Abstract
Objective
Overuse of diagnostic imaging for patients with low back pain remains common. The underlying beliefs about diagnostic imaging that could drive overuse remain unclear. We synthesised qualitative research that has explored clinician, patient or general public beliefs about diagnostic imaging for low back pain.
Design
A qualitative evidence synthesis using a thematic analysis.
Methods
We searched MEDLINE, EMBASE, CINAHL, AMED and PsycINFO from inception to 17 June 2019. Qualitative studies that interviewed clinicians, patients and/or general public exploring beliefs about diagnostic imaging for low back pain were included. Four review authors independently extracted data and organised these according to themes and subthemes. We used the Critical Appraisal Skills Programme tool to critically appraise included studies. To assess confidence in review findings, we used the GRADE-Confidence in the Evidence from Reviews of Qualitative Research method.
Results
We included 69 qualitative studies with 1747 participants. Key findings included: Patients and clinicians believe diagnostic imaging is an important test to locate the source of low back pain (33 studies, high confidence); patients with chronic low back pain believe pathological findings on diagnostic imaging provide evidence that pain is real (12 studies, moderate confidence); and clinicians ordered diagnostic imaging to reduce the risk of a missed diagnosis that could lead to litigation, and to manage patients’ expectations (12 studies, moderate confidence).
Conclusion
Clinicians and patients can believe that diagnostic imaging is an important tool for locating the source of non-specific low back pain. Patients may underestimate the harms of unnecessary imaging tests. These beliefs could be important targets for intervention.
PROSPERO registration number
CRD42017076047.
Keywords: qualitative research, back pain, magnetic resonance imaging
Strengths and limitations of this study.
This was a large systematic review that included 69 qualitative studies involving interviews with 1747 patients and clinicians.
Including both patient and clinicians allowed us to compare and contrast views and identify beliefs with confidence.
We used a comprehensive search strategy to identify relevant studies representing the phenomena of interest.
We only included English language studies.
We applied GRADE Confidence in the Evidence from Reviews of Qualitative Research to describe our confidence in the review findings.
Introduction
Imaging for low back pain is a frequently overused test. In one primary care cohort fewer than 1% of presentations had serious conditions that required immediate imaging.1 Yet physicians refer one in four patients with low back pain presenting to primary care, and one in three patients presenting to emergency care for imaging.2 Imaging is an important diagnostic tool for patients with clinical features of a serious and/or specific condition, such as an infection or spinal cord compromise, and where the results would alter management.3 However, for patients with non-specific low back pain (~95% of presentations in primary care), imaging does not improve outcomes and risks overdiagnosis and overtreatment.4
Overuse of imaging represents a substantial economic burden for low-income, middle-income and high-income countries. In the USA, there were 60 million lumbar radiographs in 2004, around one for every five US citizens5 (out-of-network charges per lumbar radiograph are US$404–US$565).6 In 2016, Australia spent $A243 million7 and Brazil spent US$13 million8 on lumbar radiographs, respectively. In the UK, £77 million was spent on lumbar radiographs in 2000.9 Advanced imaging can be particularly wasteful; a 2016 study of a US Veterans Affairs Healthcare facility estimated US$300 million is wasted on unnecessary lumbar MRIs each year.10
Attempts to reduce overuse of imaging have been largely unsuccessful.11 Although clinicians cite patient pressure and the desire for a definitive diagnosis as a reason for providing guideline-discordant imaging,12 it remains unclear what patients and clinicians believe the role of the imaging test is for people with low back pain. Surveys of patients attending primary care found that nearly 50% believed everyone with low back pain should undergo imaging,13 and 72% rated imaging to be important.14 While such survey studies provide insight into the prevalence of beliefs, they do not explore the underlying reasons for them. Without an in-depth understanding of beliefs about imaging, it will be difficult to design effective strategies to help clinicians manage patient demands and address potential drivers of overuse.
Objective
The objective of this review was to synthesise qualitative research that has explored clinician, patient or general public beliefs about diagnostic imaging for low back pain.
Methods
We searched MEDLINE, EMBASE, CINAHL, AMED and PsycINFO to locate relevant articles. We did an initial search from inception of each database until 22 September 2017 and updated our search on 17 June 2019. We used a comprehensive sampling strategy.15 To identify additional relevant papers, we conducted a manual search of reference lists of included studies and performed citation tracking of included studies using Web of Science, and contacted experts in the field through authors’ professional networks. Our full search strategy is available in online supplementary appendix 1. We have reported our study according to the Enhancing Transparency in Reporting the synthesis of Qualitative research statement.16 17
bmjopen-2020-037820supp001.pdf (5.9MB, pdf)
Two review authors (ACT and BR) screened titles and abstracts independently and performed a full-text review as necessary. Disagreements were resolved by discussion with a third reviewer (CB).
Inclusion criteria
We included studies if they: used qualitative methods for data collection and analysis; studied clinicians treating low back pain, or patients with any duration of low back pain (who may or may not have received diagnostic imaging), or sampled from the general public and interviewed participants about management of low back pain; explored beliefs about diagnostic imaging for low back pain; were conducted in any healthcare setting in any country; were published in English; and discussed diagnostic imaging of any type (eg, X-ray, CT scan, MRI).
Data extraction
To perform data extraction, three review authors (SS, ACT and CB) independently read a subset of seven included papers that were considered to have rich data on beliefs about imaging. The review authors then developed a preliminary list of themes, using NVivo for theme coding. The review team discussed and revised the preliminary list, and decided on the final list of themes, which then became our coding book. Four authors (ACT, SS, BR and MH) then independently extracted data (such as text extracts and participant quotes) from the included papers and organised these according to the themes and subthemes in the coding book. At least two authors coded each paper. The review team discussed any coding disagreements and agreed on the final organisation of data in the coding book. These steps formed part of the thematic analysis.
Critical appraisal
We used the Critical Appraisal Skills Programme (CASP) tool to assess the methodological limitations of included studies.18 The CASP tool takes into consideration items such as clarity of the aims, and the appropriateness and rigour of qualitative methods including research design, recruitment strategy, data collection method, consideration of the researcher–participant relationship, ethical issues, data analysis method, clarity of findings, and overall value of the research. Two reviewers (SS and ACT) independently applied the 10-item CASP tool to the included studies.
Assessing confidence in review findings
We summarised the robustness of the review findings following Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Confidence in the Evidence from Reviews of Qualitative Research (CERQual) method.19 To assess confidence in the review findings, two review authors (ACT and SS) independently assessed methodological limitations, relevance, coherence and adequacy of each of the main findings. For a detailed description of this process, please see the online supplement table S1.
Results
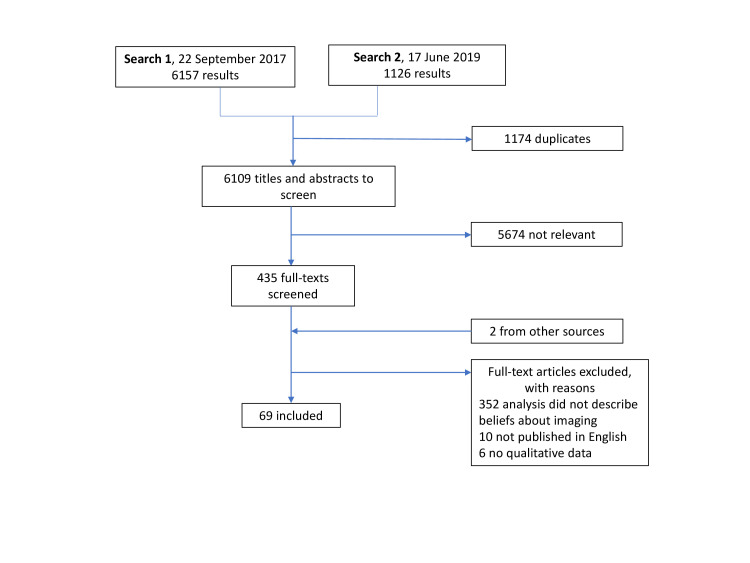
We included 69 studies (figure 1), 24 with clinicians (n=630),20–43 32 with patients (n=1072)14 44–74 13 with mixed samples of patients and clinicians (n=45) (table 1).75–87 Detailed characteristics of included studies can be found in online supplementary table S2.
Figure 1.
Selection of studies in review of beliefs about diagnostic imaging for low back pain.
Table 1.
Summary of study characteristics
| All (n=69 studies) | |
| Participants | 1747 |
| Clinicians (n, %) | |
| Total n=630 participants | |
| GPs | 337 (54) |
| Physiotherapists | 121 (19) |
| Chiropractors | 57 (9) |
| Medical specialists* | 24 (4) |
| Occupational therapists | 8 (1) |
| Other† | 83 (13) |
| Patients (n, %) | |
| Total n=1072 participants | |
| Acute low back pain | 38 (4) |
| Chronic low back pain | 515 (48) |
| Unspecified | 519 (48) |
| Mixed sample (n, %) | |
| Total n=45 participants | |
| Studies | 69 |
| Setting (n studies, %) | |
| Primary care | 46 (67) |
| Secondary care | 8 (11) |
| Tertiary care | 6 (9) |
| Mixed/not-specified | 9 (13) |
| Location (n studies, %) | |
| Europe | 42 (61) |
| Australia/New Zealand | 14 (20) |
| North America | 11 (16) |
| Asia | 2 (3) |
*Includes rehabilitation physicians(n=6), mixed group of specialists in neurology, rehabilitation medicine, orthopaedics, neurosurgery, rheumatology (n=14), pain specialist (n=4).
†Members of multidisciplinary rehabilitation team, profession not specified.
GPs, general practitioners.
Critical appraisal
Table 2 shows the results of the critical appraisal of included studies. The majority used appropriate qualitative methods (67 of 69, 97%), and research design (66 of 69, 96%). Around half of the studies appropriately reported the researcher–participant relationship (36 of 69, 52%), analysed the data in a rigorous way (32 of 69, 46%) and made a clear statement of their findings (35 of 69, 51%). Less than half of the studies (28 of 69, 41%) had clearly specified their research question and reported collecting data to achieve data saturation (online supplementary table S3).
Table 2.
Critical Appraisal Skill Programme (CASP) assessment of the methodological limitations of included studies
| CASP criteria | No* (%) (n=69) |
References of studies Reporting each criteria |
| 1. Was there a clear statement of the aims? | 64 (93) | 14 20–29 31–54 56 57 59–67 69–76 79–87 |
| 2. Is qualitative method appropriate? | 67 (97) | 14 20–29 31–35 37 38 40–57 59–67 69–77 79–87 |
| 3. Was the research design appropriate? | 66 (96) | 14 20 21 23 26 27 29–38 40 41 43–46 48–51 54–69 71–87 24 25 42 47 52 53 70 |
| 4. Was the recruitment strategy appropriate? | 49 (71) | 20 21 23 25–31 36–38 41–48 50 51 54 55 57–61 63–70 72–75 77 79 80 83–86 |
| 5. Was the data collected in a way that addressed the research issue? | 28 (41) | 23–28 32 34 36 41–44 47 50–52 54 57 61 64 69 70 74–77 85 |
| 6. Was the researcher-participant relationship considered? | 36 (52) | 20 21 26–28 32–34 36 37 41 42 45 47 50 57–61 63 65 67 69–74 77 81 83–87 |
| 7. Have the ethical issues been taken into consideration? | 51 (74) | 21–26 29–34 36–39 41–44 46 48–52 54–61 64 65 68–75 77 79–81 83 84 87 |
| 8. Was the data analysis sufficiently rigorous? | 32 (46) | 14 21 22 25–29 33 35 36 41 43–45 48 51 52 54–57 64 66 68 71 75–77 81 84 |
| 9. Is there a clear statement of findings? | 35 (51) | 20 22 23 25–27 32 36 38 41–54 57 61 64 65 69–71 75–77 79 85 |
| 10. How valuable is the research? | 50 (72) | 14 23 27 31–34 36–41 43 45–48 50–60 63–67 69–77 79 80 83–87 |
*Number of studies meeting the criterion.
Themes
Five major themes emerged from the thematic analysis: (1) Clinical presentation justifies imaging; (2) Perceptions that imaging has benefits to clinicians; (3) Perceptions that imaging has benefits to patients; (4) Imaging has potential harms and (5) Health system drivers. Online supplementary table S4 provides the full list of themes and sub-themes in each study.
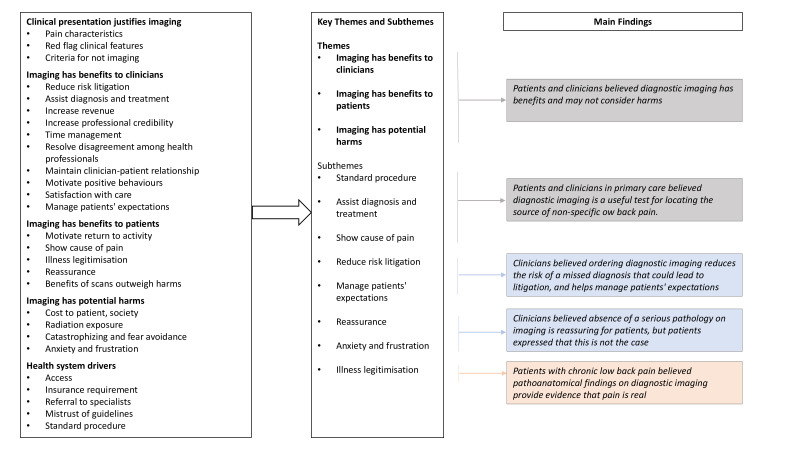
Summary of main findings
Below we describe five main findings based on our thematic analysis and subgroup analyses (figure 2). Based on our CERQual assessment, we found moderate to high confidence in our review findings, with high confidence in two review findings and moderate confidence in three review findings.
Figure 2.
Mapping of themes and subthemes to main findings. To summarise our main findings two review authors took the following three steps: (1) review all main analysis and subgroup analyses documents (left side of figure), (2) group findings into key themes and subthemes. (Middle panel) and (3) expand the concise headings of the key theme and sub-theme headings to include a more specific, detailed description of the phenomenon (right side of figure). The summary of findings statements were reviewed and refined by all authors.
1. Patients and clinicians in primary care believed diagnostic imaging is a useful test for locating the source of non-specific low back pain (33 studies, high confidence).
This belief arose strongly from the data. Irrespective of the pain duration, patients and clinicians (general practitioners (GPs), chiropractors and physiotherapists) felt it was possible to use diagnostic imaging to locate the source of low back pain. Chiropractors used imaging to assess alignment and guide treatment (eg, identifying which area of the spine to manipulate). Patients and clinicians in all healthcare settings expressed belief that diagnostic imaging is a useful test for non-specific low back pain:
X-rays help me visualize what I am going to do…it is one more piece of information. (Chiropractor)20
They couldn’t quite pick out where it was until the MRIs started and then they found it. (Patient)71
However, some clinicians expressed the contrary belief that imaging is an unreliable tool for locating the source of low back pain:
Well, a lot of them have got a perception [that] X-ray would show things, how they are getting the back problem, and I have to tell them time and time again, the X-ray actually will not show anything really, but this is the perception—it’s generalised. Most of them ask for an X-ray because they think it is a miracle diagnostic tool. It is not. (GP)82
2. Patients with chronic low back pain believed pathoanatomical findings on diagnostic imaging provide evidence that pain is real (12 studies, moderate confidence).
This finding emerged in data from patient participants with chronic low back pain, but not from those with acute low back pain. Patients with chronic low back pain felt the imaging legitimised their pain. They valued the physical evidence of pathology that imaging could provide; results they could use to convince their doctor, family, friends and colleagues that they were in pain. Pathological findings from diagnostic imaging could–paradoxically–bring a sense of relief to patients who felt stigmatised:
I kind of felt relieved. I felt like, well, here’s proof. It’s not just me going crazy or complaining. This is proof. It’s black and white, and anybody can see it. (Patient)63
This theme highlighted the role of diagnosis as a social phenomenon for people with low back pain.
3. Clinicians believed ordering diagnostic imaging reduces the risk of a missed diagnosis that could lead to litigation, and helps manage patients' expectations (12 studies, Moderate confidence).
Clinicians in primary care (GPs, chiropractors and physiotherapists) feared missing serious pathology. They mentioned referring patients for imaging even if it was not necessary to reduce the risk of litigation:
I always refer them for x-ray, not because I think there is anything broken, but purely down the line, and the ongoing medico-legal reports, and ‘did you send the patient for x-ray’, and the answer is yes, I have confirmation there is no bony injury. (GP)88
4. Clinicians believed absence of a serious pathology on imaging is reassuring for patients, but patients expressed that this is not the case (39 studies, moderate confidence).
Patients and clinicians believed that negative results provided reassurance to patients:
When patients worry, that is a heavy argument; you need the reassurance (gained from further tests) to go on with the patient. (GP)84
However, negative diagnostic imaging results were not always reassuring; some patient participants expressed frustration if they received results that ‘showed nothing.’ Diagnostic imaging results had the capacity to decrease distress. They could also increase distress if the results were inconclusive or if there were findings perceived to be permanent, degenerative or irreversible. Some clinicians appeared unaware of this negative consequence:
I think if people have a good understanding about where their problem’s coming from in the first place, that for their own piece of mind is a good thing and often they are concerned that what they have is a very serious problem, a life threatening problem and if they’ve got X-rays I explain on their X-rays. (Physio)41
5. Patients and clinicians believed diagnostic imaging has benefits and may not consider harms (63 studies, high confidence).
Clinicians focused on potential benefits, such as diagnosing the source of the pain, rather than potential harms such as radiation exposure, increased anxiety and overtreatment. Patients explicitly discussed potential harms in one study and expressed the view that perceived benefits outweighed any harms:
The only downside maybe… was the radiation, but that was the only negative. I think the less radiation you can be exposed to the better, but that having been said, the results justified that risk. I would rely on my doctor’s advice. (Patient)54
Discussion
Summary
Our review suggests that, despite guidelines recommending against the use of diagnostic imaging for non-serious low back pain for over three decades, some clinicians and their patients believe imaging is useful for locating the source of non-specific low back pain. Although clinicians appear to be aware of the downstream consequences of unnecessary imaging, patients rarely considered the potential for harm.
Strengths and limitations
This was a large systematic review that included 69 qualitative studies involving 1747 patients and clinicians. Including both patient and clinicians allowed us to compare and contrast views and identify key beliefs about imaging. We used a comprehensive search strategy to give us the best chance of locating all relevant studies representing the phenomena of interest although a limitation is that we only included English language studies. We adhered to a published protocol, which helps avoid duplication and promote transparency in our work. We applied GRADE CERQual to explain the confidence we had in our review findings.
GRADE CERQual is relatively new and not without limitations. The constructs that inform judgements of confidence in review findings (Methodological Limitations, Relevance, Adequacy, Coherence) can be challenging to measure and open to interpretation. For example, when assessing methodological limitations there is no gold-standard quality assessment tool nor is there specific guidance on including/excluding studies of low quality from reviews. There are also challenges with determining richness and coverage of data to assess Adequacy and Coherence; we acknowledge that a large amount of data does not necessarily guarantee saturation.89
We downgraded confidence in some of our findings for several reasons (online supplementary table S1). In terms of relevance, we included only a few studies primarily aimed to gather beliefs specifically about diagnostic imaging for low back pain. However, in all studies participants freely discussed the management of low back pain, and were given the opportunity to express their beliefs. In terms of adequacy, we located quotes relevant to beliefs that together provided rich data. We included studies with rehabilitation physicians, surgeons and occupational therapists as part of multidisciplinary teams, but were not able to separate quotes from these subgroups in the primary studies. This, we felt, reduced the coherence of some of our findings. However, the themes that emerged from studies of multidisciplinary teams were broadly consistent with the beliefs of the primary care physicians.
We did not find any qualitative studies examining general public beliefs about imaging for low back pain, but they are likely reflected in the beliefs of patients with low back pain who participated in the included studies. We also did not identify qualitative studies that examined beliefs of other specialists that commonly manage people with low back pain depending on setting, such as spine surgeons and other interventionalists. Understanding how closely their beliefs align with primary care clinicians is an important gap in the literature.
Comparison with existing literature
Other reviews of qualitative studies that focused on the experience of chronic pain found patients had a strong desire for a medical diagnosis in order to validate their pain.90–94 Toye et al identified a cultural need for a credible explanation of chronic pain, a need that makes it difficult for patients to give up the desire for a ‘diagnostic grail.’90 Our findings suggest that abandoning the desire for a diagnosis will be further complicated if both clinicians and patients believe that imaging can find the cause of the low back pain and legitimise the pain experience. However, we found that not all beliefs were congruent between patients and clinicians. Similar to a review by Hall et al, we found clinicians believed an absence of serious pathology on imaging provides reassurance to some patients.95 We have shown that this was not always true from the patient’s perspective; some patients with chronic low back pain seemed relieved by the presence of pathology on their imaging results—that is, the diagnostic grail. Indeed, a mega-ethnography by Toye et al found that patients with chronic musculoskeletal pain value having visual ‘proof’ in the form of imaging results to legitimise their invisible pain.94
While clinicians in our review mentioned the potential benefit of imaging to legitimise pain, we found the evidence that they were also aware of unintended harms such as the risk of disease labelling, catastrophising, overdiagnosis or overtreatment. Patients, on the other hand, did not appear to be aware of such harms. Previous reviews have suggested a clinician’s decision to ultimately pursue imaging is influenced by several complex factors including a belief that imaging is reassuring,95 misconceptions about clinical guidelines,12 and a desire to satisfy the patient.96 Our review suggests that a mismatch in beliefs and understanding about the harms of imaging could be an important new target for intervention.
A number of studies have evaluated approaches to reduce imaging rates. A Cochrane review97 found that there was little high quality evidence for interventions aimed at clinicians to improve the appropriateness of musculoskeletal imaging. However, there have been limited successes. A trial of providing feedback to GPs on their referral rates reduced imaging rates by 20%.98 Similarly, a 1987 trial found that combined patient education and a delayed referral approach reduced imaging rates by 59%.99 The latter study has never been replicated. Our findings suggest barriers to a delayed referral approach will include (1) a clinician’s belief that imaging is reassuring and (2) a patient’s belief that imaging is routine and can find the source of the pain. These beliefs could be useful targets for future strategies to reduce imaging. In addition, population approaches like mass media campaigns have also been found to shift both societal and clinician beliefs about low back pain towards more evidence-based approaches, although changing behaviours is more challenging.100–102 Population approaches, which have the advantage of simultaneously changing societal beliefs as a whole, remain an underused strategy that could enhance more targeted approaches.
Implications for research and practice
Beliefs about harms of imaging were much less frequently mentioned than beliefs about benefits of imaging. These beliefs are at odds with evidence that diagnostic imaging often adds little value to clinical decision making or patient outcomes. Therefore, these findings suggest a number of valuable areas for future inquiry. Education strategies for all clinicians who manage low back pain (GP, physiotherapists, chiropractors, specialists) are needed to address the widespread belief that imaging can reliably locate the source of low back pain. To address the role of imaging as a social phenomenon for people with low back pain, clinicians require strategies to legitimise a person’s pain experience without the use of diagnostic tests. Interventions to reduce guideline discordant imaging for low back pain should also consider potential social drivers of overuse such as clinician fear of litigation, patient expectations and the need for reassurance (figure 2). Such interventions might include targeted communication materials for the waiting room to address patient expectations and support conversations about the benefits and harms of these tests (box 1).
Box 1. Discussing imaging with a patient with low back pain.
Did you explain the limited ability of lumbar imaging to locate the source of pain?
Did you discuss potential harms of imaging?
Did you explore misperceptions expressed by your patient?
Did you give your patient enough time to discuss their concerns and did they feel listened to, valued and believed?
Conclusion
Clinicians and patients can believe that diagnostic imaging is an important tool for locating the source of low back pain. Patients may underestimate the harms of unnecessary imaging tests. These beliefs could be important drivers of overuse of imaging and key targets for intervention.
Supplementary Material
Footnotes
Twitter: @SweekritiSharma
Contributors: Study concept and design: ACT, BR, DAO, TH, CB, RB and CM. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: SS and ACT. Critical revision of the manuscript for important intellectual content: all authors. Analysis: all authors. Obtained funding: CM and RB. Study supervision: ACT and CM.
Funding: ACT is supported by an Australian Government National Health and Medical Research Council (NHMRC) Early Career Fellowship (APP1144026). DAO is supported by an NHMRC Translating Research into Practice Fellowship (APP1168749). TH is supported by an NHMRC Senior Research Fellowship (APP1154607). RB is supported by an NHMRC Senior Principal Research Fellowship (APP1082138). CM is supported by an NHMRC Principal Research Fellowship (APP1103022), a Programme Grant (APP1113532) and Centre for Research Excellence Grant (APP1113532).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as online supplementary information.
References
- 1. Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum 2009;60:3072–80. 10.1002/art.24853 [DOI] [PubMed] [Google Scholar]
- 2. Downie A, Hancock M, Jenkins H, et al. How common is imaging for low back pain in primary and emergency care? systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med 2020;54:642–51. 10.1136/bjsports-2018-100087 [DOI] [PubMed] [Google Scholar]
- 3. Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018;391:2368–83. 10.1016/S0140-6736(18)30489-6 [DOI] [PubMed] [Google Scholar]
- 4. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet 2018;391:2356–67. 10.1016/S0140-6736(18)30480-X [DOI] [PubMed] [Google Scholar]
- 5. Chou R, Deyo RA, Jarvik JG. Appropriate use of lumbar imaging for evaluation of low back pain. Radiol Clin North Am 2012;50:569–85. 10.1016/j.rcl.2012.04.005 [DOI] [PubMed] [Google Scholar]
- 6. Chou R, Qaseem A, Owens DK, et al. Diagnostic imaging for low back pain: advice for high-value health care from the American College of physicians. Ann Intern Med 2011;154:181–9. 10.7326/0003-4819-154-3-201102010-00008 [DOI] [PubMed] [Google Scholar]
- 7. Australian Government Department of Health MBS online: commonwealth of Australia. Available: http://www9.health.gov.au/mbs/search.cfm?q=spine&sopt=S
- 8. Carregaro RL, da Silva EN, van Tulder M. Direct healthcare costs of spinal disorders in Brazil. Int J Public Health 2019;64:965–74. 10.1007/s00038-019-01211-6 [DOI] [PubMed] [Google Scholar]
- 9. Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84:95–103. 10.1016/S0304-3959(99)00187-6 [DOI] [PubMed] [Google Scholar]
- 10. Avoundjian T, Gidwani R, Yao D, et al. Evaluating two measures of lumbar spine MRI overuse: administrative data versus chart review. J Am Coll Radiol 2016;13:1057–66. 10.1016/j.jacr.2016.04.013 [DOI] [PubMed] [Google Scholar]
- 11. Jenkins HJ, Hancock MJ, French SD, et al. Effectiveness of interventions designed to reduce the use of imaging for low-back pain: a systematic review. CMAJ 2015;187:401–8. 10.1503/cmaj.141183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Slade SC, Kent P, Patel S, et al. Barriers to primary care clinician adherence to clinical guidelines for the management of low back pain. Clin J Pain 2016;32:800–16. 10.1097/AJP.0000000000000324 [DOI] [PubMed] [Google Scholar]
- 13. Jenkins HJ, Hancock MJ, Maher CG, et al. Understanding patient beliefs regarding the use of imaging in the management of low back pain. Eur J Pain 2016;20:573–80. 10.1002/ejp.764 [DOI] [PubMed] [Google Scholar]
- 14. Espeland A, Baerheim A, Albrektsen G, et al. Patients' views on importance and usefulness of plain radiography for low back pain. Spine 2001;26:1356–63. 10.1097/00007632-200106150-00020 [DOI] [PubMed] [Google Scholar]
- 15. Arai L, Britten N, Popay J, et al. Testing methodological developments in the conduct of narrative synthesis: a demonstration review of research on the implementation of smoke alarm interventions. Evidence Policy 2007;3:361–83. 10.1332/174426407781738029 [DOI] [Google Scholar]
- 16. Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12:181. 10.1186/1471-2288-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Traeger AC, Reed BJ, O'Connor DA, et al. Clinician, patient and general public beliefs about diagnostic imaging for low back pain: protocol for a qualitative evidence synthesis. BMJ Open 2018;8:e019470. 10.1136/bmjopen-2017-019470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Critical Appraisal Skills Programme CASP systematic review checklist, 2018. Available: https://casp-uk.net/wp-content/uploads/2018/03/CASP-Systematic-Review-Checklist-2018_fillable-form.pdf
- 19. Lewin S, Glenton C, Munthe-Kaas H, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLoS Med 2015;12:e1001895. 10.1371/journal.pmed.1001895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ammendolia C, Bombardier C, Hogg-Johnson S, et al. Views on radiography use for patients with acute low back pain among chiropractors in an Ontario community. J Manipulative Physiol Ther 2002;25:511–20. 10.1067/mmt.2002.127075 [DOI] [PubMed] [Google Scholar]
- 21. Billis EV, McCarthy CJ, Stathopoulos I, et al. The clinical and cultural factors in classifying low back pain patients within Greece: a qualitative exploration of Greek health professionals. J Eval Clin Pract 2007;13:337–45. 10.1111/j.1365-2753.2006.00698.x [DOI] [PubMed] [Google Scholar]
- 22. Bond SJ, Soundy A. The influence of perceptions and beliefs of civilian physiotherapist working for the Ministry of defence in their management of back pain: an exploratory study using mixed methods. J R Army Med Corps 2012;158:14–21. 10.1136/jramc-158-01-05 [DOI] [PubMed] [Google Scholar]
- 23. Bussières AE, Patey AM, Francis JJ, et al. Identifying factors likely to influence compliance with diagnostic imaging guideline recommendations for spine disorders among chiropractors in North America: a focus group study using the theoretical domains framework. Implement Sci 2012;7:82. 10.1186/1748-5908-7-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Corbett M, Foster N, Ong BN. Gp attitudes and self-reported behaviour in primary care consultations for low back pain. Fam Pract 2009;26:359–64. 10.1093/fampra/cmp042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cowell I, O'Sullivan P, O'Sullivan K, et al. Perceptions of physiotherapists towards the management of non-specific chronic low back pain from a biopsychosocial perspective: a qualitative study. Musculoskelet Sci Pract 2018;38:113–9. 10.1016/j.msksp.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 26. Dahan R, Borkan J, Brown J-B, et al. The challenge of using the low back pain guidelines: a qualitative research. J Eval Clin Pract 2007;13:616–20. 10.1111/j.1365-2753.2007.00855.x [DOI] [PubMed] [Google Scholar]
- 27. Espeland A, Baerheim A. Factors affecting general practitioners' decisions about plain radiography for back pain: implications for classification of guideline barriers--a qualitative study. BMC Health Serv Res 2003;3:8. 10.1186/1472-6963-3-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Espeland A, Baerheim A. General practitioners' views on radiology reports of plain radiography for back pain. Scand J Prim Health Care 2007;25:15–19. 10.1080/02813430600973459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fullen BM, Doody C, David Baxter G, et al. Chronic low back pain: non-clinical factors impacting on management by Irish doctors. Ir J Med Sci 2008;177:257–63. 10.1007/s11845-008-0174-7 [DOI] [PubMed] [Google Scholar]
- 30. Langridge N, Roberts L, Pope C. The clinical reasoning processes of extended scope physiotherapists assessing patients with low back pain. Man Ther 2015;20:745–50. 10.1016/j.math.2015.01.005 [DOI] [PubMed] [Google Scholar]
- 31. Lin IB, Coffin J, O'Sullivan PB. Using theory to improve low back pain care in Australian Aboriginal primary care: a mixed method single cohort pilot study. BMC Fam Pract 2016;17:44. 10.1186/s12875-016-0441-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Macneela P, Gibbons A, McGuire B, et al. "We need to get you focused": general practitioners' representations of chronic low back pain patients. Qual Health Res 2010;20:977–86. 10.1177/1049732310364219 [DOI] [PubMed] [Google Scholar]
- 33. Miller JS, Pinnington MA. Straightforward consultation or complicated condition? general practitioners' perceptions of low back pain. Eur J Gen Pract 2003;9:3–9. 10.3109/13814780309160385 [DOI] [PubMed] [Google Scholar]
- 34. Nielsen M, Jull G, Hodges PW. Designing an online resource for people with low back pain: health-care provider perspectives. Aust J Prim Health 2016;22:159–66. 10.1071/PY14131 [DOI] [PubMed] [Google Scholar]
- 35. Palma Ruiz M, Conde Espejo P, Amate J, et al. PMS94 management and diagnosis of osteoporotic vertebral fractures according to primary care physicians. Value in Health 2009;12:A451 10.1016/S1098-3015(10)75232-3 [DOI] [Google Scholar]
- 36. Poitras S, Durand M-J, Côté A-M, et al. Guidelines on low back pain disability: interprofessional comparison of use between general practitioners, occupational therapists, and physiotherapists. Spine 2012;37:1252–9. 10.1097/BRS.0b013e31824b6adf [DOI] [PubMed] [Google Scholar]
- 37. Rogers WA. Whose autonomy? which choice? A study of GPs' attitudes towards patient autonomy in the management of low back pain. Fam Pract 2002;19:140–5. 10.1093/fampra/19.2.140 [DOI] [PubMed] [Google Scholar]
- 38. Sanders T, Foster NE, Bishop A, et al. Biopsychosocial care and the physiotherapy encounter: physiotherapists' accounts of back pain consultations. BMC Musculoskelet Disord 2013;14:65. 10.1186/1471-2474-14-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sanders T, Foster NE, Ong BN. Perceptions of general practitioners towards the use of a new system for treating back pain: a qualitative interview study. BMC Med 2011;9:49. 10.1186/1741-7015-9-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Shye D, Freeborn DK, Romeo J, et al. Understanding physicians' imaging test use in low back pain care: the role of focus groups. Int J Qual Health Care 1998;10:83–91. 10.1093/intqhc/10.2.83 [DOI] [PubMed] [Google Scholar]
- 41. Slade SC, Molloy E, Keating JL. The dilemma of diagnostic uncertainty when treating people with chronic low back pain: a qualitative study. Clin Rehabil 2012;26:558–69. 10.1177/0269215511420179 [DOI] [PubMed] [Google Scholar]
- 42. Stilwell P, Hayden JA, Des Rosiers P, et al. A qualitative study of doctors of chiropractic in a nova Scotian practice-based research network: barriers and facilitators to the screening and management of psychosocial factors for patients with low back pain. J Manipulative Physiol Ther 2018;41:25–33. 10.1016/j.jmpt.2017.07.014 [DOI] [PubMed] [Google Scholar]
- 43. van Onna M, Gorter S, van Meerendonk A, et al. General practitioners' perceptions of their ability to identify and refer patients with suspected axial spondyloarthritis: a qualitative study. J Rheumatol 2014;41:897–901. 10.3899/jrheum.131293 [DOI] [PubMed] [Google Scholar]
- 44. Andersson S, Andersson S, Sundberg T, Falkenberg E, et al. Patients' experiences and perceptions of integrative care for back and neck pain. Altern Ther Health Med 2012;18:25–32. [PubMed] [Google Scholar]
- 45. Borkan J, Reis S, Hermoni D, et al. Talking about the pain: a patient-centered study of low back pain in primary care. Soc Sci Med 1995;40:977–88. 10.1016/0277-9536(94)00156-N [DOI] [PubMed] [Google Scholar]
- 46. Brown M, Dean S, Hay-Smith EJC, et al. Musculoskeletal pain and treatment choice: an exploration of illness perceptions and choices of conventional or complementary therapies. Disabil Rehabil 2010;32:1645–57. 10.3109/09638281003649896 [DOI] [PubMed] [Google Scholar]
- 47. Bunzli S, Smith A, Schütze R, et al. Beliefs underlying pain-related fear and how they evolve: a qualitative investigation in people with chronic back pain and high pain-related fear. BMJ Open 2015;5:e008847. 10.1136/bmjopen-2015-008847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Carlin LE, Smith HE, Henwood F. To see or not to see: a qualitative interview study of patients' views on their own diagnostic images. BMJ Open 2014;4:e004999. 10.1136/bmjopen-2014-004999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Coole C, Drummond A, Watson PJ, et al. What concerns workers with low back pain? findings of a qualitative study of patients referred for rehabilitation. J Occup Rehabil 2010;20:472–80. 10.1007/s10926-010-9237-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Darlow B, Dean S, Perry M, et al. Easy to harm, hard to heal: patient views about the back. Spine 2015;40:842–50. 10.1097/BRS.0000000000000901 [DOI] [PubMed] [Google Scholar]
- 51. Dima A, Lewith GT, Little P, et al. Identifying patients' beliefs about treatments for chronic low back pain in primary care: a focus group study. Br J Gen Pract 2013;63:e490–8. 10.3399/bjgp13X669211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. El-Haddad C, Damodaran A, Patrick McNeil H, et al. The experience of patients admitted to hospital with acute low back pain: a qualitative study. Int J Rheum Dis 2018;21:796–803. 10.1111/1756-185X.12870 [DOI] [PubMed] [Google Scholar]
- 53. Evers S, Hsu C, Sherman KJ, et al. Patient perspectives on communication with primary care physicians about chronic low back pain. Perm J 2017;21:16–177. 10.7812/TPP/16-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hoffmann TC, Del Mar CB, Strong J, et al. Patients' expectations of acute low back pain management: implications for evidence uptake. BMC Fam Pract 2013;14:7. 10.1186/1471-2296-14-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Holloway I, Sofaer-Bennett B, Walker J. The stigmatisation of people with chronic back pain. Disabil Rehabil 2007;29:1456–64. 10.1080/09638280601107260 [DOI] [PubMed] [Google Scholar]
- 56. Holt N, Pincus T, Vogel S. Reassurance during low back pain consultations with GPs: a qualitative study. Br J Gen Pract 2015;65:e692–701. 10.3399/bjgp15X686953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Iles RA, Taylor NF, Davidson M, et al. Patient recovery expectations in non-chronic non-specific low back pain: a qualitative investigation. J Rehabil Med 2012;44:781–7. 10.2340/16501977-1019 [DOI] [PubMed] [Google Scholar]
- 58. Larsen EL, Nielsen CV, Jensen C. Getting the pain right: how low back pain patients manage and express their pain experiences. Disabil Rehabil 2013;35:819–27. 10.3109/09638288.2012.709302 [DOI] [PubMed] [Google Scholar]
- 59. Lin I, O'Sullivan P, Coffin J, et al. 'I can sit and talk to her': Aboriginal people, chronic low back pain and healthcare practitioner communication. Aust Fam Physician 2014;43:320–4. [PubMed] [Google Scholar]
- 60. Lin IB, O'Sullivan PB, Coffin JA, et al. Disabling chronic low back pain as an iatrogenic disorder: a qualitative study in Aboriginal Australians. BMJ Open 2013;3:e002654. 10.1136/bmjopen-2013-002654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lyons KJ, Salsbury SA, Hondras MA, et al. Perspectives of older adults on co-management of low back pain by doctors of chiropractic and family medicine physicians: a focus group study. BMC Complement Altern Med 2013;13:225. 10.1186/1472-6882-13-225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Madsen H, Lærum E, Espeland A. S417 communicating MRI results of the lumbar spine to low back pain patients: what are their perspectives and interpretations? Eur J Pain Suppl 2011;5:256 10.1016/S1754-3207(11)70885-9 [DOI] [Google Scholar]
- 63. McPhillips-Tangum CA, Cherkin DC, Rhodes LA, et al. Reasons for repeated medical visits among patients with chronic back pain. J Gen Intern Med 1998;13:289–95. 10.1046/j.1525-1497.1998.00093.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Myburgh C, Boyle E, Lauridsen HH, et al. What influences retrospective self-appraised recovery status among Danes with low-back problems? A comparative qualitative investigation. J Rehabil Med 2015;47:741–7. 10.2340/16501977-1987 [DOI] [PubMed] [Google Scholar]
- 65. Nichols VP, Griffiths FE, Patel S, et al. Patterns of interaction between factors that enhance or inhibit recovery from chronic low back pain. Disabil Rehabil 2015;37:194–206. 10.3109/09638288.2014.913705 [DOI] [PubMed] [Google Scholar]
- 66. Ong BN, Konstantinou K, Corbett M, et al. Patients' own accounts of sciatica: a qualitative study. Spine 2011;36:1251–6. 10.1097/BRS.0b013e318204f7a2 [DOI] [PubMed] [Google Scholar]
- 67. Rhodes LA, McPhillips-Tangum CA, Markham C, et al. The power of the visible: the meaning of diagnostic tests in chronic back pain. Soc Sci Med 1999;48:1189–203. 10.1016/S0277-9536(98)00418-3 [DOI] [PubMed] [Google Scholar]
- 68. Sanders T, Ong BN, Roberts D, et al. Health maintenance, meaning, and disrupted illness trajectories in people with low back pain: a qualitative study. Health Sociol Rev 2015;24:1–14. 10.1080/14461242.2014.999399 [DOI] [Google Scholar]
- 69. Serbic D, Pincus T. Chasing the ghosts: the impact of diagnostic labelling on self-management and pain-related guilt in chronic low back pain patients. J Pain Manag 2013;6:25–35. [Google Scholar]
- 70. Singh G, Newton C, O'Sullivan K, et al. Exploring the lived experience and chronic low back pain beliefs of English-speaking Punjabi and white British people: a qualitative study within the NHS. BMJ Open 2018;8:e020108. 10.1136/bmjopen-2017-020108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Slade SC, Molloy E, Keating JL. Stigma experienced by people with nonspecific chronic low back pain: a qualitative study. Pain Med 2009;10:143–54. 10.1111/j.1526-4637.2008.00540.x [DOI] [PubMed] [Google Scholar]
- 72. Snelgrove S, Liossi C. An interpretative phenomenological analysis of living with chronic low back pain. Br J Health Psychol 2009;14:735–49. 10.1348/135910709X402612 [DOI] [PubMed] [Google Scholar]
- 73. Toye F, Barker K. 'Could I be imagining this?' - the dialectic struggles of people with persistent unexplained back pain. Disabil Rehabil 2010;32:1722–32. 10.3109/09638281003657857 [DOI] [PubMed] [Google Scholar]
- 74. Toye F, Barker K. Persistent non-specific low back pain and patients' experience of general practice: a qualitative study. Prim Health Care Res Dev 2012;13:72–84. 10.1017/S1463423611000387 [DOI] [PubMed] [Google Scholar]
- 75. Allegretti A, Borkan J, Reis S, et al. Paired interviews of shared experiences around chronic low back pain: classic mismatch between patients and their doctors. Fam Pract 2010;27:676–83. 10.1093/fampra/cmq063 [DOI] [PubMed] [Google Scholar]
- 76. Buchman DZ, Ho A, Illes J. You present like a drug addict: patient and clinician perspectives on trust and Trustworthiness in chronic pain management. Pain Med 2016;17:1394–406. 10.1093/pm/pnv083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Hofstede SN, Marang-van de Mheen PJ, Wentink MM, et al. Barriers and facilitators to implement shared decision making in multidisciplinary sciatica care: a qualitative study. Implement Sci 2013;8:95. 10.1186/1748-5908-8-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Hooper H, Ong BN. When Harry Met Barry, and other stories: a partner's influence on relationships in back pain care. Anthropol Med 2005;12:47–60. 10.1080/13648470500049842 [DOI] [PubMed] [Google Scholar]
- 79. Laerum E, Indahl A, Skouen JS, Sture Skouen J. What is "the good back-consultation"? A combined qualitative and quantitative study of chronic low back pain patients' interaction with and perceptions of consultations with specialists. J Rehabil Med 2006;38:255–62. 10.1080/16501970600613461 [DOI] [PubMed] [Google Scholar]
- 80. McIntosh A, Shaw CFM. Barriers to patient information provision in primary care: patients' and general practitioners' experiences and expectations of information for low back pain. Health Expect 2003;6:19–29. 10.1046/j.1369-6513.2003.00197.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Ong BN, Hooper H. Comparing clinical and lay accounts of the diagnosis and treatment of back pain. Sociol Health Illn 2006;28:203–22. 10.1111/j.1467-9566.2006.00488.x [DOI] [PubMed] [Google Scholar]
- 82. Reed B, O'Connor D, Bourne A, et al. Understanding general practitioner and patient perspectives and expectations of lumbar spine imaging reports for acute low back pain: a qualitative study 2018.
- 83. Scheermesser M, Bachmann S, Schämann A, et al. A qualitative study on the role of cultural background in patients' perspectives on rehabilitation. BMC Musculoskelet Disord 2012;13:5. 10.1186/1471-2474-13-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Schers H, Wensing M, Huijsmans Z, et al. Implementation barriers for general practice guidelines on low back pain a qualitative study. Spine 2001;26:E348–53. 10.1097/00007632-200108010-00013 [DOI] [PubMed] [Google Scholar]
- 85. Sloots M, Dekker JHM, Pont M, et al. Reasons of drop-out from rehabilitation in patients of Turkish and Moroccan origin with chronic low back pain in the Netherlands: a qualitative study. J Rehabil Med 2010;42:566–73. 10.2340/16501977-0536 [DOI] [PubMed] [Google Scholar]
- 86. Sloots M, Scheppers EF, Bartels EAC, et al. First rehabilitation consultation in patients of non-native origin: factors that lead to tension in the patient-physician interaction. Disabil Rehabil 2009;31:1853–61. 10.1080/09638280902847085 [DOI] [PubMed] [Google Scholar]
- 87. White KB, Lee J, de C Williams AC. Are patients' and doctors' accounts of the first specialist consultation for chronic back pain in agreement? J Pain Res 2016;9:1109–20. 10.2147/JPR.S119851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Fullen BM, Baxter GD, O'Donovan BGG, et al. Doctors' attitudes and beliefs regarding acute low back pain management: a systematic review. Pain 2008;136:388–96. 10.1016/j.pain.2008.01.003 [DOI] [PubMed] [Google Scholar]
- 89. Morse JM. “Data were saturated". Qual Health Res 2015;25:587–8. [DOI] [PubMed] [Google Scholar]
- 90. Toye F, Seers K, Hannink E, et al. A mega-ethnography of eleven qualitative evidence syntheses exploring the experience of living with chronic non-malignant pain. BMC Med Res Methodol 2017;17:116. 10.1186/s12874-017-0392-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Froud R, Patterson S, Eldridge S, et al. A systematic review and meta-synthesis of the impact of low back pain on people's lives. BMC Musculoskelet Disord 2014;15:50. 10.1186/1471-2474-15-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Crowe M, Whitehead L, Seaton P, et al. Qualitative meta-synthesis: the experience of chronic pain across conditions. J Adv Nurs 2017;73:1004–16. 10.1111/jan.13174 [DOI] [PubMed] [Google Scholar]
- 93. Parsons S, Harding G, Breen A, et al. The influence of patients' and primary care practitioners' beliefs and expectations about chronic musculoskeletal pain on the process of care: a systematic review of qualitative studies. Clin J Pain 2007;23:91–8. 10.1097/01.ajp.0000210947.34676.34 [DOI] [PubMed] [Google Scholar]
- 94. Toye F, Seers K, Allcock N, et al. A meta-ethnography of patients' experiences of chronic non-malignant musculoskeletal pain health services and delivery research. 2013;1:1–189. [Google Scholar]
- 95. Hall AM, Scurrey SR, Pike AE, et al. Physician-reported barriers to using evidence-based recommendations for low back pain in clinical practice: a systematic review and synthesis of qualitative studies using the theoretical domains framework. Implement Sci 2019;14:49. 10.1186/s13012-019-0884-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Gardner T, Refshauge K, Smith L, et al. Physiotherapists' beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother 2017;63:132–43. 10.1016/j.jphys.2017.05.017 [DOI] [PubMed] [Google Scholar]
- 97. French SD, Green S, Buchbinder R, et al. Interventions for improving the appropriate use of imaging in people with musculoskeletal conditions. Cochrane Database Syst Rev 2010;149:CD006094. 10.1002/14651858.CD006094.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Kerry S, Oakeshott P, Dundas D, et al. Influence of postal distribution of the Royal College of radiologists' guidelines, together with feedback on radiological referral rates, on X-ray referrals from general practice: a randomized controlled trial. Fam Pract 2000;17:46–52. 10.1093/fampra/17.1.46 [DOI] [PubMed] [Google Scholar]
- 99. Deyo RA, Diehl AK, Rosenthal M. Reducing roentgenography use. can patient expectations be altered? Arch Intern Med 1987;147:141–5. 10.1001/archinte.147.1.141 [DOI] [PubMed] [Google Scholar]
- 100. Deshpande S, Marietta J, Dennett L. Mass media campaigns for back pain: a systematic review. International forum for back and neck pain research in primary care; 3-6 July, Quebec City, Canada, 2019. [Google Scholar]
- 101. Buchbinder R, Jolley D, Wyatt M. 2001 Volvo Award winner in clinical studies: effects of a media campaign on back pain beliefs and its potential influence on management of low back pain in general practice. Spine 2001;26:2535–42. 10.1097/00007632-200112010-00005 [DOI] [PubMed] [Google Scholar]
- 102. Buchbinder R, Jolley D, Wyatt M. Population based intervention to change back pain beliefs and disability: three part evaluation. BMJ 2001;322:1516–20. 10.1136/bmj.322.7301.1516 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-037820supp001.pdf (5.9MB, pdf)