Abstract
To investigate the correlation between environmental-meteorological factors and daily visits for acute otitis media (AOM) in Lanzhou, China.
Methods
Data were collected in 2014–2016 by the Departments of Otolaryngology-Head and Neck Surgery at two hospitals in Lanzhou. Relevant information, including age, sex and visiting time, was collected. Environmental data included air quality index, PM10, PM2.5, O3, CO, NO2 and SO2, and meteorological data included daily average temperature (T, °C), daily mean atmospheric pressure (AP, hPa), daily average relative humidity (RH, %) and daily mean wind speed (W, m/s). The SPSS22.0 software was used to generate Spearman correlation coefficients in descriptive statistical analysis, and the R3.5.0 software was used to calculate relative risk (RR) and to obtain exposure-response curves. The relationship between meteorological-environmental parameters and daily AOM visits was summarized.
Results
Correlations were identified between daily AOM visits and CO, O3, SO2, CO, NO2, PM2.5 and PM10 levels. NO2, SO2, CO, AP, RH and T levels significantly correlated with daily AOM visits with a lag exposure-response pattern. The effects of CO, NO2, SO2 and AP on daily AOM visits were significantly stronger compared to other factors (P < 0.01). O3, W, T and RH were negatively correlated with daily AOM visits. The highest RR lagged by 3–4 days.
Conclusions
The number of daily AOM visits appeared to be correlated with short-term exposure to mixed air pollutants and meteorological factors from 2014 through 2016 in Lanzhou.
Keywords: Acute otitis media, Air pollution and meteolofical factors, Non-parametric generalized additive model, Relative risk, Exposure-response curve
1. Introduction
Acute otitis media (AOM) is one of the most common diseases in otolaryngology practice and includes acute non-suppurate otitis media and acute suppurative otitis media. Pathogens such as bacteria and/or viruses can enter the tympanum through the Eustachian tube and cause infection of the mucosa in the middle ear cavity. AOM is often secondary to common cold within 48 h, but no more than 12 weeks (Bluestone et al., 2002). In the early stages of non-suppurate acute otitis media, the tympanic membrane can show slight congestion, invagination and light cone deformation (Xu et al., 2015). Effusion in the tympanic cavity can lead to tarnished appearance of the tympanic membrane, sometimes with arc-shaped fluid levels (Bluestone et al., 2002). Suppurative acute otitis media can be accompanied by high fever, nausea, vomiting and other systemic symptoms in addition to local persistent severe otodynia, which can be relieved upon the emergence of ear pus. Some patients also have symptoms of hearing loss. In suppurative acute otitis media, congested area of the tympanic membrane expands, with the tympanic membrane bulging and sometimes showing perforation and pus overflowing (Hayden and Schwartz, 1985).
The extensive use of antibiotics has been a public health problem in China (Yao and Yang, 2008). AOM is a main reason for prescribing antibiotics and increased healthcare cost in otolaryngology practice. AOM has a broad disease burden, requires prolonged treatment (Marchisio et al., 2014) and increases healthcare cost. Appropriate empiric antibiotic therapy for AOM requires reliable epidemiological data on the etiology and burden of AOM.
Cohort studies, case-control studies, case-crossover studies and cross-sectional studies have shown that exposure to air pollution can increase the incidence of OM (Bowatte et al., 2018). Similar findings have been reported in China indicating a positive correlation between environmental-meteorological factors and OM (Lu et al., 2017; Zhang et al., 2017). However, few Chinese studies have dealt with the correlation between meteorological conditions, air pollution and OM, especially in northwest China. Epidemiological studies (MacIntyre et al., 2014; Brauer et al., 2011) have analyzed the correlation between meteorological conditions, environmental factors and incidence of OM, and studies (Tian et al., 2016) have shown that air pollutants are related to allergic rhinitis (AR) and chronic rhinitis. However, whether AOM, as one of the upper respiratory immune related diseases, is also affected by meteorological-environmental factors has not been studied. Therefore, this study focuses on the correlation between environmental factors and the incidence of AOM.
Given the divergent findings on the effects of ambient environment and meteorological factors on AOM, the aim of this study was to assess the impact and possible determinant factors of ambient environmental-meteorological variables on the incidence of AOM. While our results are local, understanding of the effects of environmental-meteorological factors on middle ear diseases may have significant implications on future policy changes and enforcement of existing laws in China.
2. Materials and methods
2.1. Field site selection
The city of Lanzhou is located in the northwest of China (36°03′N, 103°40′E). The local climate is relatively dry with four distinct seasons and wide ranges of diurnal temperatures. There are seasonal changes in local air pollution. The altitude of Lanzhou is 1,500–3,000 m with significant ambient pressure fluctuations. What’s more, Lanzhou, as an important industrial base and transportation hub in Northwest China, consumes large quantity of resources and energy, and emits significant amounts of air pollutants. In recent years, due to the effective implementation of comprehensive air pollution prevention measures, the local air quality situation has been improved. But with the increase of vehicle exhaust emissions, Lanzhou air pollution presents new characteristics. The unique local topography, climate, change of seasons and altitude characteristics limit air flow and diffusion of pollutants, aggravate the degree of air pollution, and extend the contact time between people and pollutants. These conditions make Lanzhou a potentially useful location for studying the effects of atmospheric changes and environmental pollution on human health.
2.2. Clinical data
Clinical data were collected by the Department of Otolaryngology head and Neck Surgery at the 940th Hospital of the Chinese PLA Joint Logistics Support Unit and the Second Affiliated Hospital of Lanzhou University, from January 1, 2014 to 31 December 2016. The two hospitals are located in the adjacent Chengguan and Qilihe districts, both in the central urban area of Lanzhou. By the end of 2016, Chengguan district had a population of 1.8 million and Qilihe district had a population of 561,000, accounting for 72.8% of the total population in Lanzhou. Both the 940th Hospital and the Second Affiliated Hospital of Lanzhou University are open to the general public, providing full-scale, comprehensive integrated health services and disease prevention. The study population comprised outpatients examined and diagnosed by experienced clinicians.
2.2.1. Examination and diagnosis of AOM
-
a.
Otoscopy: congestion of external auditory canal and tympanic membrane, middle ear effusion or purulent drainage upon tympanic membrane perforation.
-
b.
Audiological tests: (1) Acoustic immittance: no effusion in early stage of non-suppurate acute otitis media. C-type or B-type tympanograms showing negative pressure and/or fluid accumulation. (2) Otoacoustic emissions: Otoacoustic emissions present indicating no middle ear effusion, or absent with middle ear effusion. (3) Pure tone audiometry: for patients with a complaint of hearing loss and able to complete testing, conductive hearing loss ≥20 dB HL with air-bone gap. (4) Auditory brainstem responses (ABRs) and multi-frequency steady-state responses (ASSRs): for patients unable to complete behavioral testing, ABRs and ASSRs were used to detect both air and bone conduction thresholds.
-
c.
CT scan of temporal bone was acquired for patients suspected of intracranial or extracranial complications.
-
d.
Routine blood tests showing increased white blood cell counts, especially neutrophils, C-reactive protein (CRP, 10 mg/L) and blood sedimentation rate.
-
e.
Pathogen detection: For suppurative otitis media, purulent discharge was cultured.
AOM was diagnosed in accordance to the International Classification of Diseases, ninth version, Clinical Modification (ICD-9-CM) codes 3810, 3820, or 3829 (Chen et al., 2013). Data of AOM from both hospitals were pooled together for analysis. Cases were identified by searching the electronic medical record retrieval system using the key word “acute otitis media”. Cases were reviewed based on specific inclusion and exclusion criteria, resulting in 11,466 cases included in the study.
2.3. Air pollutants monitoring and meteorological data
Air quality was monitored during the period from January 1, 2014 to December 31, 2016 by a network of four monitoring stations, with two of which located in the Chengguan district. The monitoring included daily average levels (concentrations) of six main air pollutants, i.e. fine particles (PM2.5), inhalable particles (PM10), sulfur dioxide (SO2), nitrogen dioxide (NO2), ozone (O3) and carbon monoxide (CO), as well as the air quality index (AQI), which was a dimensionless quantitative index of air quality. Meteorological data of the corresponding time period were obtained from the Gansu Meteorological Bureau and included daily averages temperature (T, °C), pressure (AP, H Pa), relative humidity (RH,%) and wind speed (W, m/s). Among the parameters, calculation of AQI was based on the national standards regarding ambient air quality (GB3095) revised in 2012 and rated in six grades (0–50, 51–100, 101–150, 151–200, 201–300 and over 300). The pollutant indices used in the assessment included PM2.5, PM10, SO2, NO2, O3 and CO.
2.4. Statistical analysis
2.4.1. Relevance
The SPSS22.0 software was used to calculate Spearman correlation coefficients between two variables. The R3.5.0 software was used to run generalized additive models to generate the RR and single and cumulative lag exposure-response curves for each exposure factor. Correlation between meteorological-environment factors and the number of daily AOM visits, as well as the degree of correlation, were discussed to determine main pathogenic factors.
2.4.2. Lag effects
Meteorological environment factors have a lagging effect on daily AOM visits, including single and cumulative lagging. In this study, one-day lag effect referred to the influence on the number of one-day AOM visits on a given day, while cumulative lag effect referred to the influence of a certain factor’s moving average level on the number of one-day AOM visits. In order to determine the time of strong lag effect and obtain factors with strong effect, we analyzed the Spearman correlation coefficient of single and cumulative lag effects of different factors on the average number of daily AOM visits. The day with the highest correlation coefficient or the day with the largest increase of correlation coefficient compared with the previous day was selected as a strong lag effect time. Initially, correlation coefficients of single lag and cumulative lag within 20 days for the average number of daily AOM visits were calculated, which were not statistically significant (P > 0.05), leading us to later focus on correlation coefficients of single and cumulative lag effects within 6 days (L01-L06).
2.4.3. Generalized additive model and application of R software
Generalized additive model (GAM) is a non-parametric extension of traditional generalized linear model, which can effectively deal with the complex nonlinear relationship between explanatory variables and effect variables (Dong et al., 2008). GAM is mainly used to analyze the acute damage effect of air pollution or meteorological factors on human health events (such as morbidity, hospitalization and death). The R3.5.0 and SPSS 22.0 software were used to study the case and meteorological-environmental factors data. Among them, the number of AOM visits was a continuous variable, which obeyed the Poisson distribution (Peng et al., 2006).GAM with Poisson distribution was utilized in combination with the distributed linear and non-linear lag models (DLNM) (Gestro et al., 2017). When using GAM to study the correlation between meteorological environmental factors and the average number of AOM visits, it is necessary to control the holiday and weekend factors in the time series. In this study, the spline smoothing function was used to fit the nonlinear independent variables, including time, holiday and week dummy variables. When building the basic model, we used the step-by-step method combined with the Akaike’s information criterion (AIC) to select the independent variables, i.e. the smaller the AIC, the better the model fitting, so as to select the best combination of independent variables to get the best basic model. After establishing of the basic model, the meteorological environment factors were introduced, the linear model of air pollutants fitted, and the single and cumulative lag effect analyzed, respectively. That is to say, the average mass concentration (L0-L6) and the moving average value (L01-L06) of the studied meteorological environment factors were introduced into the model one by one to establish the exposure response relationship. According to the model, the exposure response curve was estimated to calculate the RR and 95% confidence interval (95% CI) of AOM visits in relation to pollutant concentrations changes or the meteorological factors fluctuations.
2.5. Ethics
The Ethics Review Board of the 940th Hospital and Second Affiliated Hospital of Lanzhou University, Ministry of Public Health, and the Ethics Review Board of the Institute of Geographic Sciences and Natural Resources Research approved the investigation and ensured that the safety, health and rights of patients involved were protected.
2.6. Quality control
-
a.
We did not include follow up visits in this study.
-
b.
We excluded AOM patients who had an associated diagnosis, non-specific otoscopic findings, barotrauma, or other traumatic factors described in their medical histories.
-
c.
We excluded visits during holidays as the healthcare situation on holidays was different from that on normal business days.
3. Results
3.1. Gender
Of the 11,466 patients, 6,005 (52.4%) were male and 5,461 (47.6%) were female. On average, there were more monthly male AOM visits than female AOM visits (P < 0.05), suggesting higher AOM risks for men than for women.
3.2. Age
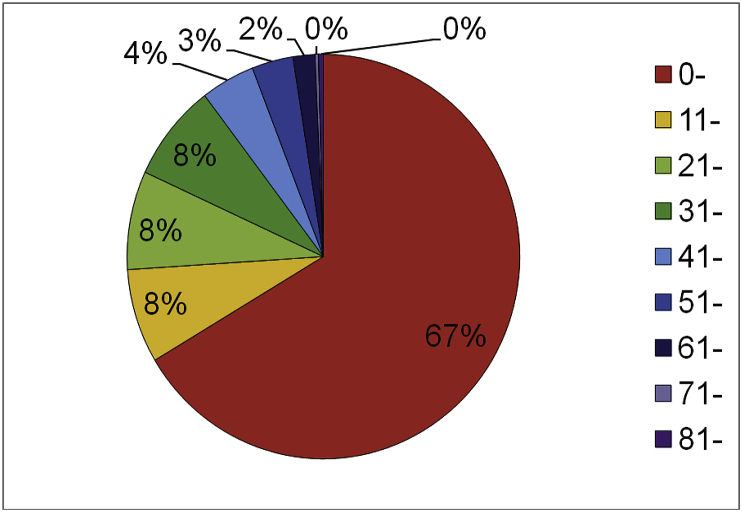
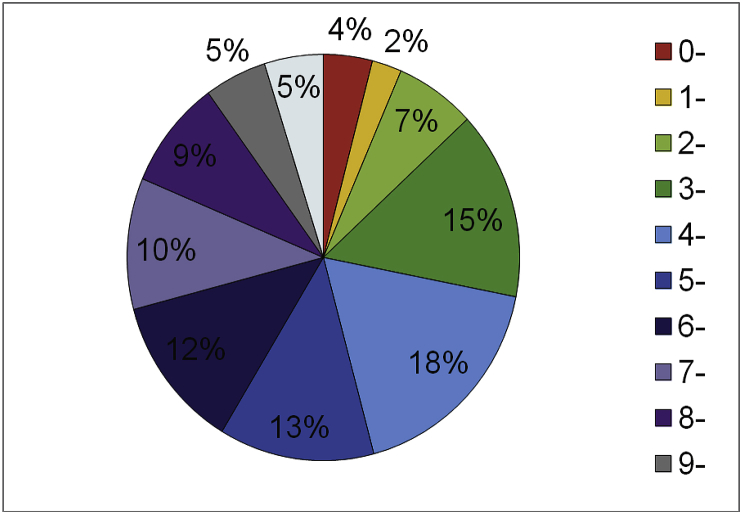
As shown in Fig. 1, young children (<10 years) were particularly vulnerable to AOM, showing the highest AOM incidence (accounting for 67% of total visits). For patients aged <10 years, children aged 3–5 years had the highest AOM incidence that peaked at the age of 4, with those under the age of 1 demonstrating the lowest incidence. AOM visits between ages 1–3 years increased rapidly, followed by a gradual decrease from 5 to 10 years, as shown in Fig. 2.
Fig. 1.
Age distribution of AOM in Lanzhou from 2014 through 2016.
Fig. 2.
Age distribution of AOM under 10 years old in Lanzhou from 2014 through 2016.
3.3. Season
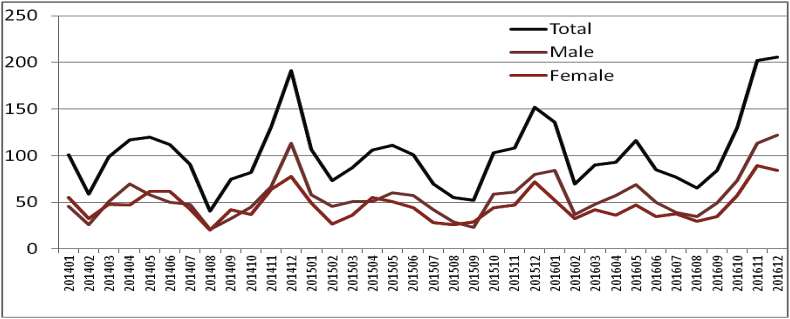
As shown in Fig. 3, AOM occurrence showed two peaks each year during the 2014–2016 period, the first in May and the second in December, with the peak value in May lower than that in December. Daily AOM visits peaks appeared in early summer and early winter, while the lowest daily AOM visit numbers were associated with the hottest (August) and coldest temperatures (February).
Fig. 3.
Monthly AOM visits during 2014–2016 period in Lanzhou.
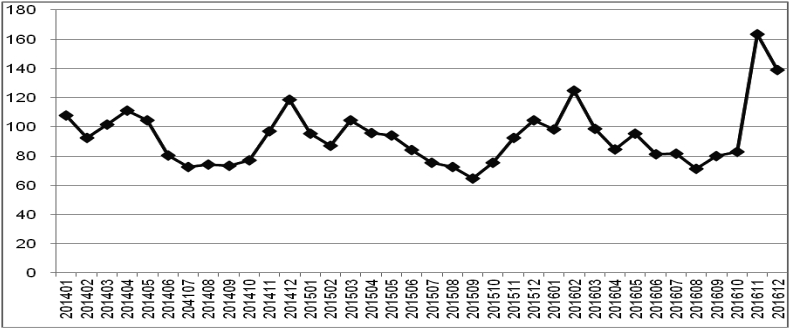
The monthly AQI change also showed two peaks in each year during the 2014–2016 period, the first from March to May and the second November to January. The peaks overlapped those of daily AOM visits, also with the first peak value lower than the second (Fig. 4).
Fig. 4.
Monthly average AQI of Lanzhou during 2014 through 2016.
3.4. Lag effects
Lag effects generally increased from L1 to L6 (L01 - L06). We detected little associations with L7/L07 (data not shown). The day with the highest increase in correlation coefficient was selected as the time of strongest lag effect.
Table 1 shows single lag effects of environmental meteorological factors on daily AOM visits. The days with strongest single lag effects are marked in red. From the table, it can be seen:
-
a.
The strongest lag effect occurred over 3–4 days.
-
b.
All environmental-meteorological factors were positively correlated with daily AOM visits, except O3 and W.
-
c.
Correlation with W did not pass significance test (P > 0.05), indicating that daily AOM visits were not affected by wind speed.
-
d.
The lag effects of environmental factors on daily AOM visits were stronger than atmospheric factors (P < 0.01).
Table 1.
Spearman analysis of single lag effects on daily AOM visits by air pollutes and meteorological factors.
| Factors | L1 | L2 | L3 | L4 | L5 | L6 |
|---|---|---|---|---|---|---|
| AQI | 0.154∗∗ | 0.170∗∗ | 0.204∗∗ | 0.238∗∗ | 0.221∗∗ | 0.233∗∗ |
| CO | 0.150∗∗ | 0.154∗∗ | 0.185∗∗ | 0.169∗∗ | 0.170∗∗ | 0.180∗∗ |
| NO2 | 0.150∗∗ | 0.167∗∗ | 0.244∗∗ | 0.204∗∗ | 0.218∗∗ | 0.236∗∗ |
| O3 | −0.061∗ | −0.066∗ | −0.071∗ | −0.067∗ | −0.062∗ | −0.067∗ |
| PM2.5 | 0.177∗∗ | 0.196∗∗ | 0.204∗∗ | 0.244∗∗ | 0.226∗∗ | 0.241∗∗ |
| PM10 | 0.163∗∗ | 0.179∗∗ | 0.236∗∗ | 0.217∗∗ | 0.224∗∗ | 0.232∗∗ |
| SO2 | 0.111∗∗ | 0.112∗∗ | 0.118∗∗ | 0.116∗∗ | 0.110∗∗ | 0.112∗∗ |
| W | −0.018 | −0.023 | −0.017 | −0.031 | −0.023 | −0.037 |
| AP | 0.088∗∗ | 0.095∗∗ | 0.119∗∗ | 0.108∗∗ | 0.098∗∗ | 0.114∗∗ |
| RH | −0.069∗ | −0.072∗ | −0.091∗ | −0.081∗∗ | −0.083∗∗ | −0.088∗∗ |
| T | −0.080∗∗ | −0.082∗∗ | −0.097∗∗ | −0.089∗∗ | −0.094∗∗ | −0.096∗∗ |
∗P < 0.05 ∗∗P < 0.01.
Table 2 shows cumulative lag effects of environmental-meteorological factors on daily AOM visits. The days with the strongest cumulative lag effects are marked in red.
-
a.
Similar to single lag effects, the stronger lag effects occurred over 3–4 days.
-
b.
All factors were positively correlated with daily AOM visits, except O3, W, T and RH.
-
c.
Again, correlation with W did not pass significance test (P > 0.05), indicating that daily AOM visits were not affected by wind speed.
-
d.
Lag effects of environmental factors (except O3) on daily AOM visits were stronger than atmospheric factors (P < 0.01).
-
e.
Cumulative lag effects were stronger than single lag effects (P < 0.01).
Table 2.
Spearman analysis of cumulative lag effects on AOM by air pollutes and meteorological factors.
| Factors | L01 | L02 | L03 | L04 | L05 | LO6 |
|---|---|---|---|---|---|---|
| AQI | 0.154∗∗ | 0.170∗∗ | 0.233∗∗ | 0.208∗∗ | 0.221∗∗ | 0.204∗∗ |
| CO | 0.140∗∗ | 0.154∗∗ | 0.180∗∗ | 0.169∗∗ | 0.170∗∗ | 0.155∗∗ |
| NO2 | 0.150∗∗ | 0.167∗∗ | 0.184∗∗ | 0.236∗∗ | 0.218∗∗ | 0.206∗∗ |
| O3 | −0.071∗ | −0.071∗ | −0.069∗ | −0.067∗ | −0.062∗ | −0.067∗ |
| PM2.5 | 0.177∗∗ | 0.196∗∗ | 0.244∗∗ | 0.224∗∗ | 0.226∗∗ | 0.221∗∗ |
| PM10 | 0.163∗∗ | 0.179∗∗ | 0.236∗∗ | 0.217∗∗ | 0.224∗∗ | 0.218∗∗ |
| SO2 | 0.111∗∗ | 0.112∗∗ | 0.113∗∗ | 0.116∗∗ | 0.110∗∗ | 0.112∗∗ |
| W | −0.060 | −0.058 | −0.074 | −0.089 | −0.114 | −0.124 |
| AP | 0.124∗∗ | 0.122∗∗ | 0.133∗∗ | 0.129∗∗ | 0.107∗∗ | 0.130∗∗ |
| RH | −0.045∗ | −0.043∗ | −0.056∗ | −0.050∗ | −0.052∗ | −0.055∗ |
| T | −0.239∗∗ | −0.241∗∗ | −0.247∗∗ | −0.241∗∗ | −0.239∗∗ | −0.241∗∗ |
∗P < 0.05 ∗∗P < 0.01.
3.5. Relative risk (RR)
RR is a risk ratio of exposure group to control group. In this study, daily AOM visits when pollutant concentration, wind speed, humidity and air pressure were zero were used as the control group. The GAM analysis showed that daily AOM visits in Lanzhou were directly correlated with daily air pollution and meteorological parameters levels. Table 3, Table 4 show the RR (95% confidence intervals, CI) of increase in daily AOM visits associated with 10 μg/m3 increase in air pollutant concentrations on different lagging days, for single-day measures and moving average measures. Lag effects beyond 6 days showed little associations and were therefore excluded from further analyses. The adjusted RR for a change in measured pollute concentrations were equal to the interquartile range of pollution distribution.
Table 3.
RR for single lag effects on AOM visits.
| L1 | L2 | L3 | L4 | L5 | L6 | |
|---|---|---|---|---|---|---|
| AQI | 1.002 | 1.002 | 1.003 | 1.002 | 1.002 | 1.002 |
| PM2.5 | 1.005 | 1.006 | 1.007 | 1.006 | 1.006 | 1.006 |
| PM10 | 1.001 | 1.001 | 1.002 | 1.001 | 1.001 | 1.001 |
| NO2 | 1.007∗ | 1.008∗ | 1.009∗ | 1.009∗ | 1.007∗ | 1.009∗ |
| SO2 | 1.009∗∗ | 1.008∗ | 1.010∗∗ | 1.010∗ | 1.009∗ | 1.008∗ |
| CO | 1.275∗ | 1.270∗ | 1.282∗ | 1.293∗ | 1.270∗ | 1.288∗ |
| O3 | 0.994 | 0.994∗ | 0.995∗∗ | 0.994 | 0.994 | 0.992 |
| RH | 0.999∗ | 1.000∗∗ | 0.982∗ | 0.982∗ | 0.981 | 0.981 |
| T | 0.981 | 0.982 | 0.995∗ | 0.995 | 0.993 | 0.993 |
| W | 0.998 | 0.998 | 1.000 | 0.999 | 0.999 | 0.999 |
| AP | 1.019∗ | 1.016∗ | 1.015∗ | 1.017∗∗ | 1.022 | 1.022 |
Significance codes:∗∗∗P = 0,∗∗P < 0.001,∗P < 0.01.
Table 4.
RR for cumulative lag effects on AOM visits.
| L01 | L02 | L03 | L04 | L05 | L06 | |
|---|---|---|---|---|---|---|
| AQI | 1.002 | 1.003 | 1.007 | 1.005 | 1.005 | 1.006 |
| PM2.5 | 1.007 | 1.009 | 1.014 | 1.011 | 1.012 | 1.013 |
| PM10 | 1.001 | 1.002 | 1.002 | 1.004 | 1.003 | 1.003 |
| NO2 | 1.009∗ | 1.010∗ | 1.016∗ | 1.013∗ | 1.014∗ | 1.015∗ |
| SO2 | 1.010∗ | 1.011∗∗ | 1.015∗ | 1.012∗∗ | 1.012∗ | 1.012∗ |
| CO | 1.297∗∗ | 1.333∗ | 1.433∗ | 1.387∗ | 1.270∗ | 1.422∗ |
| O3 | 0.993 | 0.993∗∗ | 0.993∗ | 0.992 | 0.993∗ | 0.992 |
| RH | 0.999∗ | 0.999∗ | 0.999∗ | 0.999∗ | 0.999∗ | 0.999∗ |
| T | 0.981∗ | 0.981∗ | 0.981∗ | 0.981∗ | 0.981∗ | 0.981∗ |
| W | 0.987 | 0.985 | 0.844 | 0.976 | 0.756 | 0.969 |
| AP | 1.031∗ | 1.035∗∗ | 1.030∗ | 1.040∗∗ | 1.032∗ | 1.044∗ |
Significance codes:∗∗∗P = 0,∗∗P < 0.001,∗P < 0.01.
From Table 3, it can be seen:
-
a.
RR associated with NO2 SO2 CO and AP increase were greater than with other factors.
The greatest RR associated with NO2 increase occurred on L3 (1.008667, 95% CI: 1.007–1.010338).
The greatest RR associated with SO2 increase occurred on L3 (1.010153, 95% CI: 1.007815–1.012496).
The greatest RR associated with CO increase occurred on L4 (1.292766, 95% CI: 1.236996–1.351051).
The greatest RR associated with AP increase occurred on L1 (1.018827, 95% CI: 1.011253–1.018827).
-
b.
Increase of several air pollutants, e.g. AQI, O3, PM2.5 and PM10, showed no significant RR in contrast to other pollutants.
-
c.
The greatest RR associated with increase of most studied environmental-meteorological factors were on L3 and L4.
From Table 4, it can be seen:
-
a.
RR associated with NO2, SO2, CO and AP increase were more significant than with other factors studied.
The greatest RR associated with NO2 increase occurred on L3 (1.015902, 95% CI: 1.01442–1.017384).
The greatest RR associated with SO2 increase occurred on L3 (1.0154055, 95% CI: 1.014315–1.016496).
The greatest RR associated with CO increase occurred on L3 (1.433, 95% CI: 1.341313–1.525541).
The greatest RR associated with AP increase occurred on L06 (1.044456, 95% CI: 1.033799–1.055223).
-
b.
Increase of several air pollutants, e.g. AQI, O3, PM2.5 and PM10, showed no significant RR in contrast to other pollutants.
-
c.
No significant RR was associated with increase of W (P > 0.05).
-
d.
The greatest RR associated with increase of most studied environmental-meteorological factors were again on L3 and L4.
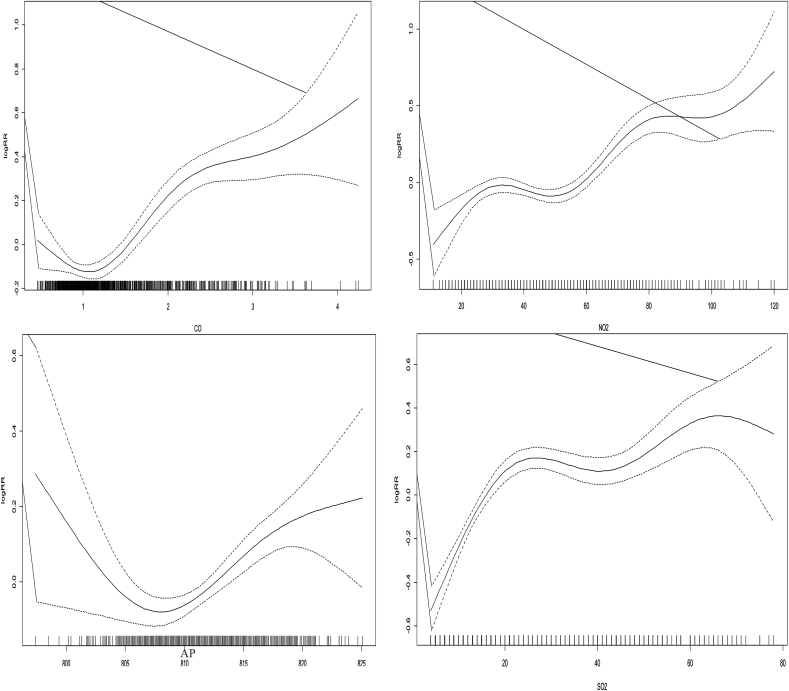
3.6. Exposure-response relationship
Exposure-response curves at different lag times were generated for various factors studied. Several factors clearly showed impacts on AOM incidence with a relatively clear risk concentration threshold, as shown in Fig. 5 (solid line = log RR for AOM visits, and dashed lines = 95% CI).
-
a.
The curve of NO2 showed a “wavy rise”, with no clear safe or dangerous threshold. Daily AOM visits increased with the increasing concentration of NO2, although the rate of increase varied at different concentrations.
-
b.
The exposure response curve of CO suggested a safety threshold. When CO concentration was <1 mg/m3, the RR of AOM visits was in a relatively safe range. However, when CO concentration reached 1 mg/m3, RR was increased with no maximal threshold identified.
-
c.
The curve of SO2 was “M” shaped with two peak threshold ranges, with the first peak RR at SO2 concentration >20 μg/m3 and <40 μg/m3 and the second peak RR at SO2 concentration >60 μg/m3 and <80 μg/m3.
-
d.
RR was the lowest when AP was near 810 hPa. RR increased with AP in the 815–820 range, followed by a decrease thereafter.
-
e.
The threshold concentrations for other factors were not identified, and the shapes of the exposure-response curves need to be further defined.
Fig. 5.
Exposure-response curves of single lag effects.
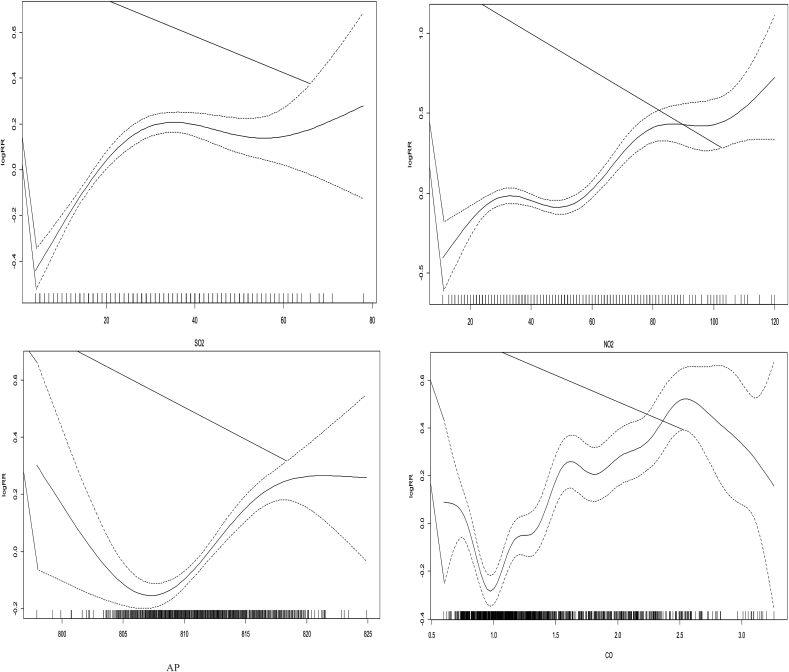
Fig. 6 shows exposure-response curves of several factors with cumulative lag effects on average daily AOM visits.
-
a.
The curve of NO2 was “M” shaped with the first peak RR at NO2 concentration of 30 μg/m3 and the second peak RR at NO2 concentration of 80 μg/m3. RR was the lowest at NO2 concentration of 50 μg/m3.
-
b.
The curve of SO2 was “S” shaped with one high risk threshold concentration. The strongest association with daily AOM visits appeared for SO2 levels between 20 and 40 μg/m3.
-
c.
Similar to CO single lag effect curve, CO cumulative lag effect curve also showed a safe threshold concentration, although the remaining part of the curve was not as smooth and showed increased volatility.
-
d.
Similar to its single lag effect curve, RR was the lowest when AP was in the 805–810 hPa range and showed an increase in the 815–820 range, followed by a decrease.
Fig. 6.
Exposure-response curves of cumulative lag effects.
4. Discussion
4.1. Age
We found that incidence of AOM was higher among preschool children, with a peak between 3 and 6 years of age. One reason for this finding may be the unique middle ear anatomy in young children (including a short, flat and straight Eustachian tube), as compared with that in adults, which is conducive to the flow of polluted air to the middle ear (Csákányi et al., 2012). Deng (Deng et al., 2017) believes that the mother’s exposure to air pollutants before childbirth from outdoor activities and to indoor air pollutants from indoor decoration after childbirth are independent related factors for early onset of AOM in infants. Increased contact between infants and the environment, gradual disappearance of immunity obtained from the mother and relatively enclosed surroundings may increase the risk of cross infection among infants. In addition, young children lack the ability of adequate verbal communication, which affect accurate expression of symptoms including hearing loss, tinnitus, and earaches.
4.2. Gender
From this study, male gender appeared to be more associated with AOM visits than female. Although the exact explanation for this difference may need to be further studied in a larger-scale epidemiological study, one possible explanation for this finding may be the gender ratio of babies born in China, i.e. 116.9:100 at birth, with 30–40 million more male newborns than female.
4.3. Season
We found that AOM visits showed a clear seasonal pattern in Lanzhou, with the highest in December and the lowest in August, consistent with findings in one of our previous studies on otitis media with effusion (OME) which was also more prevalent in winter than in summer. In winter, affected by cold temperatures and dry weather, upper respiratory tract resistance is weakened and vulnerable to invasion by pathogens, including viruses. The mucous membrane of the respiratory tract, specifically the Eustachian tube and nasal passages, loses its moisture more easily in dry winter weather, further decreases its defense against infection. In addition, influenza is mainly transmitted by air droplets. Increased people in indoor spaces create favorable conditions for viruses to spread. Therefore, cold weather in winter and upper respiratory tract infection are risk factors for AOM. Moreover, air quality in winter and early spring tends to be worse because of harsh climatic conditions and increased coal burning for heating, in addition to more frequent dust storms in the Lanzhou area. Oddly, February was the month of the year in which the number of AOM visits was low, seemingly contrary to the trend of increasing AOM visits in winter. We believe that this is because February is usually the Chinese Lunar New Year and winter vacation for students, when people may defer hospital visits until after holiday celebrations and vacations. Meteorological conditions during June to August are favorable for effectively dispersing polluted air from the local valley basin, resulting in better air quality.
4.4. Environmental-meteorological factors
Air pollution is an important risk factor for AOM. Lanzhou is an industrial manufacturing hub in Northwest China and located in a valley basin. Lanzhou’s geographic features and scale of human activities contribute to its unique climatic environment. The winter air in Lanzhou is mainly polluted by coal burning and petroleum combustion, including vehicle exhaust emissions. Lanzhou faces serious air pollution with high air concentrations of PM2.5, PM10, NO2, SO2, O3 and CO. Our study demonstrated significant associations between ambient air pollutant levels and daily AOM visits. Such associations became the strongest during November to January, as evidenced by the annual peaks in AOM visits in winter, although the RR differed among individual pollutants. Such differences likely reflect the fact that some pollutants exert stronger effects than others or that different threshold levels are required to cause adverse effects. Several reports described the adverse health effects of O3, NO2 and SO2 levels on AOM visits during the winter period (Shang et al., 2013).
Table 1, Table 2 show that seven of the air pollution indicators we studied had were correlated to daily AOM visits. Except for O3, which had a negative correlation with daily AOM visits, all other factors showed a positive correlation with daily AOM visits at different levels. Air pollutants can damage the epithelial barrier of nasal mucosa and increase the opportunity and time of exposure of upper respiratory mucosa to pollutants, leading to increased risk of AOM. Although the volume of air pollutants may be small, it can easily combine with H2O on the mucous membrane to produce various products, enhancing the permeability of respiratory tract epithelium and increasing the vulnerability and chance of contact between epithelial cells and allergens (Vawda et al., 2014). Pollutants adhering to cell surface can cause disordered cell arrangement and damaged ciliated structures, which reduce mobility of epithelial cells and induce synthesis and release of inflammatory cytokines, causing apoptosis through oxidative stress and damaging the barrier function of mucosal epithelial cells (Hong et al., 2008). Increased incidence of allergic rhinitis can in turn affect the incidence of AOM. AOM is a common acute inflammatory disease of middle ear mucosa, often secondary to acute upper respiratory tract infection. Air pollutants can increase the incidence of upper respiratory infection and respiratory tract infectious diseases (Kubesch et al., 2014; Peel et al., 2005; Darrow et al., 2014), which is in turn bound to increase the incidence of AOM.
In this study, AOM was negatively correlated with T and RH. While dry and cold air can lead to dryness of nasal and nasopharyngeal mucous membrane and decreased surface ciliary activity, the mucous membrane becomes moist during the rainy season, thus reducing the spread of pathogens. Common pathogens causing AOM include streptococcus pneumoniae, haemophilus influenzae amorphous, moraxella catarrhalis, respiratory syncytial virus, rhinovirus, etc. Numminen (Numminen et al., 2015) found that dry and cold weather is more conducive to the spread of bacteria, resulting in increased incidence of AOM when T and RH are low. Kim (Kim et al., 1996) found a significant correlation between streptococcus pneumoniae infection and T < 24 °C. The incidence of respiratory syncytial virus infection in winter is also higher than that in other seasons.
We also found that incidence of AOM was positively correlated with AP, but not with W. No reasonable explanation for this is available from the current study and further study is needed, although one possible explanation may be that the inversion layer is thick with low W (wind speed), which slows down the exchange of polluted air with clean air from outside the local valley basin, further aggravating the seasonal air pollution. The influence of meteorological factors on the incidence of AOM is a topic that needs further study.
5. Conclusion
In this study we established positive correlations between the levels of air PM2.5, PM10, SO2, CO and NO2 and the number of daily AOM visits, which was enhanced by exposure to air pollutants for 3–4 days. Our results suggest that exposure to ambient air pollutants and meteorological factors increased AOM visits in Lanzhou. In addition, we found that age was a risk factor for AOM. These findings highlight the urgency to improve air quality and can serve as a basis to advise vulnerable populations to reduce outdoor activities when poor air quality is forecasted.
-
a.
Air pollution is serious in winter. Travel should be reduced when possible with relevant protective measures taken.
-
b.
Children are more likely to be affected by atmospheric environmental factors and need additional care.
-
c.
Attention should be paid to changes of atmospheric environmental factors when planning travel.
-
d.
People with a history of relevant diseases should take preventive measures in advance.
-
e.
Adequate healthcare resources should be deployed in dealing with increased clinic work load when facing worsening air pollution conditions.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
References
- Bluestone C.D., Gates G.A., Klein J.O. Definitions, terminology, and classification of otitis media. Ann. Otol. Rhinol. Laryngol. Suppl. 2002;188(3):8. doi: 10.1177/00034894021110s304. [DOI] [PubMed] [Google Scholar]
- Bowatte G., Tham R., Perret J.L. Air pollution and otitis media in children: a systematic review of literature. Int. J. Environ. Res. Publ. Health. 2018;15(2):257–269. doi: 10.3390/ijerph15020257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brauer M., Karr C., MacIntyre E. Woodsmoke and children’s health: findings from the border air quality study. Epidemiology. 2011;22 [Google Scholar]
- Chen Y.J., Hsieh Y.C., Huang Y.C., Chiu C.H. Clinical manifestations and microbiology of acute otitis media with spontaneous otorrhea in children. J. Microbiol. Immunol. Infect. 2013 Oct;46(5):382–388. doi: 10.1016/j.jmii.2013.04.001. [DOI] [PubMed] [Google Scholar]
- Csákányi Z., Czinner A., Spangler J. Relationship of environmental tobacco smoke to otitis media (OM) in children. Int. J. Pediatr. Otorhinolaryngol. 2012;76(7):989–993. doi: 10.1016/j.ijporl.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darrow L.A., Klein M., Flanders W.D. Air pollution and acute respiratory infections among children 0-4 Years of age: an 18-year time-series study. Am. J. Epidemiol. 2014;180(10):968–977. doi: 10.1093/aje/kwu234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Q., Lu C., Jiang W. Association of outdoor air pollution and indoor renovation with early childhood ear infection in China. Chemosphere. 2017;169:288–296. doi: 10.1016/j.chemosphere.2016.11.079. [DOI] [PubMed] [Google Scholar]
- Dong Y., Zhao N.Q., Tang J.K. Application of generalized additive model in the study of health effects of temperature. Health Statistics. 2008;25(2):144–146. [Google Scholar]
- Gestro Massimo, Condemi Vincenzo, Bardi Luisella. Meteorological factors, air pollutants, and emergency department. Int. J. Biometeorol. 2017;61:1749–1764. doi: 10.1007/s00484-017-1356-7. [DOI] [PubMed] [Google Scholar]
- Hayden G.F., Schwartz R.H. Characteristics of earache among children with acute otitis media. Am. J. Dis. Child. 1985;139(7):721–723. doi: 10.1001/archpedi.1985.02140090083037. [DOI] [PubMed] [Google Scholar]
- Hong Z., Guo Z., Zhang R. Airborne fine particulate matter induces oxidative stress and inflammation in human nasal epithelial cells. J. Toxicol. Environ. Health. 2008;71:512–520. doi: 10.1620/tjem.239.117. [DOI] [PubMed] [Google Scholar]
- Kim P.E., Musher D.M., Glezen W.P. Association of invasive pneumococcal disease with season, atmospheric conditions.Air pollution, and the isolation of respiratory viruses. Clin. Infect. Dis. 1996;22(1):100–106. doi: 10.1093/clinids/22.1.100. [DOI] [PubMed] [Google Scholar]
- Kubesch N.J., de Nazelle A., Westerdahl D. Respiratory and inflammatory responses to short-term exposure to traffic-related air pollution with and without moderate physical activity. Occup. Environ. Med. 2014;72:284–293. doi: 10.1136/oemed-2014-102106. [DOI] [PubMed] [Google Scholar]
- Lu Y.X., Liang J.Q., Gu Q.L. A study on the characteristics of children’s acute otitis media in Beijing and its correlation with meteorological factors. J. Otorhinolaryngol. Head Neck Surg. 2017;52(10):724–728. doi: 10.3760/cma.j.issn.1673-0860.2017.10.002. [DOI] [PubMed] [Google Scholar]
- MacIntyre E.A., Gehring U., Molter A. Air pollution and respiratory infections during early childhood: an analysis of 10 European birth cohorts within the ESCAPE project. Environ. Health Perspect. 2014;122:107–113. doi: 10.1289/ehp.1306755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchisio P., Nazzari E., Torretta S., Esposito S., Principi N. Medical prevention of recurrent acute otitis media: an updated overview. Expert Rev. Anti Infect. Ther. 2014;12(5):611–620. doi: 10.1586/14787210.2014.899902. [DOI] [PubMed] [Google Scholar]
- Numminen E., Chewapreecha C., Turner C. Climate induces seasonality pneumococcal transmission. Sci. Rep. 2015;5:111344. doi: 10.1038/srep11344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peel J.L., Tolbert P.E., Klein M. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005;16(2):164–174. doi: 10.1097/01.ede.0000152905.42113.db. [DOI] [PubMed] [Google Scholar]
- Peng R.D., Dominici F., Louis T.A. Model choice in time series studies of air pollution and mortality. J R Stat Soc Ser A Stat Soc. 2006;169(2):179–198. [Google Scholar]
- Shang Y., Sun Z., Cao J., Wang X., Zhong L., Bi X., Li H., Liu W., Zhu T., Huang W. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ. Int. 2013;54:100–111. doi: 10.1016/j.envint.2013.01.010. [DOI] [PubMed] [Google Scholar]
- Tian Y., Wang J.Y., Zhong C.P. The influence of atmospheric environmental factors on allergic rhinitis and chronic rhinitis in Lanzhou. J. Lanzhou Univ.: Nat. Sci. 2016;52(6) /12. [Google Scholar]
- Vawda S., Mansour R., Takeda A. Associations between inflammatory and immune response genes and adverse respiratory outcomes following exposure to outdoor air pollution: a huge systematic review. Am. J. Epidemiol. 2014;179:432–442. doi: 10.1093/aje/kwt269. [DOI] [PubMed] [Google Scholar]
- Xu Z.M., Wang Z.N., Yao H.B. Diagnosis and treatment of acute infectious rhinosinusitis in children -- clinical practice guide. Chin. J. Practical. Pediatr. 2015;30(7):512–514. [Google Scholar]
- Yao K.H., Yang Y.H. Streptococcus pneumoniae diseases in Chinese children:past, present and future. Vaccine. 2008 Aug 18;26(35):4425–4433. doi: 10.1016/j.vaccine.2008.06.052. [DOI] [PubMed] [Google Scholar]
- Zhang C., Wu W., Gu J.W. Correlations between air pollution and number of patients of acute otitis media and acute tonsillitis in children. J Prev Med Chin PLA. 2017;35(3):218–221. [Google Scholar]