Abstract
Anterior cruciate ligament reconstruction after graft failure may need associated bone correction to ensure stability of the knee. This article presents a technique of posteromedial opening-wedge osteotomy using a custom cutting guide to correct increased tibial slope and metaphyseal varus deformity after recurrent graft failure. An autograft quadriceps tendon graft was selected for the revision anterior cruciate ligament graft. After exposure with an anteromedial incision a patient specific cutting guide was used to make the high tibial osteotomy. The final fixation of the posteromedial opening was achieved using a low-profile locking plate and a femoral head allograft bone wedge. The tibial tunnel was planned and included in the patient-specific cutting guide. The femoral tunnel was placed using an outside to in manner. Bioabsorbable screws were used as fixation devices.
Increased tibial slope can be a cause of anterior cruciate ligament (ACL) reconstruction failure.1 Several articles have described various techniques to correct the tibial slope deformity.2,3 Traditionally, anterior closing osteotomies have been promoted in those cases, but in combined deformities such as varus and excessive slope abnormalities, posterior openings allow simultaneous correction and avoidance of tibial tuberosity osteotomy.4 Three-dimensional patient-specific cutting guides (PSCGs) have demonstrated their benefits in terms of improved precision, reduced operative time, and a reduction in the number of fluoroscopic images taken intraoperatively.5,6 Those guides also include a tibial tunnel guide to avoid conflict between screws and ACL tunnels. The purpose of this Technical Note is to describe a high tibial osteotomy combining posteromedial opening-wedge osteotomy and an ACL reconstruction with quadriceps tendon graft in a patient requiring bone deformity correction and ACL revision in a chronic knee instability setting.
Surgical Technique
Indications and Contraindications
This surgery is indicated after ACL reconstruction failure(s) for patients presenting with an increased posterior tibial slope and a symptomatic and substantial metaphyseal tibia vara (Video 1). Christensen et al.1 identified that the addition of 2° on a normal tibial slope increased graft failure by 1.6 (95% confidence interval 1.1-2.2). Contraindications for this procedure include a Kellgren–Lawrence grade IV osteoarthritis, osteoporosis, and knee recurvatum.
Preoperative Planning
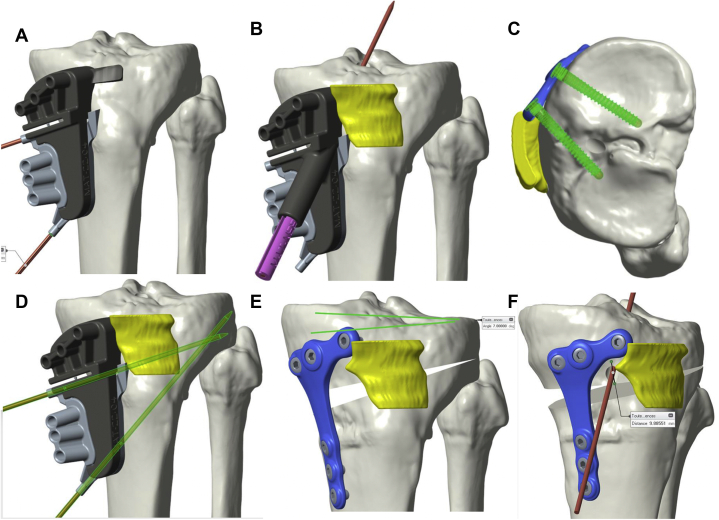
Rather than using standard radiography, one of the interests of this procedure is the ability to use 3-dimensional planning, thereby increasing the precision of the correction. There is a better understanding of the different elements (cutting plane direction, hinge and wedge position) influencing the ability to correct frontal and sagittal planes (Fig 1 A-E). A preoperative computed tomography (CT) scan is needed to plan multiple virtual osteotomies, before identifying the best option and creating the appropriate PSCG.
Fig 1.
CT scan reconstruction of a left tibia. An example of our 3-dimensional planning and virtual osteotomy. (A) AP view. Patient-specific osteotomy guide’s position. (B) AP view. Patient-specific tibial tunnel guide’s position. (C) Superior view. Position of the tibial tunnel avoiding convergence with plate and screws. (D) AP view. Position of the saw-guiding and hinge protecting K wires. (E) AP view. Virtual osteotomy: a 7° correction is planned in the frontal plane. (F) Lateral view (medial aspect of the tibia). Virtual osteotomy: a 5° correction is planned in the frontal plane.
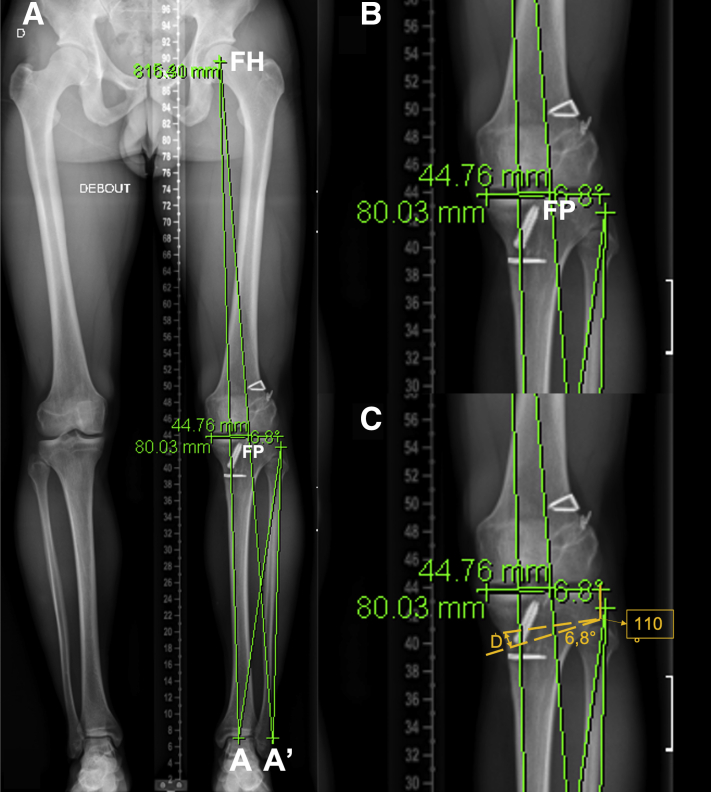
The aim of correction is to correct the tibial slope to a normal value close to 7°, but we usually limit this correction to a maximum of 8° to avoid postoperative recurvatum. Regarding the degree of correction of the varus, we usually aim for a correction of the Mikulicz line (line passing through the femoral head and the ankle joint’s centers) reaching a Fugisawa point (the intersection between the projected postoperative Mikulicz line and the tibial plateau; this point is selected by the surgeon) between 55% and 65% based on cartilage and meniscus status (Fig 2).
Fig 2.
An example of preoperative planning based on the Miniaci’s technique on a long axis X-ray (AP view); the planning is performed on the left lower-limb. The target for the Fugisawa points (FP) was set to be 65%. (A) On the full-length lower-limb radiographs, the lower-limb weight bearing line (from the femoral head center [FH] to the center of the ankle [A: line FH-A]) is drawn. A second line connecting the hip center and the Fujisawa point (line FH-FP) is drawn as well, extending to a line parallel to the ground passing through the center of the ankle previously marked (A). Line AA′ The intersection point between the line FH-FP and AA′ represent the virtual postoperative ankle’s position (A′); a line connecting the lateral tibial osteotomy site (E) and the center of the ankle joint (line 3, EA) is given, similarly another line connecting the osteotomy site and line 2 (line 4, EA′) is drawn. (B) The angle formed by lines 3 and 4 is calculated and represents the predicted correction angle (angle α). (C) A predicted osteotomy line (O) is drawn from the proximal third the fibular head to the predicted medial osteotomy site (approximately 4 cm inferior to the medial border of the tibial plateau or the medial aspect of proximal metaphyseal plateau) the optimal angulation between this line and the lateral cortex of the tibia is reported to be 110°. A predicted opening line (O′) is finally drawn from Line O at the determined correction angle (wedge angle, α). The predicted correction gap in mm at the cortical bone of the posteromedial tibia is measured (D (in mm).
To estimate the amount of correction resulting from this planning, we usually refer to the Miniaci technique7: On the preoperative anteroposterior full-length lower limb radiographs, the lower-limb weight bearing line (from the femoral head center to the center of the ankle [line FH-A]) is drawn (Fig 2A). A second line connecting the hip center and the Fujisawa point (line FH-FP) is drawn as well, extending to a line parallel to the ground passing through the center of the ankle previously marked (A) Line AA′ (Fig 2B). The intersection point between the line FH-FP and AA′ represents the virtual postoperative ankle’s position (A′). Then, a line connecting the lateral tibial osteotomy site (E) and the center of the ankle joint (line 3, EA) is given, similarly another line connecting the osteotomy site and line 2 (line 4, EA′) is drawn (Fig 2A). The angle formed by lines 3 and 4 is calculated and represents the predicted correction angle (angle α). A predicted osteotomy line (O) is drawn from the proximal third the fibular head to the predicted medial osteotomy site (approximately 4 cm inferior to the medial border of the tibial plateau or the medial aspect of proximal metaphyseal plateau). The optimal angulation between this line and the lateral cortex of the tibia is reported to be 110° (Fig 2C). A predicted opening line (O′) is finally drawn from Line O at the determined correction angle (wedge angle, α). The predicted correction gap in mm at the cortical bone of the posteromedial tibia is measured (D (in mm) (Fig 2C).
The 3-dimensional planning determines the cut line and the thickness of the added bony wedge. The CT scan is also useful to define the quality and position of previous bone tunnels. The cutting guide includes a removable piece for tibial tunnel guidance, which is also 3D planned (Fig 1). Previous tunnels are preserved, and hardware is removed as much as possible.
Surgical Procedure
The patient is placed in a dorsal decubitus position on the operating table. After general anesthesia is administered, a thigh pneumatic tourniquet is placed and supports permit a 90° flexion of the knee.
Graft Harvesting
-
•
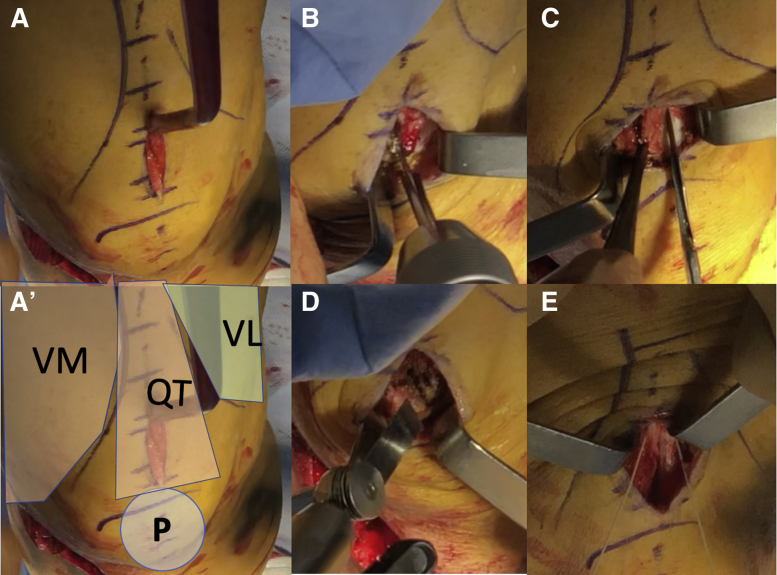
We mainly used quadriceps tendon in our revision cases: With the leg flexed to 90°, medial and lateral part of the patella are palpated.
-
•
A 4-cm vertical incision is made extending proximal from the proximal pole of the patella, just lateral to the midpoint (Fig 3A). Underlying subcutaneous tissue is dissected.
-
•
Three 2-mm holes are drilled, 2 in the distal part of the bone block to avoid fracture propagation and 1 in the middle of the bone block to put traction sutures (Fig 3B).
-
•
Farabeuf retractors are used to create a moving window including 2 cm of proximal patella and the desired length of the quadriceps graft. The central part of the patella is first prepared using electrocautery to achieve clean cut lines (Fig 3C).
-
•
A narrow saw is used to harvest the patella bone block (Fig 3D).
-
•
A Scalpel and scissors are used to dissect the superficial layer of the quadriceps tendon (Fig 3E)
-
•
The quadriceps tendon is completely closed with a resorbable thread (Fig 3G). Then, the graft is prepared with 2 nonresorbable wires and sized to determine the diameter of the tunnels (Fig 3G).
Fig 3.
Quadriceps tendon graft’s harvesting is shown. The leg flexed to 90°, and the medial and lateral part of the patella are palpated. Vastus medialis and vastus lateralis are marked. (A) A 4-cm vertical incision is made extending proximal from the proximal pole of the patella, just lateral to the midpoint. Underlying subcutaneous tissue is dissected. (A′) Orientation of the picture: VM: vastus medialis, VL: vastus Lateralis, P: patella, QT: quadriceps tendon. (B) Three 2-mm hole are drilled, 2 in the distal part of the future cut to avoid cracks and 1 in the middle of the bone block to put traction sutures. (C) Farabeuf retractors are used to create a moving window including 2 cm of proximal patella and the desired length of quadriceps graft. The central part of the patella is first prepared using cautery knife to clean cut lines. (D) A narrow saw is used to harvest the patellar bone. (E) The quadriceps tendon is completely closed with a resorbable thread.
PSCG–Opening-Wedge High Tibial Osteotomy
-
•
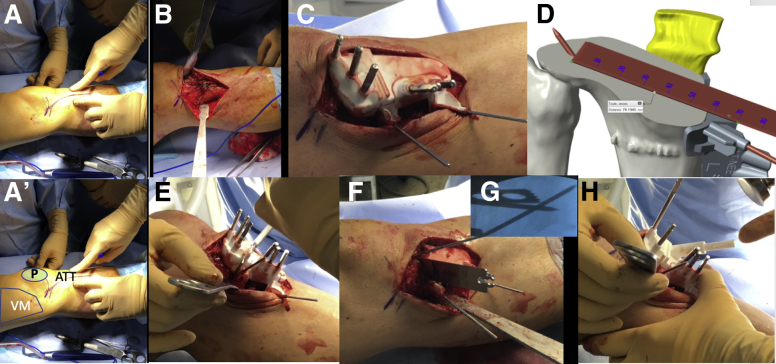
A 6- to 8-cm slightly oblique vertical incision is made along the anteromedial surface, running over the joint space down to under the tibial tuberosity (Fig 4A).
-
•
A scalpel is used to make a single-plane incision through the periosteum. The hamstrings and the medial collateral ligament are retracted posteriorly with a Cobb elevator until the medial surface of the tibia is fully visible (Fig 4B).
-
•
Previous tibial fixation devices, if present, should be removed. The deepest part of the patellar tendon is cleared down to its attachment onto the tibial tubercle. The 2 parts of PSCG are clipped together and then applied to the bone. No osteophytes have to be resected, as the guide is anatomical; therefore, satisfactory positioning of it relies on the original shape of the proximal tibia (Fig 4C). A 2.2-mm pin is inserted through the cut pin hole. Its position, determining the orientation of the cut, is computed for each patient individually to obtain the accurate hinge position. A fluoroscopic comparison is needed to confirm the good positioning of the guide.
-
•
Then, the hinge pin is inserted in the posterior distal pin hole. This pin confirms, with the aid of the fluoroscopy, the guide’s position and will avoid lateral hinge fracture during the procedure. A 4.0-mm drill bit is used through the 6 pin holes to achieve guide fixation. Adapted pins are inserted with a hammer (Fig 4).
-
•
Before proceeding to cut, the insertion depth of the saw has to be marked on the blade, using the computed measure to avoid posterior and lateral structure injuries. The saw blade is inserted on the guide’s window and the cut is made (Fig 4D).
-
•
The upper part of the guide is removed and the third part of the guide, including tibial tunnel for ACL reconstruction, is clipped (Fig 4H).
-
•
The tibial tunnel pin is inserted. To finalize the cut, proximal pins and the upper part of the guide had to be removed. When the saw blade gets in contact with the hinge pin, the required depth of cut is achieved (Fig 4F and G).
-
•
All pins and guides except the hinge pin and the tibial tunnel pin are removed. Progressive osteotomy wedges are passed through the cut line, opening the osteotomy and avoiding hinge fracture. The locking plate is applied using previous pin holes for well positioning and pins are reinserted. A bone wedge is fashioned out of a cryopreserved femoral head and is shaped to fit the osteotomy gap (Fig 5A).
-
•
The thickness of the femoral head is predetermined according to the preoperative planned correction (Fig 5B). The bone wedge is inserted in the opening osteotomy and impacted with a tamp (Fig 5C and D).
-
•
Then, the pins are then removed one by one and locking screws with predefined lengths are inserted. The most posterior proximal pin is left in place because of its close position with the tibial tunnel.
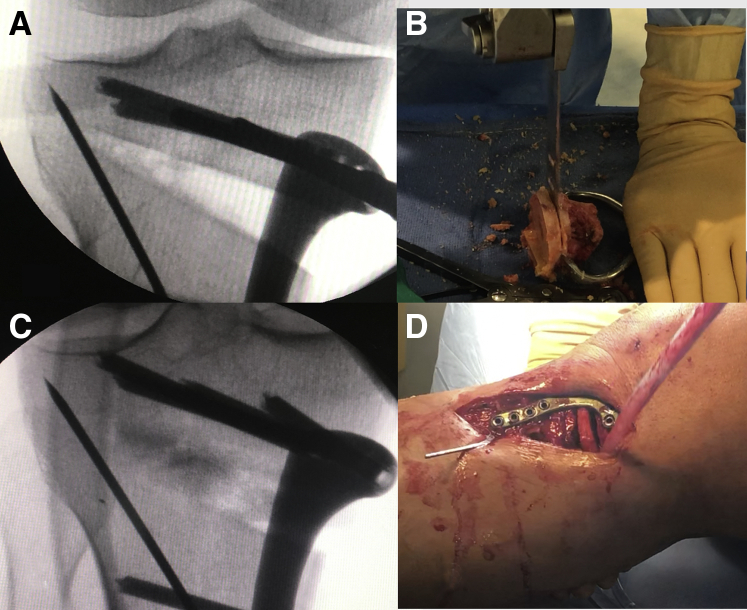
Fig 4.
The patient-specific osteotomy guide osteotomy procedure. Patient is lying supine, surgery is performed on the left lower-limb. Parts A, B, C, E, F, G, and H exhibit the medial aspect of the tibia. Part D is a 3D CT reconstruction; the view is inside of the osteotomy site, with a posterior standpoint. (A) A 6- to 8-cm slightly oblique vertical incision is made along the anteromedial surface, running over the joint space down to under the tibial tuberosity. (A′) Orientation of the picture: VM: vastus medialis; P: patella; ATT: anterior tibial tuberosity. (B) A scalpel is used to make a single-plane incision through the periosteum, then the hamstring and the medial collateral ligament are retracted posteriorly with a Cobb elevator until the medial surface of the tibia could be fully visible. (C) The 2 parts of patient-specific cutting guide are clipped together and then applied to the bone. No osteophyte has to be resected because the guide is anatomical; thus, well positioning of it depends on the original shape of the proximal tibia. A 4.0-mm drill bit is used through the 6 pin holes to achieve guide fixation. Adapted pins are inserted with a hammer. (D) Before proceeding the cut, the insertion depth of the saw has to be marked on the blade, using the computed measure to avoid posterior and lateral structure injuries. (E) The saw blade is inserted on the guide’s window and the cut is made. (H) Then, the upper part of the guide is removed and the third part of the guide, including tibial tunnel for ACL reconstruction is clipped. A tibial tunnel pin is inserted. To finalize the cut, proximal pins and the upper part of the guide had to be removed. (F/G) When the saw blade gets in contact with the hinge pin, cut is achieved under fluoroscopic control.
Fig 5.
Femoral head allograft insertion inside of the osteotomy site and plate fixation. Parts A and C depict intraoperative AP fluroscopic images of a right knee. (A) Once the osteotomy is opened and stabilized, (B) the femoral head is sculpted: a correct thickness has to be harvested according to the preoperative planned correction. (C) The bone wedge is inserted in the opening osteotomy and impacted with a tamp. (D) Intraoperative picture, the patient is lying supine, surgery of a right lower-limb, visualization of the medial aspect of the proximal tibia. The most posterior proximal pin is left in place because of its close position with the tibial tunnel.
ACL Reconstruction
-
•
We start with the standard anterolateral and anteromedial arthroscopic portals. The tibial tunnel pin is located, then the tunnel is drilled at the suitable diameter (Fig 6A).
-
•
The placement of the femoral tunnel is determined with ACL femoral origin and the previous tunnel placement. An outside-to-in guide is used to insert a femoral tunnel pin, then the tunnel is drilled. The graft is then pulled through the tibial tunnel until it reaches the proximal end of the femoral tunnel (Fig 6B).
-
•
The graft is fixed using 2 bioabsorbable screws. An arthroscopic view of the tibial tunnel allows to see the bone graft crushed by the tibial screw to ensure a solid fixation (Fig 6C).
-
•
Finally, the last locking and more anterior screw of the plate is inserted (Fig 6D).
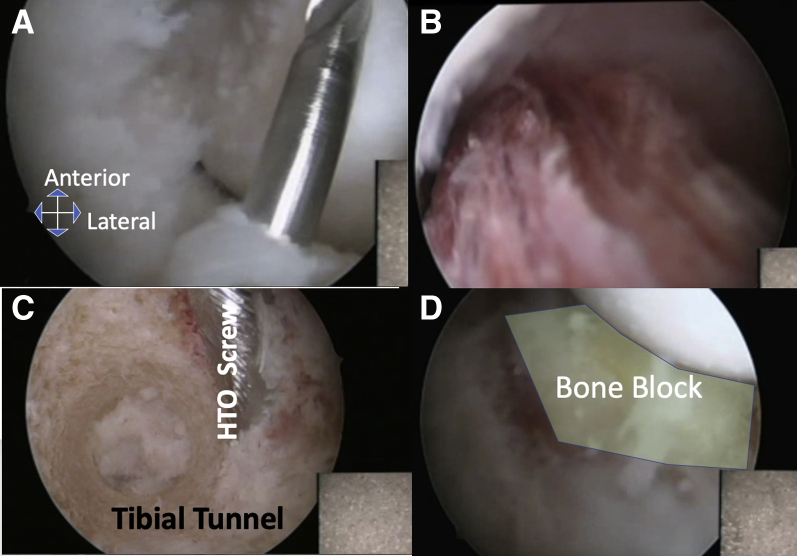
Fig 6.
Anterior cruciate ligament reconstruction. (A) We start with the standard anterior lateral and anterior medial arthroscopic portals. the tibial tunnel pin is located, then the tunnel is drilled at the suitable diameter. (B) After inside-out anteromedial femoral tunnel drilling, the graft is then pulled through the tibial tunnel until the proximal end of the femoral tunnel (Fig 5B). (C) The last locking and more anterior screw of the plate is inserted after graft fixation as this screw might interfere with the tibial tunnel. (D) The graft is fixed using 2 bioabsorbable screws. An arthroscopic view of the tibial tunnel allows one to see the bone graft crushed by the tibial screw, which ensures a solid fixation.
Postoperative Regiment
Full-body weight bearing is allowed as tolerated, with full range of motion except where there is associated cartilage or meniscus repair. Anticoagulation is needed for 1 week.
Postoperative recovery follows a classic ACL sequence: running at 3 months, pivot training at 6 months, and competition at 9 months. Pearls and pitfalls of this procedure are listed in Table 1.
Table 1.
Pearls and Pitfalls
Contraindications
|
Pearls
|
Advantages
|
Potential risks and disadvantages
|
ACL, anterior cruciate ligament; PSCG, patient-specific cutting guide; TT, tibial tuberosity.
Discussion
An increased posterior tibial slope is associated with an increased risk for early ACL graft failure, regardless of graft type.1 For this reason, it is especially important to address the tibial slope during ACL revision surgery. For many authors, the correction target is a posterior tibial slope between 3° and 5°.3 In our procedure, we set the correction target at 7° of posterior slope.
Kiapour et al. show that increased coronal tibial slope is associated with inferior clinical outcomes after ACL reconstruction. Correction of varus deformity is an important factor for the success of the procedure.8,9 Combinate varus high tibial osteotomy and ACL-reconstruction procedures show significant improvement in postoperative functional outcomes and low rates of complications, re-ruptures or revision surgery.10,11 The target is a slight overcorrected alignment with 1° to 3° of valgus.
The 3 more-common complications in these procedures are painful lack of range of motion, deep-vein thrombosis, and need for hardware removal.10 Smaller numbers of peroneal nerve or vascular injuries have been reported.11
In our procedure, using a 3-dimensional/CT PSCG, precision of the correction is increased.3 Indeed, managing 2 different plans of correction by combining coronal and sagittal correction one could normally assume a larger margin of error. This 3-dimensional correction procedure with cutting guide allows to overcome this limit. Moreover, planned procedure permits a better understanding, using 3-dimensional computed visualization during surgery.5,6
The predetermined positioning of the plate, size of screws, and the tibial tunnel avoid conflicts between fixation of the graft and screw of the plate. In addition, the predetermined size of osteosynthesis screws allow for both comfort and safety, validating the correct positioning of the plate.5,6
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.W. and M.O. report personal fees from Arthrex, NEWCLIP TECHNICS, and Stryker, outside the submitted work. K.K. reports personal fees from NEWCLIP TECHNICS and Stryker, outside the submitted work. S.P. reports personal fees from NEWCLIP TECHNICS and Zimmer Biomet, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
PSCG for HTO and ACL-R. We performed this combined surgery for a 34 years old male, suffering from his 3rd ACL reconstruction failure. He also underwent a complete medial meniscectomy with early degenerative changes on his medial femoro-tibial joint. The preoperative x-ray examination exhibited a Varus malalignment which we intend to correct. A Miniaci planning and 3D virtual osteotomy confirmed a 7degre medial opening correction. The lateral view x-ray exhibited a medial plateau tibial slope of 12d that we intend to correct by a posterior opening of 6d. The first part of this surgery is the quadricipital tendon graft harvesting. Osteotomy with cutting guide is the second step of this procedure using a patient specific cutting guide allowing both HTO and ACL-R tibial Tunnel drilling. The third part of this procedure is started with the standard anterior lateral and anterior medial arthroscopic portals. The tibial tunnel pin (inserted through the PSCG) is located, then the tunnel is drilled at the suitable diameter, then a regular ACL-R procedure is performed.
References
- 1.Christensen J.J., Krych A.J., Engasser W.M., Vanhees M.K., Collins M.S., Dahm D.L. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:2510–2514. doi: 10.1177/0363546515597664. [DOI] [PubMed] [Google Scholar]
- 2.Hees T., Petersen W. Anterior closing-wedge osteotomy for posterior slope correction. Arthrosc Tech. 2018;7:e1079–e1087. doi: 10.1016/j.eats.2018.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dejour D., Saffarini M., Demey G., Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23:2846–2852. doi: 10.1007/s00167-015-3758-6. [DOI] [PubMed] [Google Scholar]
- 4.Amendola A., Bonasia D.E. Results of high tibial osteotomy: Review of the literature. Int Orthop. 2010;34:155–160. doi: 10.1007/s00264-009-0889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pérez-Mañanes R., Burró J.A., Manaute J.R., Rodriguez F.C., Martín J.V. 3D surgical printing cutting guides for open-wedge high tibial osteotomy: Do it yourself. J Knee Surg. 2016;29:690–695. doi: 10.1055/s-0036-1572412. [DOI] [PubMed] [Google Scholar]
- 6.Shi J., Lv W., Wang Y. Three dimensional patient-specific printed cutting guides for closing-wedge distal femoral osteotomy. Int Orthop. 2019;43:619–624. doi: 10.1007/s00264-018-4043-3. [DOI] [PubMed] [Google Scholar]
- 7.Elson D.W., Petheram T.G., Dawson M.J. High reliability in digital planning of medial opening wedge high tibial osteotomy, using Miniaci's method. Knee Surg Sports Traumatol Arthrosc. 2015;23:2041–2048. doi: 10.1007/s00167-014-2920-x. [DOI] [PubMed] [Google Scholar]
- 8.Mehl J., Paul J., Feucht M.J. ACL deficiency and varus osteoarthritis: High tibial osteotomy alone or combined with ACL reconstruction? Arch Orthop Trauma Surg. 2017;137:233–240. doi: 10.1007/s00402-016-2604-8. [DOI] [PubMed] [Google Scholar]
- 9.Kiapour A.M., Yang D.S., Badger G.J. Anatomic features of the tibial plateau predict outcomes of ACL reconstruction within 7 years after surgery. Am J Sports Med. 2019;47:303–311. doi: 10.1177/0363546518823556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stride D., Wang J., Horner N.S., Alolabi B., Khanna V., Khan M. Indications and outcomes of simultaneous high tibial osteotomy and ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:1320–1331. doi: 10.1007/s00167-019-05379-5. [DOI] [PubMed] [Google Scholar]
- 11.Gupta A., Tejpal T., Shanmugaraj A. Surgical techniques, outcomes, indications, and complications of simultaneous high tibial osteotomy and anterior cruciate ligament revision surgery: A systematic review. HSS J. 2019;15:176–184. doi: 10.1007/s11420-018-9630-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PSCG for HTO and ACL-R. We performed this combined surgery for a 34 years old male, suffering from his 3rd ACL reconstruction failure. He also underwent a complete medial meniscectomy with early degenerative changes on his medial femoro-tibial joint. The preoperative x-ray examination exhibited a Varus malalignment which we intend to correct. A Miniaci planning and 3D virtual osteotomy confirmed a 7degre medial opening correction. The lateral view x-ray exhibited a medial plateau tibial slope of 12d that we intend to correct by a posterior opening of 6d. The first part of this surgery is the quadricipital tendon graft harvesting. Osteotomy with cutting guide is the second step of this procedure using a patient specific cutting guide allowing both HTO and ACL-R tibial Tunnel drilling. The third part of this procedure is started with the standard anterior lateral and anterior medial arthroscopic portals. The tibial tunnel pin (inserted through the PSCG) is located, then the tunnel is drilled at the suitable diameter, then a regular ACL-R procedure is performed.