Abstract
Introduction
It is important to ascertain the cost-effectiveness of alternative services to traditional cardiac rehabilitation while the economic credentials of the Smartphone Cardiac Rehabilitation, Assisted self-Management (SCRAM) programme among people with coronary heart disease (CHD) are unknown. This economic protocol outlines the methods for undertaking a trial-based economic evaluation of SCRAM in the real-world setting in Australia.
Methods and analysis
The within-trial economic evaluation will be undertaken alongside a randomised controlled trial (RCT) designed to determine the effectiveness of SCRAM in comparison with the usual care cardiac rehabilitation (UC) alone in people with CHD. Pathway analysis will be performed to identify all the costs related to the delivery of SCRAM and UC. Both a healthcare system and a limited societal perspective will be adopted to gauge all costs associated with health resource utilisation and productivity loss. Healthcare resource use over the 6-month participation period will be extracted from administrative databases (ie, Pharmaceutical Benefits Scheme and Medical Benefits Schedule). Productivity loss will be measured by absenteeism from work (valued by human capital approach). The primary outcomes for the economic evaluation are maximal oxygen uptake (VO2max, mL/kg/min, primary RCT outcome) and quality-adjusted life years estimated from health-related quality of life as assessed by the Assessment of Quality of Life-8D instrument. The incremental cost-effectiveness ratio will be calculated using the differences in costs and benefits (ie, primary and secondary outcomes) between the two randomised groups from both perspectives with no discounting. All costs will be valued in Australian dollars for year 2020.
Ethics and dissemination
The study protocol has been approved under Australia’s National Mutual Acceptance agreement by the Melbourne Health Human Research Ethics Committee (HREC/18/MH/119). It is anticipated that SCRAM is a cost-effective cardiac telerehabilitation programme for people with CHD from both a healthcare and a limited societal perspective in Australia. The evaluation will provide evidence to underpin national scale-up of the programme to a wider population. The results of the economic analysis will be submitted for publication in a peer-reviewed journal.
Trial registration number
Australian New Zealand Clinical Trials Registry (ACTRN12618001458224).
Keywords: health economics, rehabilitation medicine, myocardial infarction, coronary heart disease
Strengths and limitations of the study.
Health economics data will be collected prospectively along with a randomised controlled trial (RCT) to reliably capture the individual-level healthcare resource use and changes in productivity.
National administrative data collection (ie, Medicare and Pharmaceutical Benefits Scheme Australia) will be extracted to source the healthcare resource utilisation over the trial duration.
The economic evaluation is based on the sample size determined by the primary outcome of the Smartphone Cardiac Rehabilitation, Assisted self-Management RCT, which may be underpowered to detect a difference in costs.
Introduction
Cardiac rehabilitation (CR) is an effective multifactorial secondary prevention intervention that is typically delivered in centre-based (ie, face to face) settings. Centre-based CR reduces recurrent ischaemic events, improves health-related quality of life (HRQoL) and long-term prognosis for patients with coronary heart disease (CHD).1–3 CR programmes have also been reported to reduce overall premature mortality (relative risk (RR) 0.87, 95% CI 0.75 to 0.99) and cardiac deaths (RR 0.74 (95% CI 0.63 to 0.87) in comparison with no CR.4 Despite effectiveness of CR, many people with CHD do not engage in such programmes.5 For instance, CR utilisation is low in Australia; uptake (attended ≥1 session) and completion rates have been estimated at 25%–60% and 19%–42%, respectively, across the country; uptake rates as low as 10% have been reported in Victoria.6–9 Reasons underlying poor participation are complex, but accessibility barriers such as limited programme availability, transport restrictions, conflicting domestic/occupational responsibilities and geographic isolation are key contributors.10–13
For these reasons, clinicians and researchers have been prompted to seek novel strategies for delivering CR programmes to facilitate greater uptake and adherence rates. Telerehabilitation—defined as rehabilitation services that are delivered remotely through information and communication technologies—has received increasing attention as it can overcome key accessibility barriers that limit participation in centre-based CR. The effectiveness of telerehabilitation, which commonly includes telephone, internet and videoconference communication between participants and healthcare practitioners,14 has been demonstrated. Systematic reviews have consistently shown that telerehabilitation services improve cardiovascular disease (CVD) risk factors (ie, total cholesterol, blood pressure, high-density and low-density lipoprotein), compared with controls10 15; and comparisons of traditional centre-based CR with telerehabilitation have shown them to be equivalent in terms of mortality, exercise capacity and quality-of-life outcomes.16 The effectiveness of CR interventions delivered via telephone, internet and videoconference has been well established; however, few trials have capitalised on opportunities to augment intervention design and delivery by using rapidly advancing mobile communication and device technologies (ie, mobile broadband and smartphones; mHealth). Four randomised controlled trials (RCTs) have compared mHealth CR with traditional centre-based programmes. One study showed improved uptake and completion rate in comparison with the control group,17 two indicated mHealth and centre-based CR had comparable effects on maximal oxygen uptake (ie, exercise capacity),18 19 while the fourth suggested mHealth CR led to improvements in maximal oxygen uptake and quality of life.20 The results from existing economic evaluations of mHealth intervention are not consistent.18 19 21 22
We are currently undertaking a multicentre RCT of a smartphone-based platform to support remotely delivered CR called Smartphone Cardiac Rehabilitation, Assisted self-Management (SCRAM). Unlike its predecessor the remotely monitored exercise-based cardiac telerehabilitation (REMOTE-CR),18 SCRAM extends beyond a single behaviour (exercise) to include other secondary prevention self-management behaviours (medication adherence, physical activity and sedentary behaviour, healthy eating, stress management and smoking cessation). To establish the economic credentials of the SCRAM programme in the Australian setting, an economic evaluation will be conducted to examine the balance between health effects and costs of health technologies (ie, SCRAM programme, medications, diagnostic tests and medical services) to inform efficient allocation of limited healthcare funding. In response to the transparent reporting of clinical trials, this paper outlines the methods of the prospective within-trial economic evaluation to be undertaken alongside the RCT,23 to provide important evidence for policy decision-making around the provision of CR services. It will include both cost-effectiveness and cost-utility analysis (CUA) with a view to informing resource allocation, practice change and investment in the SCRAM programme. This planned economic evaluation aims to provide the evidence around the cost-effectiveness of tele-CR, assessing its value for money in Australian context.
Methods
Design
The details of the study design are reported elsewhere.23 Briefly, SCRAM is a multicentre investigator-blinded, assessor-blinded and statistician-blinded parallel two-arm RCT comparing effects and costs of the 24-week SCRAM intervention with usual care CR. A process evaluation is also being undertaken. Participants are randomised (1:1) to receive either SCRAM (intervention) or usual care CR (control).
The study protocol was prospectively registered with the Australian New Zealand Clinical Trials Registry on 30 August 2018 and adhered to the SPIRIT 2013 statement.24 The intervention has been described according to the recommendations in the Template for Intervention Description and Replication (TIDieR) and Consolidated Standards of Reporting Trials (CONSORT) (eHealth extension) statements. Reporting of trial outcomes will adhere to the CONSORT statement and its eHealth extension.25–27
The economic evaluation will be undertaken from both an Australian healthcare system plus a limited societal perspective, incorporating all healthcare costs subsidised by state and Commonwealth governments in Australia. In addition, participant absenteeism from work due to CHD will be monetised and the associated cost will be included in the estimation from the limited societal perspective. The reporting of this economic evaluation will adhere to the Consolidated Health Economic Evaluation Reporting Standards guidelines.28
Study population
A total of 220 participants (N=110 per randomised group) diagnosed with CHD within the previous 6 months are being recruited from hospitals, outpatient clinics and CR services in Sunshine, Geelong and Bendigo, Victoria, Australia. As study centres provide treatment to ~1.5 million individuals across broad catchment areas, the trial cohort is anticipated to include a geographically diverse mix of metropolitan-dwelling, regional-dwelling and rural-dwelling participants.
Participants are randomised (1:1) to receive the SCRAM programme (intervention) or usual care CR (control), stratified by sex and study centre. Key inclusion criteria at baseline are: aged over 18 years; diagnosed CHD within the previous 6 months (angina, myocardial infarction or coronary revascularisation); outpatients who have been clinically stable for at least 6 weeks; able to perform exercise; and can understand and write English. Exclusion criteria include: New York Heart Association functional class III/IV heart failure; terminal disease; significant non-CHD exercise limitations; and contraindications for maximal exercise testing.
Patient and public involvement
There is not patient and public involvement.
Sample size
The target sample will provide 90% power at a 5% significance level (two sided) to detect a clinically meaningful difference of 2.0 mL/kg/min in V̇O2max at 24 weeks (primary RCT outcome) between the control and intervention groups, assuming an SD of 6.75, a correlation of 0.8 between the preintervention and postintervention measures and 20% loss to follow-up. Minimum detectable differences in secondary RCT outcomes are outlined in the main trial protocol.23
Baseline assessment
Prior to randomisation, researchers collect the following information: sociodemographic and clinical (diagnostic, smoking, alcohol history and medication) characteristics, eHealth literacy (a questionnaire), V̇O2max and secondary outcomes (detailed below).
Randomisation
Treatment allocation follows a computer-generated schedule prepared by a biostatistician who is not involved with recruitment, treatment allocation or outcome assessment.23 Investigators, outcome assessors and the statistician remain blinded to the group allocation over the course of the trial.
Treatment arms
Usual care CR
Usual care CR typically includes face-to-face support/education to adhere to medical treatment and health-promoting lifestyle behaviours as well as supervised exercise training. Specific programme components vary across Australian healthcare providers but most offer education and exercise components29; stratification of treatment allocation by trial centre will ensure variation is balanced across treatment groups. It is unclear how many participants will opt for both SCRAM and usual care CR; nevertheless, widespread low uptake of centre-based CR suggests very few patients randomised to SCRAM programme will seek to complete both programmes.13 To explore impact on trial outcomes, self-reported usual care CR utilisation for patients assigned to SCRAM programme will be assessed.
Usual care CR is not delivered as part of this trial. All participants retain access to usual care CR—regardless of treatment allocation—as it is unethical to withhold evidence-based treatment. Participants randomised to the control group have access to usual care CR alone, as offered by their local CR provider, without further support.
Intervention: SCRAM programme
Participants randomised to the intervention group receive the 24-week dual-phase SCRAM intervention, which is described in detail in the main trial protocol.23 Briefly, during an initial 12-week intensive phase, participants receive real-time remotely prescribed, supervised and coached exercise training from accredited exercise physiologists as well as a modular multifactorial library of evidence-based and theory-based behaviour change support push notifications. This phase is designed to provide intensive support for exercise and lifestyle behaviour uptake and adherence. During a subsequent 12-week maintenance phase, participants receive reduced frequency and intensity of exercise and behaviour change support. This phase is designed to provide tapered support that transitions participants towards long-term self-determined adherence to exercise and health-promoting lifestyle behaviours. Participants receive all intervention components via the bespoke SCRAM software platform, using an Android smartphone.
Comparator
It is important for the economic evaluation to be able to ascertain whether the planned intervention is conducted in addition to existing practices, or as a replacement to them. Consistent with the RCT design,23 SCRAM intervention will be compared with usual care CR (ie, traditional centre-based CR).
Measurement of clinical endpoints
Outcome measures for the within-trial economic evaluation
Primary outcomes for the economic evaluation will be maximal oxygen uptake (V̇O2max, mL/kg/min, primary RCT outcome)—measured during an individualised treadmill cardiopulmonary exercise test—and HRQoL—measured using the Assessment of Quality of Life-8D (AQoL-8D). The Australian tariff for AQoL-8D will be used to estimate the quality-adjusted life year (QALY) gains for individual participant.30 V̇O2max is measured at baseline and 24-week follow-up, while HRQoL is assessed at baseline, 12 and 24 weeks. Secondary outcomes, including modifiable cardiovascular risk factors and adverse events, are described in the main trial protocol.23
Measurement of costs
Direct cost of delivering the SCRAM programme
In identifying relevant costs, the following principles will be adhered to:
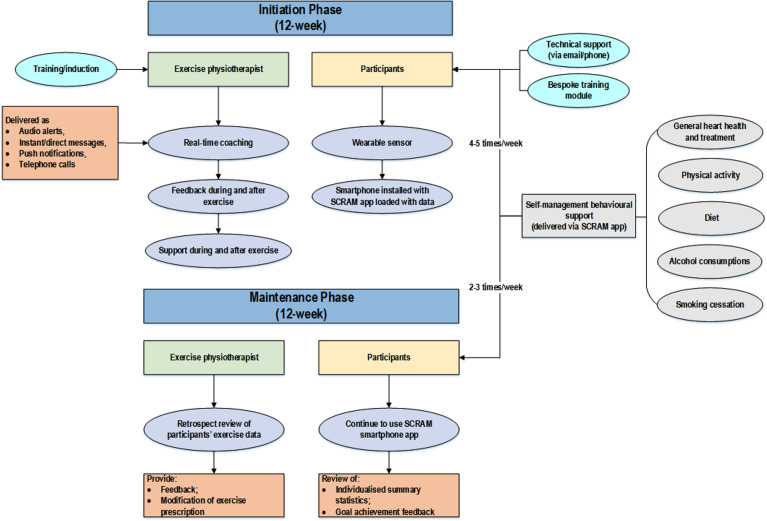
Identification of costs to be included, using ‘pathway analysis’ (figure 1), where activities in all stages of the roll out of the SCRAM project are fully specified; A healthcare system perspective and steady state operation of the intervention will be assumed (intervention is up and running, and start-up costs, such as development of SCRAM app will be excluded). Costs will largely relate to the time costs of the remote exercise physiologists and project staff (using opportunity cost principles). Any administrative resources used at the programme management level also will be identified and included. Cost items identified from pathway analysis are summarised in table 1.
Measurement of the resources consumed in natural units (number of hours spent by remote exercise physiologists to deliver the intervention, etc).
Valuation of these resources in monetary units (Australian dollars), using 2020 as the reference year.
Figure 1.
Pathway analysis for identifying the cost associated with SCRAM programme delivery. SCRAM, Smartphone Cardiac Rehabilitation, Assisted self-Management.
Table 1.
Identified cost items according to pathway analysis
| Process to be costed | Identification of costs | Measurement of costs | Valuation of costs | Who records cost data and how is it collected |
| Recruitment of participants | Researcher | Minutes/hours | Salary costs | Researcher records time taken |
| Training | ||||
| Training/induction session for participants | Project team time | Hours | Salary costs | Project team records time taken |
| Training/induction session for accredited exercise physiologist | Project team time | Hours | Salary costs | Project team records time taken |
| Capital | ||||
| Leasing of venue for training/induction sessions | Cost of leasing | Unit cost | Market price | Research team to record |
| Leasing of venues for CR professionals to deliver the SCRAM programme | Cost of leasing | Unit cost | Market price | Research team to record |
| Wearable sensor devices | Cost of sensor device | Unit cost | Market price | Research team to record |
| Smartphone | Cost of smartphone | Unit cost | Market price | Research team to record |
| Computers (desktop or laptop) | Cost of computer | Unit cost | Market price | Research team to record |
| Staffing | ||||
| CR professional | CR professional time | Hours | Salary costs | CR professional records time taken |
| Administrative support | Project staff time | Hours | Salary costs | Project staff records time taken |
| Miscellaneous costs | ||||
| Mobile phone/internet access | Cost of mobile phone, internet access | Unit cost | Market price | Research team to record |
| Stationery | Cost of stationery | Unit cost | Market price | Research team to record |
| Utilities (ie, electricity) | Cost of utility | Unit cost | Market price | Research team to record |
| Hosting (server) | Cost of server | Unit cost | Market price | Research team to record |
| Handouts (flyer and information sheet, etc) | Cost of printing | Unit cost | Market price | Research team to record |
CR, cardiac rehabilitation;SCRAM, Smartphone Cardiac Rehabilitation, Assisted self-Management.
Direct health costs of participants
Beside intervention cost, healthcare-related costs including inpatient and outpatient care associated with CHD are documented. The cost of inpatient care over the 24-week participation period (eg, emergency department (ED) visits and rehospitalisations will be estimated from self-reported adverse events documented throughout the trial. Complementary approaches will be used to calculate the cost for each hospitalisation episode: first, the cost per hospital admission from the National Hospital Cost Data Collection (actual cost per Australian refined diagnosis-related groups, AR-DRG) will be used; second the National Efficient Price (projected cost) according the AR-DRG code31 will be used to value the per hospitalisation episode adjusted for the length of hospital stay. The cost of outpatient care (eg, outpatient consultations, examinations) and medication use over the 24-week participation period will be estimated from Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Schedule (PBS) data, respectively.
Productivity cost (absenteeism from work)
Absence from work (ie, days of sick leave) due to CHD is self-reported by participants of working age (ie, ≤65 years old; people post working age do not attract productivity loss from a societal perspective) using a predesigned questionnaire at baseline and 24-week follow-up. The human capital approach will be used to value the productivity cost.32
Exclusion of trial costs
Research-driven activities will be separated from the activities that would be carried out should the programme be adopted by the healthcare system. Costs associated with trial administration, data collection and RCT outcome assessment will be excluded.
Data analysis
Within-trial economic evaluation
The within-trial economic evaluation will be based on the intention-to-treat population as per the primary outcome of the RCT.23 In particular, completers data will be used for the base-case analysis, whereas the imputed data analysis (using multiple missing data imputation approach, with the assumption that missingness is at random) will be undertaken to examine the robustness of base-case results. All evaluation results will be expressed as incremental results over and above the comparator case. In other words, the additional cost/saving of the intervention (SCRAM) compared with current practice will be expressed as a ratio by dividing by the net benefits derived. The following formula represents the calculation of the incremental cost-effectiveness ratio (ICER):
ICER=Ci−CUC/Bi−BUC, where C=costs, B=benefits, i=SCRAM intervention and UC=usual care CR.
For the cost-effectiveness analysis (CEA), the incremental cost per unit increase in benefits for both the primary and secondary outcomes will be calculated if significant between-group differences are observed. For the CUA, the QALY will be estimated from HRQoL assessed by AQoL-8D by intervention group (table 2). A plot on the cost-effectiveness plane will be drawn to illustrate the distribution of costs and effectiveness. A cost-effectiveness acceptability curve will also be plotted in order to assess the degree of uncertainty associated with the conclusion using a predetermined empirical willingness-to-pay threshold for the QALY outcome (ie, $A50 000/QALY).33
Table 2.
Expected outcomes of the economic analysis
| Analysis | Incremental costs | Incremental effectiveness | Incremental cost-effectiveness |
| Incremental cost-effectiveness analysis | AUD | Maximal oxygen uptake (VO2max, mL/kg/min) | Cost of per unit improvement in VO2max |
| AUD | Anthropometry (ie, body weight, BMI and waist/hip circumference, etc*) | Cost of per unit improvement in anthropometry outcomes | |
| AUD | Blood lipid and glucose concentrations, blood pressure | Cost per unit improvement in biomedical outcomes | |
| Incremental cost-utility analysis | AUD | QALY gained | Cost per additional QALY gained |
*Complete list of secondary outcomes could be found in the trial protocol.23
AUD, Australian dollar; BMI, body mass index; QALY, quality-adjusted life year.
Bootstrap simulation of the costs and ICER will be used to simulate the study results over 2000 iterations. This technique is used when data are skewed (cost data are nearly always highly skewed) and the CI of a ratio using skewed data is required. The within-trial economic analysis will be undertaken using STATA V.15 (StataCorp. 2017. Stata Statistical Software: Release V.15. College Station, Taxes, USA: StataCorp LLC).
Long-term modelling
Model-based long-term CEA of SCRAM versus usual care CR will be undertaken if the primary outcome (VO2max) from the RCT is proven to significantly increase. The VO2max will be converted to the reduction in overall mortality (ie, OR in mortality for 1 metabolic equivalents increase). The difference (if any, observed from the RCT) in the incidence of recurrent CVD post the index MI will also be used to model the long-term health and cost outcomes associated with the application of the two modes of CR. Benefits observed in the trial will be translated into health benefits (eg, avoided morbidity/mortality outcomes, and calculated in terms of QALY gained). The modelled economic evaluation will simulate the impact of increased maximal oxygen uptake on the overall well-being/survival of the cohort over its lifetime compared with the control group. A Markov model consisting of health states associated with CHD (ie, recurrent myocardial infarction, angina, revascularisation, stroke or death) will be used to accrue costs and benefits over the lifetime horizon. The long-term improved outcomes may translate into the cost savings due to avoided ED visit and rehospitalisation. Long-term modelling will be performed in TreeAge Pro 2019.
Sensitivity analysis
Uncertainty analyses will be conducted based on Monte Carlo simulations. The between-group differences in both costs and QALY will be bootstrapped to estimate the probability of the SCRAM programme being cost-effective regardless of the significance in between-group difference.34 A series of one-way sensitivity analyses will be undertaken to examine robustness of the base-case ICER, for example, alternative costing approach for rehospitalisation (unit costs derived from Independent Hospital Pricing Authority, Australia; Australian Institute of Health and Well-being), labours (unit costs sourced from Australia Bureau of Statistics, PayScale) and SCRAM intervention delivery (varying the quantity and unit cost of the resource used).
Ethics approval
The study protocol has been approved under the Australia’s National Mutual Acceptance agreement by the Melbourne Health Human Research Ethics Committee (HREC/18/MH/119). Ethics approval has been ratified by the Deakin University Human Research Ethics Committee (2018-251). All participants provide written informed consent prior to undertaking baseline assessments. Separate consent is sought to extract MBS/PBS data for the purpose of this study.
Discussion
This paper details the protocol of a trial-based economic evaluation that purports to assess the cost-effectiveness of the SCRAM telerehabilitation programme among people with CHD. It has a number of methodological strengths, the key one being that the economic evaluation will be undertaken alongside a prospective RCT. This has the advantage of being efficient and timely in terms of the data collected. In addition, the RCT design provides credibility through high internal validity, minimisation of bias and tight protocol control. The SCRAM RCT aims to minimise the predictable sources of bias and confounding via allocation concealment, blinded outcome assessment and intention-to-treat analysis. The primary costing data will be sourced from administrative databases including MBS, PBS and hospital costing system data; this allows for maximum accuracy of the data collected and enhances the capture of effects and outcomes. Furthermore, this RCT is recruiting participants from metropolitan, regional and rural areas of Victoria, Australia, allowing for broader representativeness of participants that will maximise generalisability of the results. Lastly, HRQoL will be assessed by the AQoL-8D, a 35-item questionnaire, which has been widely applied in measuring HRQoL for Australia-based studies.35–38 It has increased measurement sensitivity, especially in the psychosocial dimensions, compared with existing instruments (ie, EuroQol-5D-5L, Quality of Well-being, Health Utilities Index Mark 3 and 15D) that vary greatly and report inconsistent utility scores.39 Further, undertaking both completers and imputed data analyses for the trial-based economic evaluation will increased the validity of the results given the potential significant proportion of missingness in follow-up cost and QALY data. The trial-based economic evaluation only had a short 24-week timeframe and was based on the trial under strictly controlled research conditions. It cannot answer the long-term cost-effectiveness of SCRAM programme, which is pivotal for the reimbursement decision-making. The model-based economic evaluation that extrapolates the short-term trial outcome to the lifetime horizon and a real-world setting will inform the cost-effectiveness of the proposed programme in the Australian context.
The economic credentials of traditional centre-based CR versus no CR have long been established. A systematic review of 19 CEAs of such interventions concluded that the majority reported traditional CR was cost-effective versus no CR (ICER ranged from US$1065 to US$71755/QALY), especially with exercise as a component.40 41 Specifically in relation to cardiac telerehabilitation (not involving a smartphone-based REMOTE-CR component), studies are varied in terms of their results. While one within-trial economic evaluation reported that such an intervention (offering the flexibility of having the CR at hospital, healthcare centre or call centre) was not cost-effective given its high cost (ICER €400 000 per QALY),21 others have demonstrated more positive outcomes. A trial-based economic analysis home-based CR was associated with non-significantly lower costs and a high probability of being cost-effective.19 Another CUA showed that the mean cost per patient in a telemonitoring programme was €564 lower than in the control group, but with higher QALY gains (0.026), thereby making the intervention dominant (lower costs but higher benefits).22 Another CEA of home-based telerehabilitation, delivered through online videoconferencing for patients with heart failure, concluded that it was associated with significantly lower costs ($A−1590, 95% CI −$A2822 to −$A359) during the 6-month participation period.42 Our previous economic evaluation alongside a non-inferiority RCT in New Zealand indicated the REMOTE-CR smartphone-based cardiac telerehabilitation programme—a precursor to SCRAM—was associated with cost-saving (NZ$−4615/participant) and comparable benefits.18
Some methodological limitations are worth mentioning: first of all, the economic evaluation is based on the sample size determined by the primary outcome of the SCRAM RCT. It may be underpowered to detect a difference in costs. Second, while the gold standard is to undertake economic evaluations from a societal perspective (which captures all costs falling on patients, their carers and families), the current study only considers a limited societal perspective (ie, including only productivity costs); the costs borne by carers and families are excluded. However, it is believed that the healthcare system plus the limited societal perspectives will provide sufficient information to inform decision-making around investment in the SCRAM programme in Australia and elsewhere.
The results of this economic evaluation will fill the evidence gap for the cost-effectiveness of this mHealth CR programme versus usual care CR alone, given that the current economic credentials of a precursor intervention are based on a non-inferiority RCT.18 The results will assist policy makers, healthcare managers and other healthcare service providers to inform decisions regarding the ongoing use or future implementation of the SCRAM programme. If the economic evaluation finds the SCRAM programme to be cost-effective, then it can be recommended at the national or even international level as a complementary alternative CR delivery model that may meet the needs of many people who are unable or unwilling to participate in traditional centre-based CR services.
Supplementary Material
Footnotes
Twitter: @jrawstorn
Contributors: All the authors contributed to the study design and the protocol of the economic analysis. LG drafted the initial manuscript. RM, JR, KB, BO, CC, SM, KL, JA, VN, CN, SC and MM reviewed, edited and approved the final manuscript.
Funding: This study is funded by the Australian National Health and Medical Research Council (project grant 1144331).
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Montalescot G, Sechtem U, Achenbach S, et al. . Esc guidelines on the management of stable coronary artery disease. Eur Heart J 2013;34:2949. [DOI] [PubMed] [Google Scholar]
- 2.Anderson LJ, Taylor RS. Cardiac rehabilitation for people with heart disease: an overview of Cochrane systematic reviews. Int J Cardiol 2014;177:348–61. 10.1016/j.ijcard.2014.10.011 [DOI] [PubMed] [Google Scholar]
- 3.Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ 2015;351:h5000. 10.1136/bmj.h5000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fletcher GF, Ades PA, Kligfield P, et al. . Exercise standards for testing and training: a scientific statement from the American heart association. Circulation 2013;128:873–934. 10.1161/CIR.0b013e31829b5b44 [DOI] [PubMed] [Google Scholar]
- 5.Kotseva K, Wood D, De Backer G, et al. . Use and effects of cardiac rehabilitation in patients with coronary heart disease: results from the EUROASPIRE III survey. Eur J Prev Cardiol 2013;20:817–26. 10.1177/2047487312449591 [DOI] [PubMed] [Google Scholar]
- 6.Bunker S, McBurney H, Cox H, et al. . Identifying participation rates at outpatient cardiac rehabilitation programs in Victoria, Australia. J Cardiopulm Rehabil 1999;19:334–8. 10.1097/00008483-199911000-00001 [DOI] [PubMed] [Google Scholar]
- 7.Scott IA, Lindsay KA, Harden HE. Utilisation of outpatient cardiac rehabilitation in Queensland. Med J Aust 2003;179:341–5. 10.5694/j.1326-5377.2003.tb05588.x [DOI] [PubMed] [Google Scholar]
- 8.Worcester MUC, Murphy BM, Mee VK, et al. . Cardiac rehabilitation programmes: predictors of non-attendance and drop-out. Eur J Cardiovasc Prev Rehabil 2004;11:328–35. 10.1097/01.hjr.0000137083.20844.54 [DOI] [PubMed] [Google Scholar]
- 9.Johnson NA, Inder KJ, Nagle AL, et al. . Secondary prevention among cardiac patients not referred to cardiac rehabilitation. Med J Aust 2009;190:161. 10.5694/j.1326-5377.2009.tb02323.x [DOI] [PubMed] [Google Scholar]
- 10.Neubeck L, Freedman SB, Clark AM, et al. . Participating in cardiac rehabilitation: a systematic review and meta-synthesis of qualitative data. Eur J Prev Cardiol 2012;19:494–503. 10.1177/1741826711409326 [DOI] [PubMed] [Google Scholar]
- 11.Inglis SC, Clark RA, McAlister FA, et al. . Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev 2010;8:CD007228. [DOI] [PubMed] [Google Scholar]
- 12.Jones M, Jolly K, Raftery J, et al. . 'DNA' may not mean 'did not participate': a qualitative study of reasons for non-adherence at home- and centre-based cardiac rehabilitation. Fam Pract 2007;24:343–57. 10.1093/fampra/cmm021 [DOI] [PubMed] [Google Scholar]
- 13.Worringham C, Rojek A, Stewart I. Development and feasibility of a smartphone, ECG and GPs based system for remotely monitoring exercise in cardiac rehabilitation. PLoS One 2011;6:e14669. 10.1371/journal.pone.0014669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frederix I, Solmi F, Piepoli MF, et al. . Cardiac telerehabilitation: a novel cost-efficient care delivery strategy that can induce long-term health benefits. Eur J Prev Cardiol 2017;24:1708–17. 10.1177/2047487317732274 [DOI] [PubMed] [Google Scholar]
- 15.Jin K, Khonsari S, Gallagher R, et al. . Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review and meta-analysis. Eur J Cardiovasc Nurs 2019;18:260–71. 10.1177/1474515119826510 [DOI] [PubMed] [Google Scholar]
- 16.Clark RA, Conway A, Poulsen V, et al. . Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol 2015;22:35–74. 10.1177/2047487313501093 [DOI] [PubMed] [Google Scholar]
- 17.Varnfield M, Karunanithi M, Lee C-K, et al. . Smartphone-Based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: results from a randomised controlled trial. Heart 2014;100:1770–9. 10.1136/heartjnl-2014-305783 [DOI] [PubMed] [Google Scholar]
- 18.Maddison R, Rawstorn JC, Stewart RAH, et al. . Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart 2019;105:122–9. 10.1136/heartjnl-2018-313189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kraal JJ, Van den Akker-Van Marle ME, Abu-Hanna A, et al. . Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: Results of the FIT@Home study. Eur J Prev Cardiol 2017;24:1260–73. 10.1177/2047487317710803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frederix I, Hansen D, Coninx K, et al. . Medium-Term effectiveness of a comprehensive Internet-based and patient-specific Telerehabilitation program with text messaging support for cardiac patients: randomized controlled trial. J Med Internet Res 2015;17:e185. 10.2196/jmir.4799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kidholm K, Rasmussen MK, Andreasen JJ, et al. . Cost-Utility analysis of a cardiac Telerehabilitation program: the Teledialog project. Telemed J E Health 2016;22:553–63. 10.1089/tmj.2015.0194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frederix I, Hansen D, Coninx K, et al. . Effect of comprehensive cardiac telerehabilitation on one-year cardiovascular rehospitalization rate, medical costs and quality of life: a cost-effectiveness analysis. Eur J Prev Cardiol 2016;23:674–82. 10.1177/2047487315602257 [DOI] [PubMed] [Google Scholar]
- 23.Rawstorn JC, Ball K, Oldenburg B, et al. . Smartphone cardiac rehabilitation, assisted self-management (SCRAM) versus usual care: protocol for a multicentre randomised controlled trial to compare effects and costs among people with coronary heart disease. JMIR Res Protoc 2019:15022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chan A-W, Tetzlaff JM, Altman DG, et al. . Spirit 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eysenbach G, Consort-ehealth group . Consort-ehealth: improving and standardizing evaluation reports of web-based and mobile health interventions. J Med Internet Res 2011;13:e126. 10.2196/jmir.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffmann TC, Glasziou PP, Boutron I, et al. . Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 27.Schulz KF, Altman DG, Moher D, et al. . Consort 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Husereau D, Drummond M, Petrou S, et al. . Consolidated health economic evaluation reporting standards (cheers) statement. BMJ 2013;346:f1049. 10.1136/bmj.f1049 [DOI] [PubMed] [Google Scholar]
- 29.Jackson AC, Higgins RO, Murphy BM, et al. . Cardiac rehabilitation in Australia: a brief survey of program characteristics. Heart Lung Circ 2018;27:1415–20. 10.1016/j.hlc.2017.08.024 [DOI] [PubMed] [Google Scholar]
- 30.Richardson J, Sinha K, Iezzi A, et al. . Modelling utility weights for the Assessment of Quality of Life (AQoL)-8D. Qual Life Res 2014;23:2395–404. 10.1007/s11136-014-0686-8 [DOI] [PubMed] [Google Scholar]
- 31.Independent Hospital Pricing Authority Australia National efficient price determination 2018-19, 2018. Available: https://www.ihpa.gov.au/publications/national-efficient-price-determination-2018-19
- 32.Robinson R. Economic evaluation and health care. what does it mean? BMJ 1993;307:670–3. 10.1136/bmj.307.6905.670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang S, Gum D, Merlin T. Comparing the ICERs in medicine reimbursement submissions to NICE and PBAC-Does the presence of an explicit threshold affect the ICER proposed? Value Health 2018;21:938–43. 10.1016/j.jval.2018.01.017 [DOI] [PubMed] [Google Scholar]
- 34.Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ 1999;18:341–64. 10.1016/S0167-6296(98)00039-3 [DOI] [PubMed] [Google Scholar]
- 35.Dieng M, Cust AE, Kasparian NA, et al. . Protocol for a within-trial economic evaluation of a psychoeducational intervention tailored to people at high risk of developing a second or subsequent melanoma. BMJ Open 2016;6:e012153. 10.1136/bmjopen-2016-012153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chatterton ML, Mihalopoulos C, O'Neil A, et al. . Economic evaluation of a dietary intervention for adults with major depression (the "SMILES" trial). BMC Public Health 2018;18:599. 10.1186/s12889-018-5504-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gao L, Flego A, Dunstan DW, et al. . Economic evaluation of a randomized controlled trial of an intervention to reduce office workers’ sitting time: the "Stand Up Victoria" trial. Scand J Work Environ Health 2018;44:503–11. 10.5271/sjweh.3740 [DOI] [PubMed] [Google Scholar]
- 38.Harding KE, Watts JJ, Karimi L, et al. . Improving access for community health and sub-acute outpatient services: protocol for a stepped wedge cluster randomised controlled trial. BMC Health Serv Res 2016;16:364. 10.1186/s12913-016-1611-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Richardson J, Iezzi A, Khan MA, et al. . Validity and reliability of the Assessment of Quality of Life (AQoL)-8D multi-attribute utility instrument. Patient 2014;7:85–96. 10.1007/s40271-013-0036-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shields GE, Wells A, Doherty P, et al. . Cost-Effectiveness of cardiac rehabilitation: a systematic review. Heart 2018;104:1403–10. 10.1136/heartjnl-2017-312809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Edwards K, Jones N, Newton J, et al. . The cost-effectiveness of exercise-based cardiac rehabilitation: a systematic review of the characteristics and methodological quality of published literature. Health Econ Rev 2017;7:37. 10.1186/s13561-017-0173-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hwang R, Morris NR, Mandrusiak A, et al. . Cost-Utility analysis of home-based Telerehabilitation compared with centre-based rehabilitation in patients with heart failure. Heart Lung Circ 2019;28:1795–803. 10.1016/j.hlc.2018.11.010 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.