Abstract
Purpose
To systematically review the operative versus nonoperative methods for management of iliotibial band syndrome (ITBS) with comparison of the respective clinical outcomes.
Methods
By adhering to the Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines, 3 databases (Medline, Scopus, Web of Science) searched from inception to October 2019 for randomized clinical trials (RCTs) and observational studies on humans that reported the outcomes following operative or nonoperative management of ITBS. Excluded were case reports, case series with <5 participants, review articles, non-English articles, and non–peer-reviewed articles. The Methodological Index for Non-Randomized Studies (MINORS) criteria for observational studies and the Cochrane Risk of Bias Tool for RCTs were used for quality control.
Results
There were 15 eligible studies (9 for operative,6 for nonoperative treatment) examining 179 athletes (mean age 27.3 years, range: 17-53) who received conservative therapy for ITBS and 200 athletes (mean age 30.1 years, range: 14-63) who underwent surgical treatment. Most athletes were runners (65%). The mean follow-up time was significantly longer in studies reporting the outcomes following operative compared with nonoperative ITBS treatment (33.5 vs 2 months, respectively, P < .05). Significant variability in the methods used to assess the clinical outcomes precluded meta-analysis. The most commonly reported (7/9 studies, 77.7%) variable for postoperative evaluation in athletes was the return to sport rate (range: 81%-100%). Significant reduction in pain was consistently (6/6 studies,100%) found among the studies reporting the results of conservative ITBS treatment. The included RCTs were of good (1/5, 20%), fair (2/5, 40%), or poor (2/5, 40%) quality, whereas the average MINORS score was 7.4 (range: 3-13) for observational studies. The level of evidence ranged from Level II (6/15 studies) to IV (9/15 studies).
Conclusions
Based on the current literature and at a maximum follow-up time of 6 months, conservative therapy can effectively reduce ITBS symptoms in athletes. Multiple surgical options exist for athletes who do not respond to nonoperative measures, with a reported return to sport rate between 81% and 100%.
Level of Evidence
Systematic review of Level II and IV studies
Iliotibial band syndrome (ITBS) has been recognized as a common cause of lateral knee pain, especially in runners, cyclists, and other athletes who participate in sports that involve repetitive flexion–extension of the knee joint.1, 2, 3 The pathogenesis of ITBS is multifactorial, and various pathophysiologic abnormalities have been associated with this overuse injury, including repetitive rubbing of the distal iliotibial band against the lateral femoral epicondyle during knee flexion–extension; iliotibial band impingement at 30° of knee flexion; hip abductor weakness that results in iliotibial band overtightening during knee flexion–extension motion; inflammation of the lateral synovial recess or the sub-iliotibial band bursa of the lateral knee; periosteal inflammation of the lateral epicondyle; and others.4, 5, 6, 7, 8, 9, 10
Overuse injuries, including ITBS, are often challenging to treat. ITBS can cause chronic lateral knee pain that limits a patient’s daily activity and participation in sports.8 The management of ITBS most commonly begins with a course of conservative therapy, with surgical options reserved for cases unresponsive to conservative measures. Commonly used nonoperative treatment options for ITBS include physical therapy with an emphasis on iliotibial band stretching and strengthening of the hip abductors, local injection therapy to reduce inflammation and pain, and/or oral anti-inflammatory medications.8,11
Previous systematic reviews have examined the clinical outcomes following the management of ITBS in runners, and they found a lack of evidence to support the clinical efficacy of the reported treatments.4,12 No previous systematic review has examined the effectiveness of the available ITBS therapies, regardless of patient activity. During the last decade, the short-term outcomes of open and arthroscopic surgical techniques to address ITBS have been described in retrospective studies.13, 14, 15, 16, 17, 18, 19 With the expansion of the surgical techniques to treat ITBS, a comparison between patient outcomes following the operative versus non-operative treatment for ITBS is missing.
The purpose of this study was to systematically review the operative versus nonoperative methods for management of ITBS with comparison of the respective clinical outcomes. We hypothesized that the surgical and nonsurgical therapy for ITBS would yield comparable patient results.
Methods
Design, Eligibility Criteria, and Search Strategy
The methodology was in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA). The Medline, Scopus, and Web of Science databases were searched for eligible articles using the following search terms: “iliotibial band syndrome,” “iliotibial band friction syndrome,” “treatment iliotibial band syndrome,” “treatment iliotibial band friction syndrome,” “clinical outcomes iliotibial band syndrome,” and “clinical outcomes iliotibial band friction syndrome.” Inclusion criteria consisted of peer-reviewed articles published in the English language and observational studies and clinical trials on humans, which described an operative or conservative method of treatment for ITBS and reported patient outcomes. Excluded were case reports, case series with fewer than 5 participants, review articles, articles that described a conservative or surgical therapy for ITBS but did not report patient outcomes, non-English language studies, non-human studies, and non–peer-reviewed articles. There was no limitation in publication year.
Study Screening and Data Extraction
Two independent researchers (I.B., P.G.) approved the eligible articles for inclusion in this study. All articles were screened by title and abstract and then by full text, and the study criteria were applied in each stage of the selection process. A third reviewer (board-certified orthopaedic surgeon) was consulted if any discrepancy occurred between the initial investigators, until the disagreement was resolved. The reference lists of the included studies were screened for additional relevant articles.
Data extraction was conducted using predesigned tables. The variables collected were study type, level of evidence, patient demographics (sex, age, sport activity), treatment protocol for ITBS, follow-up time, clinical outcomes, and complications. For studies that reported outcomes following surgical management of ITBS, we recorded the preoperative symptoms and physical examination findings, imaging tests, attempted conservative therapy protocol, additional procedures performed during the operation for ITBS, postoperative rehabilitation protocol, and methods of thromboembolic prophylaxis.
Quality Assessment, Heterogeneity Assessment, and Data Analysis
Quality assessment of the included studies was performed by 2 independent reviewers, and any disagreement was discussed until consensus was reached. To evaluate the quality of the clinical trials, we used the Cochrane Risk of Bias Tool for the Randomized Clinical Trials and each study was characterized as of good, fair or poor quality. The observational studies were assessed using the Methodological Index for Non-Randomized Studies (MINORS) criteria, with an ideal score of 24 points for comparative studies and 16 points for noncomparative studies. The interrater reliability was measured as the percent agreement between the 2 independent reviewers. The level of evidence of the included articles was reported based on the accepted guidelines of the American Academy of Orthopaedic Surgeons.20 One author evaluated the studies for possible heterogeneity. The results were assessed for eligibility to proceed with data meta-analysis.
Results
Search Results
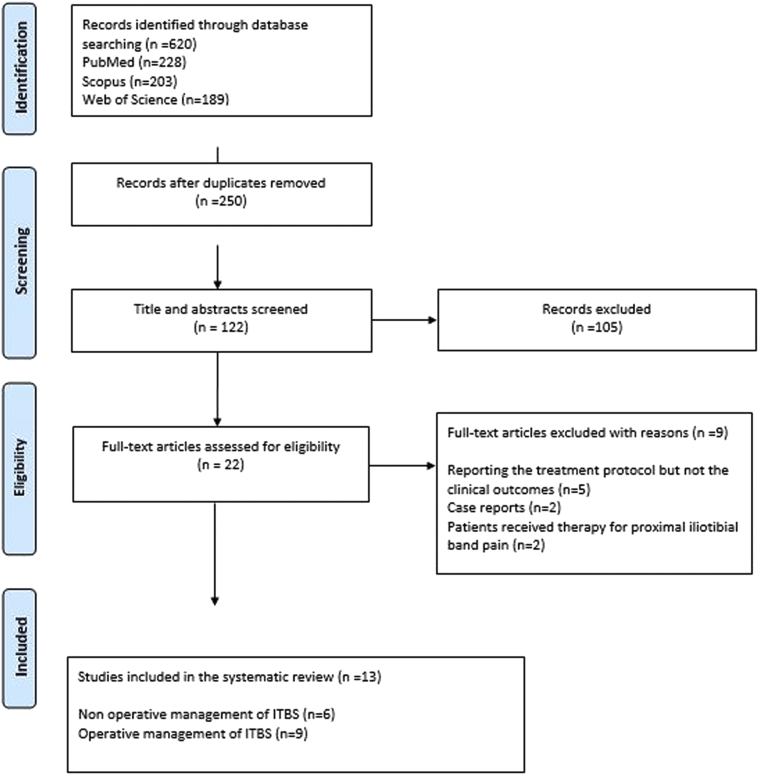
The search strategy resulted in 620 potentially relevant articles. A total of 122 abstracts and 22 full texts were selected for review, and of these, 15 studies met the inclusion criteria (Fig 1).
Fig 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram. (ITBS, iliotibial band syndrome.)
Study Quality
After we evaluated the quality of the included RCTs (5 studies) using the Cochrane Risk of Bias Tool for the Randomized Clinical Trials (Appendix, Table 1, available at www.arthroscopyjournal.org), only the most recently conducted RCT of Weckstrom et al.21 was characterized as a good-quality study (1/5, 20%), whereas the rest of RCTs were characterized as being of fair (2/5, 40%) or poor (2/5, 40%) quality. The average MINORS score of the included observational studies (Appendix Table 2, available at www.arthroscopyjournal.org) was 7.4 (range: 3-13), which indicated a fair quality of research data. The percent agreement was >90% between the 2 independent reviewers, which indicates high interrater reliability on evaluating the quality of the included articles. The level of evidence was determined to be Level II in 6 studies (1 prospective comparative study, 5 RCTs) and Level IV in 9 studies (9/9 were retrospective case series)
Study Heterogeneity and Meta-Analysis
Overall, there was significant heterogeneity between the included studies in terms of the patient population, treatment protocol followed for the management of ITBS, and reporting of outcomes. Therefore, a meta-analysis was not conducted within the 2 individual study groups (nonoperative vs operative management of ITBS). Furthermore, we were unable to compare the clinical outcomes following operative versus nonoperative therapy for ITBS.
Nonoperative Management of ITBS, Clinical Outcomes, and Complications
Six of the included articles reported the clinical outcomes of nonoperative treatment of ITBS syndrome, including 5 clinical trials (Table 1).21, 22, 23, 24, 25, 26
Table 1.
Studies Reporting Nonoperative Treatment for ITBS and the Associated Clinical Outcomes
| Study, Year, Journal Type of Study, Level of Evidence |
Study Population (Participants, Age) | ITBS Treatment Protocol | Follow-Up Assessment Tool and Timeline | Clinical Outcome | Complications |
|---|---|---|---|---|---|
| Weckstrom et al.,21 2016 Journal of Back and Musculoskeletal Rehabilitation RCT, II |
24 recreational runners (14 male, 10 female) with unilateral ITBS Age in years (mean, SD): SWT group: 33 (10) ManT group: 34 (6) |
SWT group (n = 11): shockwave therapy + standardized exercise program ManT group (n = 9): manual therapy + standardized program |
4 weeks: changes in pain (11-point scale) during treadmill running 8 weeks: changes in pain (11-point scale) during treadmill running 6 months: patients were only assessed (by telephone) for symptoms based on the current activity level |
Baseline to week 4: Similar reduction in pain between SWT and ManT groups Baseline–week 8: Similar reduction in pain between SWT and ManT groups 6 months: All pain-free subjects at week 8 remained pain-free at 6 months |
SWT group: transient reddening of skin (all subjects) ManT group: transient bruising on the lateral thigh following trigger point therapy (small but unspecified number of subjects) |
| Beers et al.,23 Physiotherapie Canada OS, II |
16 athletes (5 male, 11 female) Mean age in years: 33.7 (range: 20-53) |
6-week rehabilitation program to strengthen the hip abductors | Comparison of hip abductor strength between injured and uninjured side + AMI Evaluation at baseline Follow-up time points: 2, 4, 6 weeks |
Hip abductor strength was significantly different between injured and uninjured sides at baseline, but the difference disappeared at 6 weeks Hip abductor moments were related to physical function domain of AMI at weeks 2, 4, 6, indicating improvement in function as the injured lower extremity was becoming stronger |
none |
| Gunter et al.,22 2004 British Journal of Sports Medicine RCT, II |
18 runners with unilateral gat least grade 2 ITBS Age in years (mean, SD): 28.9 (5) |
EXP group (n = 9): ITB injection 40 mg methylprednisolone acetate + with short acting local anesthetic CON group (n = 9): ITB injection with short acting local anesthetic |
Total pain during running (calculated as area under the pain versus time graph), using 11-point pain scale every minute during treadmill running Follow-up time: Day 0 (preinjection), day 7, day 14 |
Preinjection day 7: no significant difference in total pain between EXP and CON groups Day 7–Day 14: EXP group had greater decrease in total pain compared with CON none |
None |
| Bischoff et al.,24 1995 Research in Sports Medicine: An International Journal RCT, II |
25 students (26 ITBS cases) at Navy basic underwater demolition training class Age in years (mean) group P: 23 group I: 22 |
Group I (n = 13) forced rest+ three panel knee immobilizer + 800 mg ibuprofen daily + 5-7 minutes ice massage daily Group P (n = 13): daily phonophoresis with 10% hydrocortisone cream 800 mg ibuprofen daily + 5-7 minutes ice massage daily |
Daily examination for pain Endpoint: when pain free, running 1 mile on treadmill without pain or stiffness |
Group P achieved pain free examination sooner than group 1 (2 days vs 8 days) A greater proportion of subjects from group P (100%) recovered in less than 10 days than from group I (62%). One subject from group P and three from group I experienced pain during the 1-mile run |
Not reported |
| Schwellnus et al.,25 1992 Physiotherapy RCT, II |
17 athletes with unilateral ITBS Age in years (mean, SD): Group A: 25 (6) Group B: 29 (5) |
Both groups: 0-14 days: rest, daily stretching and twice daily ice therapy 3-14 days: ultrasound treatment Group A: day 3-14 addition of deep transverse frictions Group B: no transverse frictions |
Total pain during running (calculated as area under the pain versus time graph), using 11-point pain scale every minute during treadmill running Follow-up time points: day 0, 3, 7, 14 treadmill running |
Total pain experienced during treadmill not significantly different between the groups on any of the days Significant decrease in pain in both groups over the treatment period Significant reduction in percentage of maximum pain experienced during running in both groups over the treatment period |
Not reported |
| Schwellnus et al.,26 1991 South African Medical Journal RCT, II |
43 athletes with unilateral ITBS Age (mean, SD): Group 1: 22(5) Group 2: 24(6) Group 3: 22(2) |
All 3 groups common baseline protocol: day 0-7: rest day 3-7: identical physical therapy Group 1 (n = 13): common baseline protocol + placebo Group 2 (n = 14): common baseline protocol+ anti-inflammatory medication (Voltaren, Geigy) Group 3 (N = 16): common baseline protocol+ combined anti-inflammatory/analgesic medication (myprodol, Rio ethical) |
Daily 24-hour recall pain Treadmill running test with pain scoring every minute (calculation for the area under the curve) Total running distance Total running time Day 0, 3, 7 |
24-hour recall pain scores: decreased for all the groups over the treatment period Running test: Group 3: improved their total running time and distance from day 0 to day 7 Group 1 + 2: improved total running time and running distance from day 3 to day 7 All groups: pain decreased from day 0 to day 7 All 3 treatment modalities are effective against ITBS but physiotherapy + analgesic + anti-inflammatory medication is superior. Functional running test is more sensitive for the evaluation of the therapy progress compared with 24 recall pain scores |
Group 1: nausea, headache, fatigue, abdominal pain, dizziness Group 2: nausea, headache Group 3: nausea, headache, sore throat |
Level of evidence was reported based on the American Academy of Orthopaedic Surgeons accepted criteria.20
AMI, Allan McGavin Health Status Index; CON, control; EXP: experimental group; I, knee immobilizer; ITBS, iliotibial band syndrome; ManT, manual therapy; OS, observational study, P, phonophoresis 10% hydrocortisone; RCT, randomized clinical trial; SD, standard deviation; SWT, shockwave therapy.
Operative Management of ITBS, Clinical Outcomes, and Complications
Nine of the included articles reported the clinical outcomes following surgical therapy for ITBS (Table 2)13, 14, 15, 16, 17, 18, 19,27,28 and all of them were observational studies.
Table 2.
Studies Reporting Surgical Therapy for ITBS and the Associated Clinical Outcomes
| Study, year Type of Study, Level of Evidence |
Study Population (Participants, Age) |
ITBS Treatment Protocol | Follow-Up Assessment Tool and Timeline | Clinical Outcome | Complications |
|---|---|---|---|---|---|
| Walbron et al.,13 2018 Orthopaedics and Traumatology, Surgery and Research Case series, IV |
13 athletes (14 knees) Age in years mean, (range): 36 (19-51) |
Digastric distal ITB release from Gerdy’s tubercle: via 2 cm approach above Gerdy’s tubercle, the ITB is incised longitudinally and partially released from the tubercle | Return to preoperative level of sport rate and time Satisfaction rate Postoperative Tegner and Lysholm scores Mean follow-up time: 21 (5-61) months |
Return to preoperative level of sport rate: 100% Mean time to return to sport: 4 months (range: 1-8) Mean postoperative Tegner score: 6 (range: 4-9) Mean postoperative Lysholm: 93 (range: 80-100) Patient satisfaction rate: 85.7% were very satisfied or satisfied |
DVT: 2 patients |
| Inoue et al.,16 2018 International Journal of Sports Medicine Case series, IV |
31 runners, 34 knees Mean age in years: 20.2 |
Lengthening of the central part of the ITB by splitting it into a superficial and a deep layer, maintaining the anterior and posterior fibers immediately above the lateral epicondyle |
Time to resume sports activity Personal best times to run a 5000-m race before and after surgery 2-month postsurgery muscle strength comparison between injured and healthy side Recurrence of symptoms |
Mean time to return to sport: 5.8 weeks 17 runners completed the 5000 m race before and after surgery 13/17 runners had improved time for a 5000 m race postoperatively 2 months postsurgery: the mean extensor and flexor muscle strengths on the healthy and affected sides did not significantly differ No recurrence of ITBS through the end of competitive career |
none |
| Michels et al.,14 2009 Knee Surgery Sports Traumatology Arthroscopy Case series, IV |
36 athletes (15 females, 21 males), 38 knees with ITBS Mean age: 31.7 years (range 19-44) |
Arthroscopic debridement of the lateral synovial recess up to the bone of the lateral femoral condyle | Return to activity rate Subjective functional outcome: Drogset score Patient satisfaction using visual analogue scale 0for lowest 10 for highest satisfaction Rate of patients who would have been Mean follow-up time: 28 months Pre injury: VAS, Tegner Latest postoperative follow-up: VAS, Tegner, Lysholm, IKDC, patient satisfaction with surgical outcome Mean follow-up time: 38 months (range: 20-66) Minimum follow-up: 20 months |
3 patients lost to follow-up For the remaining 33 patients: 2 months postoperative: 74.2% were able to start slow running 3 months postoperative: 100% were able to run Drogset scores: excellent results: 28 (80%) good results: 6 patients (17.1%) fair result 1 patient (2.9%) poor results:0 patients Mean patient satisfaction: 9 (range: 6-10) |
Hematoma: 1 patient (evacuated postoperative day 4) |
| Hariri et al.,17 2009 American Journal of sports Medicine Retrospective Case series, IV |
11 recreational athletes (7 males, 4 females) Mean age in years: 32 (range: 24-41) |
Diagnostic knee arthroscopy + open ITB bursectomy | VAS mean (range): Preinjury: 8 (4-10) Postoperative: 2 (0-9) Tegner score: preinjury 6 (range: 2-9) postoperative Tegner activity score 5 (range: 3-8) no significant difference = patients on average were able to return to their preinjury level of activity IKDC postoperative mean (range): 88 range, 66-100) Lysholm score postoperatively: Excellent result: 7/11 64% Good result: 4/11 34% Fair/poor result: 0/11 0% Patient satisfaction Completely satisfied with the surgical outcome: 6/11 55% Mostly satisfied: 3/11 27% Somewhat satisfied: 2/11 18% Dissatisfied: 0/11 0% Patients said that, knowing what they know now, they would have the surgery performed again for the same problem: 9/11 82% |
Not reported | |
| Barber et al.,19 2007 Journal of Knee Surgery Case series, IV |
8 runners (4 males, 4 females) Mean age in years: 39.6 (range: 17-63) |
Z-lengthening of the ITB using a 5-cm oblique incision overlying the ITB | Postoperative evaluation Cincinnati score, Tegner score, Lysholm score, IKDC activity score, pain evaluation, return to activity Mean follow-up time: 75.6 months (range: 59-97) |
Cincinnati score mean: 82.9 (range: 55-95) Tegner score 4.4 (range: 2-7) Lysholm score was 88.6 (range: 57-100) IKDC activity score: 2.6 (range: 1-4) Complete resolution of lateral knee pain + full return to preoperative activity∗ levels: 8/8 patients, 100% ∗improvement was maintained out to 8 years postoperatively |
none |
| Drogset et al.,18 1999 Scandinavian Journal of Medicine and Science in Sports Retrospective case series, IV |
45 patients (25 females, 20 males), 49 cases (6 bilateral) Mean age in years: 27 (range: 14-46) |
27/45 patients: the posterior half of the width of the ITB was transected at the level where it passes over the most prominent part of the lateral epicondyle 17/45 patients: posterior half of the width of the ITB was transected + ITB 1/45: bursectomy |
Subjective patient self-evaluation using rating scale Excellent = no pain or weakness in the operated knee during activity and rest Good = much less pain than before the surgery Fair = little less pain than before the surgery Poor = condition uncharged or worsened Mean follow-up time: 25 months (range:2-108) |
Excellent results: 22/45 (48.9%) Good results: 16/45 (35.5%, Fair results: 6/45 (13.3%) Poor result: 1/45 (2.2%) Had the postoperative result been known beforehand, 75.6% of the patients would have been operated on again |
Minor wound infection: 1 patient Persistent pain which resolve following spine surgery: 1 patient 20/45 patients pain sensation in the area at follow-up. 2/45 patients felt weakness of the knee 1/45 patients had a swelling in the operated area for some weeks after surgery |
| Holmes et al.,27 1993 American Journal of sports Medicine Retrospective case series, IV |
25 cyclists out of a group of 61 cyclists (47 males, 14 females) | 4/25 patients: percutaneous release of TIB 21/25 patients: open surgical release with elliptical excision, Note: 3/25 patients had previous percutaneous release |
Return to sport Follow-up via phone call Routine follow-up: 1,3, 8 weeks postoperatively Mean follow-up time: 6-24 months for long term follow-up via phone |
4 patients who underwent percutaneous release of ITB: ¾ failed and required open release 21 patients underwent open release: 81% (17/21) cyclists had returned to preoperative level of sport at 8 weeks 2/21 cyclists did not resume full training for 3 months postoperatively 2/21 cyclists did not resume full training for 4 months due to lateral knee discomfort Phone follow-up:
|
Seroma: 9 patients Hematoma: 2 patients |
| Martens et al.,15 1989 American Journal of Sports Medicine Retrospective case series, IV |
19 athletes (18 males, 1 female) Mean age in years: 24.5 (range: 19-33) |
Resection of a triangular piece of the ITB from the posterior base of ITB at 30° of knee flexion | Return to sport rate Mean follow-up time: 45 months (range: 2-11 years) |
Return to sport (cycling, running, football) rate: 100% time: mean 7 weeks postoperatively |
Hematoma requiring evacuation: 1 patient |
| Noble,28 1979 British Journal of Sports Medicine Retrospective case series, IV |
9 long-distance runners (total 221 cases of ITBS seen) | Surgical release of posterior fibers of ITB | Rate of return to sport Follow-up time: 2-16 months |
Return to sport rate: 89% (8/9) | Not reported |
DVT, deep venous thrombosis; IKDC, International Knee Documentation Committee; ITB, iliotibial band; ITBS, iliotibial band syndrome; VAS, visual analog scale.
Study Population
One hundred seventy-nine athletes (mean age 27.3 years, range: 17-53) received conservative therapy for ITBS and 200 athletes (mean age 30.1 years, 14-63) underwent surgical treatment. The majority of treated athletes who participated primarily in one sport activity were runners (247/379, 65%), followed by cyclists 70/379, 18.4%) (Fig 2). Many of the included studies failed to report a detailed distribution of sports among the participants.
Fig 2.
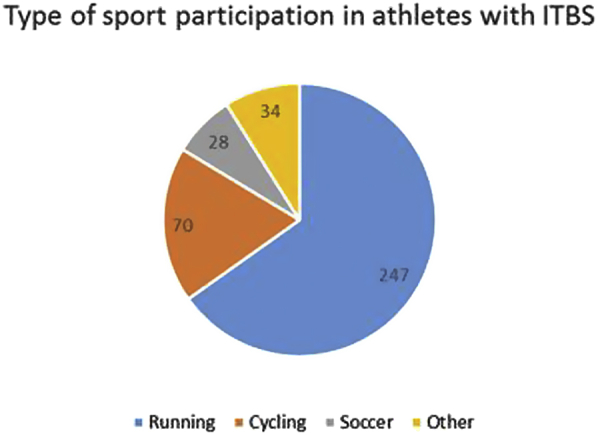
Number of athletes with ITBS who were reported to participate primarily in one sport among the included studies. (ITBS, iliotibial band syndrome.)
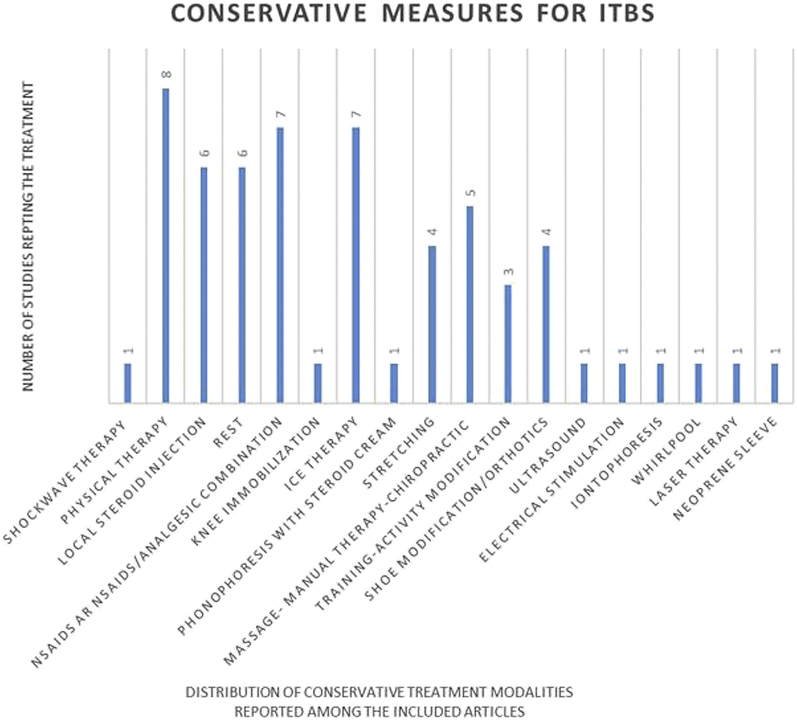
Conservative Measures Reported for the Treatment of ITBS
Physical therapy (8/15 studies, 53.3%) was the most commonly reported conservative treatment for ITBS (Fig 3), followed by nonsteroidal anti-inflammatory drugs (7/15, 46.6%), ice therapy (7/15, 46.6%), and local steroid injections (6/15, 40%), rest (6/15, 40%). For patients who underwent surgical treatment, the duration of conservative therapy was reported to range from 3 to 6 months before the procedure.
Fig 3.
Distribution of the conservative therapies for ITBS used among the included studies. (ITBS, iliotibial band syndrome.)
Reported Signs, Symptoms, and Physical Examination Findings in Patients With ITBS Who Required Surgical Treatment
Six of the 9 articles (67%) that reported the outcomes following surgical therapy for ITBS described the patient’s preoperative signs and symptoms and/or physical examination findings.15, 16, 17, 18, 19,27,28 Symptoms reported by the patients with ITBS who required surgical management included lateral knee pain that was exacerbated by activity; pain above the lateral condyle; lateral knee pain with running; lateral knee pain located around the distal iliotibial band that was exacerbated by running or other repetitive activity; atraumatic lateral knee pain related to cycling; lateral knee pain radiating proximally or distally; intermittent or progressively worse lateral knee pain during activity; lateral knee pain with walking; acute onset lateral knee pain unrelated to strenuous activity; lateral knee pain aggravated by downhill running and relieved by walking with the knee held in extension; pain just above the lateral knee joint line that might radiate below the knee; and burning or stabbing pain over the lateral knee with running.
Physical examination findings reported by patients who underwent surgical therapy were tenderness to palpation over the lateral femoral condyle; positive Noble compression test; positive Ober’s test; pain with palpation of the lateral femoral condyle while extending the knee from 90° to 0°; snapping of the distal ITB during a full knee range of motion; maximum pain at 30 degrees of knee flexion while pressure is applied on the lateral femoral condyle during active knee flexion-extension motion (compression test); crepitus over the lateral knee; lateral knee swelling.
Reported Imaging Tests and Findings in Patients With ITBS Resistant to Conservative Therapy
In 4 of the 9 studies (44.4%) that reported the outcomes of surgical therapy for ITBS, imaging testing was performed as part of the preoperative patient evaluation. Knee radiographs, ultrasound, and/or magnetic resonance imaging (MRI) were the 3 tests reported to diagnose potential ITB abnormalities and to exclude additional pathology of the knee.14, 15, 16, 17 One patient with clinical diagnosis of ITBS was reported as presenting with an “aberrant picture” around the lateral femoral condyle on ultrasound.15 Hariri et al.17 and performed preoperative knee MRI on 5 patients with ITBS, and they found a meniscal tear in 3 patients, whereas 1 patient had a Baker cyst. Michels et al.,14 however, reported negative preoperative MRI findings in surgical candidates for ITBS, although they addressed some intra-articular lesions that were seen during a diagnostic knee arthroscopy.
Knee Arthroscopy and Associated Lesions
Knee arthroscopy was the only additional procedure reported to be performed while surgically treating ITBS (5/9 studies, 55.5%). Knee arthroscopy preceded the ITBS procedure in all cases, and it was performed for diagnostic and/or therapeutic purposes.14,15,17, 18, 19 Michels et al.14 used a standard knee arthroscopic approach (anteromedial, anterolateral, superolateral portals) to perform a diagnostic knee arthroscopy and to debride the lateral synovial recess to address the ITBS. The authors reported meniscal pathology, which was not visible on preoperative MRI but required treatment, in 2 patients, whereas another patient had a calcified intra-articular loose body that was trapped in the lateral synovial recess and it was resected arthroscopically. Hariri et al.17 also performed a concomitant diagnostic knee arthroscopy and they found complete or partially imperforated suprapatellar plica with adhesions in the suprapatellar pouch (2 patients), synovitis and/or adhesions on the suprapatellar pouch (4 patients), infrapatellar plica (5 patients) medial shelf plicae (2 patents), and adhesions in the anterior interval. All plicae-adhesions were released and the synovitis was debrided.
Barber et al.19 performed the following arthroscopic knee procedures before the ITB release: chondroplasty (patella,1 patient; medial femoral condyle and patella, 2 patients; medial femoral condyle, 1 patient), medial meniscectomy (2 patients), lateral meniscectomy (2 patients), and loose body removal (1 patient). Three of 45 patients in the study of Drogset et al.18 underwent knee arthroscopy at the same time as ITB release, but the findings were not reported. Lastly, 2 of 23 patients in the study of Martens et al.15 underwent knee arthroscopy for suspected lateral meniscal pathology.
Postoperative Activity Guidelines and Deep Venous Thrombosis Prophylaxis Following Surgery for ITBS
All but 1 (8/9, 88.8%) of the included articles reporting surgical therapy of ITBS, provided information about the postoperative activity modification–rehabilitation protocol (Table 3), but only 1 study (1/9, 11.1%) reported whether or not antithrombotic prophylaxis was recommended.
Table 3.
Activity Modification and Rehabilitation Guidelines Reported Following Operative Therapy for Iliotibial Band Syndrome
| Study | Postoperative Guidelines |
|---|---|
| Walbron et al.,13 | Immediate full weight-bearing with forearm crutches |
| Inoue et al.16 | Knee range of motion + muscle strengthening exercises initiated “soon” after surgery |
| Full weight bearing → start 1 week after surgery | |
| Walking → start 2 weeks after surgery | |
| Jogging → start 3 weeks after surgery | |
| Michels et al.14 | Surgical drain removed 24 hours’ postoperatively |
| Early range of motion exercises + full weight bearing promoted | |
| Slow running starts at 2 months postoperatively | |
| Hariri et al.17 | Weight bearing as tolerated, bilateral axillary crutches |
| Postoperative week 1-2: ice, compression, high-voltage electrical stimulation weeks, gentle massage of iliotibial band with progression to stretching | |
| Passive knee and hip range of motion → start postoperative day 1 | |
| Full knee extension → postoperative day 3 | |
| Full knee and hip flexion → end of postoperative week 2 | |
| Patellofemoral joint mobilization, emphasis on medial glide of patella | |
| Progressive resistance exercises (quadriceps, hamstrings, hip abductors) start: week 1 to week 4 | |
| Week 8: reevaluation by surgeon to clear for running, cycling other sports as tolerated | |
| Full return to sport: postoperative week 12-14 | |
| Barber et al.19 | Weight bearing as tolerated with a gradual increase in motion |
| Physical therapy → start week 2 | |
| Return to sport milestones: incision healed and no tenderness to palpation | |
| Running → start 6 weeks postoperative | |
| Pivoting → start 8 weeks postoperative | |
| Drogset et al.18 | Weight bearing gradually allowed at postoperative week 2 |
| Holmes et al.27 | Indoor riding without resistance for 15 minutes → try postoperative day 3 |
| Able to ride indoors for 30 minutes without discomfort → start outdoor riding | |
| Gradual resumption of mileage and resistance, based on preoperative levels | |
| Hill work → start 4-6 weeks postoperatively | |
| Martens et al.15 | Regain sports activity postoperative week 3-4 |
Clinical Outcomes
For studies examining the clinical outcomes following the nonoperative management of ITBS, the mean follow-up time was 2 months (range: 3 days to 6 months). However, a meta-analysis was not performed due to significant data heterogeneity. The most commonly reported variable used for follow-up in studies that reported the results following conservative therapy of ITBS, was pain assessment during a treadmill running test (5/6 studies, 83.%).21,22,24, 25, 26 Four of these studies evaluated the pain every minute during the treadmill test using an 11-point visual analog scale and by calculating the area under the curve of a pain–time graph.21,22,25,26 All studies reported significant improvement in pain at follow-up, which was no longer than 6 months. Regarding the objective outcome evaluation tools used, Beers et al.23 measured the muscle strength with a handheld dynamometer to assess the effectiveness of an exercise program along with the pain evaluation.
For studies examining the clinical outcomes following operative management of ITBS (Table 2), the mean follow-up time was 33.5 months (range: 2 months to 11 years), which was significantly longer than the follow-up time reported in studies examining the results of conservative therapy (Table 1, P < .05). There was significant variability in the surgical techniques and outcome variables used to assess the results of the operative treatment for ITBS, and meta-analysis was not performed. The most commonly reported variable for postoperative evaluation of the athletes was the rate of return to sport (7/9 studies, 77.7%),13, 14, 15, 16,19,27,28 which ranged from 81% to 100%. As mentioned previously, although most of the included studies reported the composition of the study population based on the sport, the reported return to sport rate was not sport-specific. Consequently, we were unable to examine whether the rate of return to sport following surgical therapy for ITBS varies between the individual sports.
All patients who underwent surgical therapy for ITBS initially underwent a 3- to 6-month trial of conservative therapy (9/9 studies, 100%).13, 14, 15, 16, 17, 18, 19,27,28 Due to significant variability among the subjective and objective outcomes measures reported across the studies, a direct comparison of the effectiveness of conservative versus surgical therapy for ITBS could not be made.
Discussion
The most important finding of this study was that, at short-term follow-up time, conservative therapy for distal ITBS appeared to reduce pain, and surgical therapy (open, arthroscopic) was effective in returning the athletes to sport at a rate between 81% and 100%. However, there was severe literature inconsistency and low quality of evidence on the outcomes following both the nonoperative and operative management of ITBS in active individuals, including non-running athletes A formal comparison between the clinical results of surgical versus non-surgical management of ITBS was not conducted due to significant data heterogeneity.
Previous systematic reviews have examined the biomechanical factors, diagnosis and treatment of ITBS in runners.1,4,12 This current study focused on the clinical outcomes following the operative versus nonoperative management of ITBS, regardless of the activity level or type of sport. However, we found all subjects in the included articles to be recreational or high-level athletes who participated in sports involving repetitive knee flexion–extension, such as runners (65%), bikers (18.4%), and soccer players (7.3%). Interestingly, a portion of the athletes studied in this review participated in other sports, including skiing, rugby, baseball, golf, volleyball, swimming, lacrosse, gym athletics, Pilates, and yoga. The type of sport activity was inconsistently reported across the studies which constituted further sport-specific analysis impossible. Since ITBS is considered an overuse injury in physically active individuals, future research should focus on consistently describing the type and level of sport participation of research subjects, in order to identify sport-specific risk factors for the development of ITBS and develop appropriate treatment protocols and outcome evaluation tools. For example, increased evidence exists on the role of ITB in rotational knee stability through the Kaplan fibers, and therefore, repetitive knee flexion–extension might not be the only biomechanical mechanism implicated in the generation of ITBS.29 Based on that, pivoting sports might pose the ITB at risk for overuse injuries, including ITBS.
As shown in Table 1, multiple conservative therapies have been described for the management of ITBS in active patients, which were reported to be effective in the short-term (average follow-up time was 6 months) reduction of pain. Unfortunately, the amount and quality of the evidence available were not sufficient to support the overall efficacy of these treatments. This conclusion is in accordance with previous reports.4,12 Although the majority of the studies reporting the outcomes of conservative therapy for ITBS were RCTs,21,22,24, 25, 26 they were of low quality. The last was mainly due to small population size, whereas the follow-up was short-term (maximum 6 months). In addition, there was an overall lack of information regarding fundamental return-to-sport variables, which should include not only the rate of return to sport, but also the timing and level of competition upon return. As mentioned before, the follow-up variables (outcome measures, time at follow-up) reported in this group of studies were heterogenic and meta-analysis was not feasible.
The principles of surgical management for distal ITBS are based on the resection of the inflamed part of the distal ITB to reduce the athlete’s pain, but also prevent the ITBS from rubbing against the bone. However, since the distal ITB has been shown to contribute to the rotational stability of the knee, the surgeon should be careful with the amount of tissue excised in order to avoid compromising the function of the knee joint postoperatively.4,30 Multiple surgical techniques have been described for the treatment of distal ITBS and are presented in Table 2. All articles reporting the clinical outcomes following surgical treatment of ITBS were case series studies, and the majority of them were retrospective in design (5/9, 55.5%).15,17,18,27,28 Only in one study done by Michels et al.14 were patients treated arthroscopically for TIBS, while the rest of the included studies involved an open surgical technique.
Reported benefits of an arthroscopic procedure to address distal ITBS include the ability to perform knee arthroscopy to diagnose and treat other intra-articular knee pathology (for example meniscal tears); less-invasive surgical intervention compared with an open technique; but also the ability to resect only the inflamed fibers of the ITBS and the associated fat, without significantly violating the distal attachment of ITB to the femur, which might contribute to postoperative knee instability.14,30 There is an expansion of arthroscopic techniques reported to address ITBS, but they were excluded from our systematic review due to failure to report patient outcomes.30, 31, 32 There is an expansion of arthroscopic techniques reported to address ITBS, but they were excluded from our systematic review due to failure to report patient outcomes 30, 31, 32 The comparison of the clinical outcomes and safety profile between open and arthroscopic surgical techniques to address ITBS is a subject of future investigation. In contrast to the group of studies reporting the outcomes following conservative management of ITBS, the return to sport rate, timing, and level of competition upon return was more consistently reported in studies that examined the effectiveness of surgical therapy. Unfortunately, different subjective and objective evaluation tools were used when reporting the outcomes of surgical therapy, and therefore a comparison between the effectiveness of the reported techniques could not be made. However, at short-term follow-up, the surgical management of ITBS in patients who had previously undergone conservative therapy appears to be a safe and effective method to address the patients’ symptoms and allow for return to sport.
It is worth noting that, based on our results, all patients who underwent surgery to address ITBS had previously not responded to conservative treatment. We did not identify any study in which surgery was offered as first-line therapy for ITBS. Without sufficient evidence on the efficacy of conservative therapy, it is unknown if patients with ITBS would miss less time from participation in their sport if surgery was initially performed without the interval of conservative treatment. In general, our impression was that the management of ITBS remains “empiric” among the health care providers, including orthopaedic surgeons. In some of the included studies, preoperative knee imaging (MRI, radiograph, ultrasound) was performed to exclude additional knee pathology, whereas some surgeons performed a diagnostic-therapeutic knee arthroscopy, concomitantly with the ITBS procedure. Based on the aforementioned considerations, the generalizability of our results is limited. However, this overview could potentially serve as a start point toward the establishment of clinical guidelines for the diagnosis and treatment of ITBS. There is need for higher-quality research with not only well-designed RCTs, but also prospective comparative studies to establish an evidence-based approach to this condition.
Limitations
This study is limited by several factors, mostly related to the low quality of the existing literature and significant study heterogeneity. Although RCTs have been conducted to evaluate the effectiveness of conservative therapy for ITBS, the validity of their results is compromised by the extremely short follow-up time (maximum 6 months). We did not set an exclusion criterion based on the minimum follow-up time in nonoperative therapies for distal ITBS, since numerous studies did not clearly state the mean follow-up time for the entire study population. In these articles, we recorded the minimum follow-up time reported, which usually referred to a subgroup of the included patients. There was significant variability in outcome measures used to captivate the clinical progress of patients following operative and nonoperative management for ITBS including multiple subjective and objective assessment tools that did not allow for any comparison or meta-analysis of the outcomes. The last was a determining factor toward examining the hypothesis of this review but there was insufficient evidence to answer our question. Furthermore, none of outcome scores or evaluation tools used in the included articles has been validated for patients with ITBS, which limits the external validity of the individual studies.
Conclusions
Based on the current literature and at a maximum follow-up time of 6 months, conservative therapy can effectively reduce ITBS symptoms in athletes. Multiple surgical options exist for athletes who fail the nonoperative measures, with a reported return to sport rate between 81% and 100%.
Acknowledgments
The authors acknowledge The Cappo Family Research Fund.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.E.W. reports other from Arthrex, Smith & Nephew, Stryker, and Micromed, outside the submitted work. B.R.W. reports other from Vericel, Kaliber Al Vivorte, and Arthrex, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Appendix
Appendix Table 1.
Quality Assessment of Randomized Clinical Trials using the Cochrane Risk of Bias Tool for Randomized Clinical Trials
| Study, Year | Risk of Bias (High, Low, Unclear) |
Overall Study Quality (Good, Fair, Poor) | ||||||
|---|---|---|---|---|---|---|---|---|
| Random Sequence Generation | Allocation Concealment | Selective Reporting | Other Bias | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | ||
| Weckstrom et al., 2016 | Low | Low | Low | Low | Low | Low | Low | Good |
| Gunter et al., 2004 | Unclear | Unclear | Unclear | Low | Low | Low | Low | Poor |
| Bischoff et al., 1995 | Unclear | High | High | Unclear | High | Low | Unclear | Poor |
| Schwellnus et al., 1992 | Unclear | Unclear | Low | Low | Low | Low | Low | Fair |
| Schwellnus et al., 1991 | Unclear | Unclear | Unclear | Low | Low | Low | Low | Fair |
Appendix Table 2.
Quality Assessment of Observational Studies Using the MINORS Criteria
| Study, Year | MINORS Criteria |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Collection of Data | Endpoints Appropriate to The Aim of Study | Unbiased Assessment of Study Endpoint | Appropriate Follow-up Period | Loss of Follow-up Less Than 5% | Prospective Calculation of Study Size | Adequate Control Group | Contemporary Group | Baseline Equivalence of Groups | Adequate Statistical Analysis | MINORS Score |
|
| Walbron et al., 2018 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Inoue et al., 2018 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Michels et al., 2009 | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| Hariri et al., 2009 | 1 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 11 |
| Barber et al., 2007 | 2 | 2 | 2 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 10 |
| Drogset et al., 1999 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1 | 9 |
| Holmes et al., 1993 | 2 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 5 |
| Martens et al., 1989 | 2 | 2 | 2 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 9 |
| Noble et al., 1979 | 2 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 7 |
| Beer et al., 2008 | 2 | 2 | 2 | 1 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | 1 | 13 |
Each item is scored as 0 = not reported, 1 = reported but inadequate 2 = reported and adequate. Ideal score for comparative studies = 24; ideal score for non-comparative studies = 16.
MINORS, Methodological Index for Non-Randomized Studies.
Supplementary Data
References
- 1.Aderem J., Louw Q.A. Biomechanical risk factors associated with iliotibial band syndrome in runners: A systematic review. BMC Musculoskel Disord. 2015;16:356. doi: 10.1186/s12891-015-0808-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farrell K.C., Reisinger K.D., Tillman M.D. Force and repetition in cycling: Possible implications for iliotibial band friction syndrome. Knee. 2003;10:103–109. doi: 10.1016/s0968-0160(02)00090-x. [DOI] [PubMed] [Google Scholar]
- 3.Sutker A.N., Barber F.A., Jackson D.W., Pagliano J.W. Iliotibial band syndrome in distance runners. Sports Med. 1985;2:447–451. doi: 10.2165/00007256-198502060-00005. [DOI] [PubMed] [Google Scholar]
- 4.Ellis R., Hing W., Reid D. Iliotibial band friction syndrome—a systematic review. Man Ther. 2007;12:200–208. doi: 10.1016/j.math.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Fairclough J., Hayashi K., Toumi H., et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: Implications for understanding iliotibial band syndrome. J Anat. 2006;208:309–316. doi: 10.1111/j.1469-7580.2006.00531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairclough J., Hayashi K., Toumi H., et al. Is iliotibial band syndrome really a friction syndrome? J Sci Med Sports. 2007;10:74–76. doi: 10.1016/j.jsams.2006.05.017. discussion 77-78. [DOI] [PubMed] [Google Scholar]
- 7.Gose J.C., Schweizer P. Iliotibial band tightness. J Sports Phys Ther. 1989;10:399–407. doi: 10.2519/jospt.1989.10.10.399. [DOI] [PubMed] [Google Scholar]
- 8.Pegrum J., Self A., Hall N. Iliotibial band syndrome. BMJ. 2019;364:l980. doi: 10.1136/bmj.l980. [DOI] [PubMed] [Google Scholar]
- 9.Nemeth W.C., Sanders B.L. The lateral synovial recess of the knee: Anatomy and role in chronic Iliotibial band friction syndrome. Arthroscopy. 1996;12:574–580. doi: 10.1016/s0749-8063(96)90197-8. [DOI] [PubMed] [Google Scholar]
- 10.Stickley C.D., Presuto M.M., Radzak K.N., Bourbeau C.M., Hetzler R.K. Dynamic varus and the development of iliotibial band syndrome. J Athl Train. 2018;53:128–134. doi: 10.4085/1062-6050-122-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hadeed A., Tapscott D.C., Iliotibial band friction syndrome . StatPearls Publishing LLC; Treasure Island (FL): 2019. StatPearls. [PubMed] [Google Scholar]
- 12.van der Worp M.P., van der Horst N., de Wijer A., Backx F.J., Nijhuis-van der Sanden M.W. Iliotibial band syndrome in runners: A systematic review. Sports Med. 2012;42:969–992. doi: 10.2165/11635400-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Walbron P., Jacquot A., Geoffroy J.M., Sirveaux F., Mole D. Iliotibial band friction syndrome: An original technique of digastric release of the iliotibial band from Gerdy's tubercle. Orthop Traum Surg Res. 2018;104:1209–1213. doi: 10.1016/j.otsr.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 14.Michels F., Jambou S., Allard M., Bousquet V., Colombet P., de Lavigne C. An arthroscopic technique to treat the iliotibial band syndrome. Knee Surg Sports Traumatol Arthrosc. 2009;17:233–236. doi: 10.1007/s00167-008-0660-5. [DOI] [PubMed] [Google Scholar]
- 15.Martens M., Libbrecht P., Burssens A. Surgical treatment of the iliotibial band friction syndrome. Am J Sports Med. 1989;17:651–654. doi: 10.1177/036354658901700511. [DOI] [PubMed] [Google Scholar]
- 16.Inoue H., Hara K., Arai Y., et al. Outcome of low-invasive local split-thickness lengthening for iliotibial band friction syndrome. Int J Sports Med. 2018;39:232–236. doi: 10.1055/s-0043-122152. [DOI] [PubMed] [Google Scholar]
- 17.Hariri S., Savidge E.T., Reinold M.M., Zachazewski J., Gill T.J. Treatment of recalcitrant iliotibial band friction syndrome with open iliotibial band bursectomy: Indications, technique, and clinical outcomes. Am J Sports Med. 2009;37:1417–1424. doi: 10.1177/0363546509332039. [DOI] [PubMed] [Google Scholar]
- 18.Drogset J.O., Rossvoll I., Grontvedt T. Surgical treatment of iliotibial band friction syndrome. A retrospective study of 45 patients. Scand J Med Sci Sports. 1999;9:296–298. doi: 10.1111/j.1600-0838.1999.tb00249.x. [DOI] [PubMed] [Google Scholar]
- 19.Barber F.A., Boothby M.H., Troop R.L. Z-plasty lengthening for iliotibial band friction syndrome. J Knee Surg. 2007;20:281–284. doi: 10.1055/s-0030-1248058. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt A.H., Zhao G., Turkelson C. Levels of evidence at the AAOS meeting: Can authors rate their own submissions, and do other raters agree? J Bone Joint Surg Am. 2009;91:867–873. doi: 10.2106/JBJS.G.01233. [DOI] [PubMed] [Google Scholar]
- 21.Weckstrom K., Soderstrom J. Radial extracorporeal shockwave therapy compared with manual therapy in runners with iliotibial band syndrome. J Back Musculoskelet Rehabil. 2016;29:161–170. doi: 10.3233/BMR-150612. [DOI] [PubMed] [Google Scholar]
- 22.Gunter P., Schwellnus M.P. Local corticosteroid injection in iliotibial band friction syndrome in runners: A randomised controlled trial. Br J Sports Med. 2004;38:269–272. doi: 10.1136/bjsm.2003.000283. discussion 272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beers A., Ryan M., Kasubuchi Z., Fraser S., Taunton J.E. Effects of multi-modal physiotherapy, including hip abductor strengthening, in patients with iliotibial band friction syndrome. Phys Can. 2008;60:180–188. doi: 10.3138/physio.60.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bischoff C., Prusaczyk W.K., Sopchick T.L., Pratt N.C., Goforth H.W., Jr. Comparison of phonophoresis and knee immobilization in treating iliotibial band syndrome. Res Sports Med. 1995;6:1–6. [Google Scholar]
- 25.Schwellnus M., Mackintosh L., Mee J. Deep transverse frictions in the treatment of lliotibial band friction syndrome in athletes: A clinical trial. Physiotherapy. 1992;78:564–568. [Google Scholar]
- 26.Schwellnus M.P., Theunissen L., Noakes T.D., Reinach S.G. Anti-inflammatory and combined anti-inflammatory/analgesic medication in the early management of iliotibial band friction syndrome. A clinical trial. S Afr Med. 1991;79:602–606. [PubMed] [Google Scholar]
- 27.Holmes J.C., Pruitt A.L., Whalen N.J. Iliotibial band syndrome in cyclists. Am J Sports Med. 1993;21:419–424. doi: 10.1177/036354659302100316. [DOI] [PubMed] [Google Scholar]
- 28.Noble C.A. The treatment of iliotibial band friction syndrome. Br J Sports Med. 1979;13:51–54. doi: 10.1136/bjsm.13.2.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Godin J.A., Chahla J., Moatshe G., et al. A comprehensive reanalysis of the distal iliotibial band: Quantitative anatomy, radiographic markers, and biomechanical properties. Am J Sports Med. 2017;45:2595–2603. doi: 10.1177/0363546517707961. [DOI] [PubMed] [Google Scholar]
- 30.Cowden C.H., 3rd, Barber F.A. Arthroscopic treatment of iliotibial band syndrome. Arthrosc Tech. 2014;3:e57–e60. doi: 10.1016/j.eats.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pierce T.P., Mease S.J., Issa K., Festa A., McInerney V.K., Scillia A.J. Iliotibial band lengthening: An arthroscopic surgical technique. Arthrosc Tech. 2017;6:e785–e789. doi: 10.1016/j.eats.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richards D.P., Alan Barber F., Troop R.L. Iliotibial band Z-lengthening. Arthroscopy. 2003;19:326–329. doi: 10.1053/jars.2003.50081. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.