Abstract
Medial patellofemoral ligament (MPFL) reconstruction usually involves hamstring autografts and is associated with donor-site morbidity. Excellent short-term results with MPFL reconstruction using synthetic materials have been reported. Although synthetics do not sacrifice autologous tissues, their material properties are significantly different from those of biological tissues. Therefore, accurate surgical procedures are required to achieve excellent results. The purpose of this report was to describe our surgical method for MPFL reconstruction using FiberTape and knotless SwiveLock anchors.
The medial patellofemoral ligament (MPFL) is the primary ligamentous stabilizer that prevents lateral patella dislocations. Therefore, MPFL reconstructions are a logical treatment approach for lateral patellar instability,1 and the clinical results are excellent with a low re-dislocation rate.2 Although autografts, such as hamstring tendons, are most commonly used for MPFL reconstruction, they have the disadvantage of donor-site morbidity. Synthetic materials do not sacrifice autologous tissues3 and provide excellent mid-term results.4 However, synthetics have not become popular as an alternative graft option.
Recently, the use of polyester suture tape (FiberTape; Arthrex, North Naples, FL) with knotless anchors (SwiveLock; Arthrex) for MPFL reconstruction has been reported.5,6 FiberTape with SwiveLock anchors has stronger ultimate load than a hamstring tendon with soft anchors7; however, it stiffness is significantly different from that of autologous tissue.7 This is both an advantage and a disadvantage in MPFL reconstruction. One of the possible complications of synthetics is an overconstrained patellofemoral (PF) joint, which may result in prolonged postoperative rehabilitation, anterior knee pain, and degenerative change of the PF joint. The purpose of this Technical Note was to describe MPFL reconstruction using FiberTape and SwiveLock anchors in detail.
Technique
Surgical Indication
Patients with lateral patellar instability but without severe bony anomalies are good candidates for this procedure. Patients with high-grade trochlear dysplasia (Dejour type D), severe PF osteochondral damage, and skeletal immaturity are contraindicated. Bony anomalies, such as patella alta and increased tibial tubercle–trochlear groove distance (>25 mm), may necessitate concomitant bony procedures in addition to the MPFL reconstruction.
Examination Under Anesthesia and Lateral Retinacular Release
Examination under anesthesia is routinely performed to assess patellar tracking and lateral retinacular tightness. Then, diagnostic arthroscopy is performed to assess patellar tracking and intra-articular lesions. If necessary, any concomitant lesions are treated. If lateral retinacular tightness is present, lateral retinacular release (LRR) is performed. We prefer to perform LRR using Metzenbaum scissors from the anterolateral portal. After LRR, patellar tracking and improvement of lateral tilt are confirmed.
Medial Patellofemoral Ligament Reconstruction (With Video Illustration)
A demonstration of the surgical procedure is provided in Video 1. The patient is placed in the supine position, and the knee is maintained at 90° of flexion (figure-4 position) (Fig 1A). Precise lateral view of the knee joint is confirmed using an image intensifier. The MPFL femoral insertion is radiographically found anterior to the intersection of the posterior femoral cortical line and the posterior margin of the medial femoral condyle or anterior to the posterior cortex of the femur and proximal to Blumensaat’s line, which is identified as Schöttle’s point.1
Fig 1.
Patient position and skin incisions. (A) The patient is placed in the supine position, and the knee (left knee) is maintained at 90° of flexion (figure-4 position). (B) Two skin incisions are needed (anteromedial side of the left knee): the first incision is a 2- to 3-cm straight longitudinal incision on the medial border of the patella (arrowheads), and the second is a short incision over the medial femoral epicondyle (arrow).
For this procedure, 2 skin incisions are needed (Fig 1B). A 2- to 3-cm straight longitudinal skin incision is made on the medial border of the patella. Then, the medial retinaculum (the first layer) is also incised, and the vastus medialis obliquus (VMO) is identified (Fig 2 A and B). The periosteum of the medial side of the patella is cut, and the medial edge is exposed. A second short incision is made over the medial epicondyle, and a subcutaneous tunnel is created between the first and second incisions. The MPFL is located in this second layer.
Fig 2.
Identification of the MPFL layer (left knee, medial view). (A) The medial retinaculum (the first layer) is incised, and the VMO is identified. (B) Anatomy of the MPFL. The MPFL is located in this second layer. (AD, abductor tubercle; GC, medial gastrocnemius insertion; ME, medial epicondyle; MPFL, medial patellofemoral ligament; VMO, vastus medialis obliquus.)
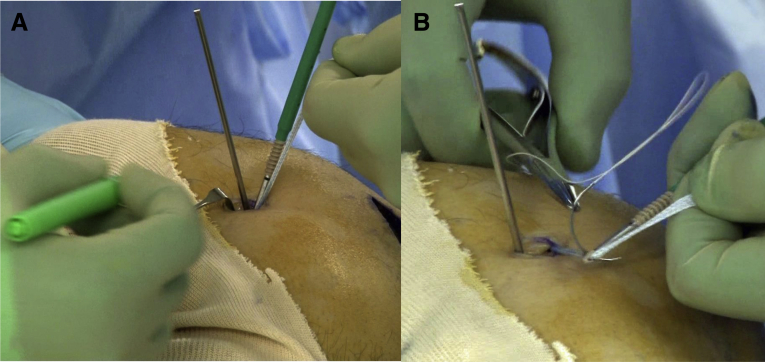
Through the first incision, 2 blind tunnels are prepared for a 3.5-mm SwiveLock anchor by predrilling and tapping as per the manufacturer’s technical instructions (Fig 3 A and B). The central portion of FiberTape is fixed with two 3.5-mm SwiveLock anchors on the medial side of the patella. The fixation points are proximal to the quadrisect and distal to the middle of the medial edge of the patella.
Fig 3.
Patellar fixation of FiberTape (left knee, medial view). (A) Fixation points on the patella are confirmed under image guidance. (B) The central portion of the FiberTape (the blue tape) is fixed with two 3.5-mm SwiveLock anchors on the medial side of the patella.
Through the second incision, a 2.4-mm Kirschner wire is inserted into Schöttle’s point. This point is confirmed under imaging guidance using the MPFL guide (JBM0200-01/2; BEAR Medic Corp., Tokyo, Japan) (Fig 4). The 2 free ends of the FiberTape are tunneled extra-articularly (second layer) from the first to the second incision and temporally fixed around the pin by a Kocher clamp. The isometry of the FiberTape and patellar tracking are checked by going through the full range of motion. If the pin position is appropriate, the 2 free ends of the FiberTape are passed through the eyelet of the SwiveLock anchor. The depth of the FiberTape position is marked at 60° to 90° of knee flexion (Fig 5A). If there is no isometric difference between flexion at 60° and 90°, 90° of flexion is recommended, as the patella is stable in the patellar groove. Then, a temporal suture is placed on the FiberTape to prevent movement within the eyelet and is fixed at the thumb holder (Fig 5B). The Kirschner wire is overdrilled using a 4.0- or 4.5-mm cannulated drill to a depth of 25 mm. The FiberTape is fixed using 4.75-mm knotless anchor on the femoral side while the patella is maintained in the center of the patellar groove (Fig 6). During final fixation, the knee should be maintained at 60° to 90° of flexion. The FiberTape should be slightly looser than the MPFL to prevent overtensioning when the fixation is completed. After fixation, arthroscopy is performed to assess patellar tracking. If the patella is overtightened, we remove the femoral SwiveLock and fix the FiberTape again.
Fig 4.
Confirmation of femoral insertion of MPFL (left knee, medial view). Schöttle’s point is confirmed under image guidance (A) using the MPFL guide (JBM0200-01/2; BEAR Medic Corp., Tokyo, Japan) (B). (MPFL, medial patellofemoral ligament.)
Fig 5.
Determination of FiberTape length (left knee, medial view). (A) The depth of the FiberTape position is marked with the knee at 60° of flexion and then at 90° of flexion. (B) A temporal suture is placed on the FiberTape to prevent movement within the eyelet.
Fig 6.
FiberTape fixation at the femur (left knee, medial view). The 2 free ends of the FiberTape are fixed with a 4.75-mm knotless anchor on the femoral side while the patella is kept in the center of the patellar groove.
The excised periosteum of the patella should be tightly sutured with no. 2-0 VICRYL stitches (Ethicon, Somerville, NJ) that cover the FiberTape, to ensure biological fixation (Fig 7). The retinaculum is also sutured. The skin incisions are closed using skin tapes.
Fig 7.
Suturing of the periosteum with FiberTape (left knee, medial view). The excised periosteum (arrows) is tightly sutured with no. 2-0 VICRYL covering FiberTape (arrowheads) to ensure biological fixation.
Postoperative Rehabilitation
Since the SwiveLock anchor fixation system provides secure initial fixation,7 patients are allowed full weight-bearing with crutches from the first day after surgery. Early range of motion and muscle control exercises, such as patellar setting and straight leg raising, are also started as soon as possible. Patients can jog at 2 months after surgery and participate in sports activities if their neuromuscular function has recovered. Advantages and disadvantages as well as pearls and pitfalls of this procedure are summarized in Tables 1 and 2.
Table 1.
Advantages and Disadvantages of MPFL Reconstruction Using FiberTape and Knotless SwiveLock Anchors
| Advantages | Disadvantages |
|---|---|
| Minimal incision | Synthetic materials |
| No graft harvest | Possibility of irritation |
| Strong initial fixation | Stiffer than native MPFL |
| Simple and reliable | |
| Facilitates postoperative rehabilitation |
MPFL, medial patellofemoral ligament.
Table 2.
Pearls and Pitfalls of MPFL Reconstruction Using FiberTape and Knotless SwiveLock Anchors
| Pearls | Pitfalls |
|---|---|
| Patients without severe bony abnormalities are good candidates. | Overtensioning of the FiberTape increases PFJ pressure,9 which results in PFJ pain and prolonged postoperative rehabilitation |
| Use of an image intensifier is recommended for precise femoral placement | Nonanatomic MPFL femoral placement is a risk factor for unsuccessful surgery1 |
| A temporal suture should be placed over the FiberTape to prevent movement within the eyelet of the SwiveLock anchor | |
| The FiberTape should be fixed at 60° to 90° of knee flexion without tensioning9 |
MPFL, medial patellofemoral ligament; PFJ, patellofemoral joint.
Discussion
We started using the FiberTape and SwiveLock anchors for MPFL reconstruction in 2016, and our short-term results were almost satisfactory. However, a few of the early patients needed a relatively long time to regain full range of motion compared with those who underwent conventional MPFL reconstruction using a hamstring autograft. During that period, we fixed the suture tape at approximately 45° of knee flexion, similar to our conventional procedure. We believe that overtensioning of the MPFL resulted in prolonged postoperative rehabilitation.
Although tension of the graft in MPFL reconstruction is affected by the knee fixation angle during graft fixation, the optimal fixation angle remains unknown. It may also be affected by the graft material property and graft fixation method. During MPFL reconstruction using synthetics (Leeds-Leio artificial ligament), Nomura et al.4 recommended using a tension spacer between the synthetics and the femur during fixation at 60° of knee flexion to avoid overtensioning, whereas Ellera Gomes3 recommended 90° of knee flexion for synthetic fixation. Lee et al.,5 who first reported MPFL reconstruction using FiberTape and SwiveLock anchors, recommended 20° of knee flexion while applying adequate tension to the graft under arthroscopic guidance. Hopper et al.6 stated the importance of avoiding excessive constraint of the suture tape since overtension leads to irritation and quadriceps inhibition. However, they did not determine the optimal knee flexion angle. For autogenous tissue reconstruction, graft fixation angles ranging from 0° to 90° have been recommended as optimal by several authors.1 Regardless of the degree of knee flexion, the MPFL should tighten only on lateral patellar translation.
Maintaining normal PF contact pressure after surgery is important to avoid compromising the PF joint. Lorbach et al.8 recommended 60° of knee flexion for gracilis tendon fixation in anatomical MPFL reconstruction, based on their biomechanical study of PF joint pressure. The effect of the knee flexion angle on PF contact pressure in MPFL reconstruction using FiberTape and SwiveLock anchors was previously investigated.9 The normalized maximum contact pressure of the medial PF joint fixed at either 0° or 30° significantly increased in deep knee flexion. Conversely, the normalized maximum contact pressure fixed at 60° and 90° remained at the same level as the intact knees at all knee flexion angles. FiberTape fixed by SwiveLock anchors was stiffer than native MPFL.7 Therefore, the suture tape should be fixed at >60° of knee flexion to avoid excessive PF joint contact pressure.
The femoral positioning of the graft and graft tension are critical steps for the overall outcome of MPFL reconstruction.1 A small displacement of the femoral fixation point dramatically changes the force and pressure to the medial PF cartilage. We have been performing postoperative 3-dimensional computed tomography, and there has been no malpositioning in our series (Fig 8). Since SwiveLock fixation does not need an oblique femoral tunnel like ENDOBUTTON fixation, a guidewire can be perpendicularly inserted into the femoral tunnel under image control. This leads to accurate graft placement, which is an advantage of this technique. Patellar fracture is one of the complications to avoid. Two small blind tunnels for 3.5-mm SwiveLock anchors may not decrease the strength of the patella and prevent patella fracture, and this is another advantage of this technique.
Fig 8.
Postoperative computed tomography image of the left knee (medial view). The femoral fixation point is located between the AD and the ME (arrowhead). The patellar fixation points are proximal to the quadricet and distal to the middle of the medial edge of the patella (arrows). (AD, abductor tubercle; ME, medial epicondyle.)
There are some limitations to this procedure. Since synthetics cannot be replaced by autologous tissue, the long-term effects on the knee joint are unknown. According to a mid-term follow-up study reported by Nomura et al.,4 MPFL reconstruction using synthetics is safe and achieves favorable results. Since the FiberTape fixed by SwiveLock anchors was stiffer than the native MPFL, minor malpositioning is a risk factor for technical failure. Further clinical studies are necessary to determine the long-term results of this procedure.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows important steps for MPFL reconstruction using FiberTape and knotless SwiveLock anchors.
ICMJE author disclosure forms
References
- 1.Sanchis-Alfonso V. Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J Am Acad Orthop Surg. 2014;22:175–182. doi: 10.5435/JAAOS-22-03-175. [DOI] [PubMed] [Google Scholar]
- 2.Lippacher S., Dreyhaupt J., Williams S.R., Reichel H., Nelitz M. Reconstruction of the medial patellofemoral ligament: Clinical outcomes and return to sports. Am J Sports Med. 2014;42:1661–1668. doi: 10.1177/0363546514529640. [DOI] [PubMed] [Google Scholar]
- 3.Ellera Gomes J.L. Medial patellofemoral ligament reconstruction for recurrent dislocation of the patella: A preliminary report. Arthroscopy. 1992;8:335–340. doi: 10.1016/0749-8063(92)90064-i. [DOI] [PubMed] [Google Scholar]
- 4.Nomura E., Horiuchi Y., Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee. 2000;7:211–215. doi: 10.1016/s0968-0160(00)00072-7. [DOI] [PubMed] [Google Scholar]
- 5.Lee P.Y.F., Golding D., Rozewicz S. Modern synthetic material is a safe and effective alternative for medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:2716–2721. doi: 10.1007/s00167-017-4711-7. [DOI] [PubMed] [Google Scholar]
- 6.Hopper G.P., Heusdens C.H.W., Dossche L., Mackay G.M. Medial patellofemoral ligament repair with suture tape augmentation. Arthrosc Tech. 2019;8:e1–e5. doi: 10.1016/j.eats.2018.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsushima T., Tsukada H., Saaki S. Biomechanical analysis of medial patellofemoral ligament reconstruction: FiberTape® with knotless anchors versus a semitendinosus tendon autograft with soft anchors. J Orthop Sci. 2019;24:663–667. doi: 10.1016/j.jos.2018.11.018. [DOI] [PubMed] [Google Scholar]
- 8.Lorbach O., Haupert A., Efe T. Biomechanical evaluation of MPFL reconstructions: Differences in dynamic contact pressure between gracilis and fascia lata graft. Knee Surg Sports Traumatol Arthrosc. 2017;25:2502–2510. doi: 10.1007/s00167-016-4005-5. [DOI] [PubMed] [Google Scholar]
- 9.Sakamoto Y., Sasaki S., Kimura Y., Yamamoto Y., Tsuda E., Ishibashi Y. Patellofemoral contact pressure for medial patellofemoral ligament reconstruction using suture tape varies with the knee flexion angle: A biomechanical evaluation. Arthroscopy. 2020;36:1390–1395. doi: 10.1016/j.arthro.2019.12.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows important steps for MPFL reconstruction using FiberTape and knotless SwiveLock anchors.
ICMJE author disclosure forms