Abstract
Purpose
We systematically reviewed the literature to compare the clinical and radiologic outcomes and retear rates of superior capsular reconstruction (SCR) using fascia lata autograft (FLA) versus human dermal allograft (HDA) in cases of massive irreparable rotator cuff tears.
Methods
Searches of Pub Med and Cochrane Library identified clinical studies addressing SCR using FLA and HDA. Two reviewers independently screened the titles, abstracts and full texts to extract data from eligible studies. Reported outcome measures were descriptively analyzed.
Results
A total of 6 studies with 2 study groups satisfied the inclusion criteria. The number of shoulders in the HDA group was 155, and in the FLA group, the number was 140 shoulders. The mean age at time of surgery for the HDA group and the FLA group was 60.49 years and 65.8 years, respectively, and the mean follow-up was 15.2 months and 44.6 months, respectively. Active elevation improved from of 121°-130° to 158°-160° in the HDA group and from 74.8°-133° to 130.4°-146° in the FLA group. Active external rotation improved from 36°-45° in the HDA group and from 13°-28° to 30°-43° in the FLA group. The Visual Analog Scale for pain improved from 4-6.25 to 0.38-1.7 points in the HDA group, whereas in the FLA group, it improved from 6-2.5 points. In the HDA group, American Shoulder and Elbow Surgeons scores improved from 42-52 to 77.5-86.5, whereas in the FLA group scores improved from 35-54.4 to 73.7-94.3. The acromiohumeral distance improved in both groups. The retear rate was 3.4%-55% in the HDA group and 4.5%-29% % in the FLA group.
Conclusions
Arthroscopic SCR for massive, irreparable rotator cuff tears using both fascia lata allograft and human dermal allograft leads to improvement in clinical outcomes and radiologic outcomes. There is a lower retear rate in fascia lata allografts. The current literature is heterogeneous and has low levels of evidence.
Level of Evidence
Level IV, systematic review of level IV studies.
Massive rotator cuff tears (MRCTs) are challenging to repair completely, because of tendon retraction, fatty infiltration and muscle atrophy.1, 2, 3
The superior shoulder capsule is a thin membranous structure deep to the rotator cuff.4 A recent anatomic study has shown that the superior shoulder capsule is attached to a substantial area (30%-61%) of the greater tuberosity, suggesting that the superior shoulder capsule is an important component of the glenohumeral joint.5
Patients with irreparable rotator cuff tears have a defect in the superior capsule, which is located on the inferior surface of the supraspinatus and infraspinatus tendons.3 Biomechanically, it was found that superior capsular defects increase glenohumeral translation in all directions, particularly superiorly, suggesting that the superior capsule works not only as a spacer but also as a stabilizer in the glenohumeral joint.4
Because irreparable rotator cuff tears include defects in the superior capsule, a repair should include a method that reduces superior migration. This was the concept behind the superior capsular reconstruction (SCR), which was pioneered by Dr. Teruhisa Mihata in Japan in 2007 using fascia lata.3 A great concern in using fascia lata autografts (FLA) as originally described by Mihata et al. is the donor-site morbidity; it was harvested through an open approach and increased the surgical time.3
Later on, in the United States, Hirahara and Adams6 proposed the use of the human dermal allograft (HDA) as an alternative to FLA. SCR using HDA is now becoming popular, and the number is growing at an exponential rate and shows encouraging results in the short term.1, 6, 7
To reduce the potential donor-site morbidity with FLA, de Campos et al.8 developed a minimally invasive FLA-harvesting technique. They reported no significant donor-site morbidity or hip dysfunction at 18 months.9
A biomechanical cadaveric study comparing SCR using FLA with HDA for irreparable rotator cuff tears demonstrated that both FLA and HDA repairs partially restored superior translation and completely restored subacromial contact and superior glenohumeral joint force. The HDA significantly elongated by 15% during testing, whereas the FLA lengths were unchanged.10
The purpose of our study was to review systematically the literature to compare the clinical and radiologic outcomes and retear rates of SCR using FLA versus HDA in cases of massive irreparable rotator cuff tears (MIRCTs). We hypothesized that patients undergoing SCR using FLA would have better functional outcomes and lower graft retear rates than patients undergoing SCR using HDA.
Methods
Study Design
This systematic literature review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and checklist.11 Before evaluating the results, this review was registered with the PROSPERO International Prospective Register of Systematic Reviews in accordance with recommendations from PRISMA, and the study protocol was published online at http://www.crd.york.ac.uk/PROSPERO/.
Search Technique
Two independent reviewers conducted a thorough literature search of the following online databases: Pub Med and Cochrane Library. The search terms used in the titles, abstracts and keywords fields included the following: massive rotator cuff tear, superior capsular reconstruction and superior capsule. The search was conducted by the 2 independent investigators separately, and the data were extracted from each relevant article. Reviews were searched from database inception to December 2018. We also searched the reference lists of the included studies for additional eligible articles, but no more articles were identified.
Eligibility Criteria
Studies were selected and systematically reviewed according to the following criteria.
Inclusion criteria were clinical studies reporting the results of arthroscopic superior capsular reconstruction for MRCTs using FLA or HDA. We included patients with MRCTs who were of any age or gender and were involved in any physical or sports activities. The duration of postoperative follow-up had to be at least 1 year. Studies had to use 1 or more of the following scores for clinical evaluation: American Shoulder and Elbow Surgeons Score (ASES), Visual Analog Scale (VAS), Subjective Shoulder Value (SSV), or Constant Score and had to confirm retears using MRI.
Exclusion criteria were nonclinical (e.g., cadaveric, animal or biomechanical) studies, systematic reviews or meta-analyses, paprs not written in English, case reports, surgical-technique articles without reported outcomes, abstracts, editors’ comments, and letters to the editor.
Data Collection and Analysis
The selection of studies was performed by 2 independent investigators separately. Any disagreement was resolved by an arbiter.The 2 investigators separately reviewed the abstract of each publication and then performed a close reading of all relevant articles to minimize selection bias and errors. For multiple published articles including the same patient population (i.e., duplicate patient populations), only the most recent publication was used for data extraction.
Finally, to avoid bias, the selected articles and the relative lists of references were reviewed, assessed and discussed by all the authors.
The data were extracted from relevant articles by each of 2 independent investigators working separately. Any disagreement was resolved by an arbiter (the most senior author). Data were extracted from the text, tables and figures of all included studies. Extracted data were collected in a standardized Excel data abstraction sheet. The extracted data included study population characteristics, intervention characteristics and outcomes of interest.
Quality Assessment
Each of the 2 investigators reviewed each study independently for study quality and bias according to the Methodologic Index for Nonrandomized Studies criteria, with a possible maximum score of 16 for nonrandomized studies and 24 for comparative studies.12 Scores were reported as absolute values and as the percentage of the total possible score. Any disagreement was resolved by an arbiter (the most senior third author).
Outcome Measures
The primary outcome measures were: (1) improvements in functional shoulder scores (VAS, SSV, Constant Score, ASES Shoulder Score); (2) improvements in postoperative acromiohumeral intervals; (3) assessment of the incidence of graft retear rates in both groups.
Secondary outcomes included improvements in active shoulder range of motion (elevation, abduction, external rotation).
Statistical Analysis
Using MedCalc statistical software version 15.8 (MedCalc software, Ostend, Belgium), the continuous data were reported as ranges. Dichotomous data (retear rates) were reported as proportions. To quantify the structured review of observational data of retear proportions in the 2 groups, the meta-analytic method of Freeman-Tukey transformation (arcsine square root transformation) was used to calculate the weighted summary proportion under the random effects model. The retear-weighted proportions of both groups were plotted in 1 forest plot graph and compared using the χ2 test with applied Yates correction for continuity. Heterogeneity was determined by estimating the proportion of between-study inconsistencies due to actual differences among studies, rather than differences due to random error or chance, using the I2 statistics. Because of the heterogeneity of the studies, random effects models in a meta-analytic framework were used. The study’s confidence interval was adjusted at the 95% level.
Results
Study Selection
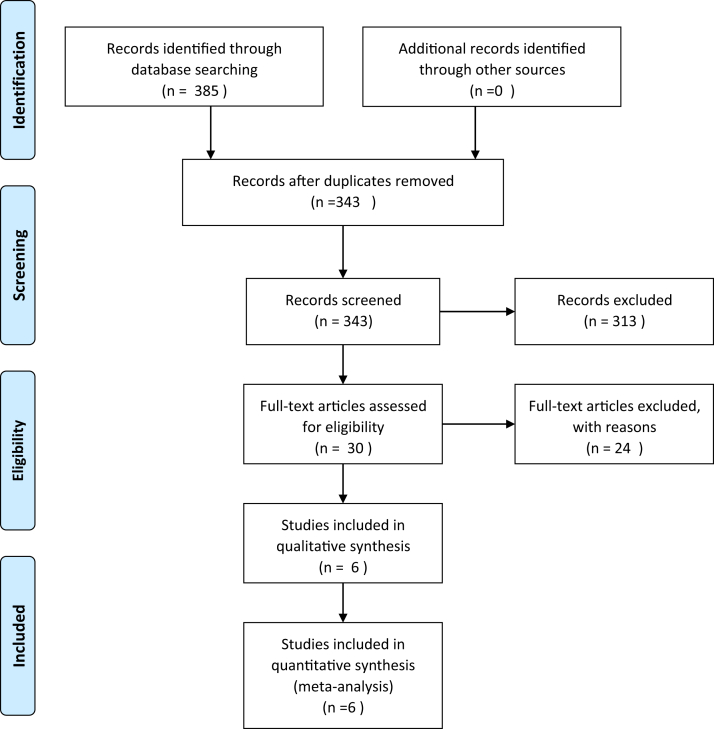
The combined search of Pub Med and Cochrane Library yielded 343 results after duplicates were removed. We returned to the reference lists of previously published systematic reviews to find additional articles to include, but no additional articles were retrieved. After title and abstract screening, 30 studies progressed to full text review, leaving 6 for analysis (Fig 1).1,8,13, 14, 15, 16 Nine technical reviews without clinical outcomes were identified by the search.6,7,17, 18, 19, 20, 21, 22, 23 One study with clinical outcomes was excluded because the number of patients with each type of graft was not mentioned.24 The same authors, Mihata et al.,3,15,25 published 3 papers at 3 different times on the same study population. We included only the most recent study to avoid population duplication.
Fig 1.
Summary of the literature search, screening and review.
Study Demographics
A total of 6 studies were included in this study (Table 1).1,8,13, 14, 15, 16 The level of evidence of all studies was IV case series. Included studies were divided into 2 groups: the human dermal allograft group (HDA group) and the fascia lata autograft group (FLA group). The number of shoulders in the HDA group was 155, with 153 patients; in the FLA group, the number was 140 shoulders in 140 patients. One patient in the FLA group was excluded because he was lost during follow-up.
Table 1.
Study Demographics
| Type of graft | Study | Study type and design | Level of evidence | Journal | MINORS | Mean age | Mean duration of follow-up |
|---|---|---|---|---|---|---|---|
| Acellular dermal allograft | Pennington et al.13 | Retrospective case series. | IV | Arthroscopy | 9/16 | 59.4 years | 12 months (range16-28 m) |
| Denard et al.1 | Case series (multicenter, prospective) | IV | Arthroscopy | 10/16 | 62. years | 17.7 months (range, 12-29 m) | |
| Hirahara14 | Cases series (prospective) | IV | The American Journal of Orthopedics | 8/16 | 61.33 years | 32.38 months (range,25-39 m) | |
| Fascia lata autograft | Mihata15 | Case series | IV | The American Journal of Sports Medicine | 10/16 | 66.2 years | 60 months (range,35-110 m) |
| Lim16 | Case series (retrospective) | IV | Archives of Orthopaedic and Trauma Surgery | 11/16 | 65.3 years | 15 months (range 12-24 m) |
|
| De Campos Azevedo et al.8 | Case series (prospective) |
IV | The Orthopaedic Journal of Sports Medicine | 13/16 | 64.8 years | 24 months |
m, months; MINORS, Methodological Index for Non-Randomized Studies.
The mean age at time of surgery for the HDA and the FLA groups was 60.49 and 65.8 years, respectively. The mean follow-up was substantially longer in the FLA group than in the HDA group: 44.6 months (range 12-110 months) and 15.2 months (range 12-39 months), respectively (Table 1).
Only 2 studies13,14 in the HDA group and 2 studies in the FLA group8,16 reported gender; there were 65 males and 29 females and 16 males and 37 females, respectively. Graft thickness in the FLA group was 5-8 mm. Graft thickness in the HDA group was 1-3 mm.
Risk of Bias and Quality Assessment
The mean Methodological Index for Non-Randomized Studies score for the HDA group studies was 9/16, and for the FLA studies, it was 11/16 (56% and 69%, respectively) (Table 1). The 3 studies in the HDA group may be biased by commercial conflicts of interest between the authors and the manufacturer of the acellular dermal allograft that was used in SCR in the 3 studies.
Clinical Outcome Measures
ASES Scores
All 3 studies1,13,14 in the HDA group (including 155 patients) and only 2 studies15,16 in the FLA group (including 119 patients) used the ASES score. In the HDA group, ASES improved from a preoperative range of 42-52 to a postoperative range of 77.5-86.5, whereas in the FLA group, it improved from a preoperative range of 35-54.4 to a postoperative range of 73.7-94.3 (Table 2).
Table 2.
Clinical Scores Outcomes
| Type of graft | Study | VAS pain (mean ± SD) Pre Post |
ASES (mean ± SD) Pre Post |
SSV (mean ± SD) Pre Post |
Constant Pre Post |
||||
|---|---|---|---|---|---|---|---|---|---|
| Acellular dermal allograft | Pennington et al.13 | 4.0306 ± 2.5478 | 1.5 ± 1.21 | 52.22 ± 19.29 | 81.56 ± 10.21 | N/R | N/R | N/R | N/R |
| Denard et al.1 | 5.8 ± 2.2 | 1.7 ± 2.1 | 43.6 ± 18.6 | 77.5 ± 22.0 | 35.0 ± 19.9 | 76.3 ± 25.2 | N/R | N/R | |
| Hirahara14 | 6.25 | 0.38 | 41.75 | 86.5 | N/R | N/R | N/R | N/R | |
| Fascia lata autograft | Mihata15 | N/R | N/R | 35 (6.7-78.3) | 94.3 (38.3-100) | N/R | N/R | N/R | |
| Lim16 | 6 ± 1.2 | 2.5 ± 1.2 | 54.4 ± 17.9 | 73.7 ± 10.8 | N/R | N/R | 51.7 ± 13.9 | 63.7 ± 8.1 | |
| de Campos Azevedo et al.8 | N/R | N/R | 33 ± 17.4 | 70 ± 23 | 17.5 ± 13.4 | 64.9 ± 18 | |||
ASES, American Shoulder and Elbow Surgeons Score; NR, not reported; SSV, Subjective Shoulder Value; VAS, Visual Analog Scale.
VAS for Pain Score
Of the 6 included studies, 3 studies1,13,14 in the HDA group, including 155 patients, and 1 study16 in the FLA group, including 31 patients, used the VAS for pain. In both groups there were improvements in the VAS for pain; in the HDA group, the VAS for pain improved from a preoperative range of 4-6.25 to a postoperative range of 0.38-1.7, whereas in the FLA group, it improved from 6 preoperatively to 2.5 postoperatively (Table 2).
Subjective Shoulder Value Score
One study in the HDA group (59 shoulders)1 and 1 study in the FLA group (22 shoulders)8 reported improvement in subjective shoulder value scores (SSV) (from 76 to 35, P < .001) and (from 70 to 33, P < .001), respectively (Table 2).
Range of Motion
Active Elevation
In the HDA group, only 2 studies reported active elevation,1,13 whereas all the studies of the FLA group did. Active elevation improved from a preoperative range of 121°-130° to a postoperative range of 158°-160° in the HDA group and from a preoperative range of 74.8°-133° to a postoperative range of 130.4°-146° in the FLA group (Table 3).
Table 3.
Range of Movement
| Type of Graft | Study | Mean Active Elevation(˚) Pre Post |
Active External Rotation Pre Post |
Abduction Pre Post |
|||
|---|---|---|---|---|---|---|---|
| Acellular dermal allograft | Pennington et al.13 | 121 (range 10-180) | 160 (range 70-180) | N/R | N/R | 103 (range 15-180) | 159 (range 68-180) |
| Denard et al.1 | 130˚ ± 48˚ | 158˚ ± 32˚ | 36˚ ± 18˚ | 45˚ ± 17˚ | N/R | N/R | |
| Hirahara14 | NR | NR | NR | NR | NR | NR | |
| Fascia lata autograft | Mihata15 | 96.5˚ (range 10-170) | 130.37˚ (range 20-180) |
27.2˚ (range 0-80) |
42.78˚ (range 0-90) |
N/R | |
| Lim16 | 133 ± 35 | 146 ± 18 | 28 ± 16 | 30 ± 15 | N/R | ||
| de Campos Azevedo et al.8 | 74.8 | 143.8 (2 yrs) | 13.2 | 35.6 | 53.2 | 120.7 | |
Active External Rotation
In the HDA group, only 1 study evaluated active external rotation,1 whereas all the FLA group studies did. The improvement in active external rotation was from 36°-45° (59 shoulders) in the HDA group and from a preoperative range of 13°-28° to a postoperative range of 30°-43° (140 shoulders) in the FLA group (Table 3).
Active Abduction
Only 1 study evaluated the active abduction in each group.8,13 The improvement in mean active abduction was from 103°-159° (88 shoulders) in the HDA group6 and from 53.2°-120.7° (22 shoulders) in the FLA group8 (Table 3).
Radiological Outcome Measures
Acromiohumeral Distance
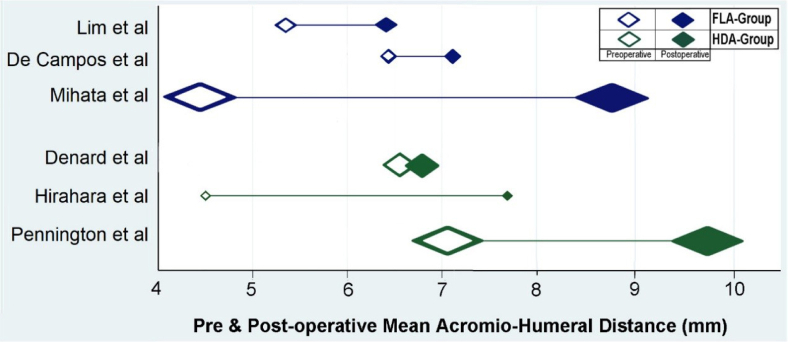
All 6 studies reported improvement in postoperative acromiohumeral distance (AHD). The acromiohumeral distance improved in the HDA group from a preoperative range of 4.5 mm-7.1 mm to a postoperative range of 6.7 mm-9.7 mm, and in the FLA group, from a preoperative range of 4.44 mm-6.4 mm to a postoperative range of 6.4 mm-9.7 mm (Fig 2). Further data concerning the Hamada and Goutallier stage of the operated shoulders are referred to in Table 4.
Fig 2.
Forest plot of mean preoperative and postoperative acromiohumeral distance of the fascia lata autograft (FLA) group and the human dermal allograft (HDA) group. The empty bullet represents the preoperative mean acromiohumeral distance (mm). The solid bullet represents the postoperative acromiohumeral distance (mm). The blue bullets represent the FLA group; the green bullets represent the HDA group. The size of the bullet represents the size of the patient population.
Table 4.
Radiologic Outcome Measures
| Type of graft | Study | Stage of osteoarthritis (Hamada classification) |
Preoperative Goutallier stage (fatty infiltration) | Acromiohumeral distance pre/post (mean ± SD) |
|
|---|---|---|---|---|---|
| Acellular dermal allograft | Pennington et al.13 | No patients were determined to have severe glenohumeral arthritis or acetabularization | Preoperative stage 3 or 4 | 7.1 | 9.7 |
| Denard et al.1 | 31 grade 1 16 grade 2 9 grade 3 1 grade 4 |
FD-SS† 0:5:9:33:10 FD-IS† 1:9:10:18:19 FD-SSc† 11:23:14:4:5 |
6.6 ± 3.0 mm | 6.7 ± 3.0 mm | |
| Hirahara14 | Mean grade 3 | Mean stage 3.25 | 4.5 ± 2.25 mm | 7.7 ± 2.08 mm | |
| Fascia lata autograft | Mihata15 | Stage 1: 17 Stage 2: 53 Stage 3: 16 Stage 4a: 1 Stage 4b: 1 |
Stage 2: 5 Stage 3: 34 Stage 4: 49 |
4.44 (range 0.6-9.0) | 8.75 (range 2.3-15.9) |
| Lim16 | Grade 1, 2 | Mean for subscapularis 1.1 ± 0.7 Supraspinatus 2.7 ± 0.6 Infraspinatus 2.5 ± 0.7 |
5.3 ± 2.2 | 6.4 ± 2.3 | |
| de Campos Azevedo et al.8 | Stage 1 :13 Stage 2: 9 |
Cumulative grade ≥ 3 | 6.4 ± 3.3 | 7.1 ±.2.5 | |
FD-IS, fatty degeneration of the infraspinatus; FD-SS, fatty degeneration of the supraspinatus; FD-SSC, fatty degeneration of the subscapularis.
Data correspond to Goutallier grades 0, 1, 2, 3, and 4, respectively.
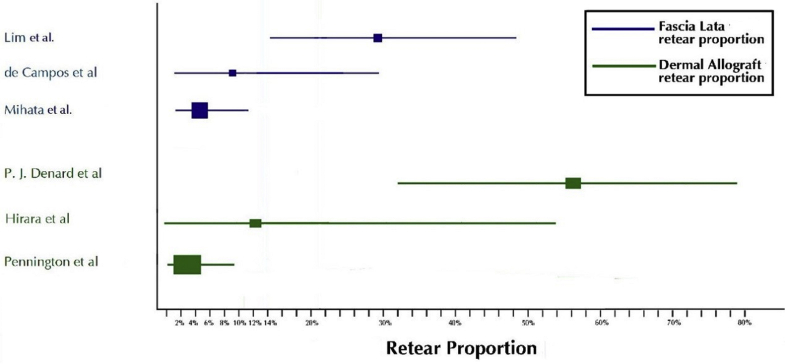
Graft Retear Rate
All 6 studies reported the graft retear rate as an outcome. Graft tear was assessed on the basis of postoperative MRI, which was done at a mean of 51.4 months (range 6 months-60 months ) in 140 patients in the FLA group , whereas in the HDA group, MRIs were done for only 113 patients, and the time of MRI follow-up was at 1 year in 1 study1 and was not mentioned in the other 2 studies.13,14
The retear rate ranged from 3.4%-55% in the HDA group, whereas in the FLA group, it ranged from 4.5%-29% (Fig 3).
Fig 3.
Forest plot of proportions of retear rates of the fascia lata autograft (FLA) group and the human dermal allograft (HDA) group. The blue bullets represent the FLA group; the green bullets represent the HDA group.
The sites of graft failure were reported in 2 studies1,13 of the HDA group; there were 10 failures on the humeral side, 3 intrasubstance and 1 on the glenoid side. In the FLA group, only Lim et al.16 mentioned the graft failure site and all were on the humeral side.
Discussion
This review demonstrates that arthroscopic SCR for MIRCTs using both FLA and HDA leads to improvement in clinical and radiologic outcomes.
There was greater improvement in the FLA group than in the HDA group in terms of range of movement. Postoperative active external rotation improved by 9° ± 1 in the HDA group and 15°-17° (range 30°-43°) in the FLA group .Postoperative active abduction improved by 56° and 67.5° in the HDA group and the FLA group, respectively. Postoperative active elevation improved by 30°-37° (range 158°-160°) and 13°-55.6° (range 130.4-146) in the HDA group and the FLA group, respectively.
There was demonstrable improvement in the VAS pain score and ASES in both groups. The improvement in the VAS pain score was greater in the HDA group, whereas the improvement in the ASES score was greater in the FLA group. One study of the HDA group1 and 1 study of the FLA group8 showed statistically significant improvement in SSV (P value < .001).
The AHD is an important prognostic radiographic marker after rotator cuff repair because it signifies improvement of shoulder joint biomechanics and rotator cuff function.26 In addition, it was found that if there is no improvement or even little improvement of AHD immediately postoperatively after arthroscopic SCR, it was associated with poor survival of the graft and increased incidence of retearing.24 Lee et al. reported that the mean AHD was significantly higher in patients with graft thickness ≥ 6 mm than that in patients with graft thickness < 6 mm.24 In this study, there was improvement of postoperative AHD in both groups, with a tendency toward better improvement in the FLA group.
Although we could not assess its statistical significance, the graft retear rate percent range in the HDA group was higher than that in the FLA group: 3.4%-55% and 4.5%-29%, respectively. There was substantial heterogeneity between the study results in each group. This demonstrated substantial heterogeneity could be explained by between-study variations in the baseline characteristics of patients in the HDA group because subscapularis tears requiring repair were included in 1 study1 and excluded in another.13 Also in the FLA group, there were notable differences in the experience levels of the surgeons in the various studies; procedures were performed by the pioneer of SCR procedures in 1 of them.15
Moreover, the graft retear rate may be higher in the HDA group than reported because postoperative MRI was not done for all patients in this group and was done within 1 year postoperatively, unlike the FLA group in which the postoperative MRI was performed for all patients at a mean of 51.4 months. In both groups, the most common site of graft tear was at the greater tuberosity footprint.1,13,15 This may be due to the greater stresses on the graft on the humeral side during movement or to attrition of the graft due to acromiohumeral contact. The thickness of the superior shoulder capsule at the attachment of the greater tuberosity ranges from 4.4-9.1 mm.5 Mihata et al. found, in a biomechanical study, that graft thicknesses of 4 mm and 8 mm significantly decrease subacromial peak contact pressure at 0° and 30° of glenohumeral abduction, but only the 8 mm graft significantly decreased superior translation at 0° and 30° of glenohumeral abduction.27 And after biomechanical testing, the single-layer HD allograft elongated in a medial-lateral direction by approximately 15%, whereas the size of the 8 mm fascia lata allograft, which completely restored superior translation, did not significantly change after testing.10 Mihata et al. suggested both anterior and posterior side-to-side suturing when using human dermal allografts in arthroscopic SCR and claimed that this may limit the amount of medial-lateral elongation because the graft is being held in an anterior-posterior direction.10
Denard et al. reported poor outcomes with 1 mm and 2 mm dermal allografts and recommended the use of 3 mm dermal allografts, which is currently the maximum thickness of dermal allografts commercially available.1
In a clinical study by Mihata et al.,3 they found that postoperative clinical outcome scores improved significantly in patients with healed grafts compared to patients with graft tears or retears after SCR. Two studies in the FLA group15,16 and 2 studies in the HDA group1,14 reported improved clinical outcomes in patients with healed grafts compared to patients with nonhealed or retorn grafts. This finding suggest that graft healing is important for improvement of shoulder function after SCR.
Limitations
This study was limited by the quality of evidence available for assessing the improvements in function, pain and retear rates after SCR when using fascia lata allograft or dermal allograft. It was also limited by the small number of patients and studies, which are all case series level IV, and that made it difficult to do meta-analyses. Most studies did not have a minimum of 24 months of follow-up and lacked sufficient follow-up data to allow accurate comparison of results between the 2 groups.
Conclusions
Arthroscopic SCR for massive irreparable rotator cuff tears using both fascia lata allograft and human acellular dermal allograft leads to improvement in clinical outcomes and radiologic outcomes. There is a lower retear rate with fascia lata allografts. The current literature is heterogeneous and has low levels of evidence.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Denard P.J., Brady P.C., Adams C.R., et al. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 2.Goutallier D., Postel J.M., Bernageau J., et al. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 3.Mihata T., Lee T.Q., Watanabe C., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 4.Ishihara Y., Mihata T., Tamboli M., et al. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2014;23:642–648. doi: 10.1016/j.jse.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 5.Nimura A., Kato A., Yamaguchi K., et al. The superior capsule of the shoulder joint complements the insertion of the rotator cuff. J Shoulder Elbow Surg. 2012;21:867–872. doi: 10.1016/j.jse.2011.04.034. [DOI] [PubMed] [Google Scholar]
- 6.Hirahara A.M., Adams C.R. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e637–e641. doi: 10.1016/j.eats.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petri M., Greenspoon J.A., Millett P.J. Arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e751–e755. doi: 10.1016/j.eats.2015.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Campos Azevedo CI, Angelo A, Vinga S. Arthroscopic superior capsular reconstruction with a minimally invasive harvested fascia lata autograft produces good clinical results. Orthop J Sports Med 2018;6:2325967118808242. [DOI] [PMC free article] [PubMed]
- 9.Angelo A., de Campos Azevedo C.I. Minimally invasive fascia lata harvesting in ASCR does not produce significant donor site morbidity. Knee Surg Sports Traumatol Arthrosc. 2019;27:245–250. doi: 10.1007/s00167-018-5085-1. [DOI] [PubMed] [Google Scholar]
- 10.Mihata T., Bui C.N.H., Akeda M., et al. A biomechanical cadaveric study comparing superior capsule reconstruction using fascia lata allograft with human dermal allograft for irreparable rotator cuff tear. J Shoulder Elbow Surg. 2017;26:158–166. doi: 10.1016/j.jse.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 11.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-6. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 13.Pennington W.T., Bartz B.A., Pauli J.M., et al. Arthroscopic superior capsular reconstruction with acellular dermal allograft for the treatment of massive irreparable rotator cuff tears: Short-term clinical outcomes and the radiographic parameter of superior capsular distance. Arthroscopy. 2018;34:1764–1773. doi: 10.1016/j.arthro.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 14.Hirahara A.M., Andersen W.J., Panero A.J. Superior capsular reconstruction: Clinical outcomes after minimum 2-year follow-up. Am J Orthop. 2017;46:266–278. [PubMed] [Google Scholar]
- 15.Mihata T., Lee T.Q., Hasegawa A., et al. Arthroscopic superior capsule reconstruction can eliminate pseudoparalysis in patients with irreparable rotator cuff tears. Am J Sports Med. 2018;46:2707–2716. doi: 10.1177/0363546518786489. [DOI] [PubMed] [Google Scholar]
- 16.Lim S., AlRamadhan H., Kwak J.M., et al. Graft tears after arthroscopic superior capsule reconstruction (ASCR): Pattern of failure and its correlation with clinical outcome. Arch Orthop Trauma Surg. 2019;139:231–239. doi: 10.1007/s00402-018-3025-7. [DOI] [PubMed] [Google Scholar]
- 17.Anderson S., Trenhaile S. All knot-less arthroscopic superior capsular reconstruction. Arthrosc Tech. 2018;7:e811–e816. doi: 10.1016/j.eats.2018.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burkhart S.S., Denard P.J., Adams C.R., et al. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407–e1418. doi: 10.1016/j.eats.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laskovski J.R., Boyd J.A., Peterson E.E., Abrams J.S. Simplified technique for superior capsular reconstruction using an acellular dermal allograft. Arthrosc Tech. 2018;7:e1089–e1095. doi: 10.1016/j.eats.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Narvani A.A., Consigliere P., Polyzois I., et al. The "pull-over" technique for arthroscopic superior capsular reconstruction. Arthrosc Tech. 2016;5:e1441–e1447. doi: 10.1016/j.eats.2016.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pennington W.T., Chen S.W., Bartz B.A., Pauli J.M. Arthroscopic superior capsular reconstruction with acellular dermal allograft using push-in anchors for glenoid fixation. Arthrosc Tech. 2018;8:e51–e55. doi: 10.1016/j.eats.2018.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heuberer P.R., Pauzenberger L., Smolen D., et al. An arthroscopic knotless technique for anatomical restoration of the rotator cuff and superior capsule: The double-layer cinch bridge. Arthrosc Tech. 2017;7:e7–e12. doi: 10.1016/j.eats.2017.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tokish J.M., Beicker C. Superior capsule reconstruction technique using an acellular dermal allograft. Arthrosc Tech. 2015;4:e833–e839. doi: 10.1016/j.eats.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee S.J., Min Y.K. Can inadequate acromiohumeral distance improvement and poor posterior remnant tissue be the predictive factors of re-tear? Preliminary outcomes of arthroscopic superior capsular reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:2205–2213. doi: 10.1007/s00167-018-4912-8. [DOI] [PubMed] [Google Scholar]
- 25.Mihata T., Lee T.Q., Fukunishi K., et al. Return to sports and physical work after arthroscopic superior capsule reconstruction among patients with irreparable rotator cuff tears. Am J Sports Med. 2018;46:1077–1083. doi: 10.1177/0363546517753387. [DOI] [PubMed] [Google Scholar]
- 26.Chung S.W., Kim J.Y., Kim M.H., et al. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med. 2013;41:1674–1683. doi: 10.1177/0363546513485719. [DOI] [PubMed] [Google Scholar]
- 27.Mihata T., McGarry M.H., Kahn T., et al. Biomechanical effect of thickness and tension of fascia lata graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy. 2016;32:418–426. doi: 10.1016/j.arthro.2015.08.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.