Abstract
Purpose
The mortality rate for severely injured patients with the injury severity score (ISS) ≥16 has decreased in Germany. There is robust evidence that mortality is influenced not only by the acute trauma itself but also by physical health, age and sex. The aim of this study was to identify other possible influences on the mortality of severely injured patients.
Methods
In a matched-pair analysis of data from Trauma Register DGU®, non-surviving patients from Germany between 2009 and 2014 with an ISS≥16 were compared with surviving matching partners. Matching was performed on the basis of age, sex, physical health, injury pattern, trauma mechanism, conscious state at the scene of the accident based on the Glasgow coma scale, and the presence of shock on arrival at the emergency room.
Results
We matched two homogeneous groups, each of which consisted of 657 patients (535 male, average age 37 years). There was no significant difference in the vital parameters at the scene of the accident, the length of the pre-hospital phase, the type of transport (ground or air), pre-hospital fluid management and amounts, ISS, initial care level, the length of the emergency room stay, the care received at night or from on-call personnel during the weekend, the use of abdominal sonographic imaging, the type of X-ray imaging used, and the percentage of patients who developed sepsis. We found a significant difference in the new injury severity score, the frequency of multi-organ failure, hemoglobine at admission, base excess and international normalized ratio in the emergency room, the type of accident (fall or road traffic accident), the pre-hospital intubation rate, reanimation, in-hospital fluid management, the frequency of transfusion, tomography (whole-body computed tomography), and the necessity of emergency intervention.
Conclusion
Previously postulated factors such as the level of care and the length of the emergency room stay did not appear to have a significant influence in this study. Further studies should be conducted to analyse the identified factors with a view to optimising the treatment of severely injured patients. Our study shows that there are significant factors that can predict or influence the mortality of severely injured patients.
Keywords: Emergency medicine, Registries, Mortality, Severely injured patients
Introduction
According to Trauma Register DGU®, the mortality rate for severely injured patients with an injury severity score (ISS) ≥16 has continuously decreased in Germany in recent years. While the observed hospital mortality rate for this patient population was 22.8% in 1999, it had decreased to 18.7% by 2005 and to only approximately 17% by 2015.1,2
Mortality depends on the overall severity and location of injury. For example, classified on the basis of the abbreviated injury scale (AIS), more severe traumatic brain injuries are associated with higher hospital mortality than thoracic injuries. Apart from the severity of trauma, survival is influenced by pre-traumatic physical health, age and sex.3 Kuhne et al.4 showed that mortality is significantly higher among patients aged over 56.
Regardless of the severity of the injury and the age of the patient, Wutzler et al.5 showed that among 3836 patients mortality was higher in patients with pre-existing heart disease, obesity, liver cirrhosis, malignancies, and coagulation disorder.
Trentzsch et al.6 found that female sex has a positive influence on outcome. For example, women (ISS≥16) were less likely to experience multi-organ failure and develop sepsis after severe trauma and were more resilient to shock associated with the injury.
Literature on the subject provides no clarity as to the role played by the after-hours admission of severely injured patients. Some studies show that this factor does not have an aggravating effect,7, 8, 9, 10 while others show that it has a negative influence.11, 12, 13
In contrast, various studies have identified a number of diagnostic and therapeutic factors that can have a favourable influence on the mortality of patients with polytrauma.
Diverging results have been published on the influence of the type of medical facility on the mortality of severely injured patients. Some authors have found a survival benefit for patients treated at a level I trauma centre as compared to those treated at hospitals with fewer resources.14,15
In 2010, Hilbert et al.16 evaluated various mortality rates and showed that the differences between them in Germany are not only attributable to the level of care of the initial hospital.
According to their results, other factors must be considered because there are also significant differences in mortality within the level I care group. A possible explanation was provided by Zacher et al.,17 who found that a volume of at least 40 severely injured patients per year was beneficial for survival. A study by Brown et al.18 in the US produced similar results and showed that increasing volume was associated with improved outcomes.
The choice of rescue vehicle also appears to have an influence. Various studies have shown that overall mortality was significantly lower when patients were transported to a level I trauma centre by rescue helicopter than by ground transport. Helicopter transport was associated with significantly higher pre-hospital rescue times.19, 20, 21
The rapid surgical control of bleeding is also considered vital in some studies and plays an important role in the early phase of treatment for bleeding trauma patients.22, 23, 24 There is agreement that the rapid surgical control of bleeding minimises blood loss and improve the prognosis of patients with penetrating trauma. Short rescue times are considered more important than pre-hospital invasive interventions.25, 26, 27
More recent studies have shown that hypotensive resuscitation in patients without traumatic brain injury along with the rapid surgical control of bleeding can have a significant survival benefit.25,27, 28, 29
Huber-Wagner et al.30,31 found a higher survival rate for haemodynamically stable and unstable severely injured patients (ISS≥16) who had undergone whole-body computed tomography (WBCT) as part of emergency room treatment when organisational conditions allowed WBCT to be carried out quickly. This conclusion was also reached in systematic reviews.32,33
In sum, multivariate analyses have identified a number of predictive factors. It remains unclear, however, why patients with the same injury pattern either survive or die. Comparative studies are difficult on account of multiple factors. Randomised blind studies are challenging for ethical reasons, especially since severely injured patients always constitute a complex patient population.
The aim of this study was to use a matched-pair analysis in order to identify factors that influence the mortality of severely injured patients (ISS ≥16). The limitations of retrospective register studies must be kept in mind.
Methods
In this study, we performed a matched-pair analysis based on data from Trauma Register DGU® in order to retrospectively analyse factors that can influence the mortality of severely injured patients.
Trauma Register DGU® of the German Trauma Society (Deutsche Gesellschaft für Unfallchirurgie, DGU) was founded in 1993. The aim of this multi-centre database is the pseudonymised and standardized documentation of severely injured patients.
Data are collected prospectively in four consecutive time phases: (1) pre-hospital phase, (2) emergency room and initial surgery, (3) intensive care unit, and (4) discharge. The documentation includes detailed information on demographics, injury pattern, comorbidities, pre- and in-hospital management, course on intensive care unit, relevant laboratory findings including data on transfusion, and the outcome of each individual. Included are patients who are admitted to hospital via the emergency room and subsequently receive intensive or intermediate care and patients who arrive at hospital with vital signs and die before admission to the intensive care unit.
The infrastructure for documentation, data management, and data analysis is provided by AUC–Academy for Trauma Surgery (AUC – Akademie der Unfallchirurgie GmbH), which is affiliated to the German Trauma Society. Scientific leadership is provided by the Committee on Emergency Medicine, Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society. Participating hospitals submit pseudonymised data to a central database via a web-based application. Scientific data analysis is approved according to a peer review procedure established by Sektion NIS.
The participating hospitals are primarily located in Germany (93%), but a rising number of hospitals in other countries (at present, Austria, Belgium, China, Finland, Luxembourg, the Netherlands, Slovenia, Switzerland and the United Arab Emirates) contribute data as well. Approximately 40,000 cases from more than 600 hospitals are currently entered into the database per year.
Participation in Trauma Register DGU® is voluntary. For hospitals associated with Trauma Netzwerk DGU® however, the entry of at least a basic data set is obligatory for reasons of quality assurance.
The present study was conducted in accordance with the publication guidelines of Trauma Register DGU® and registered as TR-DGU project ID 2014-039.
The present study included patients from Germany with an ISS≥16 between 2009 and 2014 and data from a basic data set based on the standard form and quality management (QM) form who died of their injuries and for whom a surviving matching partner was found.
Only patients who received primary care were included. Patients who were transferred from another hospital or were transferred to another hospital at an early stage were excluded.
Patients who were younger than 16 years of age and older than 55 were not included either in order to minimize age-related factors that could influence mortality such as limiting pre-existing conditions and extensive use of medication. Patients under the age of 16 were excluded to take into account the specific physiology of children and sometimes different treatment options. Similar groups were created by matching non-survivors with survivors on the basis of the criteria shown as follows.
Four age groups were created (16–25, 26–35, 36–45 and 46–55 years). Two categories, i.e. American Society of Anesthesiologists Classification System (ASA) 1, 2 and ASA 3, 4 were created to match pre-traumatic states of health, and the partners were allocated to these categories. Patients with ASA 5, 6 were excluded.
Patients were matched on the basis of the AIS for four relevant body regions in order to take into account the influence of injury patterns. For example, each head injury was assigned to a partner on the basis of the severity of the injury. The matching categories for injury severity were AIS 0–2, and 3–5. The same approach was taken for injuries to the thorax, abdomen and extremities. Trauma mechanism (blunt vs. penetrating) and the state of consciousness at the scene of the accident were also matched on the basis of the Glasgow coma scale (GCS). Three GCS categories were formed (3–8, 9–14, 15). Matching for the criterion of systolic blood pressure upon admission to the emergency room was also performed on the basis of three categories: <90 mmHg, 90–110 mmHg and ≥110 mmHg. After the data transformation of the respective matched pair criteria into a numerical code, the matching of non-survivor to a survivor was done by the authors RL and DB in four-eye principle.
Statistical analysis
Statistical analysis was carried out with SPSS (Version 23, IBM, Armonk, NY, USA). The Chi-squared test was used for comparing frequencies and the Mann-Whitney U test was used for metric and ordinal data. The level of significance was set at 5% (p < 0.05) for all tests. If a data value from one patient was unavailable, the corresponding data value from the matching partner was also excluded.
Results
Patient group and general data
Two homogeneous groups were formed, each with 657 patients. The mean age of the patients in the survivor group was nearly 37 years. A total of 97.4% of these patients had sustained a blunt trauma (Table 1).
Table 1.
Patient groups and general data.
| Variables | Survivors | Non-survivors | p value |
|---|---|---|---|
| Age (year) | 36.8 ± 12.4 | 36.9 ± 12.4 | 0.65 |
| 16-25 | 174 (26.5) | 174 (26.5) | |
| 26-35 | 109 (16.6) | 109 (16.6) | |
| 36-45 | 145 (22.1) | 145 (22.1) | |
| 46-55 | 229 (34.9) | 229 (34.9) | |
| Male | 535 (81.4) | 535 (81.4) | |
| Blunt trauma | 635 (97.4) | 635 (97.4) | |
| ISS | 30.7 ± 8,7 | 30.9 ± 9,4 | 0.86 |
| NISS | 40.2 ± 12.1 | 43.9 ± 13.9 | <0.001 |
| GCS at scene of accident | 7.4 ± 4.3 | 6.6 ± 4.5 | <0.001 |
| Systolic blood pressure at scene of accident | 121.6 ± 30.6 | 118 ± 39.6 | 0.13 |
| Heart rate at scene of accident | 94.4 ± 22.7 | 94.3 ± 28.2 | 0.98 |
| ICU intubation days | 11.3 ± 12.9 | 6.0 ± 9.3 | |
| ICU days | 17.5 ± 14.5 | 6.7 ± 11.6 | |
| Hospital days | 28.1 ± 20.6 | 8.4 ± 14.5 | |
| Died within 24 h | - | 231 (35.2) | |
| Multi-organ failure | 180 (45.7) | 228 (75.2) | <0.001 |
| Sepsis | 44 (11.3) | 47 (16.3) | 0.063 |
| RISC-II prognosis relating to death | - (12.3) | - (21) | <0.001 |
Data were presented as mean ± SD or n (%), -: not applicable.
ISS: injury severity score, NISS: new injury severity score, GCS: Glasgow coma scale, ICU: intensive care unit, RISC-II: revised injury severity classification score, version II.
On account of the design of the study and the way the groups were formed, the numbers of intensive care unit, intubation, and hospital days were significantly higher for the survivor group (Table 1). A total of 35.2% of the patients in the non-survivor group (n = 231) died within the first 24 h.
The percentage of patients who developed sepsis differed in the two groups, but not significantly (p = 0.063). However, multi-organ failure was significantly more frequent (75.2%) in the non-survivor group (p < 0.001). The revised injury severity classification score, version II prognosis differed significantly between the groups. Predicted mortality was 12.3% in the survivor group and 21.0% in the non-survivor group (p < 0.001).
The distribution of injuries according to AIS codes shows that the majority were traumatic brain injuries, with an AIS of 5 in 50% and an AIS of 4 in 22.1% of the cases. A total of 49.9% of the patients had sustained a relevant thorax injury (AIS≥3). A total of 10.3% of the cases involved relevant abdominal injuries and 21.3% relevant extremity injuries (Table 2). Since the patients were matched in accordance with an AIS severity score for each body region, the ISS in the survivor group does not differ significantly from that of the non-survivor group. The new injury severity score (NISS), on the other hand, differs significantly between the two groups (p < 0.001), with higher values in the non-survivor group (40.2 ± 12.1) vs. (43.9 ± 13.9) (Table 1).
Table 2.
Injuries on the basis of the AIS-code, n (%).
| AIS | Head | Thorax | Abdomen | Extremities |
|---|---|---|---|---|
| 0–2 | 145 (22.1) | 329 (50.1) | 589 (89.7) | 517 (78.7) |
| 3 | 38 (5.8) | 169 (25.7) | 33 (5.0) | 103 (15.7) |
| 4 | 145 (22.1) | 108 (16.4) | 23 (3.5) | 20 (3.0) |
| 5 | 329 (50.1) | 51 (7.8) | 12 (1.8) | 17 (2.6) |
According to the defined matching categories for state of consciousness on the basis of the GCS, 467 patients (71.1%) were unconscious (GCS≤8). In addition, 10.2% (n = 67) of the patients were in a state of shock (systolic blood pressure≤90 mmHg) at the scene of the accident.
Influencing factors
Cause of accident
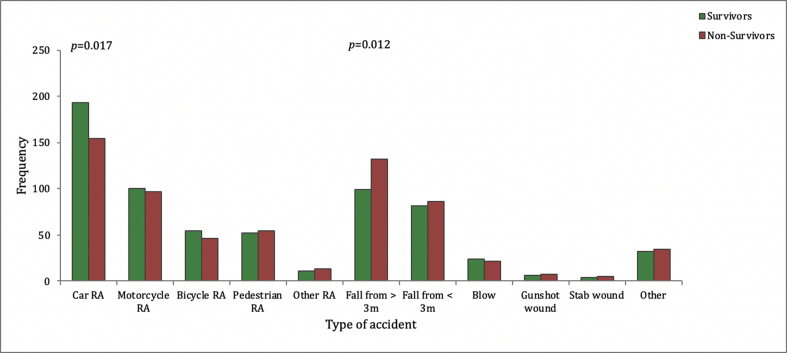
The rate of patients involved in a car accident was significantly higher (410 vs. 365, p = 0.017) in survivors. A fall from a height of more than 3 m was significantly more frequent in the non-survivor group than in the survivor group (99 vs. 132, p = 0.012). No differences were seen (41 vs. 41, p = 0.98) when attempted suicide was the cause of injury (Fig. 1).
Fig. 1.
Cause of accident. Illustration of different types of accident taking into account the various road traffic accidents. RA: road traffic accident.
Hospital and transportation
The level of care of the hospital providing initial treatment does not appear to have any influence on outcome (p = 0.62). A similar percentage of survivors and non-survivors received care at level I, level II and level III trauma centres.
Likewise, the type of transportation (ground (403 vs. 412) and air (245 vs. 234)) used to move patients to a trauma centre was similar (p = 0.56). Survival was also not significantly affected by after-hours admission (71.6% vs. 69.6%, p = 0.42).
Interestingly, a difference can be seen with regard to the type of documentation at the hospital (p < 0.001). Instead of using the compulsory short form (QM, 40 data per case), centres can voluntarily fill in the standard form (about 100 data per case). This form was used for documenting more than 61% of the patients in the survivor group. A total of 49% of the patients in the non-survivor group were documented by means of the QM form, which only contains a minimum number of parameters. These data are shown in Table 3.
Table 3.
Organisational parameters, n (%).
| Variables | Survivors | Non-survivors | p value |
|---|---|---|---|
| Trauma centre | 0.62 | ||
| Level I | 490 (74.6) | 484 (73.7) | |
| Level II | 156 (23.7) | 157 (23.9) | |
| Level III | 11 (1.7) | 16 (2.4) | |
| Documentation with QM form | 253 (38.5) | 320 (48.7) | <0.001 |
| Ground transport | 403 (62.2) | 412 (63.8) | 0.56 |
| Air transport | 245 (37.8) | 234 (36.2) | 0.56 |
| On-call duty | 465 (71.6) | 454 (69.6) | 0.42 |
| Night hours (8:00 p.m.–5:59 a.m.) | 203 (31.3) | 206 (31.7) | 0.87 |
QM: quality management.
Pre-hospital care
A comparative analysis of the overall pre-hospital time, which is defined as the length of time between an accident and the arrival at the trauma centre for primary care, showed no significant difference (p = 0.65). Pre-hospital fluid administration was performed in more than 90% of the cases in both groups. There was no significant difference in the overall amount of fluid administered (1062 mL vs. 1133 mL, p = 0.37).
A significantly higher number of patients who eventually died had been intubated prior to admission to hospital, although the percentage of unconscious patients (p = 0.009) was the same in both groups.
A total of 482 patients (73.4%) in the survivor group had been intubated, whereas 522 (79.5%) in the non-survivor group had been intubated, a difference of 6% points. In the survivor group, 1.1% (n = 7/657) of the patients underwent cardiopulmonary resuscitation (CPR) before admission to hospital. The percentage of patients in the non-survivor group who had been mechanically reanimated before admission to hospital was significantly higher with 4% (n = 26/657). Among 33 patients, 21% (n = 7/33) of them who had been reanimated before admission to hospital survive, and 79% (n = 26/33) of them who had been reanimated before admission to hospital died (Table 4).
Table 4.
Pre-hospital care provided for the survivors and non-survivors.
| Variables | Survivors | Non-survivors | p value |
|---|---|---|---|
| Pre-hospital intubation | 482 (73.4) | 522 (79.5) | 0.009 |
| Pre-hospital CPR | 7 (1.1) | 26 (4.0) | <0.001 |
| Pre-hospital fluid administration | 604 (91.9) | 601 (91.5) | 0.76 |
| Pre-hospital amount of fluid (mL) | 1062 ± 743 | 1133 ± 921 | 0.37 |
| Length of pre-hospital treatment period | 69.8 ± 30.1 | 68.6 ± 29.8 | 0.647 |
Data were presented as n (%) or mean ± SD.
CPR: cardiopulmonary resuscitation.
Emergency room
There was no difference in the vital parameters initially examined at the scene of the accident, but heart rate on arrival at the emergency room was significantly higher in the non-survivor group (88.6 ± 21.5 vs. 92 ± 27, p = 0.042).
An analysis of the documented clinical parameters showed that haemoglobin level and the base excess were significantly lower in the non-survivor group (p < 0.001). International normalized ratio was thus significantly higher (1.2 vs. 1.3, p < 0.001).
Emergency room–diagnostic procedures and treatment
A comparison of volume therapy in the emergency room revealed a significant difference in the amounts of fluid administered (1673 ± 2115 mL vs. 2118 ± 2462 mL, p = 0.007) and in the frequency of the need for transfusion (p < 0.001). For example, 16% (n = 104) of the survivors required transfusion, whereas almost one in three of the non-survivors (29%, n = 189) received packed red blood cells. The frequency of mass transfusion was also significantly higher in the non-survivor group (2.4% vs. 7.6%, p < 0.001). The administration of fresh frozen plasma (FFP) was also significantly higher in the non-survivor group (p = 0.004) (Table 5).
Table 5.
Emergency room – diagnostic procedures and treatment.
| Variables | Survivors | Non-survivors | p value |
|---|---|---|---|
| Systolic blood pressure (mmHg) in emergency room | 120.6 ± 26.4 | 120.3 ± 33 | 0.76 |
| Heart rate (beats/min) in emergency room | 88.6 ± 21.5 | 92 ± 27 | 0.042 |
| Haemoglobin (g/dl) in emergency room | 12.8 ± 2.3 | 12.2 ± 2.7 | <0.001 |
| Base excess in emergency room | 2.7 ± 4.4 | −4.5 ± 5.4 | <0.001 |
| INR in emergency room | 1.2 ± 0.5 | 1.3 ± 0.5 | <0.001 |
| Volume (mL) in emergency room phase | 1673 ± 2115 | 2118 ± 2462 | 0.007 |
| Patients with transfusion in emergency room | 104 (15.8) | 189 (28.9) | <0.001 |
| Erythrocyte concentrates | 0.84 ± 2.7 | 2.2 ± 5.6 | <0.001 |
| Patients with massive transfusion in emergency room (>10 PRBC) | 16 (2.4) | 50 (7.6) | <0.001 |
| FFP administration in emergency room | 73 (11.1) | 109 (16.6) | 0.004 |
| FFP administration (amount) | 0.63 ± 2.2 | 1.1 ± 5.7 | 0.002 |
| WBCT | 597 (91.1) | 565 (86.4) | 0.006 |
| cCT | 650 (98.9) | 622 (94.7) | <0.001 |
| FAST | 525 (80.2) | 520 (79.5) | 0.77 |
| Conventional X-ray diagnostic procedure | 258 (39.4) | 232 (35.5) | 0.14 |
| Length of emergency room stay | 57.1 ± 36.0 | 60.7 ± 44.4 | 0.621 |
| Emergency intervention | 231 (39.2) | 301 (50.4) | <0.001 |
Data were presented as mean ± SD or n (%).
INR: international normalized ratio, PRBC: packed red blood cells, FFP: fresh frozen plasma, WBCT: whole-body computed tomography, cCT: cranial computed tomography, FAST: focused assessment with sonography for trauma.
No significant difference was found in the number of X-ray diagnostic procedures carried out (p = 0.14). However, a difference was found with respect to cranial computed tomography and WBCT procedures. Both were performed significantly more frequently in the survivor group (p < 0.001 and p = 0.006). Despite these additional diagnostic procedures, the emergency room stay was not longer for this group. In fact, it tended to be shorter (57.1 min vs. 60.7 min, p = 0.621).
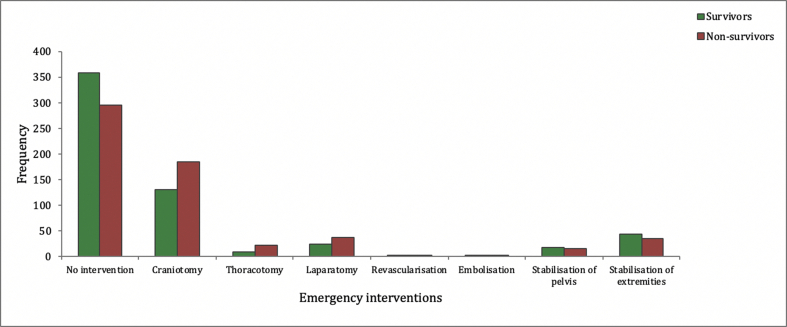
On the whole, an emergency intervention was performed more frequently (39.2% vs. 50.4%, p < 0.001) in the non-survivor group. Craniotomies were the most frequently used procedure (n = 184). Fig. 2 provides a detailed overview of the frequency of the various emergency interventions.
Fig. 2.
Emergency interventions. Detailed overview of the frequency of the various emergency interventions for survivors and non-survivors.
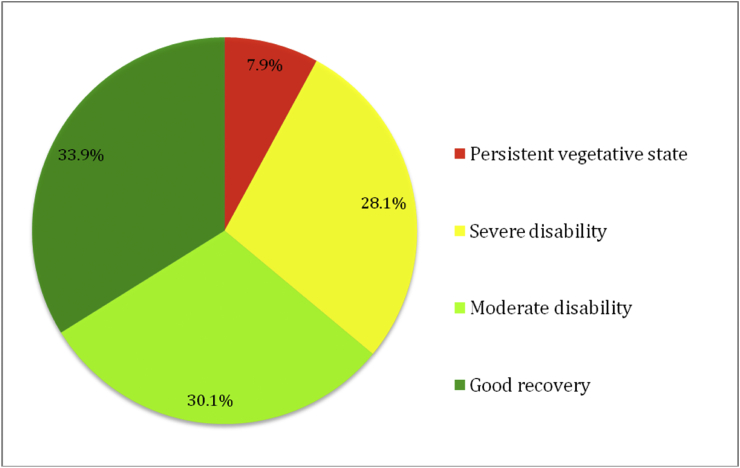
Nearly two third of the survivor group had a good outcome or only moderate disability shown after the treatment at the time of discharge (Fig. 3).
Fig. 3.
Outcome of survivors. Outcome assessment of the survivors using the Glasgow outcome scale.
Discussion
Several studies have been able to identify various relevant factors that influence the survival of severely injured patients: pre-traumatic physical health, age, and sex have an influence on survival.3,4,6,34,35
In the present study, a matched-pairs design was used to exclude several known prognostic factors such as age, sex, injury pattern, pre-traumatic physical condition, trauma mechanism, state of consciousness at scene of accident, systolic blood pressure on arrival at emergency room and ISS. An analysis of the differences between the survivor and non-survivor groups thus made it possible to identify other factors that have an influence on the outcome of seriously injured patients.
The present study identified a significant difference between the groups when it came to the mechanism of injury.
In the case of patients who were injured in a traffic accident, the number of survivors was considerably higher than the number of non-survivors. In contrast, the mortality rate was significantly higher for patients who had fallen from a height of more than 3 m. An obvious explanation for this difference is the way in which energy is transferred to patients in these two types of injury. In the case of falls, kinetic energy is transferred to them more directly.
Staudenmayer et al.36 provide another possible explanation in their latest study. In an analysis of 60,182 severely injured patients (ISS>15) in California, they showed that fall-related injuries were frequently undertriaged, whereas injuries from road accidents and penetrating trauma were often overtriaged. Undertriage was defined as a patient with an ISS>15 who was not treated in a level I or II trauma centre.
Since the analysis found no difference between the groups of survivors and non-survivors with respect to the treating trauma centre. In our cohort, this factor appears to play only a minor role.
In addition to the level of trauma centre, there was also no difference between the two groups with regard to pre-hospital transportation.
Andruszkow et al.19 reported that mortality was significantly lower when patients were transported to a level I trauma centre by a rescue helicopter as compared to ground transport, although helicopter transport resulted in significantly higher pre-hospital rescue times. In contrast to the above-mentioned studies, our analysis did not demonstrate the advantage of helicopter transport.
Our study showed a higher ISS (30.7 vs. 26.0) than the study by Andruszkow et al.19 In addition, Andruszkow et al.19 included patients with an ISS≥9, which makes it difficult to compare the two cohorts. What is interesting, however, is that the proportion of patients involved in road traffic accidents in the helicopter group was significantly higher and that the proportion of patients with fall-related injuries in the ground transport group was significantly higher. The same can be seen in the study by Hannay et al.21 They analysed 14,440 patient transports (17% of which were airborne). The ISS was significantly lower in comparison to our cohort (15.1 vs. 30.7). In addition, the cohort did not only include seriously injured patients (ISS>15 in approximately 24% of the cases). However, the study also showed that 77% of the patients transported by helicopter were patients involved in road accidents, while only 49% of patients transported by ground transport were involved in road accidents. The situation regarding fall-related injuries is the opposite. Whereas 10% of patients transported by ground transport had fall-related injuries, only 8% of patients transported by helicopter had fall-related injuries.
A comparison to the above-mentioned studies is possible only to a limited extent, as the present study cannot make statements about mortality on account of its study design. It should be noted, however, that mode of transport does not have a significant influence on mortality in the groups compared.
This also supports the above-mentioned assertion of Staudenmayer et al.36 that road accidents tend to be overtriaged while falls from heights of more than 3 m tend to be undertriaged. In keeping with this, our cohort showed that the type of accident, whether road accident or fall, could influence mortality.
In a study by Brown et al.20 only 42% of patients in the helicopter group and 21% of patients in the ground transport group had an ISS>15. The average ISS figures in this study were 15.9 and 10.2 respectively. Due to the differences in overall injury severity, it is difficult to make a clear comparison.
Our results also confirm that the GCS appears to be an independent predictor of mortality among trauma patients.37,38 For example, in the cohort we analysed, the GCS at the scene of the accident was higher in the survivor group (7.4 ± 4.3) than in the non-survivor group (6.6 ± 4.5).
There was no difference between the two groups regarding the time of admission, i.e. on weekends or during the night. Other studies have also come to this conclusion.10 Dybdal et al.7 evaluated 1985 patients and, when they compared the influence of day-time and night-time treatment, found that there was no significant increase in 30-day mortality for the subgroup of patients with an ISS>15 or for the overall cohort. In their analysis of 4000 patients, Laupland et al.8 found no differences either, attributing this to the well-developed and functioning trauma system in the Calgary (Canada) region. The authors of a study from Germany involving 1226 patients at a maximum-care facility came to the same conclusion after comparing severely injured patients admitted during the day and those admitted at night (this study also included patients transferred from other hospitals).9
The latter study also stated that good organisation is a possible explanation. Three studies do, however, find a difference in mortality between night-time and day-time admissions.9 Di Bartolomeo et al.12 attributed this finding to the fact that their study included patients who had been transferred from other hospitals, since this group of patients had often been excluded from other studies. Barbosa et al.11 showed in their single-centre study involving 563 patients that mortality was higher among patients treated at night despite risk adjustment. No statement was made about injury severity (e.g. ISS). The explanation given for this finding is that, in the hospital in question, conditions for diagnostic procedures and surgical treatment are different at night. Egol13 also showed that the risk of in-hospital mortality is higher in patients admitted at night than in those admitted during the day, with the effect being most prominent at level III/IV hospitals.
It is difficult to make a direct comparison between these studies and our findings, but we can say that more than 97% of the patients in our study were treated at certified level I and level II trauma centres and that basic organisational structures for treating trauma patients therefore exist around the clock. As the studies came to similar conclusions, this is the main reason why the time of admission was not found to be an influencing factor.
Several studies have shown that pre-hospital cardiopulmonary resuscitation after trauma reduces the likelihood of survival to hospital discharge. They found survival rates of only 5%–31%.39, 40, 41
Our matched-pair analysis also showed that pre-hospital reanimation has a significant influence on the mortality of severely injured patients.
The fact that a WBCT was performed significantly more frequently on patients in the survivor group is in agreement with the results of other studies30, 31, 32, 33 and supports the claim that WBCTs can have a favourable influence on the mortality of severely injured trauma patients. Interestingly, the emergency room stay is no longer for the survivor group despite a significant higher number of WBCTs performed. A WBCT in the trauma management is therefore not associated with a longer time in the emergency room in our study. Emergency interventions are more frequent in the non-survivor group. These results indicate that rapid management in the emergency room with comprehensive diagnostic procedures increases the likelihood of survival.
The decision to perform an emergency intervention must not be made too late as a consequence. In a study that analysed 12,971 severely injured patients in terms of whether they underwent an emergency or early operation, Logters et al.42 called for a structured algorithm for making decisions on emergency interventions which would include discontinuing emergency room diagnostic procedures.
The mortality rate was 46% among injured patients who needed an emergency operation before emergency room diagnostic procedures were completed and only 13% among injured patients who had an operation after emergency room diagnostic procedures were concluded.
The survival of severely injured patients depends primarily on injury patterns and the resulting blood loss, i.e. on the possibility of arresting bleeding in good time. Despite the same amount of fluid being administered before admission to hospital, the clinical and paraclinical parameters in the non-survivor group suggest that bleeding and, as a result, shock were significantly more frequent in the non-survivor group. In addition, the paraclinical parameters more frequently indicate the onset of acidosis and coagulopathy. As well as a higher percentage of emergency interventions, another indication of bleeding is the significantly higher transfusion rate, including mass transfusion, in the non-survivor group.
In recent years, the concept of hypotensive resuscitation in the treatment of polytrauma has gained ground because new studies have confirmed that the use of hypotensive resuscitation and rapid surgical bleeding control leads to improved survival in patients without severe traumatic brain injury.25,27, 28, 29,43,44
As the average systolic blood pressure in both groups was 120 mmHg, this would appear to indicate that the concept of hypotensive resuscitation could have been implemented more strictly until bleeding was definitively controlled even though a large percentage of patients had a traumatic brain injury.
Despite the large percentage of traumatic brain injuries and the high ISS, one third of the patients in the survivor group were rated as having only a moderate disability in accordance with the Glasgow outcome scale (GOS) and 30% only a minor disability.
The use of the AIS coding system for matching in the various body regions meant that the ISS was, as expected, almost identical in both groups, whereas the NISS was significantly higher in the non-survivor group. While the NISS is calculated on the basis of the three most severe injuries (using the AIS code), the ISS is calculated on the basis of the AIS codes of the three most severely injured body regions.
A current review shows that both scores can predict mortality, but that the quality of the prediction depends on the pattern and type of injury concerned.45
Smith et al.46 have shown that the NISS is superior to the ISS for perforating injuries. Eid et al.47 have come to the same conclusion for blunt traumas. The NISS also appears to be better at predicting post-traumatic multi-organ failure.48 The results of this matched-pair analysis are therefore consistent with the relevant literature. Multiple injuries in the same body region may thus be one reason why one of the paired patients died while the other survived. Like the NISS, the rate of multi-organ failure was significantly higher in the non-survivor group.
This study is a retrospective matched-pair analysis with groups that are comparable in many parameters. Despite good matches, matched-pair analyses have their limitations, as the groups they compare are different, if only marginally so. This is seen in our study when the NISS and ISS are compared.
The outcome of severely injured patients in particular depends on multiple factors outside of traditional trauma scores, for example the experience of the emergency medical service personnel, the time and place at which a trauma is sustained, the facility providing the treatment, the rescue equipment and vehicles, and patient factors. These factors are seldom assessed systematically. We took this opportunity to examine certain factors in a large registry. Nevertheless, several points remain unclear.
In addition, Trauma Register DGU® does not include patients who died before admission to hospital.
Another limitation is that possible constraints on treatment, such as an advance healthcare directive, were not considered. Such constraints are a possible bias, in particular with regard to patients with severe head injuries.
The results of this study show that there are significant factors that predict or influence the mortality of severely injured patients. On the basis of paraclinical values as haemoglobin level and base excess, bleeding patients in particular are likely to have an unfavourable outcome. The mechanism of injury also appears to have an influence on the likelihood of survival. In this study a car accident is associated with a significant better outcome concerning mortality and a fall of >3 m is survived significantly less. Factors that other studies have found to exert an influence, such as care level and the length of the emergency room stay, did not make a significant difference in our study.
Funding
Nil.
Ethical Statement
Not applicable. The manuscript does not report on or involve the use of any animal or human tissue.
Acknowledgements
We would like to thank the members of the Polytrauma Study Group of the German Trauma Society for their many years of hard work and commitment to Trauma Register DGU®. In 2007, the Polytrauma Study Group was integrated into the Committee on Emergency Medicine, Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society (DGU).
The authors would like to thank the German Office of Languages in Hürth for linguistic support.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Declaration of Competing Interest
DB, TP, MK and AF are members of the Committee on Emergency Medicine, Intensive Care and Trauma Management of the German Trauma Society (Sektion NIS). They received no financial funding.
RL is a member of the Committee on Emergency Medicine, Intensive Care and Trauma Management of the German Trauma Society (Sektion NIS) and a consultant for AUC GmbH and has received research support (third-party funds) from AUC GmbH.
AS, MV, EK declare that no conflict of interests exists.
References
- 1.Ruchholtz S., Lefering R., Paffrath T. Reduction in mortality of severely injured patients in Germany. Deutsches Arzteblatt international. 2008;105:225–231. doi: 10.3238/arztebl.2008.0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Committee on Emergency Medicine . TraumaRegister DGU Jahresbericht; 2016. Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society (DGU)http://www.traumaregister-dgu.de/fileadmin/user_upload/traumaregister-dgu.de/docs/Downloads/TR-DGU-Jahresbericht_2016.pdf [Google Scholar]
- 3.Zafar S.N., Shah A.A., Zogg C.K. Morbidity or mortality? Variations in trauma centres in the rescue of older injured patients. Injury. 2016;47:1091–1097. doi: 10.1016/j.injury.2015.11.044. [DOI] [PubMed] [Google Scholar]
- 4.Kuhne C.A., Ruchholtz S., Kaiser G.M. Mortality in severely injured elderly trauma patients--when does age become a risk factor? World J Surg. 2005;29:1476–1482. doi: 10.1007/s00268-005-7796-y. [DOI] [PubMed] [Google Scholar]
- 5.Wutzler S., Maegele M., Marzi I. Association of preexisting medical conditions with in-hospital mortality in multiple-trauma patients. J Am Coll Surg. 2009;209:75–81. doi: 10.1016/j.jamcollsurg.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Trentzsch H., Nienaber U., Behnke M. Female sex protects from organ failure and sepsis after major trauma haemorrhage. Injury. 2014;45:S20–S28. doi: 10.1016/j.injury.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Dybdal B., Svane C., Hesselfeldh R. Is there a diurnal difference in mortality of severely injured trauma patients? Emerg Med J. 2015;32:287–290. doi: 10.1136/emermed-2013-202754. [DOI] [PubMed] [Google Scholar]
- 8.Laupland K.B., Ball C.G., Kirkpatrick A.W. Hospital mortality among major trauma victims admitted on weekends and evenings: a cohort study. J Trauma Manag Outcome. 2009;3:8. doi: 10.1186/1752-2897-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parsch W., Hilber F., Schmucker U. While others are sleeping - performance of major trauma care at night. Zentral Chir. 2015;141:660–665. doi: 10.1055/s-0035-1546262. [DOI] [PubMed] [Google Scholar]
- 10.Zafar S.N., Libuit L., Hashmi Z.G. The sleepy surgeon: does night-time surgery for trauma affect mortality outcomes? Am J Surg. 2015;209:633–639. doi: 10.1016/j.amjsurg.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Barbosa Lde S., dos Reis Junior G.S., Chaves R.Z. Night admission is an independent risk factor for mortality in trauma patients - a systemic error approach. Rev Col Bras Cir. 2015;42:209–214. doi: 10.1590/0100-69912015004003. [DOI] [PubMed] [Google Scholar]
- 12.Di Bartolomeo S., Marino M., Ventura C. A population based study on the night-time effect in trauma care. Emerg Med J. 2014;31:808–812. doi: 10.1136/emermed-2013-202338. [DOI] [PubMed] [Google Scholar]
- 13.Egol K.A., Tolisano A.M., Spratt K.F. Mortality rates following trauma: the difference is night and day. J Emergencies, Trauma, Shock. 2011;4:178–183. doi: 10.4103/0974-2700.82202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Curtis K., Chong S., Mitchell R. Outcomes of severely injured adult trauma patients in an Australian health service: does trauma center level make a difference? World J Surg. 2011;35:2332–2340. doi: 10.1007/s00268-011-1217-1. [DOI] [PubMed] [Google Scholar]
- 15.Garwe T., Cowan L.D., Neas B. Survival benefit of transfer to tertiary trauma centers for major trauma patients initially presenting to nontertiary trauma centers. Acad Emerg Med. 2010;17:1223–1232. doi: 10.1111/j.1553-2712.2010.00918.x. [DOI] [PubMed] [Google Scholar]
- 16.Hilbert P., Lefering R., Stuttmann R. Trauma care in Germany: major differences in case fatality rates between centers. Deutsch Arztebl Int. 2010;107:463–469. doi: 10.3238/arztebl.2010.0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zacher M.T., Kanz K.G., Hanschen M. Association between volume of severely injured patients and mortality in German trauma hospitals. Br J Surg. 2015;102:1213–1219. doi: 10.1002/bjs.9866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown J.B., Rosengart M.R., Kahn J.M. Impact of volume change over time on trauma mortality in the United States. Ann Surg. 2017;266:173–178. doi: 10.1097/SLA.0000000000001838. [DOI] [PubMed] [Google Scholar]
- 19.Andruszkow H., Lefering R., Frink M. Survival benefit of helicopter emergency medical services compared to ground emergency medical services in traumatized patients. Crit Care. 2013;17:R124. doi: 10.1186/cc12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown J.B., Stassen N.A., Bankey P.E. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69:1030–1034. doi: 10.1097/TA.0b013e3181f6f450. [DOI] [PubMed] [Google Scholar]
- 21.Hannay R.S., Wyrzykowski A.D., Ball C.G. Retrospective review of injury severity, interventions and outcomes among helicopter and nonhelicopter transport patients at a Level 1 urban trauma centre. Can J Surg. 2014;57:49–54. doi: 10.1503/cjs.000113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bansal V., Fortlage D., Lee J.G. Hemorrhage is more prevalent than brain injury in early trauma deaths: the golden six hours. Eur J Trauma Emerg Surg. 2009;35:26–30. doi: 10.1007/s00068-008-8080-2. [DOI] [PubMed] [Google Scholar]
- 23.Alarhayem A.Q., Myers J.G., Dent D. Time is the enemy: mortality in trauma patients with hemorrhage from torso injury occurs long before the "golden hour. Am J Surg. 2016;212:1101–1105. doi: 10.1016/j.amjsurg.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 24.Lauerman M.H., Dubose J., Cunningham K. Delayed interventions and mortality in trauma damage control laparotomy. Surgery. 2016;160:1568–1575. doi: 10.1016/j.surg.2016.05.044. [DOI] [PubMed] [Google Scholar]
- 25.Seamon M.J., Fisher C.A., Gaughan J. Prehospital procedures before emergency department thoracotomy: "scoop and run" saves lives. J Trauma. 2007;63:113–120. doi: 10.1097/TA.0b013e31806842a1. [DOI] [PubMed] [Google Scholar]
- 26.Swaroop M., Straus D.C., Agubuzu O. Pre-hospital transport times and survival for hypotensive patients with penetrating thoracic trauma. J Emergencies, Trauma, Shock. 2013;6:16–20. doi: 10.4103/0974-2700.106320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Band R.A., Pryor J.P., Gaieski D.F. Injury-adjusted mortality of patients transported by police following penetrating trauma. Acad Emerg Med. 2011;18:32–37. doi: 10.1111/j.1553-2712.2010.00948.x. [DOI] [PubMed] [Google Scholar]
- 28.Busch J. Shots fired: when a police car becomes an ambulance. In Philadelphia cops can transport penetrating-trauma patients; will other systems follow suit? EMS World. 2013;42:I8. [PubMed] [Google Scholar]
- 29.Hussmann B., Lendemans S. Pre-hospital and early in-hospital management of severe injuries: changes and trends. Injury. 2014;45:S39–S42. doi: 10.1016/j.injury.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 30.Huber-Wagner S., Biberthaler P., Haberle S. Whole-body CT in haemodynamically unstable severely injured patients--a retrospective, multicentre study. PloS One. 2013;8 doi: 10.1371/journal.pone.0068880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huber-Wagner S., Lefering R., Qvick L.M. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet. 2009;373:1455–1461. doi: 10.1016/S0140-6736(09)60232-4. [DOI] [PubMed] [Google Scholar]
- 32.Caputo N.D., Stahmer C., Lim G. Whole-body computed tomographic scanning leads to better survival as opposed to selective scanning in trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;77:534–539. doi: 10.1097/TA.0000000000000414. [DOI] [PubMed] [Google Scholar]
- 33.Hajibandeh S., Hajibandeh S. Systematic review: effect of whole-body computed tomography on mortality in trauma patients. J Inj Violence Res. 2015;7:64–74. doi: 10.5249/jivr.v7i2.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trentzsch H., Lefering R., Nienaber U. The role of biological sex in severely traumatized patients on outcomes: a matched-pair analysis. Ann Surg. 2015;261:774–780. doi: 10.1097/SLA.0000000000000789. [DOI] [PubMed] [Google Scholar]
- 35.Wutzler S., Maegele M., Wafaisade A. Risk stratification in trauma and haemorrhagic shock: scoring systems derived from the TraumaRegister DGU®. Injury. 2014;45:S29–S34. doi: 10.1016/j.injury.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 36.Staudenmayer K., Wang N.E., Weiser T.G. The triage of injured patients: mechanism of injury, regardless of injury severity, determines hospital destination. Am Surg. 2016;82:356–361. [PMC free article] [PubMed] [Google Scholar]
- 37.Demetriades D., Kuncir E., Murray J. Mortality prediction of head abbreviated injury score and glasgow coma scale: analysis of 7,764 head injuries. J Am Coll Surg. 2004;199:216–222. doi: 10.1016/j.jamcollsurg.2004.02.030. [DOI] [PubMed] [Google Scholar]
- 38.Sartorius D., Le Manach Y., David J.S. Mechanism, glasgow coma scale, age, and arterial pressure (MGAP): a new simple prehospital triage score to predict mortality in trauma patients. Crit Care Med. 2010;38:831–837. doi: 10.1097/CCM.0b013e3181cc4a67. [DOI] [PubMed] [Google Scholar]
- 39.Deasy C., Bray J., Smith K. Traumatic out-of-hospital cardiac arrests in Melbourne, Australia. Resuscitation. 2012;83:465–470. doi: 10.1016/j.resuscitation.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 40.Grasner J.T., Wnenet J., Seewald S. Cardiopulmonary resuscitation traumatic cardiac arrest--there are survivors. An analysis of two national emergency registries. Crit Care. 2011;15:R276. doi: 10.1186/cc10558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zwingmann J., Lefering R., Feucht M. Outcome and predictors for successful resuscitation in the emergency room of adult patients in traumatic cardiorespiratory arrest. Crit Care. 2016;20:282. doi: 10.1186/s13054-016-1463-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Logters T., Lefering R., Schneppendahl J. Interruption of the diagnostic algorithm and immediate surgical intervention after major trauma--incidence and clinical relevance. Analysis of the Trauma Register of the German Society for Trauma Surgery. Unfallchirurg. 2010;113:832–838. doi: 10.1007/s00113-010-1772-1. [DOI] [PubMed] [Google Scholar]
- 43.Seamon M.J., Doane S.M., Gaughan J.P. Prehospital interventions for penetrating trauma victims: a prospective comparison between advanced life support and basic life support. Injury. 2013;44:634–638. doi: 10.1016/j.injury.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 44.Zafar S.N., Haider A.H., Stevens K.A. Increased mortality associated with EMS transport of gunshot wound victims when compared to private vehicle transport. Injury. 2014;45:1320–1326. doi: 10.1016/j.injury.2014.05.032. [DOI] [PubMed] [Google Scholar]
- 45.Deng Q., Tang B., Xue C. Comparison of the ability to predict mortality between the injury severity score and the new injury severity score: a meta-analysis. Int J Environ Res Publ Health. 2016;13:825. doi: 10.3390/ijerph13080825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smith B.P., Goldberg A.J., Gaughan J.P. A comparison of injury severity score and new injury severity score after penetrating trauma: a prospective analysis. J Trauma Acute Care Surg. 2015;79:269–274. doi: 10.1097/TA.0000000000000753. [DOI] [PubMed] [Google Scholar]
- 47.Eid H.O., Abu-Zidan F.M. New Injury Severity Score is a better predictor of mortality for blunt trauma patients than the Injury Severity Score. World J Surg. 2015;39:165–171. doi: 10.1007/s00268-014-2745-2. [DOI] [PubMed] [Google Scholar]
- 48.Balogh Z., Offner P.J., Moore E.E. NISS predicts postinjury multiple organ failure better than the ISS. J Trauma. 2000;48:624–627. doi: 10.1097/00005373-200004000-00007. [DOI] [PubMed] [Google Scholar]