Abstract
The reverse sural artery flap (RSAF) was first described approximately four decades ago and has since been used frequently for reconstruction of soft tissue defects in the distal part of the leg. Although the popularity of this flap never reached the extent of that of free perforator flaps, it still serves as a reliable alternative. This has been demonstrated by the increased rate of publication on the technique in recent years. The number of authors reporting data has risen up to 20 reports a year.
During this time, several new modifications of the flap were inaugurated in order to boost the efficiency and reliability of the flap. The goal of this systematic analysis of the literature was to gain information on the influences of the modifications of the RSAF with regard to consistency and complication rates.
An overall survival rate of 95% and a rate of complications of 14% were reported in all the analyzed cases. Some modifications were able to improve flap viability but not at a statistically significant extent. Venous supercharging and the adipofascial variant of the RSAF provided the best results.
The RSAF is still a remarkable flap design, especially as a backup solution or in circumstances without a microsurgical skilled surgeon. Further investigation with controlled randomized prospective trials is vital to confirm this finding with more evidence.
Keywords: Reverse sural artery flap, Pedicled flap, Fasciocutaneous flap, Lower limb reconstruction, Adipofascial flap
Introduction
The reverse sural artery flap (RSAF) represents a safe-to-perform technique to cover soft tissue defects of the distal limb, with the focus on the feet and ankles.1, 2, 3, 4 In comparison to more demanding microsurgical free flaps, a common practice used for similar indications, the RSAF bears several advantages, including low donor site morbidity and a shorter operative duration.5 Furthermore, this technique can be sufficiently adapted and performed by less experienced microsurgeons. Multiple studies reported excellent outcomes for the RSAF; however, discussion includes an uncertainty with the safety of the procedure.6 Therefore, various modifications have been introduced to improve the reliability of the RSAF. The delayed two stage technique, venous supercharging with an additional microanastomosis of the small saphenous vein, and sparing of the skin paddle by using the adipofascial flap or incorporating a gastrocnemius muscle cuff have been presented in recent decades.5,7, 8, 9
The aim of this systematic analysis is to provide evidence for the improvement of the RSAF through an in-depth investigation of various modifications introduced since 1983. We hypothesize that the overall flap survival has increased during recent decades due to the reported modifications.
The aim of the analysis was to answer the following questions:
-
1.
What is the overall survival rate of the RSAF in literature?
-
2.
What is the overall complication rate of the RSAF in literature?
-
3.
How have these rates changed since the various modifications have been introduced?
-
4.
Do modifications improve the outcome of the RSAF?
Methods
The PICO strategy was used to define the research question construction and literature search.10 Pubmed, Embase, and Cochrane Library for Reviews were used for data screening. The literature search was performed by two individual investigators. The search terms were “sural flap” or “sural flaps” including the corresponding MeSH Terms. The search returned 1352 hits. After screening these articles, we were left with 218 articles with sufficient patient data (Table 1). Recommendations from the Oxford Centre for Evidence-based Medicine (EbM) were used to assess the level of evidence.
Table 1.
Prisma flow diagram of the data selection.
 |
To avoid study bias, all articles were analyzed for number of flaps, specific site of injury (foot; heel; ankle; distal/ proximal leg) or localization of the defect, incidence of complications and detail of complications (complete flap loss; partial flap loss; margin necrosis; venous congestion; infection; donor site breakdown), and flap survival rate. The following variables were also documented for each patient: age, gender, and indication for reconstruction (trauma; wound breakdown; open fracture; ulcer; pressure sore; burn; cancer).
To avoid double counts of flaps, we compared data on authorship, recruitment years, data source, and geographic location. If a patient population was found to overlap, we included the article with the most comprehensive data.
For the pooled analysis, all patients were aggregated into a single data file, and descriptive statistics were calculated for the patients reported in all studies.
For statistical analysis, Kruskal Wallis tests were conducted as appropriate with p-values <0.05.
Results
General flap results
During literature research, 73% of the studies were excluded (Table 1). Up to 218 publications with 5145 RSAFs were included. All flaps were described as distal pedicled sural artery flaps. On average, there were 7.2 studies per annum ranging from one study in 1983 to 20 studies in 2007 (Fig. 1). Eight publications with children under the age of 16 contained 149 flaps. The majority of publications (95%) represented case control series (EBM Level 4), and only 5% showed nonrandomized controlled retrospective cohort/ follow-up studies (EBM Level 3). No controlled randomized prospective clinical trial was found. Many studies (N = 161) reported more than 10 (10-188) patients, and only 57 authors reported less than 10 patients.
Fig. 1.
Publications from the History of the RSAF Flap.
The overall flap-survival rate was 95.2%. Major complications requiring therapy/revision surgery were reported in 14% of all patients. The most common complication was venous congestion 75.3%, followed by a rate of 63% of epidermal losses and tip necrosis of the flap in 55.9% of the cases, which were treated either conservative or operative with split skin grafting.
Nearly half of the cases were carried out by plastic surgeons working in Asia (44%), followed by Europe (28.9%) and North America (12.3%). Most of the patients were male (74.7%), with a mean age of 45.3 years. The age of the patient did not differ statistically in the compared groups except in 8 articles with 149 children and a mean age of 12.7 years.
Sural flaps were used to cover defects of the heel (28.2%), foot (14.4%), or ankle (25.8%). The mean flap dimensions were 8.8 × 5.6 cm (SD 5.3cm). Trauma was the most common indication, followed by chronic ulcers and burns and defects after tumor resection.
Modified flap results
The classic fasciocutaneous unmodified RSAF (4386 flaps, 85%) showed a total failure rate of 5.1% accompanied by 14.8% relevant complications.
A total of 759 (15%) modified flaps were detected. They exhibited a failure rate of 3.2% and a complication rate of 9.1%. The failure rate did not differ from the classic RSAF at a statistically relevant level (p = 0.392). The complication rate showed a significant difference (p = 0.016*).
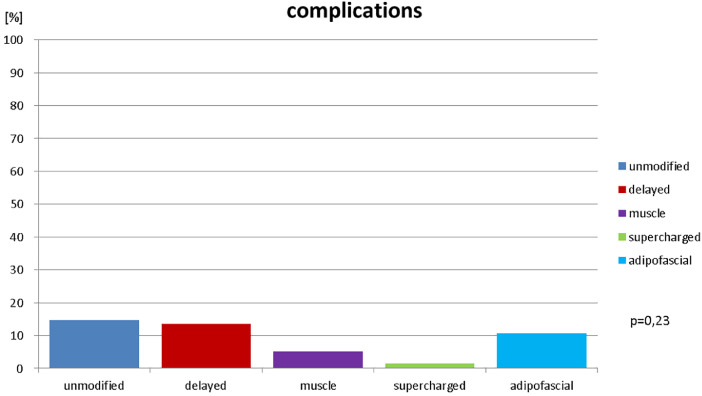
In order to compare the main modifications of the RSAF, four different groups were generated, as shown in Fig. 2: 1. delayed two stage operations, 2. combination with a muscle calf of the gastrocnemius belly, 3. supercharged venous drainage, and 4. skin-sparing adipofascial flap with mesh graft. The four different groups were compared using statistical analysis.
Fig. 2.
Distribution of RSAF Modifications.
Group 1 (delayed): The delayed flap group consisted of 11 studies with 224 (4.4% of all) patients. The total failure rate was 3.6%, and the complication rate was 13.4%. The difference with the classic RSASF group was not evident (Failure rate p = 0.697, Complication rate p = 0.718).
Group 2 (muscle): Flap combination with a gastrocnemius muscle cuff was present in 10 records with 115 (2.2%) patients leading to a total flap loss rate of 2.6% and a complication rate of 5.2%. There was no significant improvement to the unmodified RSAF (Failure rate p = 0.649, Complication rate p = 0.698).
Group 3 (venous supercharged): In venous supercharged flaps, 7 studies with 130 (2.5%) patients were identified with a total flap loss rate of 0.8% and a complication rate of 1.5%. Group 3 showed no statistically relevant difference in failure rate, but it showed an evident improvement in complication rate (Failure rate p = 0.398, Complication rate p = 0.009*).
Group 4 (adipofascial): 14 studies with 290 (5.6%) adipofascial patients were found, and total flap failure was seen in 0.7% of cases, with complications reported in 11% of cases. The difference was not evident at a rate of p = 0.05 (Failure rate p = 0.207, Complication rate p = 0.201).
Fig. 3.
Total failure Rate of RSAF Modifications.
Fig. 4.
Rate of Complications of RSAF Modifications.
Comparing all four groups with each other, the statistical analysis proved insignificant with regard to all groups (Failure rate p = 0.952, Complication rate p = 0.234).
Additional results
Eight articles with 149 children were identified with a success rate of 100% and a complication rate of 8.7%. In burn patients, 77 flaps were performed in three studies with a survival rate of 100% and a complication rate of 1.3%.
A total of 55 studies reported on less than 10 patients. These showed flap failure in 3%, and complications in 10.4% of cases.
No improvement of flap survival during history could be detected. The literature showed a very low flap failure rate, particularly in the first 10 years; in this time the authors reported a failure rate of 0%.
Discussion
Several clinical studies regarding the RSAF were published in recent years, highlighting the ongoing controversial debate on its reliability.11,12
Some interesting systematical reviews showed that trauma is the most common indication for soft tissue reconstruction with the RSAF in the lower leg.10,13,14 More than 60% of sural flaps were indicated because of trauma of the distal leg. Unfortunately, it is not frequently well documented nor differentiated in the literature whether the trauma caused open fracture, osteomyelitis, exposed osteosynthesis material, or only exposed soft tissue.
Persaud et al13 presented a review for the treatment of underlying osteomyelitis and found a failure rate of 8.9% and a complication rate of 13.7% in 110 patients from 5 studies. Other studies showed no difference between patients with diabetic ulcers and traumatic defects.14
Baumeister et al6 highlighted age and comorbidities as predicting variables.
De Baclam et al10 represented a systematic review and pooled analysis dealing with risk factors for the sural flap. They also did not correlate the indication like trauma or open fracture but comorbidities and age with the outcome of the flaps.
This analysis is an approach to correlate technical modifications of the RSAF with the reliability of the flap.
There are some evidence-based suggestions regarding the flap that have led to major modifications in the past. One of the most feared and most frequent complications is venous congestion. In fact, it is also the most common cause for total flap failure.15 The relation between width and length of the pedicle is crucial for flap survival, which suggests that a smaller volume of the flap might also support survival rates .16,17 Moreover, decreasing flap volume is also supported by data of the adipofascial flaps.5
Comparing all modifications of our data analysis, we found adipofascial flap and the venous supercharged flap to be the most reliable outcomes. Both modifications aim to improve the venous flow, and both prevent venous congestion. The venous supercharged flap provides an additional vein in order to gain an increased venous outflow, and the adipofascial flap design diminishes flap volume and prevents venous congestion by increasing exudation via the mesh graft surface during the first postoperative days. Although the supercharging technique changes the operation into a more complex microsurgical demanding procedure, the adipofascial technique requires no further skills and is less time-demanding than the classic RSAF.5 All other modifications showed less improvement compared to the total rates. The venous supercharged flap design was the only modification that reached a statistically relevant difference to the unmodified RSAF in complication rate. All other designs showed no statistically significant differences.
The following limitations were faced while conducting our study. Firstly, the amount of available data with high evidence was very limited. There is no controlled randomized prospective study, which indicates the possibility of a publication bias, which is often suspected in retrospective trials.18 This suggestion is strengthened by the fact that all data derived from articles with limited study participants or a special surgical technique tend to reach better results than the average rates. We selected the burn and children group not as an example to show how good this flap performs but to show the effect of small patient numbers and special selected indications on a presumed publication bias.
It is also remarkable that during the first decade of RSAF trials almost no flap failures nor complications were reported. This fact seems to bear a conspicuous publication bias which influences the rates of the classic RSAF.
The majority of studies were of low quality (EBM 4), and there is little to no statistical relevance and hence no difference in flap survival or major complication rates. Therefore, as the available data implies, the flap continues to be of limited reliability despite suggested technical improvements.
Nevertheless, compared with total flap survival rates of free perforator flaps, which could be identified in the literature,19 the RSAF still seems to be a promising alternative. The especially low failure rates reassert the use of this technique. On the other hand, literature data show a complication rate of 14.9% other than total failure, which is considerably high. As quality of life after RSAF compared to free flaps is not changed and the surgery is much simpler and faster, this analysis supports the assumption that RSAF is better than initially thought.20
Our analysis strongly supports further investigation of the best modifications (adipofascial and supercharged) of the RSAF. Therefore, we recommend prospective clinical trials particularly analyzing the impact of these modifications to lower the complication rate.
No potential conflict of interest relevant to this article was reported.
Funding: Global Open Access Funding University of Wuerzburg.
Contributor Information
Karsten Schmidt, Email: schmidt_k@ukw.de.
Michael Jakubietz, Email: jakubietz_m@ukw.de.
Rainer Meffert, Email: meffert_r@ukw.de.
Fabian Gilbert, Email: gilbert_f@ukw.de.
Martin Jordan, Email: jordan_m@ukw.de.
Rafael Jakubietz, Email: jakubietz_r@ukw.de.
References
- 1.Donski PK, Fogdestam I. Distally based fasciocutaneous flap from the sural region. A preliminary report.S Scand J Plast Reconstr Surg. 1983;17:191–196. doi: 10.3109/02844318309013118. [DOI] [PubMed] [Google Scholar]
- 2.Le Huec JC, Calteux N, Chauveaux D. The distally based sural fascio-cutaneous flap. A new technic for the coverage of loss of substance of the lower leg] J Chir (Paris) 1987;124:276–280. [PubMed] [Google Scholar]
- 3.Masquelet AC, Romana MC, Wolf G. Skin island flaps supplied by the vascular axis of the sensitive superficial nerves: anatomic study and clinical experience in the leg. Plast Reconstr Surg. 1992;89:1115–1121. doi: 10.1097/00006534-199206000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa M, Torii S, Katoh H, Esaki S. The distally based superficial sural artery flap. Plast Reconstr Surg. 1994;93:1012–1020. doi: 10.1097/00006534-199404001-00016. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt K, Jakubietz M, Djalek S. The distally based adipofascial sural artery flap: faster, safer, and easier? A long-term comparison of the fasciocutaneous and adipofascial method in a multimorbid patient population. Plast Reconstr Surg. 2012;130:360–368. doi: 10.1097/PRS.0b013e3182589b0e. [DOI] [PubMed] [Google Scholar]
- 6.Baumeister SP, Spierer R, Erdmann D. A realistic complication analysis of 70 sural artery flaps in a multimorbid patient group. Plast Reconstr Surg. 2003;112:129–140. doi: 10.1097/01.PRS.0000066167.68966.66. discussion 141-142. [DOI] [PubMed] [Google Scholar]
- 7.Kneser U, Bach AD, Polykandriotis E. Delayed reverse sural flap for staged reconstruction of the foot and lower leg. Plast Reconstr Surg. 2005;116:1910–1917. doi: 10.1097/01.prs.0000189204.71906.c2. [DOI] [PubMed] [Google Scholar]
- 8.Tan O, Atik B, Bekerecioglu M. Supercharged reverse-flow sural flap: a new modification increasing the reliability of the flap. Microsurgery. 2005;25:36–43. doi: 10.1002/micr.20072. [DOI] [PubMed] [Google Scholar]
- 9.Le Fourn B, Caye N, Pannier M. Distally based sural fasciomuscular flap: anatomic study and application for filling leg or foot defects. Plast Reconstr Surg. 2001;107:67–72. doi: 10.1097/00006534-200101000-00011. [DOI] [PubMed] [Google Scholar]
- 10.de Blacam C, Colakoglu S, Ogunleye AA. Risk factors associated with complications in lower-extremity reconstruction with the distally based sural flap: a systematic review and pooled analysis. J Plast Reconstr Aesthet Surg. 2014;67:607–616. doi: 10.1016/j.bjps.2014.01.044. [DOI] [PubMed] [Google Scholar]
- 11.Parrett BM, Pribaz JJ, Matros E. Risk analysis for the reverse sural fasciocutaneous flap in distal leg reconstruction. Plast Reconstr Surg. 2009;123:1499–1504. doi: 10.1097/PRS.0b013e3181a07723. [DOI] [PubMed] [Google Scholar]
- 12.Da Costa Santos CM, de Mattos Pimenta CA, Nobre MRC. The PICO strategy for research question construction and evidence search. Rev Lat Am Enfermagem. 2007;15:508–511. doi: 10.1590/s0104-11692007000300023. [DOI] [PubMed] [Google Scholar]
- 13.Persaud S, Chesser A, Pereira R, Ross A. Sural Flap Use for the Treatment of Wounds With Underlying Osteomyelitis: Graft Size a Predictor in Outcome, a Systematic Review. Foot Ankle Spec. 2017;10(6):5. doi: 10.1177/1938640017729496. [DOI] [PubMed] [Google Scholar]
- 14.Assi C, Samaha C, Chamoun Moussa M, Hayek T, Yammine K. A Comparative Study of the Reverse Sural Fascio-Cutaneous Flap Outcomes in the Management of Foot and Ankle Soft Tissue Defects in Diabetic and Trauma Patients. Foot Ankle Spec. 2019;12(5):432–438. doi: 10.1177/193864001881637860-56610.1177/1938640017729496. [DOI] [PubMed] [Google Scholar]
- 15.Sugg KB, Schaub TA, Concannon MJ. The Reverse Superficial Sural Artery Flap Revisited for Complex Lower Extremity and Foot Reconstruction. Plast Reconstr Surg Glob Open. 2015;22:e519. doi: 10.1097/GOX.0000000000000500. eCollection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsai J, Liao HT, Wang PF. Increasing the success of reverse sural flap from proximal part of posterior calf for traumatic foot and ankle reconstruction: patient selection and surgical refinement. Microsurgery. 2013;33:342–349. doi: 10.1002/micr.22099. [DOI] [PubMed] [Google Scholar]
- 17.Wei JW, Dong ZG, Ni JD. Influence of flap factors on partial necrosis of reverse sural artery flap: a study of 179 consecutive flaps. J Trauma Acute Care Surg. 2012;72:744–750. doi: 10.1097/TA.0b013e31822a2f2b. [DOI] [PubMed] [Google Scholar]
- 18.Torgerson CJ. Publication bias: the Achilles heel of systematic reviews? Br J Education Studies. 2006;54:89–102. [Google Scholar]
- 19.Hollenbeck ST, Woo S, Komatsu Longitudinal outcomes and application of the subunit principle to 165 foot and ankle free tissue transfers. Plast Reconstr Surg. 2010;126:924–934. doi: 10.1097/PRS.0b013e3181cc9630. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt K, Jakubietz RM, Gilbert F. Quality of Life after Flap Reconstruction of the Distal Lower Extremity: Is There a Difference Between a Pedicled Suralis Flap and a Free Anterior Lateral Thigh Flap? Plast Reconstr Surg Glob Open. 2019;7:e2114. doi: 10.1097/GOX.0000000000002114. [DOI] [PMC free article] [PubMed] [Google Scholar]