) will predict changes in depression and anxiety following a psychedelic experience, and in a path model we expect to find that H2) acute psychedelic effects will be directly related to increases in psychological flexibility, H3) increases in psychological flexibility will be directly related to decreases in depression/anxiety, and H4) psychological flexibility will mediate the relationships between acute psychedelic effects and decreases in depression and anxiety symptoms.
Method
Procedure
The current study data were collected as part of a large anonymous internet-based cross-sectional survey of individuals who reported having a moderate to strong psychedelic experience in the past. Specifically, people were recruited as part of a larger study examining acute insight (e.g., an awareness into emotions, behaviors, beliefs, memories, relationships, etc.) gained as a result of a psychedelic experience. Recruitment from the parent study is ongoing and results will be published in a forthcoming article. Respondents were recruited by using electronic message postings and advertisements on several internet websites (e.g., www.erowid.com; www.facebook.com; www.reddit.com), electronic mail announcements, and via an article published by Motherboard/VICE). Advertisements directed potential respondents to a secure web-based survey (hosted by: www.qualtrics.com), and those who clicked a study link were presented with a consent document detailing the inclusion criteria. Eligible volunteers had to endorse being at least 18 years old, able to read, write and speak English fluently, have taken a dose of a single psychedelic (e.g., psilocybin mushrooms, psilocybin, LSD, ayahuasca, mescaline, N,N-DMT, 5-MeO-DMT, peyote, 4-Acetoxy-DMT, Salvia, Ibogaine, etc.) that produced moderate to strong psychoactive effects, and after taking the substance they must have had an experience that contributed to gaining psychological insight. Following consent, respondents completed each study questionnaire (described below). The study was approved by the Johns Hopkins School of Medicine Institutional Review Board and the full survey is available from the corresponding author. No incentives were offered in this study.
Study Recruitment Flow
Respondents were recruited from June 2018 through January 2019. Of all individuals who clicked the advertisement link (n=14,911), 3080 consented and completed the survey. However, 960 of these respondents were excluded because they reported using more than one substance in their psychedelic experience. Of the remaining 2120, a total of 985 were included in the final sample because they indicated experiencing a change in anxiety or depression as a result of a psychedelic experience.
Measures
Psychedelic Experience
We asked respondents to report which psychedelic substance they had used (e.g., psilocybin, LSD, N,N-DMT, Ayahuasca, 5-MeO-DMT, Mescaline, Salvia/Salvinorin A, peyote cactus, Iboga/ibogaine, or “Other”), the subjective level of dose (i.e., Low, Moderate, Moderately high, High), route of administration (i.e., Oral, Sublingual, Smoked or Vaporized, Buccal, Intravenous, Intranasal), and length of time since the experience (e.g., 3-6 months ago, 7-11 months ago, 1-2 years ago, etc.).
Acute Mystical Experiences
The Mystical Experiences Questionnaire (MEQ) was used to assess subjective mystical-type phenomena that may have occurred after taking the psychedelic (MacLean et al., 2012; Barrett, Johnson & Griffiths, 2015). Respondents were asked to think back on their experience with a psychedelic and then to rate the extent to which each of 30 descriptors applied at any point during their session on a 6-point scale from 0 = “None; not at all” to 5 = “Extreme (more than ever before in my life).” Similar to prior research (Davis et al., 2018; Davis et al., 2019), we calculated a total mean score of all items on the questionnaire. Internal consistency reliability of the total scale was excellent (alpha = .94).
Acute Insight Experiences
The Psychological Insight Questionnaire (PIQ) was created to assess the degree to which respondents experienced acute insight (e.g., gained an awareness into your emotions, behaviors, beliefs, memories, or relationships) that sometimes occurs after taking a psychedelic. Respondents were asked to think back on their experience with a psychedelic and then to rate the intensity with which they experienced each of 28 insight experiences at any point during their session, and similar to the MEQ they rated each item on a 6-point scale from 0 = “No; not at all” to 5 = “Extremely (more than ever before in my life).” A total score was calculated as the mean of the responses to each item, and the internal reliability of this total score was excellent (alpha = .93). The PIQ is under development and the psychometric properties of this questionnaire will be reported in a forthcoming manuscript. See Table 1 for items, item means (and standard deviations), and percent endorsement of each item (“No, not at all” = 0 and all other response options = 1).
Table 1.
Psychological Insight Questionnaire item means and standard deviations (N=985).
| Item | Mean(SD) | Proportion of sample that endorsed at any intensity levela |
|---|---|---|
| Realized how current feelings or perceptions are related to events from my past | 3.51 (1.52) | 93.1% |
| Awareness of uncomfortable or painful feelings I previously avoided | 3.17 (1.67) | 88.1 |
| Realized ways my beliefs may be dysfunctional | 3.53 (1.55) | 91.4 |
| Discovered how aspects of my life are affecting my well-being | 3.93 (1.21) | 97.6 |
| Gained a deeper understanding of events/memories from my past | 3.48 (1.52) | 93.4 |
| Experienced validation of my life, character, values, or beliefs | 3.71 (1.43) | 94.5 |
| Realized the importance of my life | 3.84 (1.48) | 92.8 |
| Awareness of dysfunctional patterns in my actions, thoughts, and/or feelings | 3.66 (1.43) | 94.2 |
| Discovered specific techniques for coping with difficulties | 3.19 (1.57) | 90.6 |
| Realized how critical or judgmental views I hold towards myself are dysfunctional | 3.58 (1.50) | 93.3 |
| Discovered I could explore uncomfortable or painful feelings I previously avoided | 3.47 (1.55) | 91.7 |
| Gained a deeper understanding of previously held beliefs and/or values | 3.84 (1.27) | 97.1 |
| Discovered a vivid sense of the paradoxes in life | 3.63 (1.57) | 92.0 |
| Realized I could experience memories previously too difficult to experience | 2.37 (1.86) | 72.9 |
| Awareness of beneficial patterns in my actions, thoughts, and/or feelings | 3.29 (1.45) | 93.1 |
| Discovered a clear pattern of avoidance in my life | 2.76 (1.72) | 83.1 |
| Realized the nature and/or origins of my defenses or other coping strategies | 3.04 (1.63) | 88.0 |
| Discovered new insights about my work or career | 2.29 (1.88) | 70.6 |
| Gained resolution or clarity about past traumas or hurtful events | 2.91 (1.78) | 83.6 |
| Discovered clear similarities between my past and present interpersonal relationships | 2.83 (1.74) | 83.1 |
| Discovered new feelings or perspectives about significant relationships in my life | 3.65 (1.48) | 93.0 |
| Realized certain actions I should take in regards to important relationships in my life | 3.42 (1.56) | 91.4 |
| Discovered new actions that may help me achieve my goals | 3.28 (1.53) | 91.7 |
| Realized the point of view or actions of others that had been difficult to understand previously | 3.25 (1.61) | 89.7 |
| Discovered clarity or creative solutions about how to solve a problem in my life | 3.28 (1.55) | 91.7 |
| Awareness of information that helped me understand my life | 4.14 (1.14) | 97.8 |
| Discovered ways to see my problems with more clarity | 3.81 (1.30) | 96.0 |
| Awareness of my life purpose, goals, and/or priorities | 3.77 (1.42) | 94.7 |
Note. Range of scores of all items was 0-5.
Response options were on a scale from 0 = “No, Not at all” to 5 = “Extremely (more than ever before in my life)”. Data in this column show the proportion of respondents who endorsed any option other than “No, Not at all.”
Anxiety and Depression
The Depression, Anxiety, and Stress Scale (DASS-21) was used to assess for anxiety and depression symptoms during the 3 months before and 3 months after the psychedelic experience. This 21-item scale (Lovibond & Lovibond, 1995) examines the core negative emotional experiences of depression and anxiety that respondents reported experiencing. The DASS-21 is comprised of three subscales: depression, anxiety, and stress, of which we used a subscale consisting of the combined depression and anxiety subscales in the current study. There are seven items in each subscale and respondents are asked to respond to each item on a scale from 0 = “Never” to 3 = “Almost always.” Internal consistency reliability was good for the before measures (depression subscale alpha = .91; anxiety subscale alpha = .80) and adequate-to-good for the after measures (depression subscale alpha = .84; anxiety subscale alpha = .69). In the present study, we examined subjective changes in depression and anxiety following a psychedelic experience by calculating a mean total change score by subtracting the total depression and anxiety after scores from the total depression and anxiety before scores for each respondent (e.g., negative scores represent a decrease in depression/anxiety). A single measure combining depression and anxiety subscales (depression/anxiety) was analyzed as the dependent measure in analyses reported in this report. Separate analyses for depression and anxiety subscales are reported in supplementary material.
Psychological Flexibility
The Acceptance and Action Questionnaire II (AAQII; Bond et al., 2011) was developed as a measure of psychological inflexibility, and in the present survey it was used to assess the degree of psychological flexibility respondents experienced before and after the psychedelic experience. The AAQII is comprised of 7 items and respondents were asked to respond to each item on a scale from 1 = “Never true” to 7 = “Always true.” Lower scores on this measure indicate greater psychological flexibility. Internal consistency reliability was good for the psychological flexibility before measure (alpha = .88) and the psychological flexibility after measure (alpha = .88). We examined changes in psychological flexibility by calculating a mean change score. This calculation involved subtracting the mean psychological flexibility before score from the mean psychological flexibility after score for each respondent in order to ease interpretation (i.e., we calculated a positive change score to denote increases in psychological flexibility). This change score was used in all analyses.
Demographics
We included items inquiring about the age, sex, gender, race, ethnicity, country/region of residence, income, level of education, and relationship status of each respondent.
Data Analyses
Data Quality.
Study completion time was examined in order to identify cases of rushed and possibly careless responding. Overall, respondents completed the survey in approximately 47 minutes. Only 3 respondents took less than 15 minutes to complete the survey; 25% of the sample completed the survey in less than approximately 33 minutes; and 75% of the sample completed the survey in less than approximately 67 minutes. Although 3 respondents completed the survey in less than 15 minutes, a review of their responses did not provide any indication of careless responding. This pattern of response time suggests that careless responding was not a concern.
Analytic Plan.
First, descriptive statistics for demographic and background characteristics for all study variables were calculated. Pearson and point biserial correlation coefficients were calculated to examine the relationships among all primary study variables (age, sex, acute insight and mystical effects, depression/anxiety change score, and psychological flexibility change score). Given the large number of respondents in the sample, we used a coefficient cutoff of .20, and used an alpha cutoff of p < .001, to determine whether a correlation was both meaningful and statistically significant, respectively. Next, a regression analysis was used to test (H1): acute mystical and insight experiences will be negatively associated with depression/anxiety change score. A path analysis was then used to test hypothesized direct effects (H2-H3: Intensity of psychological insight and mystical effects have a direct effect on changes in psychological flexibility, and changes in psychological flexibility have a direct effect on changes in depression/anxiety) and mediation effects (H4): Intensity of psychological insight and mystical effects are indirectly related to changes in depression/anxiety via and the path analyses. Analyses were conducted in SPSS v 25 (IBM Corp, 2018) and MPlus version 7.0 using weighted least square mean and variance estimators (Muthén and Muthén 1998-2017).
Results
Respondent Characteristics
Most of the sample reported they were male (72%), Caucasian/white (84%), never married (51%), currently live in the United States (65%) and earned $35,000 or more in income (60%). Average age in the sample was 32.2 (SD = 12.6). Over three-quarters of the sample reported that their psychedelic experience was occasioned by LSD (42%) or psilocybin/mushrooms (38%) as the psychedelic substance used to occasion their experience. Furthermore, about one-half of the sample reported that the dose was moderately-high (36%) or high (21%). The psychedelic experience had occurred at least 1 year prior to the survey in 75% of the sample). Overall, there was a mean decrease in depression/anxiety (M=−6.80; SD=5.61; Range: −21 to +9), and a mean increase in psychological inflexibility (M=2.01; SD=1.44; Range: −4.14 to +6), from before to after the psychedelic experience. Additional details about respondent characteristics are shown in Supplemental Table 1.
Associations between acute psychedelic effects and changes in psychological flexibility and depression/anxiety
A series of point-biserial correlations revealed that the type of psychedelic drug used by respondents (Psilocybin: No = 0, Yes = 1; LSD: No = 0, Yes = 1; Other Psychedelic: No = 0, Yes = 1) was unrelated (range: −.19 to .14) to all other variables (age, sex, acute insight and mystical effects, depression/anxiety change score, and psychological flexibility change score). Additionally, as Table 2 shows, the intensity of mystical effects was moderately correlated with insight effects and to a lesser degree with decreases in depression/anxiety and increases in psychological flexibility. Intensity of psychological insight was moderately correlated with decreases in depression/anxiety; and the intensity of psychological insight and decreases in depression/anxiety were correlated with increases in psychological flexibility.
Table 2.
Means, standard deviations, and correlations among variables included in path analysis (i.e., mystical experiences score, psychological insight score, depression/anxiety symptom change score, psychological flexibility change score; N = 985).
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1. Age | 32.19 (12.6) | . | .07 | .09 | −.09 | .14 | −.07 |
| 2. Sexa | 1.27 (0.45) | . | .09 | .01 | −.06 | .08 | |
| 3. Mystical Experiences | 3.80 (0.89) | . | .41 | −.19 | .28 | ||
| 4. Psychological Insight | 3.38 (0.91) | . | −.31 | .50 | |||
| 5. Decrease in anxiety/depression | −6.80 (5.61) | . | −.62 | ||||
| 6. Increase in psychological flexibilityb | 2.09 (1.44) | . |
Note. Bolded items were considered statistically significant (p<.001) and meaningful (coefficient > .20).
Sex coded Male = 1, Female = 2
The AAQII was originally developed as a measure of psychological inflexibility. Reduction in AAQ scores indicates an increase in psychological flexibility. However, to ease interpretation, we have calculated a positive change score to denote increases in psychological flexibility.
Regression analysis
Table 3 shows data from the multiple linear regression including acute mystical (M=3.81; SD=.89) and insight effects (M=3.38; SD=.91) as predictors of decreases in depression/anxiety (M=−6.80; SD=5.61). The overall model was significant (p <.001), accounting for 10% of the variance in depression/anxiety change scores (H1). Although accounting for a relatively small amount of variance in this model, the intensities of both mystical and insight effects were associated with decreases in depression/anxiety (see Table 3).
Table 3.
Summary of multiple linear regression showing significant predictors of changes in depression or anxiety (spontaneous and intended) from before to after a psychedelic experience (N=985).
| Variables | B | SE B | β | t | p |
|---|---|---|---|---|---|
| Constant | .90 | .83 | |||
| Mystical effects | −.51 | .21 | −.08 | −2.428 | .015* |
| Psychological insight effects | −1.71 | .20 | −.28 | −8.395 | .000*** |
| Adjusted R2 | .10 |
Note. The overall model was significant, F(2, 984) = 55.675, p<.001.
p < .05
p < .001
Path analysis
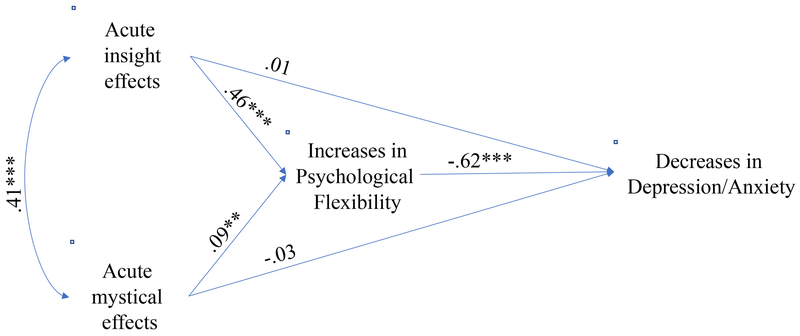
As shown in Figure 1, the path analysis controlling for age and sex revealed that greater mean intensity of acute mystical and psychological insight effects were directly related (Mystical: β=.09, p<.01; Insight: β=.46, p<.001) to mean increases in psychological flexibility (Mincrease=2.09; SD=1.44; supporting H2), mean increases in psychological flexibility were directly related (β=−.62, p<.001) to mean decreases in depression/anxiety (supporting H3), and indirect effects were found wherein psychological flexibility mediated the relationships between the intensity of acute mystical (β=.06, SE=.02, p < .01) and insight (β=.29, SE=.02, p < .001) effects and mean decreases in depression/anxiety (supporting H4). Model fit was good: root mean square error of approximation = .055 (95% CI: .01, . 12); comparative fit index = .995; weighted root-mean-square residual = .394.
Figure 1.
Path analysis showing that increases in psychological flexibility mediate relationship between acute effects of psychedelics and decreases in depression/anxiety (full sample, N=985). **p<.01, ***p<.001.
Supplementary analyses
The sample used for our primary analyses (described above) was a group of individuals who reported a spontaneous or intended change in anxiety (intended N = 142; spontaneous N = 197) or depression (intended N = 366; spontaneous N = 280) following a psychedelic experience. In the path analysis shown in Figure 1, we collapsed these groups into one sample (N = 985), and averaged measures of depression and anxiety into a single measure, in order to examine our primary study hypotheses in a more concise manner. However, we also analyzed all study hypotheses (H1-H4) within each of these subgroups using the same analytic approach described above, and these tables and figures are available in supplementary files (Suppl. Tables 1–4; Suppl. Figures 1–4). In short, all hypotheses were replicated in each subsample, with two notable exceptions. Among those who intended to change their anxiety after a psychedelic experience, the regression analyses (Suppl. Table 3) showed that intensity of mystical effects was not significantly associated with changes in anxiety (contrary to H1). Furthermore, in the path analysis (Suppl. Figure 3), intensity of mystical effects was not significantly associated with increases in psychological flexibility (contrary to H2), nor were there indirect relationships between acute mystical effects and decreases in anxiety via increases in psychological flexibility. However, all other findings showed that our models were identical regardless of whether one intended to change their depression/anxiety or had a spontaneous or intended change in these conditions.
Discussion
The present retrospective cross-sectional survey study examined whether psychedelic occasioned mystical-type or psychological insight experiences predicted decreases in depression and anxiety following a psychedelic experience (H1), acute psychedelic effects predicted increases in psychological flexibility (H2), increases in psychological flexibility predicted decreases in depression/anxiety, (H3) and whether increases in psychological flexibility mediated the relationships between acute psychedelic effects and decreases in depression and anxiety symptoms (H4). Findings from our regression and path analysis models supported each of these hypotheses. Consistent with prior studies (Griffiths et al., 2016; Ross et al., 2016; Davis et al, 2019), in the present study mystical experiences were associated with decreases in depression and anxiety. Importantly, these observations were extended by showing that experiences of psychological insight during a psychedelic experience are also associated with decreases in depression and anxiety. Further, when mystical and psychological insight effects were included simultaneously as predictors of changes in our models, results showed that psychological insight stands out as a more robust predictor of change, as evidenced by the larger direct (Insight: β=.46 versus Mystical: β=.09) and indirect (Insight: β=.29 versus Mystical: β=.06) coefficients in the path analysis.
That psychological insight is strongly related to decreases in depression and anxiety is perhaps not surprising given the history of insight-oriented therapies (Connolly Gibbons et al., 2007), but it has also been questioned whether gaining insight is sufficient in and of itself to produce lasting changes in behavior or mental health functioning (Kuncewicz, Lachowicz-Tabaczek, and Zaluski, 2014; Leichsenring et al., 2006). To this point, our models also showed that psychological insight was predictive of change when accounting for the correlation between insight and mystical experiences. Insightful as well as mystical-type experiences have been identified as subtypes of the phenomenon of quantum change, which refers to a sudden, distinctive, benevolent, and enduring experience resulting in personal transformations that affect a broad range of personal emotions, cognitions and behaviors (Miller and C’de Baca, 2001). Such experiences after taking a psychedelic have also been implicated in decreases in alcohol use among individuals with alcohol use disorder (Garcia-Romeu et al., 2019).
Furthermore, findings from the present study underscore a potential explanation for how acute psychedelic experiences, including gaining psychological insight and mystical experiences, may exert such changes. Specifically, we demonstrated the importance of increases in psychological flexibility as a mediator of the positive therapeutic effects. Although several other mechanisms have been proposed at various levels of functioning, from changes in the entropy of brain network connectivity (Carhart-Harris et al., 2014) to the importance of awe/ego dissolution (Hendricks, 2018; Preller & Vollenweider, 2018), findings from this study are consistent with evidence demonstrating that psychedelic effects are associated with changes in psychological flexibility among a small sample of subjects who use the psychedelic ayahuasca (Kuypers et al., 2016), and research showing that increases in psychological flexibility is associated with positive depression and anxiety outcomes (Twohig & Levin, 2017).
Although the exploration of potential mediators of psychedelic effects on therapeutic outcomes is in its early stages, if psychological flexibility emerges as a consistent and robust mediator of effects in prospective clinical trials, then the field of psychedelic-assisted psychotherapy should consider integrating psychedelic administration with contextual behavioral therapies (e.g., ACT; Hayes et al., 2006) or other therapies designed to target psychological flexibility. Such therapies are designed to enhance processes of change by supporting increases in psychological flexibility which could be enhanced through the administration of a psychedelic. Moreover, it is possible that some acute psychedelic effects overlap with the core processes of the ACT model of psychopathology (Hayes et al., 2006). For example, consistent with the core processes of ACT, qualitative analysis of first-hand accounts of tobacco smokers in a clinical trial examining the effect of psilocybin-assisted therapy (Noorani et al., 2018; Johnson et al., 2014), suggested that their psychedelic experiences helped them see themselves in the context of their addiction (i.e., self as context), realize that they are not the labels (e.g., smoker) which they previously identified as (i.e., defusion), understood their values more clearly than before (i.e., values), and connected with the fullness of the present moment and their experience of it (i.e., contact with the present moment). Although not highlighted in the qualitative reports per se, another component of the ACT model, committed action, was demonstrated in the clinical trial by the high rates (80%) of biologically verified abstinence at 6 months post-treatment (Johnson et al., 2014). These data suggest that psychedelics appear to occasion both mindfulness/acceptance processes as well as commitment and behavior change processes. However, more research is needed to systematically investigate these processes in rigorous longitudinal trials among individuals with depression or anxiety in order to replicate these findings in this population.
This study has several limitations. Internet-based recruitment and data collection procedures were anonymous. Although this likely increased participation from individuals from a variety of geographical locations, it would have excluded people who prefer not to participate in research conducted on the internet. Further, a limitation of survey methods is that all reports are retrospective, increasing the likelihood that current affect and personality bias could influence recollection of subjective psychedelic experiences as well as depression and anxiety symptoms that were experienced many years ago. However, this potential confound is not expected to be more or less than similar confounds in other retrospective survey research (Davis et al., 2018; Davis et al, 2019). Additionally, the parent study from which the data were drawn, was designed to investigate the acute effect of gaining insight during a psychedelic experience. Although the mean score of the intensity of mystical experiences in this sample was similar to prior studies (Davis et al., 2018), suggesting comparably strong mystical effects in addition to insight effects, we cannot rule out the possibility that recruiting people who specifically reported gaining insight as part of a psychedelic experience accounts for some of the differential strength in the association between acute insight and other study variables.
Another limitation to this study is that, despite our efforts to recruit individuals with diverse backgrounds by placement of notices on a variety of internet forums, respondents were primarily young, white, and male. Although our sample is consistent with prior studies of psychedelic users using similar recruitment procedures (Davis et al., 2018; Barret et al., 2016), similar to Michaels et al. (2018) we strongly encourage future researchers to continue efforts in recruiting a diverse sample. There are several possible explanations for the lack of diverse representation in psychedelic survey studies. For example, it could be that the topic of these studies are not interesting to some potential respondents, that there is a perceived risk involved with reporting an illegal behavior, or that the internet computer format excluded individuals from differing socio-economic backgrounds. Efforts to overcome these factors could include a community-based participatory research methodology (Israel et al., 2005), wherein the study is designed through engagement with leaders from a variety of diverse backgrounds, with the intention of better understanding the ways in which the study can be designed to connect with individuals from these communities.
Conclusion
The findings from the present study highlight the role of psychological flexibility as a mediator of acute psychedelic effects and depression/anxiety outcomes. Future studies should examine the effect of psychedelic drug administration on psychological flexibility in a laboratory setting using a controlled trial design in order to ascertain the causal influences of psychological processes that predict therapeutic effects of hallucinogens. Such work should include measurement of the core processes of ACT (e.g., defusion, values, self as context, etc.) in order to examine whether changes in these core processes occur and predict enduring effects of psychedelic substances on therapeutic outcomes. If psychological flexibility continues to be shown to mediate positive therapeutic outcomes, future research should explore whether such therapeutic effects can be further enhanced by using a psychotherapeutic approach to psychedelic-assisted therapy that specifically targets processes of change within a transdiagnostic psychological flexibility model.
Supplementary Material
Highlights.
Acute psychedelic effects are related to changes in depression/anxiety
Changes in psychological flexibility fully mediate this relationship
Psychological flexibility should be examined in clinical trials with psychedelics
Acknowledgments
Financial Support: Effort for the authors was provided by NIH grants RO1DA03889 and T32DA07209, and from support from Tim Ferriss, Matt Mullenweg, Craig Nerenberg, Blake Mycoskie, and the Stephen and Alexandra Cohen Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interests: Dr. Griffiths is a board member of Heffter Research Institute and Dr. Davis is a board member of Source Research Foundation. Neither organization was involved in the design/execution of this study or the interpretation or communication of findings.
References
- A-Tjak JGL, Davis ML, Morina N, Powers MB, Smits JAJ, & Emmelkamp PMG (2015). A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychotherapy & Psychosomatics, 84, 30–36. [DOI] [PubMed] [Google Scholar]
- Araújo AM, Carvalho F, Bastos M de L, Guedes de Pinho P, & Carvalho M (2015). The hallucinogenic world of tryptamines: an updated review. Archives Of Toxicology, 89, 1151–1173. [DOI] [PubMed] [Google Scholar]
- Bandelow B, & Michaelis S (2015). Epidemiology of anxiety disorders in the 21st century. Dialogues In Clinical Neuroscience, 17, 327–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett FS, Johnson MW, & Griffiths RR (2015). Validation of the revised Mystical Experience Questionnaire in experimental sessions with psilocybin. Journal of Psychopharmacology, 29, 1182–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett FS, Bradstreet MP, Leoutsakos J-MS, Johnson MW, & Griffiths RR (2016). The Challenging Experience Questionnaire: Characterization of challenging experiences with psilocybin mushrooms. Journal of Psychopharmacology, 30, 1279–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum HG, Kessler RC, Kelley D, Ben-Hamadi R, Joish VN, & Greenberg PE (2010). Employer burden of mild, moderate, and severe major depressive disorder: mental health services utilization and costs, and work performance. Depression & Anxiety (1091–4269), 27, 78–89. [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, … Zettle RD (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42, 676–688. [DOI] [PubMed] [Google Scholar]
- Carhart-Harris RL, Bolstridge M, Rucker J, Day CMJ, Erritzoe D, Kaelen M, … Nutt DJ (2016). Psilocybin with psychological support for treatment-resistant depression: An open-label feasibility study. The Lancet Psychiatry, 3, 619–627. [DOI] [PubMed] [Google Scholar]
- Carhart-Harris RL, Williams TM, Sessa B, Tyacke RJ, Rich AS, Feilding A, & Nutt DJ (2011). The administration of psilocybin to healthy, hallucinogen-experienced volunteers in a mock-functional magnetic resonance imaging environment: A preliminary investigation of tolerability. Journal of Psychopharmacology, 25, 1562–1567. [DOI] [PubMed] [Google Scholar]
- Carhart-Harris RL, Leech R, Hellyer PJ, Shanahan M, Feilding A, Tagliazucchi E, … Nutt D (2014). The entropic brain: A theory of conscious states informed by neuroimaging research with psychedelic drugs. Frontiers in Human Neuroscience, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris RL, Roseman L, Bolstridge M, Demetriou L, Pannekoek JN, Wall MB, . . . Nutt DJ (2017). Psilocybin for treatment-resistant depression: FMRI-measured brain mechanisms. Scientific Reports, 7, 13187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins KA, Westra HA, Dozois DJA, & Burns DD (2004). Gaps in accessing treatment for anxiety and depression: Challenges for the delivery of care. Clinical Psychology Review, 24, 583–616. [DOI] [PubMed] [Google Scholar]
- Collimore KC, & Rector NA (2014). Treatment of anxiety disorders with comorbid depression: A survey of expert CBT clinicians. Cognitive and Behavioral Practice, 21, 485–493. [Google Scholar]
- Connolly Gibbons MB, Crits-Christoph P, Barber JP, & Schamberger M (2007). Insight in psychotherapy: A review of empirical literature In Castonguay L & Hill C (Eds.), Insight in psychotherapy (pp. 143–165). Washington, DC: APA Press. [Google Scholar]
- Coull G, & Morris PG (2011). The clinical effectiveness of CBT-based guided self-help interventions for anxiety and depressive disorders: A systematic review. Psychological Medicine, 41, 2239–2252. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, & Reynolds CF III. (2014). Adding psychotherapy to antidepressant medication in depression and anxiety disorders: A meta-analysis. World Psychiatry, 13, 56–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis AK, Barsuglia JP, Lancelotta R, Grant R & Renn E (2018). The epidemiology of 5-Methoxy-N,N-Dimethyltryptamine (5-MeO-DMT) use: Benefits, consequences, patterns of use, subjective effects, and reasons for consumption. Journal of Psychopharmacology, 32, 779–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis AK, So S, Lancelotta R, Barsuglia JP, & Griffiths RR (2019). 5-Methoxy-N,N-Dimethyltryptamine (5-MeO-DMT) used in a naturalistic setting is associated with unintended improvements in depression and anxiety. The American Journal of Drug and Alcohol Abuse, 45, 161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- dos Santos RG, Osorio FL, Crippa JAS, Riba J, Zuardi AW, & Hallak JEC (2016). Antidepressive, anxiolytic, and antiaddictive effects of ayahuasca, psilocybin, and lysergic acid diethylamide (LSD): a systematic review of clinical trials published in the last 25 years. Therapeutic Advances in Psychopharmacology, 6, 193–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French K, Golijani-Moghaddam N, & Schroder T (2017). What is the evidence for the efficacy of self-help acceptance and commitment therapy? A systematic review and meta-analysis. Journal of Contextual Behavioral Science, 6, 360–374. [Google Scholar]
- Garcia-Romeu A, Davis AK, Erowid F, Erowid E, Griffiths RR, & Johnson MW (2019). Cessation and reduction in alcohol consumption and misuse after psychedelic use. Journal of Psychopharmacology. [DOI] [PubMed] [Google Scholar]
- Gloster AT, Meyer AH, & Lieb R (2017). Psycholiogical flexibility as a malleable public health target: Evidence from a representative sample. Journal of Contextual Behavioral Science, 6, 166–171. [Google Scholar]
- Griffiths RR, Richards W, Johnson M, McCann U, & Jesse R (2008). Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later. Journal of Psychopharmacology, 22, 621–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths RR, Johnson MW, Richards WA, Richards BD, McCann U, & Jesse R (2011). Psilocybin occasioned mystical-type experiences: Immediate and persisting dose related effects. Psychopharmacology, 218, 649–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths RR, Johnson MW, Carducci MA, Umbricht A, Richards WA, Richards BD, … Klinedinst MA (2016). Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. Journal of Psychopharmacology, 30, 1181–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker T, Stone P, & MacBeth A (2016). Acceptance and commitment thearpy – Do we know enough? Cumulative and sequential meta-analyses of randomized controlled trials. Journal of Affective Disorders, 190, 551–565. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, & Lillis J (2006). Acceptance and Commitment Therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44, 1–25. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, & Wilson KG (2012). Acceptance and commitment therapy: The process and practice of mindful change, 2nd ed. New York, NY: Guilford Press. [Google Scholar]
- Hendricks PS (2018). Awe: a putative mechanism underlying the effects of classic psychedelic-assisted psychotherapy. International Review Of Psychiatry (Abingdon, England), 30, 331–342. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, & Fang A (2012). The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognitive Therapy Research, 36, 427–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corp IBM. (2018). IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. [Google Scholar]
- Israel BA , Eng E , Schulz AJ , & Parker EA (2005). Methods in community-based participatory research for health. San Francisco: Jossey-Bass. [Google Scholar]
- Johnson MW, Garcia-Romeu A, Cosimano MP, & Griffiths RR (2014) Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. Journal of Psychopharmacology, 28, 983–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW & Griffiths RR (2017). Potential Therapeutic Effects of Psilocybin. Neurotherapeutics, 14, 734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Garcia-Romeu A, Johnson PS, & Griffiths RR (2017). An online survey of tobacco smoking cessation associated with naturalistic psychedelic use. Journal of Psychopharmacology, 31, 841–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB & Rottenberg J (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30, 865–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon WJ (2011). Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues in Clinical Neuroscience, 13, 7–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koen N & Stein DJ (2011). Pharmacotherapy of anxiety disorders: a critical review. Dialogues in Clinical Neuroscience, 13, 423–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuncewicz D, Lachowicz-Tabaczek K, & Zaluski J (2014) Why insight in psychotherapy does not always lead to behaviour change? Polish Journal of Applied Psychology, 12, 99–122. [Google Scholar]
- Kuypers KPC, Riba J, de la Fuente Revenga M, Barker S, Theunissen EL, & Ramaekers JG (2016). Ayahuasca enhances creative divergent thinking while decreasing conventional convergent thinking. Psychopharmacology, 223, 3395–3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leichsenring F, Hiller W, Weissberg M, & Leibing E (2006). Cognitive-behavioral therapy and psychodynamic psychotherapy: techniques, efficacy, and indications. American Journal of Psychotherapy, 60, 233–259 [DOI] [PubMed] [Google Scholar]
- Lovibond PF & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behavior Research and Therapy, 33, 335–343. [DOI] [PubMed] [Google Scholar]
- Maclean KA, Leoutsakos J-MS, Johnson MW, & Griffiths RR(2012). Factor Analysis of the Mystical Experience Questionnaire: A Study of Experiences Occasioned by the Hallucinogen Psilocybin. Journal of the Scientific Study of Religion, 51, 721–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaels TI, Purdon J, Collins A, & Williams MT (2018). Inclusion of people of color in psychedelic-assisted psychotherapy: a review of the literature. BMC Psychiatry, 18, 245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, (2004). The phenomenon of quantum change. Journal of Clinical Psychology, 60, 453–460. [DOI] [PubMed] [Google Scholar]
- Miller WR & C’de Baca J, (2001). Quantum change: When epiphanies and sudden insights transform ordinary lives. Guilford Press. [Google Scholar]
- Muthén LK and Muthén BO 1998-2017. Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén and Muthén [Google Scholar]
- Niles AN, Dour HJ, Stanton AL, Roy-Byrne PP, Stein MB, Sullivan, … Craske MG (2015). Anxiety and depressive symptoms and medical illness among adults with anxiety disorders. Journal of Psychosomatic Research, 78, 109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noorani T, Garcia-Romeu A, Swift TC, Griffiths RR, & Johnson MW (2018). Psychedelic therapy for smoking cessation: Qualitative analysis of participant accounts. Journal of Psychopharmacology, 32, 756–769. [DOI] [PubMed] [Google Scholar]
- Otto MW, & Hearon BA (2016). Combination treatment for anxiety and mood disorders: Benefits and issues for the combination of cognitive-behavioral therapy and pharmacotherapy In: The Oxford handbook of cognitive and behavioral therapies. New York, NY: Oxford University Press; p. 482–493. [Google Scholar]
- Palhano-Fontes F, Barreto D, Onias H, Andrade KC, Novaes MM, Pessoa JA, … Araujo DB (2018). Rapid antidepressant effects of the psychedelic ayahuasca in treatment-resistant depression: a randomized placebo-controlled trial. Psychological Medicine, 49, 655–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preller KH, & Vollenweider FX (2018). Phenomenology, Structure, and Dynamic of Psychedelic States. Current Topics In Behavioral Neurosciences, 36, 221–256. [DOI] [PubMed] [Google Scholar]
- Roseman L, Nutt DJ, & Carhart-Harris RL (2018). Quality of acute psychedelic experience predicts therapeutic efficacy of psilocybin for treatment-resistant depression. Frontiers in Pharmacology, 8, 974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross S, Bossis T, Guss J, Agin-Liebes G, Malone T, Cohen B, … Schmidt BL (2016). Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. Journal of Psychopharmacology, 30, 1165–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabucedo P (2017). The psychological flexibility model from a cultural perspective: an interpretive analysis of two Native American healing rituals. Internaltional Journal of Culture and Mental Health, 10, 367–375. [Google Scholar]
- Santos RG, Landeira-Fernandez J, Strassman RJ, Motta V, & Cruz APM (2007). Effects of ayahuasca on psychometric measures of anxiety, panic-like, and hopelessness in Santo Daime members. Journal of ethnopharmacology, 112, 507–513. [DOI] [PubMed] [Google Scholar]
- Sinyor M, Schaffer A, & Levitt A (2010). The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Trial: A Review. Canadian Journal of Psychiatry, 55, 126–135. [DOI] [PubMed] [Google Scholar]
- Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, & Silove D (2014). The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. International Journal of Epidemiology, 43, 476–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud JB, Freeman TP, Leech R, Hindocha C, Lawn W, Nutt DJ, Curran HV, & Carhart-Harris RL (2017). Psilocybin with psychological support improves emotional face recognition in treatment-resistant depression. Psychopharmacology, 235, 459–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twohig MP & Levin ME (2017). Acceptance and Commitment Therapy as a treatment for anxiety and depression: A review. Psychiatric Clinics of North America, 40, 751–770. [DOI] [PubMed] [Google Scholar]
- Uthaug MV, van Oorsouw K, Kuypers KPC, van Boxtel M, Broers NJ, Mason NL, … Ramaekers JG (2018). Sub-acute and long-term effects of ayahuasca on affect and cognitive thinking style and their association with ego dissolution. Psychopharmacology, 235, 2979–2989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh Z & Thiessen MS (2018). Psychedelics and the new behaviourism: considering the integration of third-wave behavior therapies with psychedelic-assisted therapy. International Review of Psychiatry, 30, 343–349. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.