Abstract
High tibial osteotomy for medial-compartment knee osteoarthritis (OA) is an established biological knee reconstruction surgical procedure. In open- and closed-wedge high tibial osteotomy, the angulation correction axes are away from the center of rotation and angulation. This results in translation deformity, which alters the orientation of the adjacent joint and the length of the limb. In the present study, we combined the distal tibial tuberosity focal dome osteotomy centered on the center of rotation and angulation with the longitudinal condylar osteotomy (focal dome condylar osteotomy) for knee OA. The advantages of this procedure are as follows: physiological orientation of adjacent joint is achieved; limb length is maintained; joint stabilization in the coronal plane is achieved; patella infra is prevented; sufficient bone contact between the medial and posterior cortex is achieved; early weight-bearing walking is possible; and fibular osteotomy is not required. This study describes the details of the surgical procedure, including our compass cutter for accurate dome osteotomy and the postoperative rehabilitation program for patients with knee OA and moderate-to-severe varus deformity.
High tibial osteotomy (HTO) is an established biological knee reconstruction surgery1, 2, 3 for medial-compartmental osteoarthritis (OA) of the knee joint wherein medial open-wedge high tibial osteotomy (OWHTO)4 and lateral closed-wedge high tibial valgus osteotomy (CWHTO)5 are mainly applied. Recently, OWHTO has been widely performed6,7 with improvements that include fixation with a locking plate for improved stability,8 biplanar osteotomy for a better bony union,9 and the use of new bone-substituting biomaterials to achieve local stability.10, 11, 12 This procedure has been associated with several drawbacks, such as difficulty in obtaining sufficient correction in the case of a severe varus deformity, alterations in the anteroposterior tibial slope angle, increase in limb length, and development of patellar infra with large correction, which leads to patellofemoral joint OA over the course of time.13, 14, 15
CWHTO is technically much more demanding, has a high complication rate, and needs a relatively long period for bone union.16 Moreover, it requires additional fibular osteotomy, which is associated with the potential risk for peroneal nerve injury. Recently, a new surgical procedure combining OWHTO and CWHTO with improved bone union has been introduced, although a fibular osteotomy is still mandatory.17
OW and CW HTO are not concerned with the relationship of the center of rotation and angulation (CORA), resulting in a secondary translation deformity in many cases, which leads to the non-physiological orientation of the adjacent ankle joint.18
The CORA in the OA knee exists at the level of the intersection of the mechanical axis of the femur and tibia.19, 20, 21 The best outcome of HTO is achieved when the mechanical axis of the lower limb passes through the Fujisawa point22; therefore, the corrective osteotomy in the OA knee should be performed at this point. Using this method, the CORA in the OA knee is estimated in the coronal plane. Focal dome osteotomy is a dome-shaped osteotomy wherein the CORA corresponds to the center of the dome; thus, the development of a secondary translation deformity is avoided and the physiological adjacent joint orientation is maintained.23
In this study, we present a technique for medial-compartmental knee OA treatment called the FDCO (focal dome condylar osteotomy). This procedure offers the CORA method-oriented proximal tibial osteotomy and achieves the physiological orientation of the adjacent joint. In addition, improvement in joint instability in the coronal plane is achieved by gap opening via intra-articular osteotomy. Osteotomy performed below the tibial tuberosity prevents patella infra, and dome osteotomy achieves bony contact, resulting in a potentially secure fixation that could lead to an improved union of the bones after the osteotomy.
Surgical Technique
Indications
The indications for this technique include symptomatic medial-compartmental knee OA (Kellgren–Lawrence OA grade >2), spontaneous osteonecrosis of the medial femoral condyle without lateral compartmental OA, no systemic inflammatory arthritis, and an intact anterior cruciate ligament (ACL).
Preoperative Planning
Anteroposterior, lateral, and skyline views of the knee, an anteroposterior view of the weight-bearing knee, and a full-length lower limb radiograph are required. Magnetic resonance imaging is used to diagnose ACL, meniscal, and cartilage injuries.
Preoperative planning is performed using a prone, full-length radiograph of the lower limb. The mechanical lateral distal femoral angle and mechanical medial proximal tibial angle are measured to confirm the origin of the limb deformity. Then, the weight-bearing line is drawn from the center of the femoral head to the center of the talar dome. The point where the mechanical axis (MA) crosses the tibial plateau is determined. Preoperative planning is used to see that the MA passes the Fujisawa point on the lateral tibial plateau after surgery22 (Fig 1A). Then, the mechanical tibial axis is drawn as it orthogonally crosses the talar dome. The point where the 2 lines cross is defined as the CORA (Fig 1B). When the CORA exists near the knee joint, the below tibial tubercle dome osteotomy centering CORA is determined. The correction angle is determined by the 2 lines. The ascending intra-articular osteotomy is set just lateral to the patellar tendon (Fig 1C). After the correction, the MA passes through the Fujisawa point and crosses the ankle joint orthogonally (Fig 1 D and E). A simple, one-plane dome osteotomy combined with gradual correction using external fixator may be applied in cases in which the CORA exists far above or below the knee joint.23
Fig 1.
Scheme of the focal dome condylar osteotomy in the right lower limb. (A) Check the mechanical axis of the lower limb and Fujisawa point (red star). (B) Check mechanical axis of the tibia passes through Fujisawa point. (C) Focal dome osteotomy (red dome line) and intra-articular longitudinal osteotomy (red line). (D) Correction. (E) Plate fixation and artificial bone grafting (blue trapezoid). Lateral cortex of the tibia is maintained.
Preparation and Patient Positioning (With Video Illustration)
The patient is placed in a supine position on the radiolucent operating table under general and epidural anesthesia (Video 1).22, 23, 24 The whole lower limb is sterilized with povidone–iodine.
Arthroscopic Technique
Diagnostic arthroscopy is performed to confirm the presence of isolated medial-compartment OA, an intact lateral compartment, and an intact ACL. Subsequently, arthroscopic debridement, meniscectomy, and synovectomy are performed. The osteophytes are arthroscopically harvested for subsequent implantation into the gap formed by the osteotomy.24
Exposure
An 8- to 10-cm longitudinal incision is made from the anteromedial parapatellar portal to the anteromedial tibial cortex. The tendons of the semitendinosus muscle and gracilis muscle are incised in an L-shaped pattern. The superficial medial collateral ligament (MCL) and the underlying periosteum are partially elevated with a Cobb elevator. The posterior aspect of the tibial periosteum was carefully elevated to protect the neurovascular bundle (Fig 2).
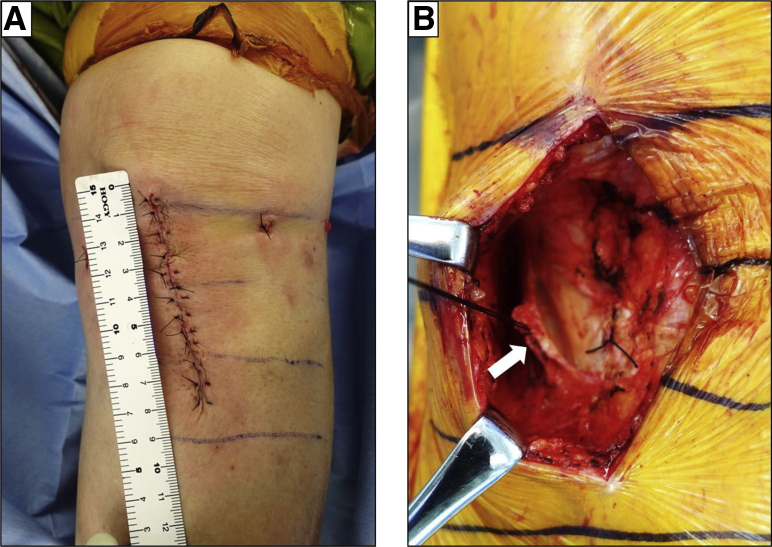
Fig 2.
Skin incision and exposure (left leg). (A) An 8-cm skin incision is made from medial parapatellar portal to the proximal tibia of the left leg. (B) Tendons of the semitendinosus muscle and gracilis muscle are incised with an L-shape (white arrow).
Determination of Dome Osteotomy Lines
A previously planned CORA is determined using C-arm fluoroscopic imaging. A 3-mm-thick Kirschner wire (K wire) is inserted into the CORA from the anterior to posterior direction as the center of the dome osteotomy (Fig 3A). A compass cutter (Zimmer Biomet, Warsaw, IN) is applied to the K wire and the radius is determined based on the preoperative planning (Fig 3B). Another 3-mm K wire is inserted lateral to the patellar tendon and parallel to the CORA wire (Fig 3C).
Fig 3.
Focal dome condylar osteotomy procedure using the Sawbone model (right leg). (A) Previously planned CORA is determined and a 3-mm-thick Kirschner wire (K wire) is inserted at the center of the dome osteotomy. (B) The radius of the dome osteotomy is determined using a compass cutter. (C) Another 3-mm K wire is inserted just lateral to the patellar tendon. (D) A 2-mm K wire is inserted from the lateral tibial plateau to the distal tibia to protect the lateral cortex. (E) Focal dome osteotomy is performed with a reciprocating saw using a compass cutter. (F) Two 1.2-mm K wires are inserted just below the tibial plateau to protect hinge during gap opening. (G) Longitudinal intra-articular osteotomy is performed. (H) The longitudinal osteotomy site is opened using a spreader until the mechanical axis passes through the Fujisawa point. (I) A TriS plate (Olympus Terumo Biomaterials, Tokyo, Japan) is used for the fixation. (CORA, center of rotation and angulation.)
A 2-mm K wire is percutaneously inserted from the edge of the lateral tibial plateau to the distal tibia, lateral to the 3-mm K wires to protect the lateral cortex of the tibia during dome osteotomy (Fig 3D). A radiolucent retractor was inserted between the tibia and the detached posterior structures to protect the neurovascular structures.
A reciprocating saw is used through the compass cutter to perform the dome osteotomy (Fig 3E). Two to three 1.2-mm K wires are percutaneously inserted just below the tibial plateau to protect hinge during gap opening (Fig 3F). Subsequently, longitudinal osteotomy is performed between the 3-mm K wires using the reciprocating saw (Fig 3G and 4A).
Fig 4.
C-arm imaging of the operation (right leg). The surgical position of the knee is at full extension with the patella upward. A CORA K wire and lateral cortex protection K wire are inserted. A radiolucent retractor was inserted between the tibia and the detached posterior structures to protect the neurovascular structures. (A) Focal dome osteotomy is performed using compass cutter. And longitudinal osteotomy is performed. (B) After hinge protection, K wires are inserted percutaneously, longitudinal osteotomy site is opened using spreader to the mechanical axis passes through the Fujisawa point. (CORA, center of rotation and angulation.)
After ensuring that the osteotomies are completed with the hinge area intact, the longitudinal osteotomy site is opened with several chisels and a bone spreader until the MA passed through the Fujisawa point (Fig 3H and 4B).
Implant Placement
A TriS plate (Olympus Terumo Biomaterials, Tokyo, Japan) is used for the fixation. After plate fixation, the gap formed by the osteotomy is filled using harvested autologous osteophyte grafts and β-TCP (Osferion 60; Olympus Terumo Biomaterials). Finally, bi-cortical screw fixation from the tuberosity to the posterior tibia is performed to prevent tuberosity avulsion fracture during rehabilitation. The wound is irrigated and a surgical drain is placed. Closure of the wound is achieved with absorbable sutures placed in layers then 5-0 nylon suture. The preoperative and postoperative (6 months) radiographs are shown in Figure 5, and the postoperative (2 weeks and 3 months) reconstruction computed tomography imaging of the osteotomy site is shown in Figure 6.
Fig 5.
Pre- and 6 months' postoperative radiograph of right leg in a 40-year-old female patient with knee osteoarthritis. (A) Preoperative anteroposterior view. (B) Preoperative lateral view. (C) Preoperative whole leg standing view. The weight-bearing line (white line) goes through the medial compartment of the knee. (D) Postoperative anteroposterior view. (E) Postoperative lateral view. (F) Postoperative whole leg standing view. The weight-bearing line (white line) is shifted laterally and orthogonally cross the ankle joint.
Fig 6.
Postoperative CT imaging of the dome osteotomy site. (A) Coronal reconstruction of the CT imaging of dome osteotomy site (white circle) 2 weeks after surgery. Wide cancellous bone contact of the osteotomy site is achieved. (B) Sagittal reconstruction of the CT imaging of dome osteotomy site (white circle) 2 weeks after surgery. Bony contact of the posterior cortex is achieved. (C) Coronal reconstruction of the CT imaging of dome osteotomy site (white circle) 3 month after surgery. Bony union and continuity of the cancellous bone is observed. (D) Sagittal reconstruction of the CT imaging of dome osteotomy site (white circle) 3 month after surgery. Callus formation is observed at posterior cortex. (CT, computed tomography.)
Postoperative Rehabilitation
The day after the surgery, the drain is removed and active and passive range-of-motion exercises, including continuous passive motion and quadriceps muscle strengthening exercises, are initiated. The patient is asked to remain non-weight-bearing for 2 weeks. The weight-bearing is gradually increased with clinical and radiographic evidence of bone healing. Moderate sports activities are allowed at 3 months postoperatively.
Discussion
This is the study to describe the concept, indication, and the surgical technique of FDCO for medial knee OA. The described procedure has several advantages compared with OWHTO and CWHTO (Table 1). OWHTO has been reported to increase the length of the lower limb, whereas CWHTO decreases the length of the lower limb.25 In the FDCO procedure, the dome osteotomy centering CORA; thus, the length of the leg is not altered.
Table 1.
Advantages and Disadvantages of FDCO
| Advantages |
|
| Limitations |
|
CORA, center of rotation of angulation; FDCO, focal dome condylar osteotomy; OWHTO, opening-wedge high tibial osteotomy.
The OWHTO and CWHTO procedures do not involve the CORA, and the osteotomy site is away from the angulation correction axis. Thus, secondary translation deformity leads to a change in the orientation of the adjacent ankle joint after osteotomy.18 For FDCO, the mechanical tibial axis is drawn as it orthogonally crosses the talar dome; hence, in the case of focal dome osteotomy, the physiological orientation of the adjacent ankle joint is maintained. The advantages of a dome osteotomy are adjustability, large bone to bone contact, and stability.26 The disadvantages include technical difficulties and incompatibility with rotational correction. The technical difficulty can be overcome by a compass cutter. And there is risk for damaging neurovascular bundle during osteotomy. The posterior aspect of the tibial periosteum must be carefully elevated, and a retractor must be inserted between the tibia and the detached posterior structures during osteotomy to prevent neurovascular damaging (Table 2).
Table 2.
Pearls and Pitfalls
| Pearls |
|
|
|
| Pitfalls |
|
|
Dome osteotomy of the FDCO is performed above the attachment of the superficial layer of the MCL, and the redundant MCL is tightened after correction. This improves joint stability in the coronal plane. Unlike in the OWHTO procedure, when the dome osteotomy is performed below the tibial tuberosity, the orientation of the patella and femur are maintained after correction. Progression of the patellofemoral OA after OWHTO has been observed in 27% of cases, radiographically; in addition, chondral damage has been reported in 45% of cases by arthroscopy.27 Dome osteotomy below the tibial tubercle prevents the increase in patellofemoral pressure and may prevent patellofemoral OA.
High stability of the osteotomy site is necessary for bone healing in HTO. This technique maintains the wide contact surface area of the cancellous bone and posterior cortex around the dome osteotomy site, which may lead to early bone union, and early weight-bearing is possible. Limitation of the FDCO is that this procedure can be applied when the CORA exists near the knee joint. A simple one-plane dome osteotomy combined with gradual correction using external fixator may be applied in cases in which the CORA exists far above or below the tibial plateau.23
One limitation of this study is that only the concept and procedure of our osteotomy technique was presented. To prove the significance of this procedure, it is necessary to conduct a randomized controlled trial with conventional OWHTO.
In this study, we have introduced a surgical technique, FDCO, as a CORA method-oriented MA re-alignment with proximal tibial osteotomy for medial-compartmental knee OA. This method helps in the physiological orientation of the adjacent ankle joint after the surgery. Gap opening with intra-articular osteotomy improves joint stability in the coronal plane. Osteotomy below the tibial tuberosity prevents patella infra and minimizes the risk for patellofemoral pathology. In addition, dome osteotomy achieves medial and posterior bony contact and a potentially tight fixation, which leads to an improved union of the bone. Additional randomized clinical trials with conventional OWHTO will be necessary to demonstrate the clinical significance of this procedure.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows the surgical technique of distal tibial tuberosity focal dome osteotomy combined with intra-articular condylar osteotomy in the left knee. The patient is placed in a supine position on the radiolucent operating table under general and epidural anesthesia. The other leg is positioned at a lower level to provide for an easier approach to the medial aspect of the operative knee during the surgery. Diagnostic arthroscopy is performed from anterolateral parapatellar portal to confirm the isolated medial-compartment osteoarthritis. Subsequently, arthroscopic debridement and meniscectomy are performed from anteromedial parapatellar portal. The osteophytes are arthroscopically harvested for subsequent implantation into the gap formed by the osteotomy.24 An 8-cm longitudinal incision is made from the anteromedial portal to the anteromedial tibial cortex. The tendons of the semitendinosus muscle and gracilis muscle are incised in an L-shaped pattern. The posterior aspect of the tibial periosteum is carefully elevated to protect the neurovascular bundle. A previously planned CORA23 is determined using C-arm fluoroscopic imaging. A 3-mm K wire is inserted into the CORA as the center of the dome osteotomy. A compass cutter is applied to the K wire and the radius is determined. Another 3-mm K wire is inserted on the radius. A 2-mm K wire is percutaneously inserted to the distal tibia to protect the lateral cortex of the tibia during dome osteotomy. A reciprocating saw is used through the compass cutter to perform the dome osteotomy. Subsequently, longitudinal osteotomy is performed. The longitudinal osteotomy site is opened with several chisels and a bone spreader until the mechanical axis passes through the Fujisawa point.22 A locking plate is used for the fixation. The gap is filled using harvested autologous osteophyte grafts and formed β-tricalcium phosphate wedges. In addition, bi-cortical screw fixation from the tuberosity is performed using a cannulated screw. A surgical drain is placed. Closure of the wound is achieved with absorbable sutures placed in layers. (CORA, center of rotation and angulation.)
References
- 1.Jackson J.P., Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43:746–751. doi: 10.1302/0301-620X.43B4.746. [DOI] [PubMed] [Google Scholar]
- 2.Coventry M.B. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. J Bone Joint Surg Am. 1965;47:984–990. [PubMed] [Google Scholar]
- 3.Akizuki S., Shibakawa A., Takizawa T., Yamazaki I., Horiuchi H. The long-term outcome of high tibial osteotomy. J Bone Joint Surg Br. 2008;90:592–596. doi: 10.1302/0301-620X.90B5.20386. [DOI] [PubMed] [Google Scholar]
- 4.Floerkemeier S., Staubli A.E., Schroeter S., Goldhahn S., Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: A retrospective evaluation of 533 patients. Knee Surg Sport Traumatol Arthrosc. 2013;21:170–180. doi: 10.1007/s00167-012-2087-2. [DOI] [PubMed] [Google Scholar]
- 5.Efe T., Ahmed G., Heyse T.J. Closing-wedge high tibial osteotomy: Survival and risk factor analysis at long-term follow up. BMC Musculoskelet Disord. 2011;12:46. doi: 10.1186/1471-2474-12-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lobenhoffer P., Agneskirchner J.D. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sport Traumatol Arthrosc. 2003;11:132–138. doi: 10.1007/s00167-002-0334-7. [DOI] [PubMed] [Google Scholar]
- 7.Staubli A.E., Simoni C De, Babst R., Lobenhoffer P. TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia—early results in 92 cases. Injury. 2003;34:55–62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 8.Niemeyer P., Koestler W., Kaehny C. Two-year results of open-wedge high tibial osteotomy with fixation by medial plate fixator for medial compartment arthritis with varus malalignment of the knee. Arthrosc J Arthrosc Relat Surg. 2008;24:796–804. doi: 10.1016/j.arthro.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 9.Birmingham T.B., Giffin J.R., Chesworth B.M. Medial opening wedge high tibial osteotomy: A prospective cohort study of gait, radiographic, and patient-reported outcomes. Arthritis Rheum. 2009;61:648–657. doi: 10.1002/art.24466. [DOI] [PubMed] [Google Scholar]
- 10.Onodera J., Kondo E., Omizu N., Ueda D., Yagi T., Yasuda K. Beta-tricalcium phosphate shows superior absorption rate and osteoconductivity compared to hydroxyapatite in open-wedge high tibial osteotomy. Knee Surg Sport Traumatol Arthrosc. 2014;22:2763–2770. doi: 10.1007/s00167-013-2681-y. [DOI] [PubMed] [Google Scholar]
- 11.Osti M., Gohm A., Schlick B., Benedetto K.P. Complication rate following high tibial open-wedge osteotomy with spacer plates for incipient osteoarthritis of the knee with varus malalignment. Knee Surg Sport Traumatol Arthrosc. 2015;23:1943–1948. doi: 10.1007/s00167-013-2757-8. [DOI] [PubMed] [Google Scholar]
- 12.Saito T., Kumagai K., Akamatsu Y., Kobayashi H., Kusayama Y. Five- to ten-year outcome following medial opening-wedge high tibial osteotomy with rigid plate fixation in combination with an artificial bone substitute. Bone Joint J. 2014;96:339–344. doi: 10.1302/0301-620X.96B3.32525. [DOI] [PubMed] [Google Scholar]
- 13.Elmalı N., Esenkaya İ., Can M., Karakaplan M. Monoplanar versus biplanar medial open-wedge proximal tibial osteotomy for varus gonarthrosis: A comparison of clinical and radiological outcomes. Knee Surg Sport Traumatol Arthrosc. 2013;21:2689–2695. doi: 10.1007/s00167-012-2040-4. [DOI] [PubMed] [Google Scholar]
- 14.Gaasbeek R.D.A., Sonneveld H., van Heerwaarden R.J., Jacobs W.C.H., Wymenga A.B. Distal tuberosity osteotomy in open wedge high tibial osteotomy can prevent patella infera: A new technique. Knee. 2004;11:457–461. doi: 10.1016/j.knee.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Longino P.D., Birmingham T.B., Schultz W.J., Moyer R.F., Giffin J.R. Combined tibial tubercle osteotomy with medial opening wedge high tibial osteotomy minimizes changes in patellar height. Am J Sports Med. 2013;41:2849–2857. doi: 10.1177/0363546513505077. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki T., Yagi T., Monji J., Yasuda K., Tsuge H. High tibial osteotomy combined with anterior displacement of the tibial tubercle for osteoarthritis of the knee. Int Orthop. 1986;10:31–40. doi: 10.1007/BF00266270. [DOI] [PubMed] [Google Scholar]
- 17.Takeuchi R., Ishikawa H., Miyasaka Y., Sasaki Y., Kuniya T., Tsukahara S. A novel closed-wedge high tibial osteotomy procedure to treat osteoarthritis of the knee: Hybrid technique and rehabilitation measures. Arthrosc Tech. 2014;3:431–437. doi: 10.1016/j.eats.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi G.W., Yang J.H., Park J.H. Changes in coronal alignment of the ankle joint after high tibial osteotomy. Knee Surg Sport Traumatol Arthrosc. 2017;25:838–845. doi: 10.1007/s00167-015-3890-3. [DOI] [PubMed] [Google Scholar]
- 19.Paley D. Problems, obstacles and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;(250):81–104. [PubMed] [Google Scholar]
- 20.Paley D., Tetwworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res. 1992;280:48–64. [PubMed] [Google Scholar]
- 21.Paley D., Herzenberg J.E., Tetsworth K., McKie J., Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 22.Fujisawa Y., Masuhara K., Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10:585–608. [PubMed] [Google Scholar]
- 23.Paley D. Springer-Verlag; New York: 2002. Principles of deformity corrections. [Google Scholar]
- 24.Akiyama T., Okazaki K., Mawatari T., Ikemura S., Nakamura S. Autologous osteophyte grafting for open-wedge high tibial osteotomy. Arthrosc Tech. 2016;5:989–995. doi: 10.1016/j.eats.2016.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bae D.K., Song S.J., Kim H.J., Seo J.W. Change in limb length after high tibial osteotomy using computer-assisted surgery: A comparative study of closed- and open-wedge osteotomies. Knee Surg Sport Traumatol Arthrosc. 2013;21:120–126. doi: 10.1007/s00167-012-1898-5. [DOI] [PubMed] [Google Scholar]
- 26.Watanabe K., Tsuchiya H., Sakurakichi K., Matsubara H., Tomita K. Acute correction using focal dome osteotomy for deformity about knee joint. Arch Orthop Trauma Surg. 2008;128:1373–1378. doi: 10.1007/s00402-008-0574-1. [DOI] [PubMed] [Google Scholar]
- 27.Goshima K., Sawaguchi T., Shigemoto K., Iwai S., Nakanishi A., Ueoka K. Patellofemoral osteoarthritis progression and alignment changes after open-wedge high tibial osteotomy do not affect clinical outcomes at mid-term follow-up. Arthroscopy. 2017;33:1832–1839. doi: 10.1016/j.arthro.2017.04.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows the surgical technique of distal tibial tuberosity focal dome osteotomy combined with intra-articular condylar osteotomy in the left knee. The patient is placed in a supine position on the radiolucent operating table under general and epidural anesthesia. The other leg is positioned at a lower level to provide for an easier approach to the medial aspect of the operative knee during the surgery. Diagnostic arthroscopy is performed from anterolateral parapatellar portal to confirm the isolated medial-compartment osteoarthritis. Subsequently, arthroscopic debridement and meniscectomy are performed from anteromedial parapatellar portal. The osteophytes are arthroscopically harvested for subsequent implantation into the gap formed by the osteotomy.24 An 8-cm longitudinal incision is made from the anteromedial portal to the anteromedial tibial cortex. The tendons of the semitendinosus muscle and gracilis muscle are incised in an L-shaped pattern. The posterior aspect of the tibial periosteum is carefully elevated to protect the neurovascular bundle. A previously planned CORA23 is determined using C-arm fluoroscopic imaging. A 3-mm K wire is inserted into the CORA as the center of the dome osteotomy. A compass cutter is applied to the K wire and the radius is determined. Another 3-mm K wire is inserted on the radius. A 2-mm K wire is percutaneously inserted to the distal tibia to protect the lateral cortex of the tibia during dome osteotomy. A reciprocating saw is used through the compass cutter to perform the dome osteotomy. Subsequently, longitudinal osteotomy is performed. The longitudinal osteotomy site is opened with several chisels and a bone spreader until the mechanical axis passes through the Fujisawa point.22 A locking plate is used for the fixation. The gap is filled using harvested autologous osteophyte grafts and formed β-tricalcium phosphate wedges. In addition, bi-cortical screw fixation from the tuberosity is performed using a cannulated screw. A surgical drain is placed. Closure of the wound is achieved with absorbable sutures placed in layers. (CORA, center of rotation and angulation.)