Abstract
Nowadays, several techniques are available for preserving the lateral aspect of the knee after meniscectomy; meniscus transplantation is the gold standard, and meniscus scaffold implantation is an effective alternative. However, meniscus transplantation is technically difficult and has many potential complications, whereas scaffolds resorb over time. Autografts are commonly used for labroplasty in shoulder and hip surgeries. We attempted to adapt this technique to the knee, using autografts for meniscus replacement. In this report, we describe a meniscus-replacement technique, using a peroneus longus autograft, for lateral meniscus deficits. This technique significantly simplifies the procedure and is cost effective, and thus can be considered as an alternative technique for preventing osteoarthritis of the lateral aspect of the knee.
The high risk for early osteoarthritis progression after lateral meniscectomy is well known.1 Several surgical procedures are available to prevent the risk of progression, including allograft transplantation, collagen meniscus implants, and implantation for the prevention of osteoarthritis. The disadvantages of meniscus allograft implantation are the difficulty of the surgical procedure, allograft failure, potential risk of infection, and disease transmission. Collagen meniscus implants show progressive graft resorption over time.
Recently, there has been a tendency to adapt ideas from shoulder surgery to knee surgery and vice versa. Autografts are commonly used for labroplasty in shoulder and hip surgeries. The idea here was to adapt this technique to the knee—from labroplasty to meniscoplasty using an autograft. Most techniques describe meniscus transplantation with a bone block; however, some recent studies have confirmed that meniscus transplantation without a bone block is possible. This, too, can be an argument for using a tendon autograft as a soft-tissue transplant.2,3
Autografts of the peroneus longus tendon are becoming popular in knee surgery for reconstruction of the anterior cruciate ligaments (ACLs) and posterior cruciate ligaments.4, 5, 6 In this report, we aimed to describe a meniscus-replacement technique, using a peroneus longus tendon graft, for lateral meniscus deficits. To optimize the surgical technique, we adapted some steps from shoulder surgery.
Surgical Technique (With Video Illustration)
Diagnostic Arthroscopy and Meniscus Rim Preparation
The procedure is performed with the patient in the supine position on the operating table with a tight tourniquet, and the knee is flexed to 90°. After diagnostic arthroscopy with standard portals, the meniscus footprint is prepared with a shaver and a diamond rasp (Smith & Nephew, Andover, MA). The remaining meniscus tissue is resected to the red zone as described by Spalding et al.3 The parameniscus is prepared for bleeding stimulation with a meniscal rasp. Finally, the length of the native meniscus is approximately measured with a graduated probe or ruler.
Peroneus Longus Graft Harvesting and Preparation
In a regular situation, the tendon is harvested from the same leg. Through a 3-cm incision, the peroneus longus is identified (Fig 1). The distal part of the peroneus longus is sutured to the peroneus brevis with 3 simple stitches and cut proximally. The proximal part of the tendon is sutured with 4 Krakow stitches. The peroneus longus is then harvested carefully, avoiding peroneus nerve injury. The wound is then closed following standard procedures.4
Fig 1.
Peroneus longus tendon graft harvesting.
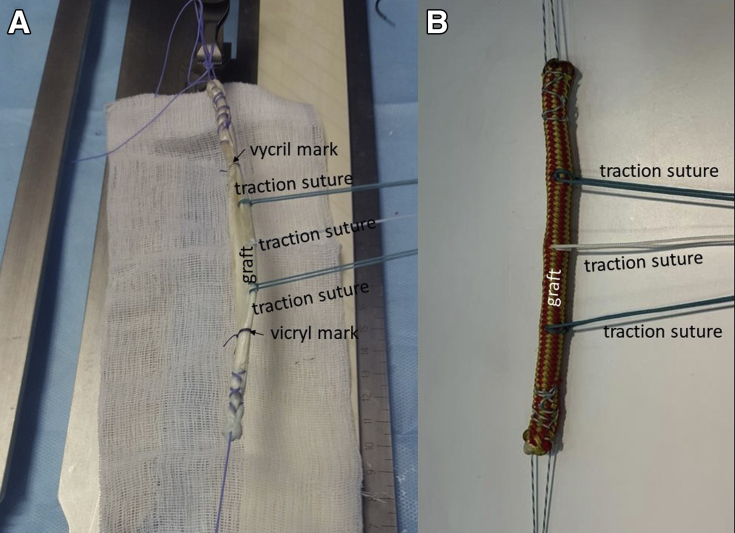
After being harvested, the peroneus longus tendon is sutured on the preparation table by suturing 2 to 3 cm from each end with nonabsorbable sutures. The borders of the intra-articular parts of the graft are marked with VICRYL absorbable sutures (Ethicon, Somerville, NJ) or with a marker, which was measured during the stage of diagnostic arthroscopy. One side of the tendon is sutured by 3 different-colored traction sutures at equal intervals, starting from the middle of the tendon, where the first traction suture is placed with a lasso loop.7 The second and third traction sutures are placed midway between the central one and the VICRYL marks (Fig 2). The graft diameter is measured with a sizer.
Fig 2.
Peroneus tendon graft preparation in a live specimen (A) and model (B). The ends of the peroneus longus tendon are sutured with nonabsorbable stitches. Traction sutures and VICRYL marks are placed.
Bone Tunnel Preparation for Graft Roots
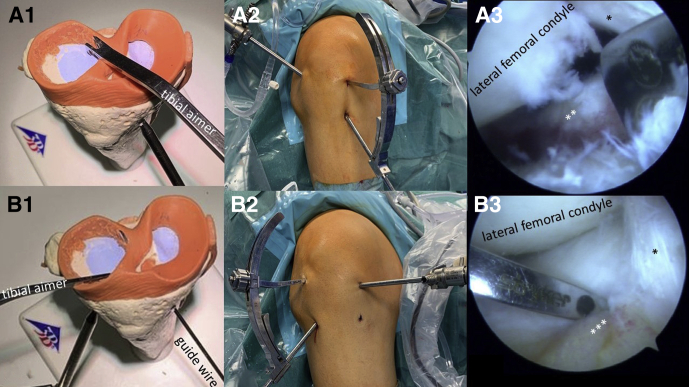
Intra-articular graft insertion tunnels are located as described by Spalding et al.3 For anterior horn bone tunnel preparation, the tip of a tibial aimer is positioned anterior to the lateral tibial spine and just lateral to the ACL. The bullet of the guide passes through a 1-cm incision localized 1 cm lateral to the tibial tuberosity and 2 to 3 cm distal to the joint level (Fig 3B).
Fig 3.
Creation of bone tunnels for anterior and posterior graft insertion in the right knee. Tibial aimer placement in a model (A1). Tibial aimer placement for posterior graft insertion in an extra-articular view (A2). Arthroscope is placed through the standard anterior lateral portal; the tibial aimer is inserted through the standard anterior medial portal. The bullet of the guide is located 3 cm below the joint line, in the posterior third of the medial tibial plateau. Intra-articular view (A3) of the tip of the tibial aimer, which is positioned just posterior to the ACL, between the tibial spines. Tibial aimer placement for anterior graft insertion in a model (B1). Extra-articular view (B2): the arthroscope is placed through the standard anterior medial portal; the tibial aimer is inserted through the standard anterior lateral portal. The bullet of the guide passes through a 1-cm incision localized 1 cm lateral to the tibial tuberosity and 2 to 3 cm distal to the joint level. Intra-articular view (B3): the tip of a tibial aimer is positioned anterior to the lateral tibial spine and just lateral to the ACL. ∗Anterior cruciate ligament; ∗∗remnants of posterior horn; ∗∗∗remnants of anterior horn. (ACL, anterior cruciate ligament.)
For the posterior horn, the tip of the tibial aimer is positioned just posterior to the ACL, between the tibial spines. The bullet of the guide is located 3 cm below the joint line, in the posterior third of the medial tibial plateau (Fig 3A).
Guided pins are inserted through the aimers. The bone tunnels are drilled using a classic drill or retrodrilling device. The size of the drill should be equal to the graft diameter.
Graft Passage
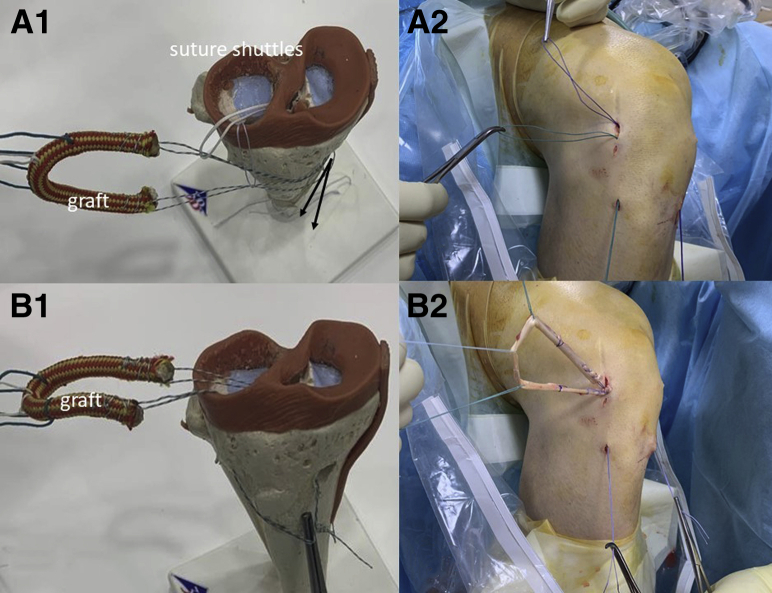
Shuttling sutures of 2 different colors are inserted into the joint through the tunnels and are pulled through the anterior lateral portal (Fig 4A). The sutures that are fixed to the ends of the graft are connected to the shuttling sutures on the graft, which is then inserted into the joint (Fig 4B).
Fig 4.
Graft passage through the tunnels. (A) Shuttling sutures connected to the anterior and posterior part of the transplant seen in a model (A1). Extra-articular view of the right knee. The blue shuttling suture is passed through the posterior tunnel, the green shuttling suture is passed through the anterior tunnel (A2). (B) Sutures connected to the anterior and posterior part of the transplant pass through the tunnels seen in a model (B1) and in an extra-articular view of the right knee (B2).
Graft Fixation
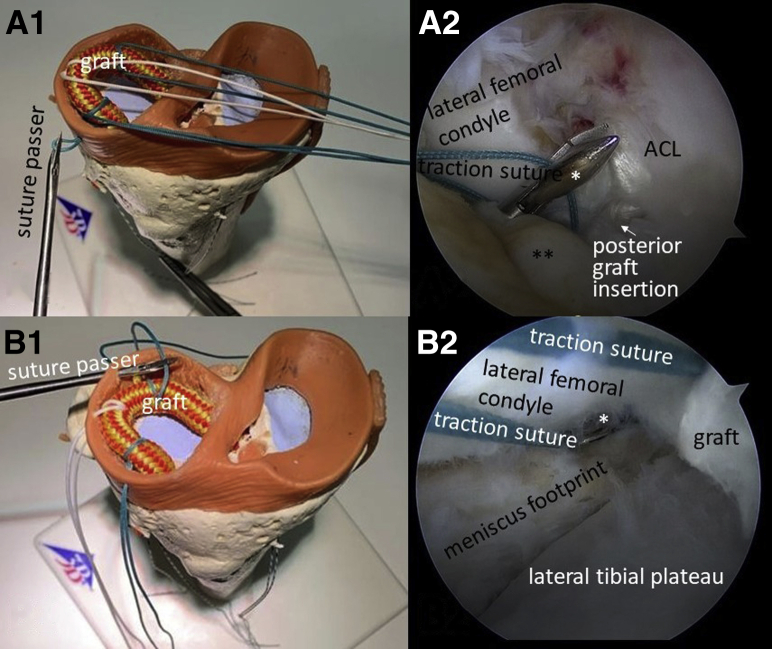
After insertion, the anterior and posterior ends of the graft are inserted through the tunnels until the level of the VICRYL marks. Through a 1- to 2-cm lateral incision, the traction sutures are caught with a bird beak grasper, and the sutures are fixed onto the capsule (Fig 5). After fixation of the traction sutures, the posterior horn of the lateral meniscus is routinely fixed with FAST-FIX 360 suturing devices (Smith & Nephew) (Fig 6). The anterior horn and meniscus body are fixed with additional multiple sutures, using a regular outside-in technique. At the end of the procedure, the graft roots are fixed with suture buttons, knotless anchors, or interference screws at the surgeon’s discretion (Fig 7). Table 1 and Video 1 summarize the steps of the procedure.
Fig 5.
Fixation of the traction sutures with shoulder penetration grasper through the capsule in an outside-in direction. (A) Fixation of the anterior part of the transplant in a model (A1) and in an intra-articular view of the right knee from the standard anterior medial portal (A2). (B) Fixation of the body and posterior part of the transplant in a model (B1) and in an intra-articular view of the right knee from the standard anterior lateral portal (B2). ∗Suture grasper; ∗∗remnants of anterior horn.
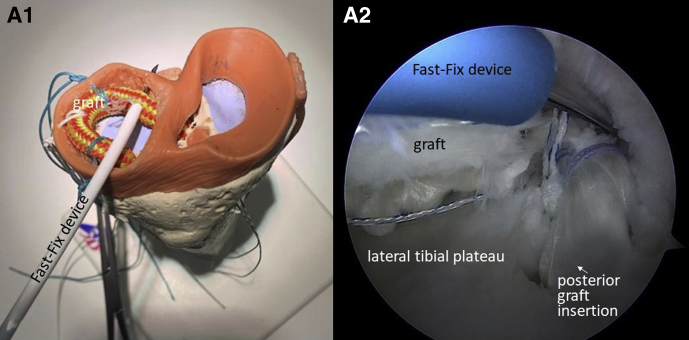
Fig 6.
Posterior part of the graft is fixed with a FAST-FIX 360 device (Smith & Nephew) as seen in a model (A1) and in an intra-articular view of the right knee (A2). The arthroscope is inserted through the standard anterior medial portal; FAST-FIX device is inserted through the standard anterior lateral portal
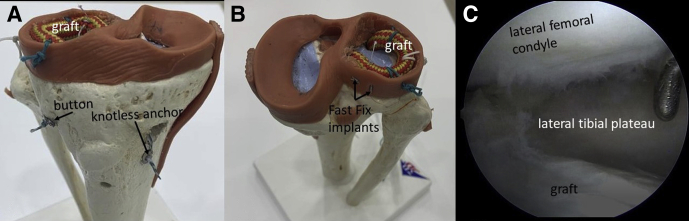
Fig 7.
Final view in a model. (A) Anterior view: anterior root of the graft is fixed with a button on the lateral tibial condyle. Posterior graft root is fixed with a knotless anchor. (B) Posterior view: traction sutures fix the graft to the capsule and remnants of the meniscus. Posterior part of the graft is fixed with 2 FAST-FIX devices (Smith & Nephew). (C) Final intra-articular view of the right knee.
Table 1.
Steps of the Procedure
| Step | Description |
|---|---|
| 1 | Diagnostic arthroscopy and meniscus rim preparation with shaver and meniscus rasp. |
| 2 | Peroneus longus graft harvesting and preparation. |
| 3 | Creation of bone tunnels for anterior and posterior graft insertion in the centers of the meniscus roots. |
| 4 | Graft passage into the joint and through the tunnels with suture shuttles. |
| 5 | Graft fixation: traction sutures are fixed in an outside-in direction. Posterior part is fixed with FAST-FIX devices. Graft roots are fixed into the tunnels. |
| 6 | Final joint examination. |
Discussion
It is well known that the risk of early osteoarthritis after lateral meniscectomy is greater than that after the medial procedure.1 Even after partial meniscectomy of the discoid lateral meniscus, there is radiographic evidence of progression to high-grade osteoarthritis, as demonstrated in a study with a minimum follow-up of 5 years.8 To prevent the development of osteoarthritis, several techniques are described in the scientific literature, including meniscus transplantation, which is the gold standard treatment for postmeniscectomy syndrome. Nevertheless, the procedure is technically complicated and expensive. The main technical difficulty is the meniscus size mismatch between the donor and recipient. This procedure is also traumatic because it requires bone-block adaptation into the joint. Moreover, there is residual pain, and recovery after meniscus transplantation and returning to professional sport is slow and sometimes impossible. In addition, there is always the possibility of transplantation failure.9 Finally, in some countries, allograft transplantation may produce legal complications as well.
Another treatment option is meniscus scaffold implantation.10 Long-term results of the procedure are positive, but some studies have described constant meniscus scaffold resorption.11
Moreover, collagen scaffold implantation can only be performed for partial replacement of the meniscus.
Recently, practitioners started using tendon autografts to replace the labrum in the hip and shoulder joints.12,13 Tendon autografts have several undeniable advantages: (1) there is no immunologic reaction, (2) recovery is relatively fast, (3) it is possible to replace the entire meniscus, (4) it is suitable for every size of meniscus, (5) the autograft can be used in countries in which using allografts is impossible, and (6) the autograft is more cost-effective. Nevertheless, semitendinosus and gracilis tendon autografts are not acceptable because the diameter of the tendon is insufficient to replace the resected part of the meniscus in most of the cases.
Use of the peroneus longus tendon autograft for lateral meniscus replacement is possible because the size and biomechanical characteristics of the peroneus longus tendon autograft are similar to that of the native meniscus, making this transplantation procedure promising and safe.14 The suggested technique is easier in comparison with allotransplantation of the meniscus. It uses standard preparation and harvesting techniques and can be performed using standard procedures and knee and shoulder instrument sets. Moreover, it is cost-effective and produces no immunologic reactions. Furthermore, size measurement is not critical compared with meniscus allograft transplantation because excess tissue can be easily passed through the tunnel and resected or fixed extra-articularly. Biomechanical requirements (130-150 megapascal on average) can be met by compression load of the peroneus graft.14
The main indications for our procedure are similar to allograft transplantation and meniscus scaffolds implantation: lateral pain syndrome after lateral meniscectomy in young patients without significant osteoarthritic changes. It is possible to perform this procedure for patients with nonsignificant malalignments and stable knee. The contraindications of the procedure are obesity, synovial disease, inflammatory arthritis, and previous joint infections.
There is a potential risk of morbidity at the donor site, and although there is the theoretical possibility of peroneus nerve injury, limp, or collapsed arch, Rhatomy et al.5 and Shi et al.6 have described that the frequency of complications is low with this technique. Furthermore, the technique has several limitations. It has a potential resorption risk; and the direction of the fibers in the graft differs from that in the meniscus; thus, the use of this technique in professional athletes is unknown. Moreover, the procedure requires a high degree of surgical skill.
Tables 2 and 3 summarize the advantages and disadvantages and pearls and pitfalls, respectively, of our technique. The outcomes of the first 2 cases in which this technique was performed were positive (Fig 8), and the length of follow-up was 6 to 10 months; thus, we are able to conclude that the technique can be used and improved.
Table 2.
Advantages and Disadvantages of This Technique
| Advantages | Disadvantages |
|---|---|
| Cost-effective | Potential resorption risk |
| No immunologic reaction | Fiber direction differs from that in the natural meniscus |
| No disease transmission | Requires a high degree of surgical skill |
| Standard preparation and harvesting techniques | The possibility of donor-site morbidity exists |
| Can be performed using standard, known techniques and shoulder and knee instrument sets | The possibility of using this technique for professional athletes is under consideration |
| Size measurement is not critical because excess tissue can be easily resected or passed through the tunnel | |
| Graft biomechanical characteristic (130-150 megapascal in average) is sufficient for the anticipated compression load |
Table 3.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Accurate debridement of the recipient zone | Osteoarthritic changes in the lateral part and cartridge deficit are contraindications to this technique |
| The bone tunnel divergence and position for graft roots are critical | Accurate protection of posterior–lateral neurovascular structures is critical |
| For solid fixation, all methods of meniscus suturing are required (outside-in, inside-out, all inside) | |
| Shoulder-penetration graspers make this technique easier and reproducible |
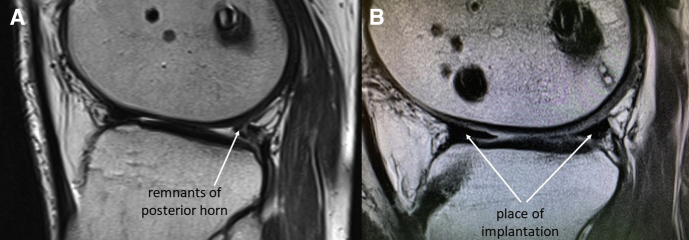
Fig 8.
(A) Sagittal plain MRI of the right knee before meniscus replacement. (B) Sagittal plain MRI of the right knee 3 months after meniscus replacement. (MRI, magnetic resonance imaging.)
Footnotes
The authors report the following potential conflicts of interest or sources of funding: O.M. reports other from DePuy Synthes, nonfinancial support from Arthrex, and personal fees from Arthrex, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The video describes a technique for lateral meniscus replacement using a peroneus longus tendon autograft in a step-by-step manner. After diagnostic arthroscopy, the peroneus longus tendon graft is harvested by standard procedures and prepared, and both ends are sutured. Thereafter, traction tunnels are prepared with a tibial guide. The graft is inserted into the joint and fixed, first with traction sutures and then with solid outside-in, inside-out, and all-inside sutures.
References
- 1.Peña E., Calvo B., Martinez M.A., Palanca D., Doblaré M. Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study. J Orthop Res. 2006;24:1001–1010. doi: 10.1002/jor.20037. [DOI] [PubMed] [Google Scholar]
- 2.Woodmass J.M., Johnson N.R., Levy B.A., Stuart M.J., Krych A.J. Lateral meniscus allograft transplantation: The bone plug technique. Arthrosc Tech. 2017;6:e1215–e1220. doi: 10.1016/j.eats.2017.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spalding T., Parkinson B., Smith N.A., Verdonk P. Arthroscopic meniscal allograft transplantation with soft-tissue fixation through bone tunnels. Arthrosc Tech. 2015;4:e559–e563. doi: 10.1016/j.eats.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Setyawan R., Soekarno N.R., Asikin A.I.Z., Rhatomy S. Posterior cruciate ligament reconstruction with peroneus longus tendon graft: 2-years follow-up. Ann Med Surg. 2019;43:38–43. doi: 10.1016/j.amsu.2019.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rhatomy S., Asikin A.I.Z., Wardani A.E., Rukmoyo T., Lumban-Gaol I., Budhiparama N.C. Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:3552–3559. doi: 10.1007/s00167-019-05455-w. [DOI] [PubMed] [Google Scholar]
- 6.Shi F.D., Hess D.E., Zuo J.Z. Peroneus longus tendon autograft is a safe and effective alternative for anterior cruciate ligament reconstruction. J Knee Surg. 2019;32:804–811. doi: 10.1055/s-0038-1669951. [DOI] [PubMed] [Google Scholar]
- 7.Lafosse L., Van Raebroeckx A., Brzoska R. A new technique to improve tissue grip: “The lasso-loop stitch. Arthroscopy. 2006;22 doi: 10.1016/j.arthro.2006.05.021. 1246.e1-1246.e3. [DOI] [PubMed] [Google Scholar]
- 8.Ahn J.H., Kang D.M., Choi K.J. Risk factors for radiographic progression of osteoarthritis after partial meniscectomy of discoid lateral meniscus tear. Orthop Traumatol Surg Res. 2017;103:1183–1188. doi: 10.1016/j.otsr.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Rosso F., Bisicchia S., Bonasia D.E., Amendola A. Meniscal allograft transplantation: A systematic review. Am J Sports Med. 2015;43:998–1007. doi: 10.1177/0363546514536021. [DOI] [PubMed] [Google Scholar]
- 10.Myers K.R., Sgaglione N.A., Goodwillie A.D. Meniscal scaffolds. J Knee Surg. 2014;27:435–442. doi: 10.1055/s-0034-1388656. [DOI] [PubMed] [Google Scholar]
- 11.Schenk L., Bethge L., Hirschmann A., Lüthi B.U., Arnold M.P., Hirschmann M.T. Ongoing MRI remodeling 3-7 years after collagen meniscus implantation in stable knees. Knee Surg Sports Traumatol Arthrosc. 2019;18:1–6. doi: 10.1007/s00167-019-05714-w. [DOI] [PubMed] [Google Scholar]
- 12.Milenin O., Toussaint B. Labral repair augmentation by labroplasty and simultaneous trans-subscapular transposition of the long head of the biceps. Arthrosc Tech. 2019;8:e507–e512. doi: 10.1016/j.eats.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rahl M.D., LaPorte C., Steinl G.K., O’Connor M., Lynch T.S., Menge T.J. Outcomes after arthroscopic hip labral reconstruction: A systematic review and meta-analysis. Am J Sports Med. 2019;21 doi: 10.1177/0363546519878147. 0363546519878147. [DOI] [PubMed] [Google Scholar]
- 14.Wong A.K., Calvo M.R., Schaffler B.C. Biomechanical and geometric characterization of peroneus longus allografts with respect to age. Clin Biomech. 2019;67:90–95. doi: 10.1016/j.clinbiomech.2019.04.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video describes a technique for lateral meniscus replacement using a peroneus longus tendon autograft in a step-by-step manner. After diagnostic arthroscopy, the peroneus longus tendon graft is harvested by standard procedures and prepared, and both ends are sutured. Thereafter, traction tunnels are prepared with a tibial guide. The graft is inserted into the joint and fixed, first with traction sutures and then with solid outside-in, inside-out, and all-inside sutures.