Abstract
Meniscal root tears are an increasingly recognized condition. These tears can cause the meniscus to become extruded outside the joint, which can diminish the biomechanical functionality of the meniscus. Anatomic repair of the meniscal root has previously been described, but this surgical procedure may not adequately address severe extrusion of the meniscal tissue. Additionally, when a primary anatomic repair fails, meniscal extrusion can increase, which can possibly accelerate joint degeneration if untreated. Therefore, the purpose of this Technical Note is to describe our surgical technique for revision medial meniscal root repair with a peripheral stabilization suture to address medial meniscal root tears with severe meniscal extrusion.
A meniscal root tear is defined as a tear or avulsion within 1 cm of the meniscal root attachment site.1 Tears of the posterior-medial meniscal root are most common in middle-aged patients, whereas posterior-lateral meniscal root tears most commonly occur in younger patients with concomitant anterior cruciate ligament injuries.2, 3, 4 Recent biomechanical and clinical data have established the role of the meniscal root on knee biomechanics; meniscal root deficiency leads to, among other problems, altered tibiofemoral contact forces, variations in cruciate graft forces, subchondral insufficiency fractures, and an increased risk of development of end-stage osteoarthritis.4, 5, 6, 7, 8, 9, 10, 11, 12
Meniscal root tears occur when the meniscal root becomes detached from the tibial plateau, which limits the functionality of the meniscus, alters the native knee kinematics, and can lead to meniscal extrusion.10,13 Meniscal extrusion has traditionally been identified using magnetic resonance imaging (MRI) and defined as meniscal tissue extending greater than 3 mm outside the edge of the tibial plateau at the level of the medial collateral ligament.14 Medial meniscal extrusion has been linked to cartilage loss and a more rapid progression of osteoarthritis in patients with meniscal tears.15
Although modern anatomic surgical techniques are able to successfully repair the meniscal root to its anatomic attachment site, nonanatomic root repair techniques do not restore the contact area or mean contact pressures of the intact knee or anatomic repair.13,16, 17, 18, 19 Recent biomechanical evidence suggests that use of a peripheral stabilization suture is able to help restore the contact mechanics of the knee and decrease the amount of extrusion.17 Thus, this describes our team’s surgical technique for a 3-tunnel revision medial meniscal root repair with a peripheral stabilization suture at the apex of the posteromedial aspect of the tibial plateau.17
Surgical Technique
The technique is detailed in Video 1. Pearls and pitfalls of this technique and advantages and disadvantages of our approach are described in Table 1 and Table 2, respectively.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| A curved suture-passing device should be used for the root repair, and a straight suture-passing device should be used for the peripheral stabilization suture. | Failure to stabilize the posterior horn may result in continued meniscal extrusion, causing altered tibiofemoral contact pressures and knee kinematics. |
| A sufficient peripheral meniscocapsular junction release should be performed to allow the meniscus to be reapproximated and pulled back into the joint. | Tying the sutures directly over the bone should be avoided because they can cut the bone, which can cause the repair to become loose and cause local irritation. |
| The root repair should be tied over a button to allow for secure fixation without cutting the bone and to allow postoperative visualization of the root repair.20 | Nonanatomic repair of the root does not restore the biomechanical properties of the meniscus and can lead to altered contact pressures and knee kinematics.19 |
| Use of a medial unloader brace should be considered in patients in valgus malalignment to protect the repair. | An insufficient peripheral release does not allow the meniscus to be pulled back into an anatomic location. |
| Meniscal extrusion should be assessed on a coronal magnetic resonance imaging sequence and arthroscopically intraoperatively. | |
| Trephination (pie-crusting) with a spinal needle will enhance visualization and maneuverability in the medial compartment. |
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| The repair is performed by an anatomic technique that restores the posterior meniscal root and stabilizes a significantly extruded meniscus. | An additional transtibial tunnel and an additional suture fixation device are needed. This can lead to increased irritation. |
| The technique uses a single additional transtibial tunnel for the peripheral stabilization in addition to the 2 tunnels that are used for the meniscal root repair. | The technique is technically challenging. |
| The technique prevents future extrusion of the medial meniscus after surgical repair of the medial root. | The patient has to be compliant with the postoperative rehabilitation protocol. |
Indications and Contraindications
The indications for meniscal root repair with a peripheral stabilization suture are clinical and radiographic evidence of complete detachment of the medial meniscus at or near (0-9 mm) the posterior root attachment with significant extrusion of meniscal tissue outside the joint, confirmed during arthroscopy. Contraindications for a meniscal root repair are severe (grade III or IV) chondromalacia in the ipsilateral compartment, comorbidities that make a patient unable to follow the postoperative rehabilitation protocol, and severe malalignment. Although patients with open physes are an atypical age demographic for this injury, open physes are not a contraindication for root repair with a peripheral stabilization suture, as recently suggested by DePhillipo et al.21 Preoperative anteroposterior, Rosenberg, and lateral radiographs, including full-length weight-bearing radiographs to assess for genu varum or valgum malalignment and joint space narrowing, should be obtained. Additionally, MRI should be used to assess the status of the meniscal root attachment and the degree of meniscal extrusion (Fig 1).
Fig 1.
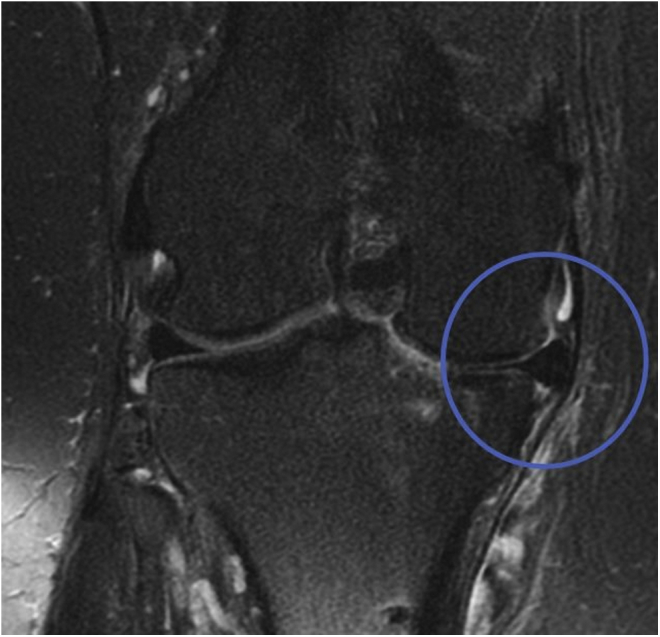
Coronal magnetic resonance image showing meniscal extrusion. By use of measurement software, the meniscus is determined to be extruded 4.4 mm outside the joint.
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table. After the induction of general anesthesia, a bilateral clinical knee examination is performed to evaluate knee range of motion and to assess for concurrent pathologies such as ligamentous instability. Next, a well-padded, high-thigh tourniquet is placed on the leg, which is then placed into a leg holder (Mizuho OSI, Union City, CA), whereas the contralateral limb is placed in an abduction stirrup (Birkova Products, Gothenburg, NE).
Surgical Approach
Standard anterolateral and anteromedial portals are established adjacent to the patellar tendon. The joint is insufflated with normal saline solution and visualized with a 30° arthroscopic camera (Smith & Nephew, Andover, MA). An arthroscopic shaver (Smith & Nephew) is inserted into the knee, and any significant adhesions are debrided. In the revision setting, this includes excision of loose sutures or remnants of the previous repair. Next, the root attachment site is identified approximately 9.6 mm posterior and 0.7 mm lateral to the medial tibial eminence apex and decorticated using a curved curette or curved shaver (meniscal root repair kit; Smith & Nephew) until healthy bony bleeding is observed (Fig 2).22 A significant peripheral release is then performed using rotary scissors (Acufex; Smith & Nephew) along the meniscocapsular junction of the posterior horn of the medial meniscus up to the level of the deep medial collateral ligament, to allow the meniscus to be sufficiently reapproximated back into the joint.23 The peripheral release is performed by cutting along the posterior meniscocapsular junction of both the superior and inferior aspects of the meniscus while leaving the midbody meniscocapsular attachments intact. The peripheral release is continued to the anterior aspect of the deep medial collateral ligament. An arthroscopic grasper (Alligator Grasper; Smith & Nephew) can now be used to ensure that the release is sufficient to reapproximate the meniscal root to its anatomic footprint. If visualization of the medial meniscal root is insufficient, trephination, or “pie-crusting,” of the meniscofemoral attachment of the superficial medial collateral ligament with a spinal needle can be performed to help open the medial compartment further. Pie-crusting can allow for improved visualization, as well as more space to maneuver instruments, and can limit the risk of iatrogenic damage to the medial femoral condyle and tibial plateau.24
Fig 2.
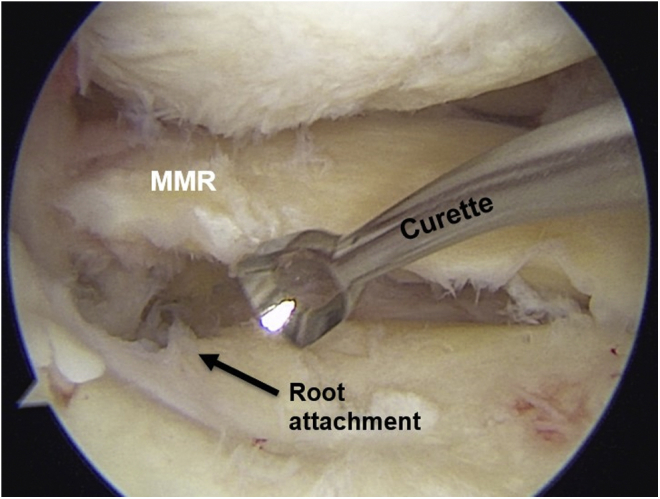
Arthroscopic view of a right knee from an anteromedial portal showing decortication of the medial meniscal root (MMR) attachment site using a curved curette. The footprint should be decorticated until healthy bony bleeding is observed.
Transtibial Tunnels
A skin incision for the transtibial tunnels is made approximately 5 cm distal to the joint line, just medial to the tibial tubercle. This incision is made approximately 1 cm larger than the traditional 2-transtibial meniscal root repair pullout technique to allow for the additional peripheral stabilization suture tunnel.25 After sharp dissection down to the periosteum, a Cobb elevator is used to remove the periosteum to allow for secure fixation of the cortical buttons on the bone. By use of a tibial drill guide (Smith & Nephew) to position a drill pin, the first transtibial tunnel is created at the desired reattachment site (Fig 3). A meniscal root tibial tunnel guide (Smith & Nephew) is then used to ream the first tunnel. The second tunnel is placed 5 mm from the first tunnel within the decorticated plateau area using an offset guide (Smith & Nephew).10,16 The 2 tunnels are visualized arthroscopically. This system has a 2.4-mm cannula that stays in place while the drill pin is removed. Once the tunnel position is verified to be within the decorticated bone area, the drill pins are removed, leaving the 2 cannulas in place for suture passage. After the root repair sutures are passed and the root tear is pulled into place, an additional tunnel for the transtibial peripheral stabilization suture is created at the apex of the posteromedial aspect of the medial tibial plateau using the aforementioned drill guide system.
Fig 3.
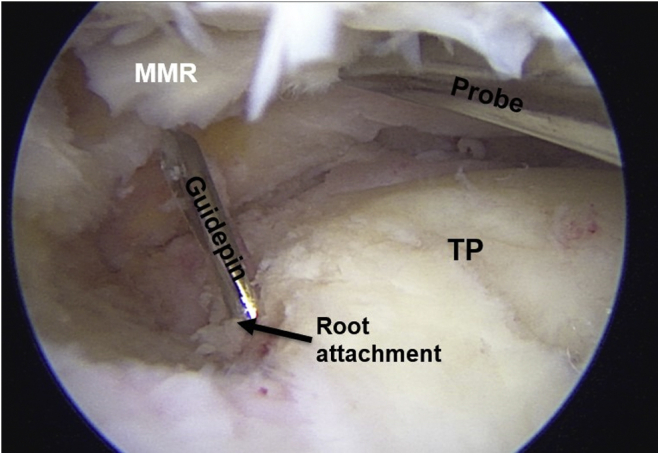
Arthroscopic view of a right knee from an anteromedial portal showing the location of the anterior tibial tunnel at the anatomic footprint of the posterior medial meniscal root (MMR). The footprint is directly observed while placing the guide pin to ensure that it is placed in an anatomic location. (TP, tibial plateau.)
Suture Passage
A curved suture-passing device (FirstPass Mini; Smith & Nephew) is used to pass the 2 root repair suture tapes. The first suture tape is placed through the far-posterior portion of the detached posterior medial meniscal root, approximately 7 mm medial to the lateral edge (Fig 4). The suture is passed from the tibial to femoral side. The suture device pulls out the suture tape through a cannula in the anteromedial portal as the device is removed from the joint. Before the second suture is placed, the first suture is shuttled through the more posterior tibial tunnel using a looped nylon passing suture. The second suture is passed in a similar fashion through the anterior aspect of the detached meniscal root (Fig 4). This anterior suture is passed through the anterior transtibial tunnel at the anatomic root attachment. The ability of the suture tapes to reduce the meniscal tear back to the prepared area is then assessed by placing traction on the suture tapes.
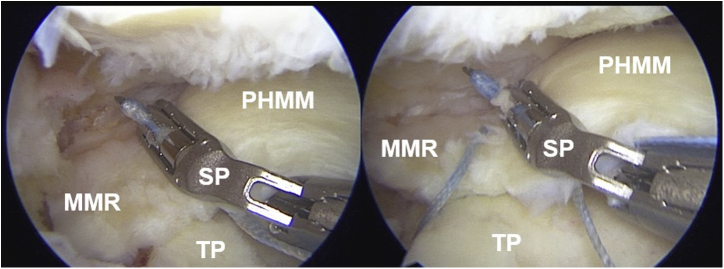
Fig 4.
Arthroscopic view of a right knee from an anteromedial portal showing suture passage at the medial meniscal root (MMR). A curved suture-passing device (SP) is used to place 2 separate suture tapes through the meniscal root. Passage of the first suture tape is shown on the left, and passage of the second suture tape is shown on the right. (PHMM, posterior horn of medial meniscus; TP, tibial plateau.)
Next, the suture tape is placed for the peripheral stabilization of the extruded meniscus. A straight suture passer is used to place a suture through the apex of the posterior horn of the medial meniscus from the tibial side to the femoral side (Fig 5, Fig 6, Fig 7). The suture is then pulled through the anteromedial portal. The same end of the suture tape is reloaded into the suture passer, and the device is inverted and re-advanced through the posterior horn of the medial meniscus, adjacent to (approximately 2 mm from) the position where suture was previously passed. This inversion allows the suture to be passed from the femoral side to the tibial side, creating a double-loaded suture construct using only 1 suture, with both ends of the suture exiting the meniscus at the inferior portion. The suture tape is then passed down the cannula in the same manner as the root repair suture tapes.
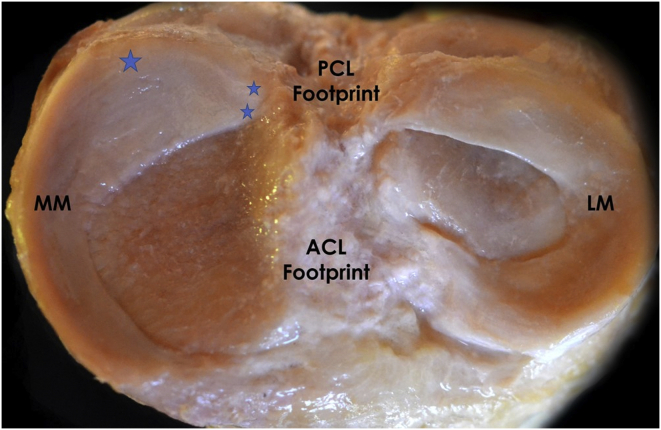
Fig 5.
Arthroscopic view of a right knee from an anteromedial portal showing passage of the peripheral stabilization suture tape. A peripheral stabilization suture is placed at the apex of the posterior horn of the medial meniscus (PHMM). Passage of the suture using a straight suture-passing device (SP) is shown on the left. The peripheral stabilization suture tape being pulled taut is shown on the right.
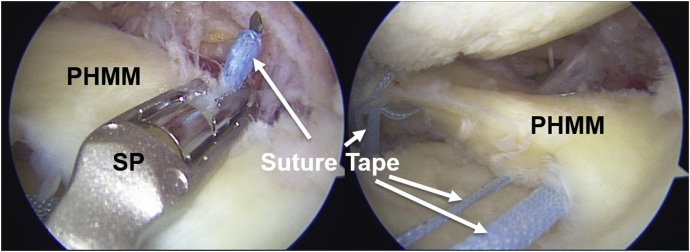
Fig 6.
Axial view looking down at a cadaveric dissection in a left knee. The 2 small stars represent the locations of the 2 transtibial tunnels created in the medial meniscal root repair. The large star at the apex of the posterior horn of the medial meniscus (MM) represents the location of the peripheral stabilization suture and the respective transtibial tunnel. (ACL, anterior cruciate ligament; LM, lateral meniscus; PCL, posterior cruciate ligament.)
Fig 7.
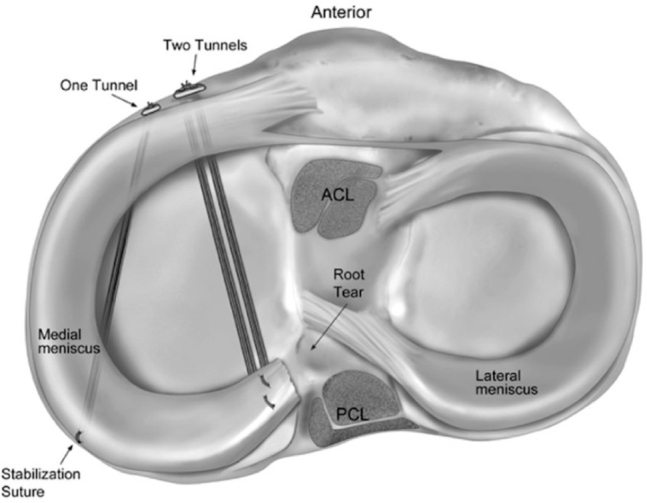
Axial view of medial meniscal root repair with a peripheral stabilization suture. One tunnel is used for the peripheral stabilization suture, and 2 tunnels are used for the medial meniscal root repair. Adapted from Daney et al.17 (ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.)
Suture Tape Fixation
Each suture tape is tied down over a cortical fixation device (EndoButton; Smith & Nephew) on the anteromedial tibia while the meniscus is visualized arthroscopically to confirm a secure repair. The 2 suture tapes placed through the meniscal root are tied down using a single cortical button device while the peripheral stabilization suture is secured using a second button. Finally, the complete fixation is probed and observed arthroscopically (Fig 8).
Fig 8.
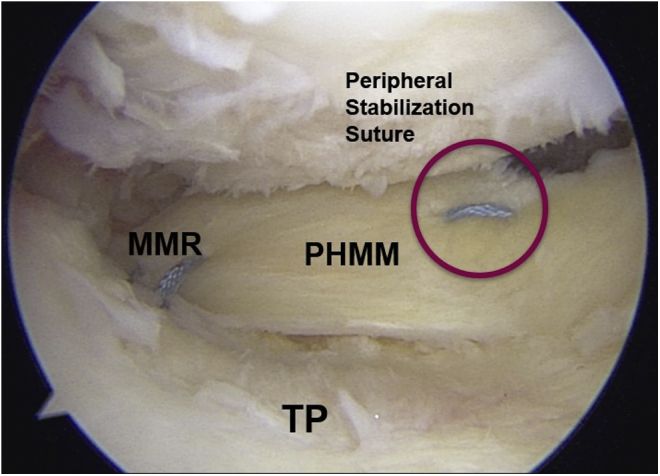
Arthroscopic view of a right knee from an anteromedial portal showing the final secure posterior medial meniscal root (MMR) repair with a peripheral stabilization suture. (PHMM, posterior horn of medial meniscus; TP, tibial plateau.)
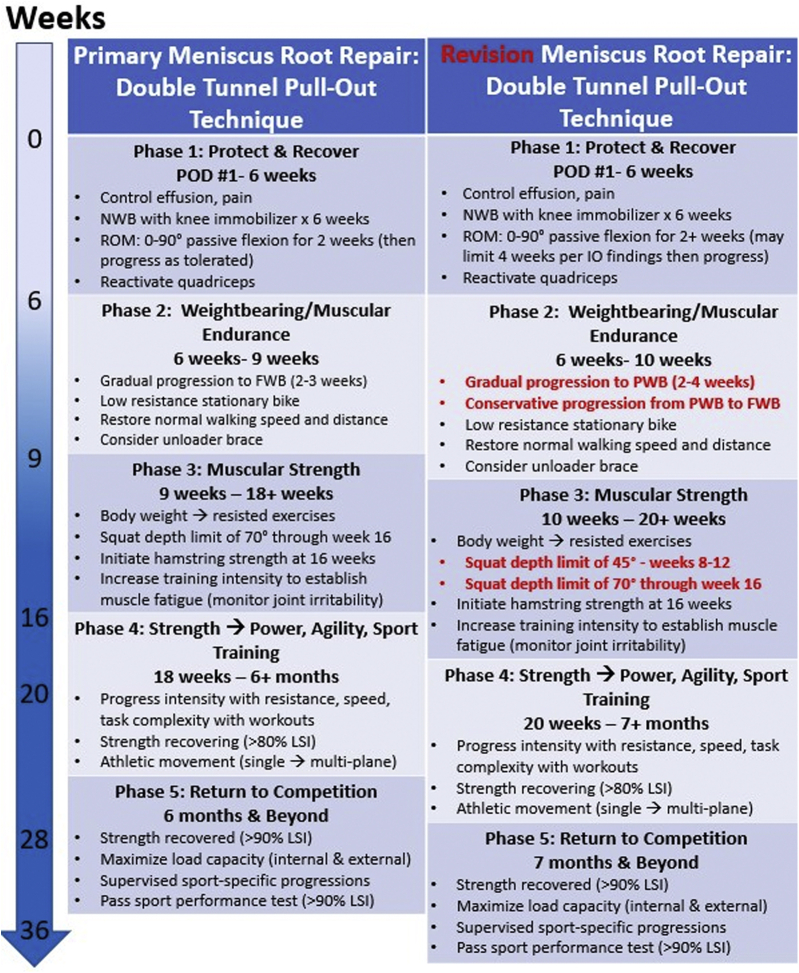
Postoperative Protocol
The patient is non–weight bearing in a knee immobilizer brace for 6 weeks postoperatively because biomechanical evidence has shown that early loading of meniscal root repairs before healing causes unrecoverable and progressive loosening of the repair.26 Physical therapy begins on postoperative day 1, with an early focus on pain control, edema reduction, and knee motion. Knee range of motion is limited to 0° to 90° for the first 2 weeks after the procedure to protect the repair. Typically, after 2 weeks, range of motion is progressed as tolerated. However, intraoperative concerns over root stability in a revision context may give cause for prolonging the maximal flexion limit an additional week or 2 weeks. Knee flexion motion is performed passively during the first 6 weeks after surgery to minimize the semimembranosus pulling through its insertion at the posteromedial capsular region, which may increase the stress on the healing posterior-horn meniscal region. At 6 weeks postoperatively, weight bearing is initiated and gradually progressed toward full weight bearing over the course of the next 2 to 3 weeks. In the revision setting, a more extended period of partial weight bearing before a return to full weight bearing may be advisable, per intraoperative findings, to manage hoop stresses and root pressures endured at the meniscus with the knee in the extended position.27 Low-resistance cycling on a stationary bike may be initiated at 6 weeks for the purpose of joint motion and nutrition, but aggressive pushing through a flexed knee for more intensive cardiovascular fitness should be avoided. If a patient is in genu varum alignment, a medial unloader brace (Ossur Americas, Foothill Ranch, CA) is used, once weight bearing begins, for a minimum of 4 months postoperatively. Once patients can tolerate 20 minutes of walking with a non-antalgic gait and a baseline therapy program is not observed to cause increased joint irritability (increased pain and/or swelling lasting >24 hours), a periodized strength regimen may be initiated. This training program focuses on sequential development of muscular endurance, strength, and power, respectively. Body weight exercises are performed initially, before progressing into exercise with external resistance. With an index meniscal root repair procedure, the knee flexion angle is limited to 70° with flexed-knee activities performed for strengthening in weight bearing (squat, step, lunge, leg press) for the first 16 weeks after surgery. Meniscal root pressures have been observed to increase notably from 30° to 60°, so a stricter restriction of squat depth may be recommended in a revision context.28 At our center, we impose a weight-bearing knee flexion limit of 0° to 45° from postoperative weeks 8 to 12 and then allow the patient to progress to a limit of 70° through week 16. After this time, the patient is able to gradually progress into deeper squatting per symptoms and lifestyle demands. Patients may begin a gradual return to activity at 5 months postoperatively as they master a progressively more challenging rehabilitation routine. Ultimate clearance to return to all activities is determined after patients pass a series of functional sports tests, clinical examination, and evaluation of plain radiographs; this typically occurs at 6 to 7 months postoperatively (Fig 9).29,30 Of note, there have been no direct comparisons between rehabilitation protocols after a transtibial single-tunnel root repair technique and protocols for a transtibial double-tunnel pullout technique. The recommendations in this article are based on the existing body of biomechanical and surgical literature, along with our clinical experience, because rehabilitation protocols are varied, are ill defined, and lack standardization for these procedures.
Fig 9.
Flowchart describing progression of rehabilitation after primary root repair (left) and revision root repair (right). (FWB, full weight bearing; LSI, limb symmetry index; NWB, non–weight bearing; POD, postoperative day; PWB, partial weight bearing; ROM, range of motion.)
Discussion
This Technical Note describes our preferred technique for revision medial meniscal root repair with a peripheral stabilization suture to address medial meniscal root tears with severe meniscal extrusion. A detailed understanding of medial meniscal anatomy, including the posterior root and posterior horn, is key for successful anatomic root repair with peripheral stabilization of the posterior horn. The severity of meniscal extrusion should be assessed radiographically on MRI and arthroscopically in patients with meniscal root tears to ensure adequate presurgical and intraoperative planning. Use of a peripheral stabilization suture is valuable because it helps restore the native biomechanical properties of the medial meniscus by keeping the previously extruded meniscus inside the joint.17 Potential complications of this technique include irritation on the tibia around the fixation device and repair failure.
Success after meniscal root repair surgery with an anatomic transtibial double-tunnel pullout technique is reported to be high, with only 6.7% of patients requiring revision surgery.18,30 In the event of a retear, revision repair surgery has been reported to have encouraging outcomes.31 Although biomechanical studies have reported that both transtibial single- and double-tunnel tunnel pullout techniques are able to restore the native contact pressures of the knee after root repair, we advocate the transtibial double-tunnel technique, particularly in the revision setting, because it provides broader coverage on the anatomic footprint.32,33
In complete type II radial meniscal root tears, disruption of the characteristic hoop stress causes the meniscus to extrude outside the joint soon after injury.2,34 Meniscal extrusion has been reported to be more prevalent in medial meniscal root tears than in lateral meniscal root tears.35,36 Furthermore, it has been linked to more severe cartilage degeneration and, subsequently, subjective arthritic symptoms.12,37, 38, 39, 40 Previous studies have shown that certain refixation techniques for meniscal root repair do not always address meniscal extrusion.16,41, 42, 43 Failure to reapproximate the meniscus back into the joint has been speculated to allow further progression of cartilage degeneration and does not fully restore the native knee kinematics.43,44 No previous clinical studies have described a surgical technique to specifically address meniscal extrusion by providing a secondary fixation point for the meniscus inside the joint.17
This Technical Note describes an approach for anatomic revision repair of a posterior medial meniscal root tear with significant extrusion. The use of a peripheral stabilization suture through an additional transtibial tunnel at the apex of the posterior horn may help prevent additional extrusion of the meniscal tissue outside the joint. Although this technique has shown success biomechanically,17 further clinical and radiographic studies are needed to assess both the clinical outcomes and radiographic success of meniscal root repairs with peripheral stabilization.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. receives grant support from Arthrex, Linvatec, Ossur, and Smith & Nephew and receives personal fees from Arthrex, Ossur, and Smith & Nephew, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Our team’s technique for revision medial meniscal root repair using the transtibial double-tunnel pullout technique with a peripheral stabilization suture is described. Magnetic resonance imaging is used preoperatively to identify the meniscal root tear, nonanatomic location of the previous repair, and severe extrusion of the medial meniscus. The patient is placed in the supine position on the operating table, with the nonsurgical limb flexed and abducted and the surgical limb flexed and allowed to hang freely. Next, standard anterolateral and anteromedial portals are established. A spinal needle can be used for trephination, or pie-crusting, of the superficial medial collateral ligament to improve visualization of the medial compartment. The anatomic root attachment site on the tibial plateau is decorticated with an arthroscopic shaver, curved curette, and ablation device (Ambient Super Turbovac 90; Smith & Nephew) until healthy bony bleeding is observed. A sufficient peripheral release is then performed using arthroscopic scissors along the meniscocapsular junction. By use of an arthroscopic grasper, the meniscus is positioned back into the joint, and the root is reapproximated to its anatomic attachment. Externally, a skin incision is made on the tibia, 5 cm distal to the joint line and just medial to the tibial tubercle. Next, the tibial tunnel is drilled using a tibial drill guide and cannula, and the guide pin is aimed at the anatomic footprint. A second guide pin is then placed approximately 5 mm from the first guide pin at the root attachment site. A curved suture-passing device is used to place a suture tape through the meniscus, and the tape is shuttled through the transtibial tunnel cannula. The second suture is then passed in a similar fashion through the second tunnel. Before the sutures are tied down, a transtibial tunnel is drilled at the periphery of the tibial plateau and a guide pin is placed, just inferior to the apex of the posteromedial aspect of the posterior horn of the medial meniscus. Next, a straight suture-passing device is used to pass a suture through the apex of the posterior horn of the medial meniscus at the level of the guide pin. The suture is first passed from the tibial side to the femoral side. By use of the same end of the suture, the suture-passing device is reloaded, inverted, and re-advanced into the meniscus approximately 2 mm from the initial pass. The second pass of the same suture travels from the femoral side to the tibial side. The double-loaded suture construct is then shuttled through the transtibial tunnel. The 2 root repair suture tapes are tied over a single cortical button. The peripheral stabilization suture tape is tied over a separate cortical button. The repair is then observed and probed. The portal sites and distal tibial incision are closed in the standard manner. Finally, rehabilitation protocols are summarized.
References
- 1.LaPrade C.M., James E.W., Cram T.R., Feagin J.A., Engebretsen L., LaPrade R.F. Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 2.Pache S., Aman Z.S., Kennedy M. Meniscal roots: Current concepts review. Arch Bone Jt Surg. 2018;6:250–259. [PMC free article] [PubMed] [Google Scholar]
- 3.Chahla J., LaPrade R.F. Meniscal root tears. Arthroscopy. 2019;35:1304–1305. doi: 10.1016/j.arthro.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 5.Faucett S.C., Geisler B.P., Chahla J. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: Clinical and economic effectiveness. Am J Sports Med. 2019;47:762–769. doi: 10.1177/0363546518755754. [DOI] [PubMed] [Google Scholar]
- 6.Samuelsen B.T., Aman Z.S., Kennedy M.I. Posterior medial meniscus root tears potentiate the effect of increased tibial slope on anterior cruciate ligament graft forces. Am J Sports Med. 2020;48:334–340. doi: 10.1177/0363546519889628. [DOI] [PubMed] [Google Scholar]
- 7.Kennedy M.I., Strauss M., LaPrade R.F. Injury of the meniscus root. Clin Sports Med. 2020;39:57–68. doi: 10.1016/j.csm.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Hussain Z.B., Chahla J., Mandelbaum B.R., Gomoll A.H., LaPrade R.F. The role of meniscal tears in spontaneous osteonecrosis of the knee: A systematic review of suspected etiology and a call to revisit nomenclature. Am J Sports Med. 2019;47:501–507. doi: 10.1177/0363546517743734. [DOI] [PubMed] [Google Scholar]
- 9.Steineman B.D., LaPrade R.F., Santangelo K.S., Warner B.T., Goodrich L.R., Haut Donahue T.L. Early osteoarthritis after untreated anterior meniscal root tears: An in vivo animal study. Orthop J Sport Med. 2017;5 doi: 10.1177/2325967117702452. 2325967117702452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.LaPrade R.F., LaPrade C.M., James E.W. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23:71–76. doi: 10.5435/JAAOS-D-14-00003. [DOI] [PubMed] [Google Scholar]
- 11.Cinque M.E., Chahla J., Moatshe G., Faucett S.C., Krych A.J., LaPrade R.F. Meniscal root tears: A silent epidemic. Br J Sports Med. 2018;52:872–876. doi: 10.1136/bjsports-2017-098942. [DOI] [PubMed] [Google Scholar]
- 12.Matheny L.M., Ockuly A.C., Steadman J.R., LaPrade R.F. Posterior meniscus root tears: Associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23:3127–3131. doi: 10.1007/s00167-014-3073-7. [DOI] [PubMed] [Google Scholar]
- 13.LaPrade C.M., Jansson K.S., Dornan G.J., Smith S.D., Wijdicks C.A., LaPrade R.F. Altered tibiofemoral contact mechanics due to pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 14.Costa C.R., Morrison W.B., Carrino J.A. Medial meniscus extrusion on knee MRI: Is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183:17–23. doi: 10.2214/ajr.183.1.1830017. [DOI] [PubMed] [Google Scholar]
- 15.Berthiaume M.J., Raynauld J.P., Martel-Pelletier J. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LaPrade C.M., Foad A., Smith S.D. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43:912–920. doi: 10.1177/0363546514566191. [DOI] [PubMed] [Google Scholar]
- 17.Daney B.T., Aman Z.S., Krob J.J. Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med. 2019;47:1591–1600. doi: 10.1177/0363546519844250. [DOI] [PubMed] [Google Scholar]
- 18.Padalecki J.R., Jansson K.S., Smith S.D. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42:699–707. doi: 10.1177/0363546513499314. [DOI] [PubMed] [Google Scholar]
- 19.Stärke C., Kopf S., Gröbel K.H., Becker R. The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: A biomechanical study. Arthroscopy. 2010;26:358–365. doi: 10.1016/j.arthro.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Cerminara A.J., LaPrade C.M., Smith S.D., Ellman M.B., Wijdicks C.A., LaPrade R.F. Biomechanical evaluation of a transtibial pull-out meniscal root repair: Challenging the bungee effect. Am J Sports Med. 2014;42:2988–2995. doi: 10.1177/0363546514549447. [DOI] [PubMed] [Google Scholar]
- 21.DePhillipo N.N., Dean R.S., LaPrade R.F. Medial meniscus root repair in patients with open physes. Arthrosc Tech. 2020;9:e723–e728. doi: 10.1016/j.eats.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johannsen A.M., Civitarese D.M., Padalecki J.R., Goldsmith M.T., Wijdicks C.A., LaPrade R.F. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40:2342–2347. doi: 10.1177/0363546512457642. [DOI] [PubMed] [Google Scholar]
- 23.DePhillipo N.N., Kennedy M.I., Chahla J., LaPrade R.F. Type II medial meniscus root repair with peripheral release for addressing meniscal extrusion. Arthrosc Tech. 2019;8:e941–e946. doi: 10.1016/j.eats.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dubois de Mont-Marin G., Babusiaux D., Brilhault J. Medial collateral ligament lengthening by standardized pie-crusting technique: A cadaver study. Orthop Traumatol Surg Res. 2016;102:S209–S212. doi: 10.1016/j.otsr.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Chahla J., Moulton S.G., LaPrade C.M., Dean C.S., LaPrade R.F. Posterior meniscal root repair: The transtibial double tunnel pullout technique. Arthrosc Tech. 2016;5:e291–e296. doi: 10.1016/j.eats.2016.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steineman B.D., LaPrade R.F., Haut Donahue T.L. Loosening of transtibial pullout meniscal root repairs due to simulated rehabilitation is unrecoverable: A biomechanical study. Arthroscopy. 2019;35:1232–1239. doi: 10.1016/j.arthro.2018.11.041. [DOI] [PubMed] [Google Scholar]
- 27.Abraham A.C., Villegas D.F., Kaufman K.R., Haut Donahue T.L. Internal pressure of human meniscal root attachments during loading. J Orthop Res. 2013;31:1507–1513. doi: 10.1002/jor.22408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Becker R., Wirz D., Wolf C., Göpfert B., Nebelung W., Friederich N. Measurement of meniscofemoral contact pressure after repair of bucket-handle tears with biodegradable implants. Arch Orthop Trauma Surg. 2005;125:254–260. doi: 10.1007/s00402-004-0739-5. [DOI] [PubMed] [Google Scholar]
- 29.Mueller B.T., Moulton S.G., O’Brien L., LaPrade R.F. Rehabilitation following meniscal root repair: A clinical commentary. J Orthop Sports Phys Ther. 2016;46:104–113. doi: 10.2519/jospt.2016.6219. [DOI] [PubMed] [Google Scholar]
- 30.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 31.Fuchs A., Kloos F., Bode G., Izadpanah K., Südkamp N.P., Feucht M.J. Isolated revision meniscal repair—Failure rates, clinical outcome, and patient satisfaction. BMC Musculoskelet Disord. 2018;19:446. doi: 10.1186/s12891-018-2368-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim J.G. Editorial commentary: Save the meniscal root, why not? Arthroscopy. 2019;35:2207–2210. doi: 10.1016/j.arthro.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 33.LaPrade C.M., LaPrade M.D., Turnbull T.L., Wijdicks C.A., LaPrade R.F. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015;43:899–904. doi: 10.1177/0363546514563278. [DOI] [PubMed] [Google Scholar]
- 34.Furumatsu T., Kodama Y., Kamatsuki Y., Hino T., Okazaki Y., Ozaki T. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29:295–301. doi: 10.5792/ksrr.17.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Koo J.H., Choi S.H., Lee S.A., Wang J.H. Comparison of medial and lateral meniscus root tears. PLoS One. 2015;10 doi: 10.1371/journal.pone.0141021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ding C., Martel-Pelletier J., Pelletier J.P. Knee meniscal extrusion in a largely non-osteoarthritic cohort: Association with greater loss of cartilage volume. Arthritis Res Ther. 2007;9:R21. doi: 10.1186/ar2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee D.H., Lee B.S., Kim J.M. Predictors of degenerative medial meniscus extrusion: Radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19:222–229. doi: 10.1007/s00167-010-1274-2. [DOI] [PubMed] [Google Scholar]
- 38.Kijima H., Yamada S., Nozaka K., Saito H., Shimada Y. Relationship between pain and medial meniscal extrusion in knee osteoarthritis. Adv Orthop. 2015;2015:210972. doi: 10.1155/2015/210972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kijima H., Miyakoshi N., Kasukawa Y. Cut-off value of medial meniscal extrusion for knee pain. Adv Orthop. 2017;2017:6793026. doi: 10.1155/2017/6793026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ellman M.B., LaPrade C.M., Smith S.D. Structural properties of the meniscal roots. Am J Sports Med. 2014;42:1881–1887. doi: 10.1177/0363546514531730. [DOI] [PubMed] [Google Scholar]
- 41.Chung K.S., Ha J.K., Ra H.J., Kim J.G. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24:1455–1468. doi: 10.1007/s00167-015-3832-0. [DOI] [PubMed] [Google Scholar]
- 42.Feucht M.J., Kühle J., Bode G. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: A systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31:1808–1816. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 43.Chung K.S., Ha J.K., Yeom C.H. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: A minimum 5-year follow-up. Arthroscopy. 2015;31:1941–1950. doi: 10.1016/j.arthro.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 44.Papalia R., Vasta S., Franceschi F., D’Adamio S., Maffulli N., Denaro V. Meniscal root tears: From basic science to ultimate surgery. Br Med Bull. 2013;106:91–115. doi: 10.1093/bmb/ldt002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Our team’s technique for revision medial meniscal root repair using the transtibial double-tunnel pullout technique with a peripheral stabilization suture is described. Magnetic resonance imaging is used preoperatively to identify the meniscal root tear, nonanatomic location of the previous repair, and severe extrusion of the medial meniscus. The patient is placed in the supine position on the operating table, with the nonsurgical limb flexed and abducted and the surgical limb flexed and allowed to hang freely. Next, standard anterolateral and anteromedial portals are established. A spinal needle can be used for trephination, or pie-crusting, of the superficial medial collateral ligament to improve visualization of the medial compartment. The anatomic root attachment site on the tibial plateau is decorticated with an arthroscopic shaver, curved curette, and ablation device (Ambient Super Turbovac 90; Smith & Nephew) until healthy bony bleeding is observed. A sufficient peripheral release is then performed using arthroscopic scissors along the meniscocapsular junction. By use of an arthroscopic grasper, the meniscus is positioned back into the joint, and the root is reapproximated to its anatomic attachment. Externally, a skin incision is made on the tibia, 5 cm distal to the joint line and just medial to the tibial tubercle. Next, the tibial tunnel is drilled using a tibial drill guide and cannula, and the guide pin is aimed at the anatomic footprint. A second guide pin is then placed approximately 5 mm from the first guide pin at the root attachment site. A curved suture-passing device is used to place a suture tape through the meniscus, and the tape is shuttled through the transtibial tunnel cannula. The second suture is then passed in a similar fashion through the second tunnel. Before the sutures are tied down, a transtibial tunnel is drilled at the periphery of the tibial plateau and a guide pin is placed, just inferior to the apex of the posteromedial aspect of the posterior horn of the medial meniscus. Next, a straight suture-passing device is used to pass a suture through the apex of the posterior horn of the medial meniscus at the level of the guide pin. The suture is first passed from the tibial side to the femoral side. By use of the same end of the suture, the suture-passing device is reloaded, inverted, and re-advanced into the meniscus approximately 2 mm from the initial pass. The second pass of the same suture travels from the femoral side to the tibial side. The double-loaded suture construct is then shuttled through the transtibial tunnel. The 2 root repair suture tapes are tied over a single cortical button. The peripheral stabilization suture tape is tied over a separate cortical button. The repair is then observed and probed. The portal sites and distal tibial incision are closed in the standard manner. Finally, rehabilitation protocols are summarized.