Abstract
Alexithymia and dissociation have been consistently linked in the literature, particularly in psychiatric populations. Both arise from a disconnection between conscious aspects of self-experiences and perceptions at both the mental self and bodily levels. This results in difficulty integrating thoughts, feelings and experiences into consciousness and memory, negatively impacting emotion awareness/regulation and reflective functioning. We conducted a meta-analysis to examine the strength of the relationship between alexithymia and dissociation in both clinical and non-clinical populations. Studies using two common measures of these constructs were included (i.e., the Toronto Alexithymia Scale - TAS, and the Dissociative Experiences Scale - DES). Analyzing the effect sizes derived from 19 studies (including a total of 4664 participants) revealed moderate to strong relationships between alexithymia and dissociation. The strength of the association was higher in clinical and younger aged non clinical populations. These findings are discussed in the context of treatment recommendations..
Key words: Alexithymia, Dissociation, Meta-analysis
Introduction
Alexithymia involves a diminished capacity to process emotional experiences, difficulties distinguishing between emotions and bodily sensations, difficulties identifying and verbally describing emotions, and an externally oriented thinking style (Taylor, Bagby, & Parker, 1997). It is thought that emotion awareness develops over time, with young children mainly experiencing the physical sense of emotions, and with the help of caregivers, they learn to mentally identify and verbally name affects. This normal developmental process can be disrupted if caregivers are non-empathetic or unresponsive (Schimmenti, 2016). Higher levels of alexithymia are observed in the context of invalidating or abusive environments where children learn that communicating emotional experiences is inappropriate, ineffective or potentially dangerous (Aust, Härtwig, Heuser, & Bajbouj, 2013; Paivio & McCulloch, 2004).
Alexithymia has been linked with dysfunctional methods of affect regulation (i.e., avoidant defenses such as conscious and deliberate avoidance of distressing wishes, feelings or experiences, unconscious dissociating when distressed, and trouble recalling distressing events or unpleasant experiences), as well as primitive defense styles such as projection and denial (Parker, Taylor & Bagby, 1998; Taylor, Bagby, & Parker, 1997; Meganck, Vanheule, & Desmet, 2013). These patterns of emotion modulation further disrupt the capacity to map internal emotional experiences and limit awareness of wishes and needs signaled through emotions.
Alexithymia places individuals at risk for a range of psychiatric illnesses including psychotic, mood and anxiety disorders (Frewen, Dozois, Neufeld, & Lanius, 2008; Li, Zhang, Guo & Zang, 2015; Westwood, Kerr-Gaffney, Stahl, & Tchanturia, 2017), and may negatively influence treatment expectations and responsiveness (Evren et al., 2008). Difficulty identifying feelings appears to be the strongest predictor of negative outcomes, supporting the underlying importance of emotion awareness in the regulation of psychological stress (Grabe et al., 2008; Ogrodniczuk, Piper, & Joyce, 2011; Terock et al., 2017; Terock et al., 2015).
Dissociation constitutes an altered state of consciousness characterized by separation of sensation, emotions and cognition. Dissociation can vary from normal experience (e.g., absorption/day dreaming) to severe pathology characterized by detachment from body and/or reality (e.g., Dissociative Identity Disorder). A higher rate of pathological dissociation is found in populations exposed to childhood trauma, particularly those with resulting attachment anxiety, and in psychiatric samples (Rafiq, Campodonico, & Varese, 2018; Dalenberg et al., 2012; Kong, Kang, Oh & Kim, 2018; Lyssenko et al., 2017). Attachment anxiety typically results when caregivers are inconsistent and unpredictable; thus are not attuned or responsive to the child’s emotions. Dissociation yields both positive and negative symptoms. In the positive state, emotions, sensations, and perceptions are overly present in that prior traumatic events are re-experienced, while in the negative symptomatic state, these components are reduced or even absent. Negative dissociation modulates extreme affect in response to perceived inescapable threat. Thus, pathological or more severe negative dissociation has been considered an automatic defense mechanism against intolerable or overwhelming negative emotions, and as a way to unconsciously disconnect from one’s identity or perception. As such, negative dissociation (similar to alexithymia) inhibits the capacity to integrate emotions into conscious experience.
Dissociation is commonly seen in many mental health disorders and is considered a difficult symptom to treat (Lyssenko et al., 2017). Disconnection from emotional experiences can limit treatment outcomes or delay treatment response, as capacity for emotional processing is an important factor for treatment effectiveness (Arntz, Stupar-Rutenfrans, Bloo, van Dyck & Spinhoven, 2015; Groves, Douglas, & Porter, 2018; Jepson, Langeland, & Heir, 2014; Kleindienst et al., 2011; Prasko et al., 2016; Spitzer, Barrow, Freyberger, & Grabe, 2007; Rufer et al., 2006). The relationship between dissociation and treatment outcomes remains even after baseline level of pretreatment psychopathology are controlled (Kleindienst et al., 2011).
The linking mechanisms between alexithymia and negative dissociation are still under debate; however, both appear to be related to the experience of developmental trauma, with trauma potentially playing a mediating role between the two (Craparo et al., 2014). According to Bucci’s (1997) multiple code theory of emotion processing, there are two primary components of emotion schema, sensory/visceral sensation with motoric urges, and symbolic representations (images and words). These are bodily and psychological phenomena. When these components do not link, the integration between cognition and emotion is hindered (i.e., alexithymia occurs). With dissociation, there is a psychological disconnection between aspects of self-experiences and perceptions (i.e., part of one’s psychic functioning seems to operate independently from other parts) that limits the integration of cognition and emotion. Thus alexithymia may more strongly reflect a capacity deficit, while dissociation may constitute a psychological mechanisms of invasive defense to cope with high arousal and overwhelming feelings or unbearable states of mind (Schimmenti & Caretti, 2014). Ultimately, both alexithymia and dissociation limit the ability to modulate affective processes via cognitive processes, negatively impacting experiencing, interpretation, and regulation of emotions.
Alexithymia and dissociation are considered dimensional constructs; they exist on a continuum from nonpathological to pathological. Non pathological levels of alexithymia (e.g. reduced emotion clarity) and dissociation (e.g., absorption) occur in the normal population (Evren, et al., 2008; de Ruiter, Elzinga & Phaf, 2006). Pathological or more severe levels of alexithymia and dissociation are more likely to exist in clinical populations with a history of childhood trauma (Kefeli, Turow, Yildirim & Boysan, 2018). Research suggests a strong relationship between alexithymia and dissociation, particularly in clinical populations (New et al., 2012; Zorzella, Muller, Cribbie, Brambah, & Classen, 2019).
The purpose of this study was to complete a meta-analytic review examining the strength of the association between alexithymia and negative dissociation in both clinical and nonclinical populations. We hypothesized that the strength of the relationship between alexithymia and dissociation would differ between clinical and nonclinical groups, with a stronger association anticipated in individuals with psychiatric disorders.
Methods
Literature Search
A literature search was conducted on all published studies examining the association between alexithymia and dissociation. Due to the heterogeneity in how these constructs are conceptualized and assessed, only studies employing two commonly used measures were included: Toronto Alexithymia Scale (TAS) and Dissociative Experiences Scale I or II(DES or DES II). Retrieved data was cross-sectional in nature.
A computer search on PsycINFO was completed using the search terms: i) alexithymia and dissociation, ii) alexithymia and dissociative, iii) alexithymia and depersonalization, and iv) alexithymia and derealization. To be included in the meta-analysis, studies had to meet the following criteria: i) the sample populations were adults (mean age over age 18 years), ii) the study examined the association between the TAS and the DES or DES-II, and reported the strength of this association in the article, iii) studies were published in a peer reviewed journal, and iv) studies were written in the English language. Studies mixing clinical and non-clinical samples in the analysis were excluded. Two raters independently coded the data. Disagreements were resolved through discussion and by seeking further information as needed (Figure 1).
Toronto Alexithymia Scale (Bagby, Parker, & Taylor, 1994)
Currently, the most widely used measure of alexithymia is the 20-item Toronto Alexithymia Scale (TAS- 20). The TAS asks participants to rate on a 5-point likert scale (ranging from 1 = never true, to 5 = very often true) the degree to which they agree with each statement. The English language version of this self-report scale has a three-factor structure that corresponds to the theoretical construct of alexithymia: Difficulty Identifying Feelings (DIF) (e.g., I am often confused about what I am feeling), Difficulty Describing Feelings (DDF) (e.g., it is difficult for me to find the right words for what I am feeling), and Externally Oriented Thinking (EOT) (e.g., I prefer to talk to people about their daily activities rather than their feelings). DIF refers to problems distinguishing between emotions and bodily sensations, as well as difficulties distinguishing between different emotions. DDF concerns the inability to verbally express emotions to others. EOT denotes an impoverished imaginative life marked by concrete and poor introspective thinking.
The factorial validity and reliability of the dimensions ‘identifying feelings’ (DIF) and ‘describing feelings’ (DDF) has been replicated in many studies; however, the subscale EOT appears to be unreliable. The dimensions ‘identifying feelings’ and describing feelings’ have been found to collapse into one single factor (Kooiman, Spinhoven, & Trijsburg, 2002; Precce, Becerra, Robinson & Dandy, 2018). As a result, use of the EOT subscale as a measure of alexithymia is not recommended, and alexithymia may not be well-represented by the global severity score (Haviland & Reise, 1996). Based on these findings, we used the DIF subscale as a measure of alexithymia when available (and the total TAS score when not).
Dissociative Experiences Scale I and II (Carlson & Putnam, 1993)
By far, the most commonly used psychometric instrument for the assessment of dissociative experience is the Dissociative Experiences Scale (DES). The DES is a selfrating instrument comprising 28 items that builds on the assumption of a “dissociative continuum” ranging from mild normative (i.e., absorption), to severe pathological dissociation. Subjects are asked to make slashes on 100- mm lines to indicate where they fall on a continuum for questions on experiences of absorption, depersonalization, derealization and amnesia (e.g., “some people have the experience of driving a car and suddenly realizing that they don’t remember what has happened during all or part of the trip, mark the line to show what percentage of time this happens to you”). As the scoring procedure of the continuous scale was time consuming, a revised version of the scale (DES-II) uses an 11-point Likert scale ranging from 0 to 100.
Meta-analyses
Meta-analyses were conducted to examine the association between alexithymia and dissociation. All identified studies meeting inclusion criteria were included. The characteristics of these studies are detailed in Tables 1, 2 and 3. The meta-analyses were performed using the Meta- Essentials Program (Suurmond, van Rhee & Hak, 2017). The studies were weighed by sample size. Heterogeneity of effect sizes was assessed using the I² test. The I² test examines the percentage of observed variance which is accounted for by true heterogeneity rather than chance, with 0% to 40% representing ‘might not be important’, 30-60% ‘may represent moderate heterogeneity’, 50-90% ‘may represent substantial heterogeneity’ and 75%-100% ‘considerable heterogeneity’ (Higgins et al., 2019). The effect size calculations were based on correlation coefficients. Standardized effect sizes were classified as follows: 0-0.1 insubstantial, 0.1-0.3 small, 0.3-0.5 moderate, and 0.5-1.0 large (Cohen, 1988).
Results
Forest plots examining correlations between dissociation and alexithymia in clinical and nonclinical populations (correlations and confidence intervals) are displayed in Figures 1 and 2.
Table 4 summarize the results of the meta-analyses. This table lists the number of studies that examined the association between TAS and DES, the number of participants included in each meta-analysis, the mean weighted effect size for each association, and the results of the heterogeneity of effect sizes I² test. A fail-safe N value is also reported. Failsafe N’s estimate the total number of unpublished studies with nonsignificant findings that would need to exist for the overall mean effect size to become nonsignificant.
The meta-analysis examining the relationship between alexithymia and dissociation in clinical populations showed a large effect size (r = .56). The result of this meta-analysis was initially heterogeneous. Examination of the data revealed that the heterogeneity was due to an outlying value in one of the studies (Zlotnick et al., 1996). This study included female inpatients admitted to a psychiatric unit (77% reporting a history of self-injury in the previous 3 months). The association between alexithymia and dissociation in this study population was much lower than the other samples (r = .13). This could potentially be related to a higher level of emotion dysregulation in this population and may reflect a group of individuals who are more inclined to display positive symptoms of dissociation such as ‘re-experiencing’ (i.e., with self-injurious acts employed to reduce excessive arousal) in contrast to negative dissociate mechanisms involving a disconnection between conscious aspects of self-experiences and perceptions). A meta-analysis examining the relationship between alexithymia and dissociation in nonclinical populations was also initially heterogeneous. When nonclinical populations were separated into samples of young adults versus general population samples with a higher mean age the results were homogeneous. The mean effect size for younger adults was higher than that of older adults (r = .41 versus r = .34).
Figure 1.
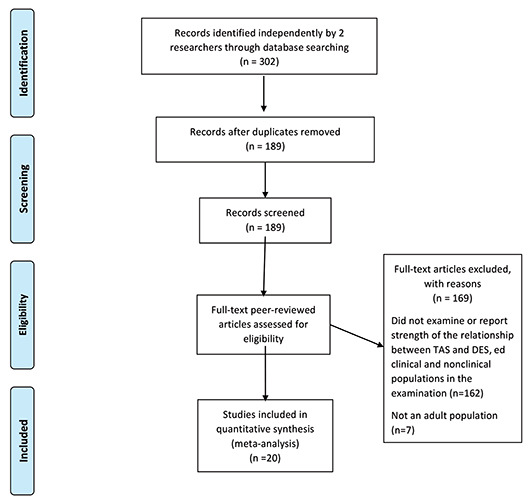
PRISMA Flow Diagram.
Figure 2.
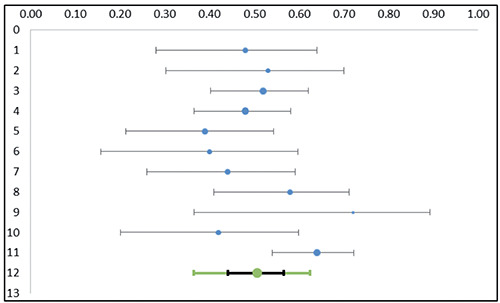
Forest plot examining correlations between dissociation and alexithymia in clinical populations (correlations and confidence intervals). Vertical numbers correspond to study numbers listed in Table 1.
Figure 3.
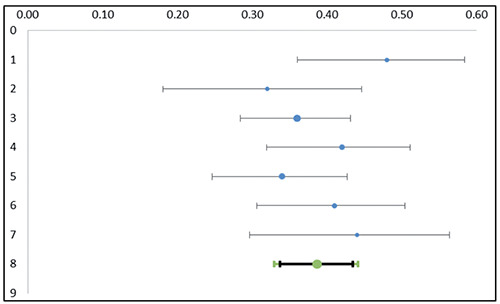
Forest plot examining correlations between dissociation and alexithymia in young adults, nonclinical population. Vertical numbers correspond to study numbers listed in Table 2.
Discussion
Alexithymia and dissociation have been consistently linked in the literature, particularly in psychiatric populations (New et al., 2012; Zorzella et al., 2019). Both result in a disconnection between conscious aspects of self-experiences and perceptions at both the mental self and bodily levels. This results in difficulty integrating thoughts, feelings and experiences into consciousness and memory, and can negatively impact emotion awareness/regulation and reflective functioning. We conducted a meta-analysis to examine the strength of the association between alexithymia and dissociation in both clinical and non-clinical populations. We anticipated a significant correlation between these factors. Analyzing the effect sizes derived from 19 studies (including 4664 participants) revealed a moderate to strong relationship between alexithymia and dissociation. The strength of the relationship between alexithymia and dissociation was highest in clinical populations, followed by and younger and then older nonclinical populations. decreased with advancing age in nonclinical populations. Previous study findings indicate dissociation in nonclinical populations is relatively stable or declines slightly over time, while alexithymia tends to increase with age which may explain the weaker association found in studies including older individuals (Baker et al., 2003; Marranen et al., 2008; Mattila, Salminen, Nummi, & Joukamaa, 2006; Onor, Trevisiol, Spano, Aguglia, & Paradiso, 2010).
Table 1.
Studies examining the relationship between alexithymia and dissociation in clinical populations.
| Study | Sample | N | Correlation and confidence intervals |
|---|---|---|---|
| 1. Berenbaum, Valera & Kerns, 2003 | European-American and African-American women aged 18-74 with schizotypal symptoms (mean age 38.7: SD 14.2) | 75 | .48¹ (.28-.64) |
| 2. Evren & Can, 2007 | Male soldiers from Turkey with conversion disorder (mean age 43.1: SD 9.5) | 55 | .53¹ (.30—.70) |
| 3. Evren et al., 2008 | Inpatients from Istanbul with alcohol use disorder (mean age 21.1:SD 2.0) | 176 | .52¹ (.40-.62) |
| 4. Evren, Cinar, & Evren, 2012 | Men from Istanbul with substance dependence admitted to an inpatient dependency treatment unit (mean age 35.4: SD 10.54) | 200 | .48¹ (.36-.58) |
| 5. Frewen et al., 2008 | Individuals from Canada with PTSD (88% female, mean age 38.7: SD 9.9) | 105 | .39² (.21-.54) |
| 6. Kienle et al., 2017 | Individuals from Germany with dissociative disorders (75% female, mean age 42.6: SD 12.3) | 60 | .40² (.16-.60) |
| 7. Majohr et al., 2011 | Individuals from Germany with panic disorder (62% female, mean age 35.2: SD 12.4) | 95 | .44¹ (.26-.59) |
| 8. New et al., 2012 | Individuals from the US with borderline personality disorder (67% female, mean age 34.8: SD 11.6) | 79 | .58² (.41-.71) |
| 9. O’Brien et al., 2015 | Individuals from Ireland diagnosed with psychogenic, non-epileptic seizures (47% with conversion disorder, 42% personality disorder and 10.5% other disorder) (68% female, mean age 30: SD 8.8) | 19 | .72² (.36-.89) |
| 10. Yilmaz et al., 2016 | Psychiatric patients from Istanbul with borderline personality disorder (32.9% female, mean age 34.7: SD 12.04) | 70 | .42¹ (.20-.60) |
| Zlotnick et al., 1996 | Female inpatients from the US admitted to a psychiatric unit (77% reporting a history of self-injury in the previous 3 months) (mean age 33: SD 9.23) | 148 | .13² (-0.03-0.29) |
| 11. Zorzella et al., 2019 | Canadian treatment seeking women with a history of childhood abuse (mean age 39.2: SD 11.5) | 167 | .64¹ (.54-.72) |
TAS Total = Toronto Alexithymia Scale Total; TAS DIF = Toronto Alexithymia Scale, Difficulty Identifying Feelings Subscale; Zlotnick et al., 1996 study was not included in the meta-analysis; Superscript 1 = DIF & superscript 2 = total TAS score.
Table 2.
Studies examining the relationship between alexithymia and dissociation in non-clinical populations (young adults).
| Study | Sample | N | Correlation and confidence intervals |
|---|---|---|---|
| 1. Alfasi and Soffer-Dudek, 2018 | Undergraduate students from Israel (70.6% female, mean age 23.4: SD 1.44) | 187 | 0.48¹ (0.36-0.58) |
| 2. Berenbaum & James, 1994 | Undergraduate students from the US (60.9% female, mean age 20.1: SD 1.3) | 180 | 0.32² (.18-0.45) |
| 3. De Berardis et al., 2009 | Female undergraduate students from Italy (mean age 22.5: SD 1.9) | 546 | .36¹ (.28-.43) |
| 4. Craparo et al., 2014 | Young adult flood victims from Italy (44.6% female, mean age 18.33: SD .68) | 287 | .42¹ (.32-.51) |
| 5. Mason, Tyson, Jones & Potts, 2005 | Undergraduate students From the UK (48.8% female, mean age 19.10: SD 2.4) | 371 | .34¹ (.25-.43) |
| 6. Modestin, Lötscher, & Erni, 2002 | Medical students from Switzerland (46.7% female, mean age 24.4: SD 3.0) | 276 | .41¹ (.31-.50) |
| 7. Schimmenti, Sideli, LaMarca, Gori, & Terrone, 2019 | Adult volunteers (56.8% female, mean age 25.7; SD 6.9) | 144 | .44² (.30-.56) |
TAS Total = Toronto Alexithymia Scale Total; TAS DIF = Toronto Alexithymia Scale, Difficulty Identifying Feelings subscale; Superscript 1 = DIF & superscript 2 = total TAS score.
Dissociation appears to be a relatively stable and unconsciously organized cognitive style of dealing with emotional conflict or impulses. With dissociation, information processing is impaired. As a result, social cues regarding potentially unhealthy or dangerous situations/relationships may be missed. These social cues normally trigger adaptive emotions such as fear and anxiety that aid in the identification of unsafe situations and signal the need for defensive behaviors. However, dissociation restricts healthy defensive responding by keeping unpleasant emotions and associated thoughts outside of conscious awareness (Zamir, Szepsenwol, Englund, & Simpson, 2018). Thus, a reliance on dissociation as a coping strategy that continues into adulthood may place individuals at risk for further re-victimization, and can maintain this defense (i.e., dissociation may perpetuate dissociation).
Research findings indicate a general age-related decline in emotion recognition capacities (i.e., sensitivity to internal emotional experiences decreases during the course of adult development) (Manenti, Brambilla & Cotelli, 2019). This may explain the observed increase in alexithymia with advancing age. However, individuals with elevated levels of alexithymia not only have a deficit in the cognitive processing of their emotions, they also have a less complex and integrated sense of self and others, contributing to relational difficulties and decreasing autonomy, environmental mastery and self-acceptance over time (Ziadni, Jasinski, Labouvie-Vief, & Lumley, 2017). This may compound the emotional processing deficits with a defensive component, further limiting capacities with advancing age.
Consistent with this hypothesis, Schimmenti (2016) recently examined the developmental roots of dissociation and alexithymia in individuals who experienced emotional neglect during childhood. He found support for a model linking reduced levels of theory of mind and higher levels of alexithymia with an over activation of dissociative processes. The author suggested that individuals who experience emotional neglect during childhood are likely to perceive distressful experiences as disorganizing, as their capacity to reflect on mental states and interpret emotions are less developed. As a result, they may learn to rely on dissociative or other defensive processes as a means to reduce intense negative arousal and affects.
Figure 4.
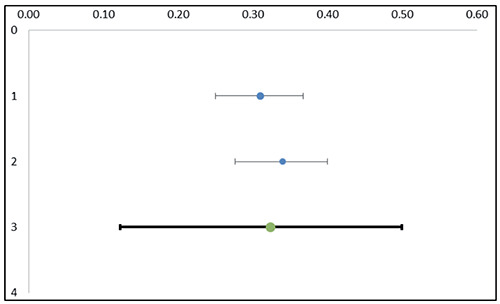
Forest plot examining correlations between dissociation and alexithymia in the general population. Vertical numbers correspond to study numbers listed in Table 2.
Table 3.
Studies examining the relationship between alexithymia and dissociation in non-clinical populations (general population).
| Study | Sample | N | Correlation and confidence intervals |
|---|---|---|---|
| 1. Lipsanen, Saarijärvi, & Lauerma, 2004 | Random sample from the population register of Finland (39.9% female, mean age 40.1: SD 12.6) | 924 | .31² (.25-.37) |
| 2. Schimmenti, 2016 | Recruited from five cities in Italy (54.9% females, mean age 35.8: SD 10.95) | 792 | .34² (.28-.40) |
TAS Total = Toronto Alexithymia Scale Total; TAS DIF = Toronto Alexithymia Scale, Difficulty Identifying Feelings subscale; Superscript 1 = DIF & superscript 2 = total TAS score.
Table 4.
Meta-analyses examining the association between alexithymia and dissociation in clinical and nonclinical samples (young adults and general population).
| # of Studies | Total N | Mean Weighted Effect Size (CI) | I² | Fail safe N | |
|---|---|---|---|---|---|
| Clinical Samples | 11 | 1101 | .56 (.49-.63) | 30.96% | 210 |
| Young Adults (nonclinical) | 6 | 1847 | .41 (.35-46) | 4.7% | 296 |
| General Population | 2 | 1716 | .34 (.03-.64) | 0.00% | 4127 |
Alexithymia and dissociation have been found to negatively impact treatment outcomes (Arntz et al., 2015; Corchs, et al., 2008; Jepson et al., 2014; Kleindienst et al., 2011; Prasko et al., 2016; Terock et al., 2017; Terock et al., 2015). Fortunately, both of these factors appear to be partly modifiable through specific psychotherapeutic interventions, although differential effects are observed depending on the nature of the treatment and time of outcome assessment (post-treatment versus follow-up) (Cameron, Ogrodniczuk, & Hadjipavlou, 2014; Cloitre, Perkova, Wang, & Lu, 2012; Da Silva, Vasco, & Watson, 2018). With regards to alexithymia, treatments that directly target this deficit (e.g., place therapeutic emphasis on identifying describing and understanding emotional states and associated bodily sensations) appear to more consistently result in positive outcomes (Cameron et al., 2014). This suggests that bodily experiences must be integrated with cognition to enhance therapeutic effectiveness.
Improvements in alexithymia from baseline or pretreatment levels is associated with improvements in dissociation at posttreatment (Zorzella et al., 2019). It is possible that when an individual becomes more aware of, and understands their emotional experiences, emotional dysregulation decreases. As a result, dissociative mechanism are less likely to be employed to dampen extreme arousal, and the individual is better able to use adaptive coping strategies to deal with dysregulation. Thus, treatments that sequence specific techniques (e.g., skill training to enhance distress tolerance and develop emotion awareness/regulation capacities, followed by narrative exposure and emotional processing work) may be more effective (Cloitre et al., 2012; Klein & Reyno, 2016; 2017; 2019). Additionally, individuals with alexithymia and dissociation often report maladaptive self and other schema arising from attachment ruptures and other developmental or relational traumas that hinder treatment progress (Saariaho, Saariaho, Mattila, Karukivi, & Joukamaa, 2015). To accelerate psychotherapeutic efforts, a conscious alliance and active engagement are required. This may be achieved by overcoming ambivalence through the deconstruction of maladaptive thinking patterns prior to, or in conjunction with developing more adaptive emotion processing skills.
Conclusions
The results of this meta-analytic review found a strong association between alexithymia and dissociation, particularly in clinical populations. This association will require confirmation employing other methods of measuring these constructs, as the strength of the observed relationship may have been inflated due to state-dependent responding (i.e., inclusion of only self-report measures). It is unclear from the findings, if or how, specific psychological comorbidities or trauma experiences influence the strength of this association. Additional longitudinal studies are required examining alexithymia and dissociation in a broader range of clinical populations to illuminate common mechanisms, and inform the development and evaluation of transdiagnostic and optimally sequenced treatments.
References
- Alfasi D., Soffer-Dudek N. (2018). Does alexithymia moderate the relation between stress and general sleep experiences? Pers Individual Differences 122:87-92. [Google Scholar]
- Arntz A., Stupar-Rutenfrans S., Bloo J., van Dyck R., Spinhoven P. (2015). Prediction of treatment discontinuation and recovery from Borderline Personality Disorder: Results from an RCT comparing Schema Therapy and Transference Focused Psychotherapy. Behav Res Ther 74:60-71. [DOI] [PubMed] [Google Scholar]
- Aust S., Härtwig E.A., Heuser I., Bajbouj M. (2013). The role of early emotional neglect in alexithymia. Psychological Trauma 5:225-32. [Google Scholar]
- Bagby R. M., Parker J. D. A., Taylor G. J. (1994). The twenty-item Toronto Alexithymia scale—I. Item selection and cross-validation of the factor structure. J Psychosomatic Res 38:23–32. [DOI] [PubMed] [Google Scholar]
- Baker D., Hunter E., Lawrence E., Medford N., Patel M., Senior C., Sierra M., Lambert M.V., Phillips M.L., David A.S. (2003). Depersonalisation disorder: Clinical features of 204 cases. British J Psychiatry 182:428–33. [PubMed] [Google Scholar]
- Berenbaum H., James T. (1994). Correlates and retrospectively reported antecedents of alexithymia. Psychosomatic Medicine, 56, 553-559. [DOI] [PubMed] [Google Scholar]
- Berenbaum H., Valera E. M., Kerns J.G. (2003). Psychological trauma and schizotypal symptoms. Schizophr Bull 29:143-52. [DOI] [PubMed] [Google Scholar]
- Bucci W. (1997). Psychoanalysis and Cognitive Science. A Multiple Code Theory. New York, NY: Guilford Press. [Google Scholar]
- Cameron K., Ogrodniczuk J., Hadjipavlou G. (2014) Changes in alexithymia following psychological intervention: A review. Harvard Rev Psychiatry 22:162-78. [DOI] [PubMed] [Google Scholar]
- Carlson E.B., Putnam F.W. (1993). An update on the Dissociative Experiences Scale. Dissociation: Progress in the Dissociative Disorders. Dissociation 6:6–27 [Google Scholar]
- Cloitre M., Petkova E., Wang J., Lu Lassell F. (2012). An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depression and Anxiety 29:709-17. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical Power Analysis for the Behavioral Sciences (2nd ed). New Jersey: Lawrence Erbaum. [Google Scholar]
- Corchs F., Corregiari F., Ferrão Y.A., Takakura T., Mathis M. E., Lopes A. C., Miguel E. C., Bernik M. (2008). Personality traits and treatment outcome in obsessive-compulsive disorder. Braz J Psychiatry 30:246-50. [DOI] [PubMed] [Google Scholar]
- Craparo G., Gori A., Mazzola E., Petruccelli I., Pellerone M., Rotondo G. (2014). Posttraumatic stress symptoms, dissociation and alexithymia in an Italian sample of flood victims. Neuropsychiatr Dis Treat 10:2281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Silva A.N., Vasco A.B., Watson J.C. (2018). Alexithymia and emotional processing: A longitudinal mixed methods research. Research in Psychotherapy: Psychopathology, Process and Outcome 21:40-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalenberg C.J., Brand B.L., Gleaves D.H., Dorahy M.J., Loewenstein R.J., Cardena E., Spiegel D. (2012). Evaluation of the evidence for the trauma and fantasy models of dissection. Psychological Bull 138:550-88. [DOI] [PubMed] [Google Scholar]
- De Berardis D., Serroni N., Campanella D., Carano A., Gambi F., Valchera A., Ferro F.M. (2009). Alexithymia and its relationships with dissociative experiences, body dissatisfaction and eating disturbances in a non-clinical female sample. Cognitive Ther Res 33:471-9. [Google Scholar]
- de Ruiter M.B., Elzinga B.M., Phaf R.H. (2006). Dissociation: Cognitive capacity or dysfunction? J Trauma Dissociation 7:115-34. [DOI] [PubMed] [Google Scholar]
- Evren C., Can S. (2007). Clinical correlates of dissociative tendencies in male soldiers with conversion disorder. Israel j Psychiatry Related Sci 44:33-9. [PubMed] [Google Scholar]
- Evren C., Cinar O., Evren B. (2012). Relationship of alexithymia and dissociation with severity of borderline personality features in male substance-dependent inpatients. Comprehensive Psychiatry 53:854-9. [DOI] [PubMed] [Google Scholar]
- Evren C., Sar V., Evren B., Semiz U., Dalbudak E., Cakmak D. (2008). Dissociation and alexithymia among men with alcoholism. Psychiatry Clin Neurosci 62:40-7. [DOI] [PubMed] [Google Scholar]
- Frewen P.A., Lanius R. L., Dozois D.J.A., Neufeld R.W.J., Pain C., Hopper J.W., Stevens T.K. (2008). Clinical and neural correlates of alexithymia in posttraumatic stress disorder. j Abnorm Psychol 117:171-81. [DOI] [PubMed] [Google Scholar]
- Frewen P., Dozois D., Neufeld R., Lanius R. (2008). Metaanalysis of alexithymia in posttraumatic stress disorder. j Traumatic Stress 21:243-6. [DOI] [PubMed] [Google Scholar]
- Grabe H. J., Frommer J., Ankerhold A., Ulrich C., Groger R., Franke G.H., Spitzer C. (2008). Alexithymia and outcome in psychotherapy. Psychother Psychosomatics 77:189-94. [DOI] [PubMed] [Google Scholar]
- Groves S., Douglas K., Porter R. (2018). A Systematic Review of Cognitive Predictors of Treatment Outcome in Major Depression. Frontiers in Psychiatry, 9:382. doi: 10.3389/fpsyt.2018.00382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haviland M.G., Reise S.P. (1996) Structure of the Twenty- Item Toronto Alexithymia Scale. J Pers Assess 66:116-25. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Thomas J. Chandler J. Cumpston M. Li T. Page M.J. Welch V.A., editors (2019). Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons. [Google Scholar]
- Jepson E.K.K., Langeland W., Heir T. (2014). Early traumatized inpatients high in psychoform and somatoform dissociation: Characteristics and treatment response. j Trauma Dissoc 15:572-87. [DOI] [PubMed] [Google Scholar]
- Kienle J., Rockstroh B., Bohus M., Fiess J., Huffziger S., Steffen-Klatt A. (2017). Somatoform dissociation and postraumatic stress syndrome – two sides of the same medal? A comparison of symptom profiles, trauma history and altered affect regulation between patients with functional neurological symptoms, and patients with PTSD. BMC Psychiatry 17:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kefeli M.C., Turow R.G., Yildirim A., Boysan M. (2018). Childhood maltreatment is associated with attachment insecurities, dissociation and alexithymia in bipolar disorder. Psychiatry Res 260:391-9. [DOI] [PubMed] [Google Scholar]
- Kinley J.L., Reyno S.M. (2019). The price of needing to belong: Neurobiology of working through attachment trauma. Psychodynamic Psychiatry 47:39-51. [DOI] [PubMed] [Google Scholar]
- Kinley J.L., Reyno S.M. (2017). Advancing Freud’s dream: A dynamic-relational neurobiologically informed approach to psychotherapy. Neuropsychoanal 19:127-42. [Google Scholar]
- Kinley J.L., Reyno S.M. (2016). Project for a scientific psychiatry: A neurobiologically informed, phasic, brain-based model of integrated psychotherapy. J Psychotherapy Integration 26:61-73. [Google Scholar]
- Kleindienst N., Limberger M.F., Ebner-Priemer U.W., Keibel-Mauchnik J-K., Dyer A., Berger M. (2011). Dissociation predicts poor response to dialectical behavioral therapy in female patients with borderline personality disorder. J Pers Disord 25:432-47. [DOI] [PubMed] [Google Scholar]
- Kong S.S., Kang D.R., Oh J.M., Kim N.H. (2018). Attachment insecurity as a mediator of the relationship between childhood trauma and adult dissociation. j Trauma Dissoc 19:214-31. [DOI] [PubMed] [Google Scholar]
- Kooiman C.G., Spinhoven P., Trijsburg R.W. (2002). The assessment of alexithymia: A critical review of the literature and a psychometric study of the Toronto Alexithymia Scale -20. j Psychosomatic Res 53:1083-90. [DOI] [PubMed] [Google Scholar]
- Li S., Zhang B., Guo Y., Zhang J. (2015). The association between alexithymia as assessed by the 20-item Toronto Alexithymia Scale and depression: A meta-analysis. Psychiatry Res 227(1):1-9. [DOI] [PubMed] [Google Scholar]
- Lipsanen T., Saarijärvi S., Lauerma H. (2004). Exploring the relations between depression, somatization, dissociation and alexithymia – Overlapping or independent constructs? Psychopathol 37:200-6. [DOI] [PubMed] [Google Scholar]
- Lyssenko L., Schmahl C., Bockhacker L., Vonderlin R., Bohus M., Kleindienst N. (2017). Dissociation in psychiatric disorders: A meta-analysis of studies using the Dissociative Experiences Scale. Am J Psychiatry 175: 37–46. [DOI] [PubMed] [Google Scholar]
- Meganck D., Vanheule S., Desmet M. (2013). Affective Processing and Affect Regulation: A Clinical Interview Study. J Am Psychoanal Assoc 61:12-6 [DOI] [PubMed] [Google Scholar]
- Majohr K. L., Leenen K., Grabe H. J., Jenewein J., Nuñez D. G., Rufer M. (2011). Alexithymia and its relationship to dissociation in patients with panic disorder. J Nervous Mental Dis 199:773-7 [DOI] [PubMed] [Google Scholar]
- Mason O., Tyson M., Jones C., Potts S. (2005). Alexithymia: Its prevalence and correlates in a British undergraduate sample. Psychol Psychotherapy 78:113-25. [DOI] [PubMed] [Google Scholar]
- Mattila A. K., Salminen J. K., Nummi T., Joukamaa M. (2006). Age is strongly associated with alexithymia in the general population. J Psychosomatic Res 61:629–35. [DOI] [PubMed] [Google Scholar]
- Modestin J., Lötscher K., Erni T., (2002). Dissociative experiences and their correlates in young non-patients. Psychol Psychotherapy 75:53-64. [DOI] [PubMed] [Google Scholar]
- New A.S., Rot M.A.H., Ripoll L.H., Perez-Rodriguez M.M., Lazarus S., Zipursky E., Siever L.J. (2012). Empathy and alexithymia in borderline personality disorder: Clinical and laboratory measures. J Pers Disord 26:660-75. [DOI] [PubMed] [Google Scholar]
- O’Brien F.M., Fortune G.M., Dicker P., O’Hanlon E., Cassidy E., Delanty N., Murphy K. C. (2015). Psychiatric and neuropsychological profiles of people with psychogenic nonepileptic seizures. Epilepsy Behav 43:39-45. [DOI] [PubMed] [Google Scholar]
- Ogrodniczuk J.S., Piper W. E., Joyce S.J. (2011). Effect of alexithymia on the process and outcome of psychotherapy: A programmatic review. Psychiatry Res 190:43-8. [DOI] [PubMed] [Google Scholar]
- Onor M.L., Trevisiol M., Spano M., Aguglia E., Paradiso S. (2010). Alexithymia and aging. J Nervous Ment Dis 198:891-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paivio S.C., McCulloch C.R. (2004). Alexithymia as a mediator between childhood trauma and self-injurious behaviors. Child Abuse and Neglect 28:339-54. [DOI] [PubMed] [Google Scholar]
- Parker J.D., Taylor G.J., Bagby R.M. (1998). Alexithymia: relationship with ego defense and coping styles. Comprehensive Psychiatry 39:91-8. [DOI] [PubMed] [Google Scholar]
- Prasko J., Grambal A., Kasalova P., Kamardova D., Ociskova M., Holubova M., Zatkova M. (2016). Impact of dissociation on treatment of depressive and anxiety spectrum disorders with and without personality disorders. Neuropsychiatr Dis Treat,ent 12:2659-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafiq S., Campodonico C., Varese F. (2018). The relationship between childhood adversities and dissociation in severe mental illness: A meta-analytic review. Acta Psychiatrica Scandinavica 138:509-25. [DOI] [PubMed] [Google Scholar]
- Rufer M., Held D., Cremer J., Fricke S., Moritz S., Peter H., Hand I. (2006). Dissociation as a predictor of cognitive behavior therapy outcome in patients with obsessive-compulsive disorder. Psychotherapy Psychosomatics 75:40-6. [DOI] [PubMed] [Google Scholar]
- Saariaho A.S., Saariaho T.H., Mattila A.K., Karukivi M., Joukamaa N.I. (2015). Alexithymia and early maladaptive schemas in chronic pain patients. Scandinavian J Psychol 56:428-37. [DOI] [PubMed] [Google Scholar]
- Schimmenti S. (2016). The developmental roots of dissociation: A multiple mediation analysis. Psychoanal Psychol 34:96-105. [Google Scholar]
- Schimmenti A., Caretti V. (2014). Linking the overwhelming with the unbearable. Developmental trauma, dissociation, and the disconnected self. Psychoanal Psychol 33:106-28. [Google Scholar]
- Schimmenti A., Sideli L., LaMarca L., Gori A., Terrone G. (2019). Reliability, validity, and factor structure of the Maladaptive Daydreaming Scale (MDS-16) in and Italian sample. J Pers Assess 23:1-13. [DOI] [PubMed] [Google Scholar]
- Spitzer C., Barrow S., Freyberger H.J., Grabe H. (2007). Dissociation predicts symptom-related treatment outcome in short-term inpatient psychotherapy. Australian New Zealand J Psychiatry 41:682-7. [DOI] [PubMed] [Google Scholar]
- Suurmond R., van Rhee H., Hak T. (2017). Introduction, comparison and validation of Meta-Essentials: A free and simple tool for meta-analysis. Res Synth Methods 8:537-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor G.J., Bagby R.M., Parker J.D.A. (1997). Disorders of affect regulation: alexithymia in medical and psychiatric illness. Cambridge University Press, New York, N.Y. [Google Scholar]
- Terock J., Janowitz D., Spitzer C., Miertsch M., Freyberger H.J., Grabe H.J., (2015). Alexithymia and self-directedness as predictors of psychopathology and psychotherapeutic treatment outcome. Comprehensive Psychiatry 62:34-41. [DOI] [PubMed] [Google Scholar]
- Terock J., Janowitz D., Grabe H.J., Freyberger H.J., Schneider W., Klauer T. (2017). Alexithymia and Psychotherapeutic treatment motivation: Main and interactional effects on treatment outcome. Psychother Psychosomatics 86:185-1286. [DOI] [PubMed] [Google Scholar]
- Westwood H., Kerr-Gaffney J., Stahl D., Tchanturia K. (2017). Alexithymia in eating disorders: Systematic review and meta-analyses of studies using the Toronto Alexithymia Scale. J Psychosomatic Res 99:66-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz O., Ateş M.A., Semiz Ü.B., Tütüncü R., Bez Y., Algül A, Çetin M. (2016). Childhood traumas in patients with bipolar disorder: Association with alexithymia and dissociative experiences. Australian J Psychiatry 17:188-95. [Google Scholar]
- Zamir O., Szepsenwol O., Englund M.M., Simpson J.A. (2018). The role of dissociation in revictimization across the lifespan: A 32-year prospective study. Child Abuse and Neglect 79:144-53. [DOI] [PubMed] [Google Scholar]
- Ziadni M.S., Jasinsji M.J., Labouvie-Vief G., Lumley M.A. (2017). Alexithymia, defenses, and ego strength: Cross sectional and longitudinal relationships with psychological well-being and depression. J Happiness Stud 18:1799-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotnick C., Shea M.T., Pearlstein T., Simpson E., Costello E., Begin A. (1996). The relationship between dissociative symptoms, alexithymia, impulsivity, sexual abuse and self-mutilation. Comprehensive Psychiatry 37:12-6. [DOI] [PubMed] [Google Scholar]
- Zorzella K.P., Muller R.T., Cribbie R.A., Bambrah V., Classen C.C. (2019). The role of alexithymia in trauma therapy outcomes: Examining improvements in PTSD, dissociation and interpersonal problems. Psychological Trauma: Th Res Pract Policy. doi: 10.1037/tra0000433. [DOI] [PubMed] [Google Scholar]


