Graphical abstract
Keywords: Takotsubo cardiomyopathy, Recurrent, Variant, Echocardiography
Highlights
-
•
TCM is an increasingly recognized clinical entity.
-
•
Variants include apical, midventricular, basal, and focal.
-
•
The authors present a unique case in which one patient developed three variants.
Introduction
The first case reports of takotsubo cardiomyopathy (TCM) were published in the early 1990s and described a pattern of apical ballooning.1,2 Since then, the literature on TCM has rapidly expanded as the diagnosis has become an increasingly recognized clinical entity. Until the mid-2000s, TCM was considered primarily a disease of the apex and midventricular segments of the left ventricle. However, it is now understood that there are generally four recognized variants, with relative incidences of 81.7% (apical), 14.6% (midventricular), 2.2% (basal), and 1.5% (focal).3, 4, 5, 6 In many patients, cardiac function recovers within a few months, and mortality is similar to that among age- and sex-matched cohorts.7,8 However, a smaller subset of patients develop in-hospital and chronic complications including cardiogenic shock, persistent heart failure, recurrence of TCM, and death.3 We present the case of a patient who developed four separate episodes and three unique variants of TCM over the course of 1.5 years.
Case Presentation
The patient is a 51-year-old woman with a history of hypertension, who initially presented in July 2017 to an emergency department with abdominal pain, nausea, and emesis. Electrocardiography (ECG) was notable for T-wave inversions, and her troponin level was elevated. Transthoracic echocardiography (TTE) demonstrated mild left ventricular (LV) enlargement, apical ballooning with mid and apical akinesis, and an estimated LV ejection fraction (LVEF) of 35%. Left heart catheterization was performed, which demonstrated no evidence of obstructive coronary artery disease, and ventriculography also showed apical ballooning with midventricular and apical akinesis with preservation of the basal segments. The patient was discharged after a complicated hospital course and then presented again 1 month later with similar symptoms of abdominal pain, nausea, and emesis. Given her recent history of TCM, TTE was performed. Per the report, this study demonstrated resolution of the previously seen regional wall motion abnormalities and an LVEF of 55%. Her presenting symptoms were attributed to gastroparesis, and the patient was again discharged.
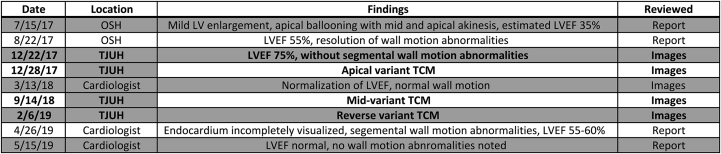
Unfortunately, between July 2017 and February 2019, the patient was admitted to the hospital seven times and required repeat endoscopies for management of her abdominal symptoms. This case report focuses on the multiple variants of TCM with which the patient presented throughout her hospitalizations (Figure 1). All echocardiograms in boldface type are available and presented in this case report.
Figure 1.
Serial echocardiograms. This is a chronological reporting of the available echocardiograms between July 2017 and May 2019. Given that the patient presented to multiple hospitals and providers with different electronic medical records, not all the images were available to be reviewed. Locations at which reviewed echocardiograms were performed included Thomas Jefferson University Hospital (TJUH), local outside hospitals (OSH), and a private cardiologist's office. For each echocardiogram, when available, both the images and reports were reviewed. This figure highlights the multiple variants of TCM that are explored in this report.
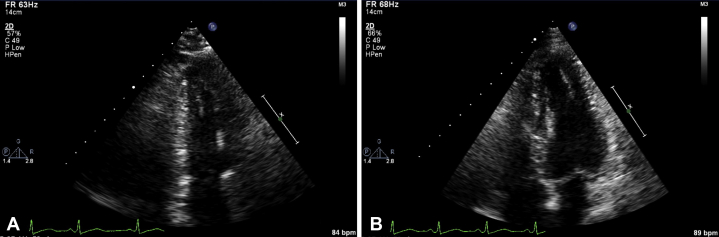
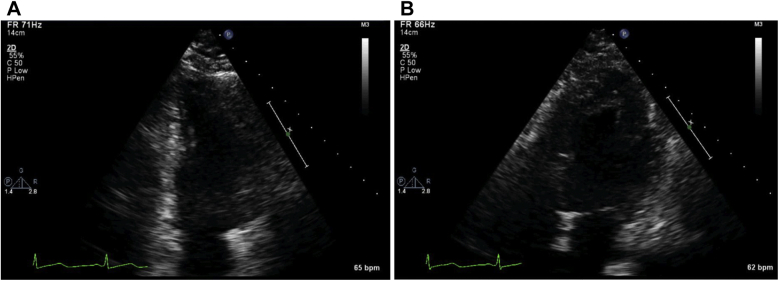
The patient first presented to our hospital in December 2017 with a chief symptom of abdominal pain. During her hospitalization, TTE not only showed normalization of LVEF, but it actually showed hyperdynamic LV systolic function (LVEF 75%) without segmental wall motion abnormalities (Figure 2, Videos 1 and 2).
Figure 2.
Normal echocardiographic findings. TTE demonstrating hyperdynamic LV function with no segmental wall motion abnormalities. Apical two-chamber view (A) and apical four-chamber view (B).
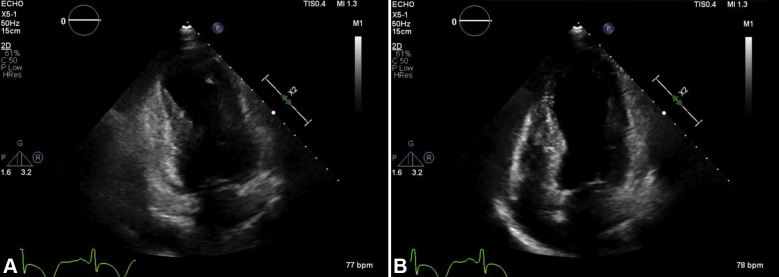
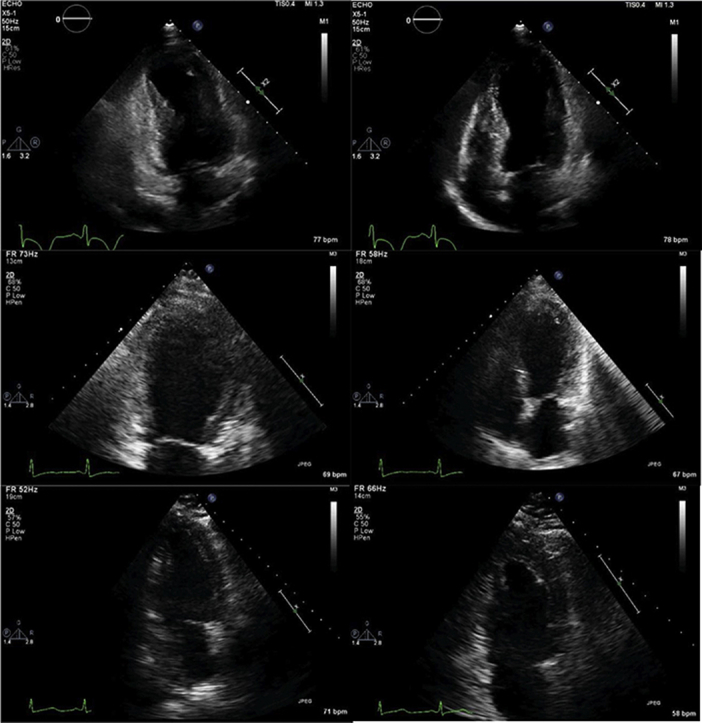
About 1 week into her hospitalization, the patient developed acute onset of substernal, nonradiating chest pain. ECG demonstrated new, diffuse T-wave inversions and poor R-wave progression. Troponin was again mildly elevated. TTE again demonstrated recurrent apical ballooning with midventricular and apical akinesis with preservation of the basal segments and an LVEF of 33% (Figure 3, Videos 3 and 4). With the patient's known history, the findings were attributed to a recurrence of TCM, and she was treated medically. In follow-up with her outpatient cardiologist, repeat echocardiography showed normalization of the left ventricle with normal wall motion.
Figure 3.
Apical-variant TCM. TTE demonstrating apical ballooning with midventricular and apical akinesis with preservation of the basal segments. Apical two-chamber view (A) and apical four-chamber view (B).
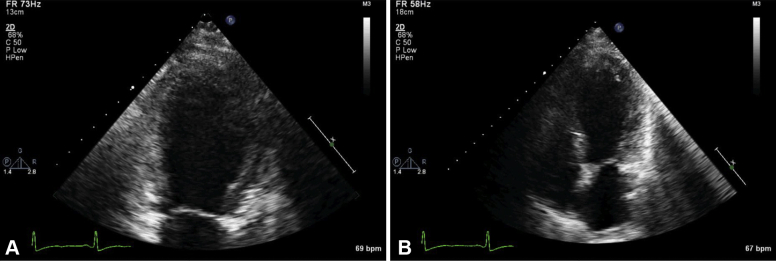
Nine months later, she returned with recurrent gastroparesis. ECG demonstrated diffuse T-wave inversions and a prolonged corrected QT interval. Troponins were again mildly elevated. TTE demonstrated a different segmental pattern of TCM compared with her two prior episodes: midventricular-variant akinesis with preservation of the apical and basal segments, with an LVEF of 25% (Figure 4, Videos 5 and 6).
Figure 4.
Midventricular-variant TCM. TTE demonstrating midventricular-variant akinesis with preservation of the apical and basal segments. Apical two-chamber view (A) and apical four-chamber view (B).
Most recently, 18 months after her initial episode of TCM, the patient was again admitted for abdominal pain. ECG demonstrated sinus bradycardia without T-wave inversions, and troponins were mildly elevated. TTE at this time demonstrated her third variant of TCM, with basal akinesis (reverse pattern) and an LVEF of 45% (Figure 5, Videos 7 and 8). She recovered without incident and was discharged home after repeat endoscopy with onabotulinum toxin A injection. Notably, since the patient underwent left heart catheterization for her initial presentation, she has been managed conservatively without repeat catheterization for her recurrent cardiomyopathy.
Figure 5.
Basal-variant TCM. TTE demonstrating basal akinesis (reverse pattern). Apical two-chamber view (A) and apical four-chamber view (B).
Discussion
TCM is now a well-recognized entity in the differential diagnosis of acute onset chest pain, non–ST-segment elevation myocardial infarction, and ST-segment elevation myocardial infarction. Episodes are often incited by significant emotional or physical stressors, but there are cases in which no stressor can be identified.9 Female gender and the presence of neurologic and psychiatric disease have repeatedly been demonstrated to be associated with TCM.3 These groups of patients have higher levels of sympathetic activation, and there is an incompletely understood relationship between neurohormonal function and the development of TCM.10
However, although TCM is an important clinical entity, there is still a lack of consensus regarding diagnostic criteria. Perhaps the most well-known criteria are the Mayo criteria, which were proposed in 2004 and modified in 2008. These criteria define TCM as (1) transient hypokinesis, akinesis, or dyskinesis of a LV segment with regional wall motion abnormalities that extend beyond distribution of a single vascular distribution; (2) absence of coronary artery disease; (3) new electrocardiographic abnormalities; and (4) the absence of pheochromocytoma or myocarditis. However, does this mean that every patient presenting with possible TCM needs catheterization, biochemical workup for pheochromocytoma, and cardiac magnetic resonance imaging to rule out myocarditis? In our case, the patient had no other signs of a pheochromocytoma, and recent computed tomographic angiography of the abdomen was reviewed but did not show any adrenal abnormalities. Cardiac magnetic resonance imaging was also not performed, likely because of limited inpatient availability and lack of outpatient follow-up. A recently published European Heart Journal expert consensus document grapples with some of these questions and suggests a new InterTak diagnostic score for TCM based on gender, emotional stress, physical stress, ST-segment changes, psychiatric disorders, neurologic disorders, and corrected QT interval prolongation.11,12 Patients with high probability undergo TTE, which can then be used to determine the need for cardiac computed tomographic angiography versus catheterization. Cardiac magnetic resonance imaging is recommended only in the case of suspected infectious myocarditis or lack of resolution of wall motion abnormalities, and laboratory testing for pheochromocytoma is not included.11,12 Whether this consensus document will influence clinical practice remains to be seen, but clearly the diagnostic criteria and workup of TCM are still rapidly changing.
Although TCM was initially thought to be a benign disease with favorable outcomes, there is now evidence that acute in-hospital complications and long-term mortality are similar to acute coronary syndrome, with major adverse cardiovascular and cerebrovascular events of 9.9% per patient year and mortality of 5.6% per patient year.3 Recurrence of TCM has been estimated at 2.8% to 11.4%, with the highest risk during the first year after onset and decreasing rates after that (2.9% per year vs 1.3% per year).6,7 Low body mass index and midventricular outflow obstruction may be predictors of recurrence, and echocardiographic variables such as decreased LVEF, higher E/e′ ratio, and reversible moderate to severe mitral regurgitation may predict higher risk for major adverse events.6,13 However, so far no therapeutic intervention has been shown to improve outcomes in patients with TCM.
The case presented is similar to a few other case reports of single patients developing multiple variants of TCM.14,15 To our knowledge, this is the first case report of a single patient who developed four recurrences of TCM demonstrating the three discrete variants of apical ballooning, midventricular, and basal (or reverse) variants with normalization between episodes. Because of the increasing use of cardiovascular imaging, these cases of recurrent TCM may become more common as we continue to longitudinally follow patients. Alternatively, these cases may remain relatively rare and help provide insight into therapeutic targets to reduce recurrences and comorbidities of TCM. In addition, increased awareness of this phenomenon may help physicians more effectively and efficiently manage patients with recurrent episodes of TCM.
Conclusion
Since TCM was first described, four LV variants have been recognized: apical, midventricular, basal, and focal. We describe a unique case of one patient, with four discrete episodes of TCM, demonstrating three distinct variants.
Footnotes
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2020.01.009.
Supplementary Data
Normal echocardiographic findings, apical two-chamber view. TTE demonstrating hyperdynamic LV function with no segmental wall motion abnormalities.
Normal echocardiographic findings, apical four-chamber view. TTE demonstrating hyperdynamic LV function with no segmental wall motion abnormalities.
Apical-variant TCM, apical two-chamber view. TTE demonstrating apical ballooning with midventricular and apical akinesis with preservation of the basal segments.
Apical-variant TCM, apical four-chamber view. TTE demonstrating apical ballooning with midventricular and apical akinesis and preservation of the basal segments.
Midventricular-variant TCM, apical two-chamber view. TTE demonstrating mid-ventricular variant akinesis with preservation of the apical and basal segments.
Midventricular-variant TCM, apical four-chamber view. TTE demonstrating midventricular variant akinesis with preservation of the apical and basal segments.
Basal-variant TCM, apical two-chamber view. TTE demonstrating basal akinesis (reverse pattern).
Basal-variant TCM, apical four-chamber view. TTE demonstrating basal akinesis (reverse pattern).
References
- 1.Dote K., Sato H., Tateishi H., Uchida T., Ishihara M. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol. 1991;21:203–214. [PubMed] [Google Scholar]
- 2.Sato H.T.H. Tako-tsubo-like left ventricular dysfunction due to multivessel coronary spasm [in Japanese] In: Kodama K., Haze K., Hori M., editors. Clinical aspect of myocardial injury: from ischemia to heart failure. Kagakuhyoronsha Publishing; Tokyo: 1990. pp. 56–64. [Google Scholar]
- 3.Templin C., Ghadri J.R., Diekmann J., Napp L.C., Bataiosu D.R., Jaguszewski M. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 4.Hurst R.T., Prasad A., Askew J.W., Sengupta P.P., Tajik A.J. Takotsubo cardiomyopathy: a unique cardiomyopathy with variable ventricular morphology. JACC Cardiovasc Imaging. 2010;3:641–649. doi: 10.1016/j.jcmg.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Kurowski V., Kaiser A., von Hof K., Killermann D.P., Mayer B., Hartmann F. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132:809–816. doi: 10.1378/chest.07-0608. [DOI] [PubMed] [Google Scholar]
- 6.Nishida J., Kouzu H., Hashimoto A., Fujito T., Kawamukai M., Mochizuki A. “Ballooning” patterns in takotsubo cardiomyopathy reflect different clinical backgrounds and outcomes: a BOREAS-TCM study. Heart Vessels. 2015;30:789–797. doi: 10.1007/s00380-014-0548-x. [DOI] [PubMed] [Google Scholar]
- 7.Elesber A.A., Prasad A., Lennon R.J., Wright R.S., Lerman A., Rihal C.S. Four-year recurrence rate and prognosis of the apical ballooning syndrome. J Am Coll Cardiol. 2007;50:448–452. doi: 10.1016/j.jacc.2007.03.050. [DOI] [PubMed] [Google Scholar]
- 8.Previtali M., Repetto A., Camporotondo R., Citro R., Faggiano P., Bovelli D. Clinical characteristics and outcome of left ventricular ballooning syndrome in a European population. Am J Cardiol. 2011;107:120–125. doi: 10.1016/j.amjcard.2010.08.055. [DOI] [PubMed] [Google Scholar]
- 9.Tsuchihashi K., Ueshima K., Uchida T., Oh-mura N., Kimura K., Owa M., Angina Pectoris-Myocardial Infarction Investigations in Japan Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. J Am Coll Cardiol. 2001;38:11–18. doi: 10.1016/s0735-1097(01)01316-x. [DOI] [PubMed] [Google Scholar]
- 10.Wittstein I.S., Thiemann D.R., Lima J.A., Baughman K.L., Schulman S.P., Gerstenblith G. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–548. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 11.Ghadri J.R., Wittstein I.S., Prasad A., Sharkey S., Dote K., Akashi Y.J. International expert consensus document on takotsubo syndrome (part II): diagnostic workup, outcome, and management. Eur Heart J. 2018;39:2047–2062. doi: 10.1093/eurheartj/ehy077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghadri J.R., Wittstein I.S., Prasad A., Sharkey S., Dote K., Akashi Y.J. International expert consensus document on takotsubo syndrome (part I): clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J. 2018;39:2032–2046. doi: 10.1093/eurheartj/ehy076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Citro R., Rigo F., D'Andrea A., Ciampi Q., Parodi G., Provenza G. Tako-Tsubo Italian Network Investigators. Echocardiographic correlates of acute heart failure, cardiogenic shock, and in-hospital mortality in tako-tsubo cardiomyopathy. JACC Cardiovasc Imaging. 2014;7:119–129. doi: 10.1016/j.jcmg.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 14.Ghadri J.R., Jaguszewski M., Corti R., Luscher T.F., Templin C. Different wall motion patterns of three consecutive episodes of takotsubo cardiomyopathy in the same patient. Int J Cardiol. 2012;160:e25–e27. doi: 10.1016/j.ijcard.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Yoshida T., Nishizawa T., Yajima K., Tsuruoka M., Fujimaki T., Oguri M. A rare case of tako-tsubo cardiomyopathy with variable forms of left ventricular dysfunction: a new entity. Int J Cardiol. 2009;134:e73–e75. doi: 10.1016/j.ijcard.2007.12.092. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Normal echocardiographic findings, apical two-chamber view. TTE demonstrating hyperdynamic LV function with no segmental wall motion abnormalities.
Normal echocardiographic findings, apical four-chamber view. TTE demonstrating hyperdynamic LV function with no segmental wall motion abnormalities.
Apical-variant TCM, apical two-chamber view. TTE demonstrating apical ballooning with midventricular and apical akinesis with preservation of the basal segments.
Apical-variant TCM, apical four-chamber view. TTE demonstrating apical ballooning with midventricular and apical akinesis and preservation of the basal segments.
Midventricular-variant TCM, apical two-chamber view. TTE demonstrating mid-ventricular variant akinesis with preservation of the apical and basal segments.
Midventricular-variant TCM, apical four-chamber view. TTE demonstrating midventricular variant akinesis with preservation of the apical and basal segments.
Basal-variant TCM, apical two-chamber view. TTE demonstrating basal akinesis (reverse pattern).
Basal-variant TCM, apical four-chamber view. TTE demonstrating basal akinesis (reverse pattern).