Abstract
Body dissatisfaction is common in adolescence and associated with negative outcomes (e.g., eating disorders). We identified common individual trajectories of body dissatisfaction from mid-adolescence to adulthood, and predictors of divergent patterns. Participants were 1,455 individuals from four waves of Project EAT (Eating and Activity in Teens and Young Adults), a population-based, 15-year longitudinal study. Aggregate body dissatisfaction increased over 15 years, which was largely attributable to increases in weight. Growth mixture modeling identified four common patterns of body dissatisfaction, revealing nearly 95% of individuals experienced relatively stable body dissatisfaction from adolescence through adulthood. Baseline depression, self-esteem, parent communication/caring, peer dieting, and weight-based teasing predicted differing trajectories. Body dissatisfaction appears largely stable from mid-adolescence onward. There may be a critical period for body image development during childhood/early adolescence. Clinicians should intervene upon body dissatisfaction before it becomes chronic, and target depression, self-esteem, parent/child connectedness, and responses to teasing and peer dieting.
Keywords: body dissatisfaction, trajectories, adolescence, longitudinal, population-based
Body dissatisfaction is highly prevalent among adolescents; studies have found that 24% – 46% of adolescent girls and 12% – 26% of adolescent boys report marked dissatisfaction with their bodies (Bucchianeri et al., 2016; Neumark-Sztainer, Goeden, Story, & Wall, 2004; Presnell, Bearman, & Stice, 2004; Stice & Whitenton, 2002). Of concern, these fairly common attitudes are associated with a variety of negative outcomes. Body dissatisfaction prospectively predicts disordered eating (Neumark-Sztainer, Paxton, Hannan, Haines, & Story, 2006; Stice & Shaw, 2001) and diagnosed eating disorders (Rohde, Stice, & Marti, 2015; Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004). Body dissatisfaction also predicts overweight/obesity (Haines, Neumark-Sztainer, Wall, & Story, 2007; Loth, Watts, van den Berg, & Neumark-Sztainer, 2015; van den Berg & Neumark-Sztainer, 2007). In addition, body dissatisfaction longitudinally predicts other psychological concerns, such as low self-esteem (Paxton, Neumark-Sztainer, Hannan, & Eisenberg, 2006), depressive symptoms (Holsen, Kraft, & Roysamb, 2001), and suicidal ideation (Kim & Kim, 2009), and is concurrently associated with impairment in health-related and subjective quality of life (Mond et al., 2013) and functional impairment in domains of work, home, and social relationships (Mond & Hay, 2007).
Given the distress and impairment associated with body dissatisfaction, it is important to understand how prevalence of these attitudes varies throughout the lifespan, in order to know when to most optimally intervene. Most studies examining body dissatisfaction have followed individuals through adolescence and young adulthood, finding that aggregate levels of body dissatisfaction increase throughout adolescence (mid-teens; Johnson & Wardle, 2005; Rodgers, McLean, Marques, Dunstan, & Paxton, 2016) as well as from adolescence to young adulthood (mid-twenties) for both males and females (Eisenberg, Neumark-Sztainer, & Paxton, 2006; Quick, Eisenberg, Bucchianeri, & Neumark-Sztainer, 2013). However, little is known about how body dissatisfaction shifts after early adulthood, as individuals enter their thirties. The mid-twenties and mid-thirties are distinct developmental stages, with shifting life roles and social relationships, different career responsibilities, and changes in body shape and weight as age increases (Arnett, 2000; Tiggemann & Lynch, 2001; Whitbourne & Skultety, 2002). Few studies have examined changes in body dissatisfaction during adulthood developmental periods, and results from this literature are mixed. Whereas some studies have shown body dissatisfaction to increase with age as men and women enter adulthood (Neumark-Sztainer et al., 2018; Quick et al., 2013), others have found that women become more accepting and satisfied with their bodies over time (Heatherton, Mahamedi, Striepe, Field, & Keel, 1997; Keel, Baxter, Heatherton, & Joiner, 2007). These mixed findings suggest that there may be heterogeneity within lifetime body dissatisfaction patterns.
Indeed, the majority of studies conducted to date have examined composite time courses in body dissatisfaction, as well as predictors of population-level body dissatisfaction, which do not permit detection of heterogeneity in the trajectories of body dissatisfaction. Although these approaches can be valuable in examining population trends over time, collapsing disparate body dissatisfaction patterns could mask subgroup trends. For example, stable low and high (or increasing and decreasing) patterns of body dissatisfaction among subgroups of the population, when combined, could generate population-level trajectories demonstrating stable average levels of body dissatisfaction. Similarly, variables that predict population-level averages of body dissatisfaction may not predict differing individual body dissatisfaction trajectories. Latent modeling of time course heterogeneity has the potential to complement population-level statistics by empirically identifying common trends to body dissatisfaction over time. Indeed, these methods have been applied to identify subgroups of individuals with increasing, decreasing, or stable eating disorder symptoms and behaviors through early adolescence and young adulthood, who have been found to demonstrate distinct patterns on transdiagnostic (e.g., negative urgency, depressive symptoms) and eating-disorder specific risk factors (e.g., thinness expectancies; Allen, Crosby, Oddy, & Byrne, 2013; Pearson & Smith, 2015). A recent study also derived trajectories of body dissatisfaction among girls throughout early adolescence, finding common patterns of high, moderate-increasing, moderate-decreasing, and low body dissatisfaction (Rodgers et al., 2016). However, to the best of our knowledge, no research to date has used these techniques to examine, at an individual rather than aggregate level, whether there are different common time courses of body dissatisfaction from adolescence through adulthood. Such latent trajectory analyses can provide important information about whether different individuals experience peak levels of body dissatisfaction at different time points, and can thereby inform key intervention points.
Additionally, there has been little research to identify risk and protective factors that predict different patterns of body dissatisfaction. Previous research has examined body dissatisfaction over 5-year (Eisenberg et al., 2006) and 10-year (Quick et al., 2013) periods utilizing data from the first three waves of the data set being used in the current study, Project EAT (Eating and Activity in Teens and Young Adults), a 15-year longitudinal study examining eating, weight, and psychological variables among adolescents and young adults. Results from these analyses have shown that, at a population level, lower self-esteem and greater body dissatisfaction, depression, weight teasing and pressure to diet, and body mass index (BMI) during adolescence predict increases in body dissatisfaction over time. These predictors have generally been examined independently, although as a linear combination, these variables (along with demographics) accounted for approximately 27% of the variance in body dissatisfaction at 10-year follow-up. However, it is not clear whether these same risk factors would predict specific patterns of body dissatisfaction (e.g., persistent or later onset of body dissatisfaction), in addition to the presence or severity of body dissatisfaction, in adulthood. Identifying predictors of distinct trajectories may be particularly important if they assist in identifying which individuals might go on to follow more clinically problematic (e.g., chronic or increasing body dissatisfaction) or less concerning (e.g., consistently low or decreasing body dissatisfaction) patterns among individuals who initially present with similar levels of body dissatisfaction.
Therefore, the current study aimed to build upon these previous findings by empirically deriving common individual trajectories of body dissatisfaction over a 15-year period from early to middle adolescence and ending in adulthood, using data from Project EAT-I, II, III, and IV. Additionally, this study examined whether particular risk and protective factors (e.g., social and individual variables) predicted these different trajectories of body dissatisfaction. Although we did not have specific hypotheses about the exact nature of individual trajectories, based on previous research (Rodgers et al., 2016), we did expect that initially high or low levels of body dissatisfaction would be largely maintained. Similarly, we hypothesized that psychological and environmental variables, including greater depression, parent dieting, and peer dieting, as well as less self-esteem and parent communication/caring would predict more severe trajectories. This knowledge of how body dissatisfaction varies across the lifespan for different individuals, as well as what factors in adolescence predict the problematic trajectories (e.g., chronic or increasing body dissatisfaction), can aid in increasing specificity for the timing and targets of prevention and intervention efforts for various mental health concerns.
Method
Study Design and Population
The current study used data from four waves of Project EAT. The sample for the current study included 1,455 participants (847 women, 589 men) who responded at each of the four waves (in middle/high school, 5, 10, and 15 years later). Participants were originally recruited in 1998 from middle schools and high schools in the Minneapolis/St. Paul metropolitan area (N=4,746; mean age=14.8 ± 1.6) where they completed in-person surveys and anthropometric measures as part of a cross-sectional study (Project EAT-I; Neumark-Sztainer et al., 2002a; Neumark-Sztainer, Story, Hannan, & Croll, 2002b). Given growing research interest in the eating- and weight-related health of young people, a decision was made to follow participants from the original sample. Due to privacy, this follow-up was restricted to only those who had provided sufficient contact information at Project EAT-I (N=3,672 of 4,746, 77%).
Follow-up assessments were conducted at five-year intervals by sending mailed invitations to all baseline participants with usable contact information at Project EAT-II (Time 2; 2003–04; N=2,516; mean age=19.4 ± 1.7) and Project EAT-III (Time 3; 2008–09; N=2,287; mean age=25.3 ± 1.7), with response rates per time point ranging from 60 – 70%. For Project EAT-IV, invitations were sent only to participants who had completed surveys at either or both Times 2 and 3 (Time 4; 2015–16; N=1,830; mean age=31.0 ± 1.6), and accordingly responders represent only 50% of those with usable contact information from baseline. Additional details of the methodology have previously been published (Haynos et al., 2018; Neumark-Sztainer, Wall, Eisenberg, Story, & Hannan, 2006; Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011). All study protocols were approved by the University of Minnesota’s Institutional Review Board Human Subjects Committee. Of relevance to the current analysis using all four time points, Time 4 surveys were completed by 1455 of the 1902 participants who had previously completed surveys at Time 1, Time 2, and Time 3 (76.5%). Attrition from the cohort over time has not occurred completely at random and thus to account for missing data, we used previously developed non-response weights for longitudinal analyses of Project EAT I-IV (Puhl et al., 2017) which account for differential attrition (see statistical analysis section) and provide estimates representative of the original Project EAT I sample. After weighting, there were no significant differences between the analytic sample and the Time 1 full sample on these Time 1 variables (ps>0.20). In the current weighted sample, participants were 46.9% White, 19.0% African American, 19.2% Asian, 5.2% Hispanic, 3.5% Native American, and 6.2% Mixed or other/race ethnicity. Participants were of low (16.8%), middle-low (18.5%), middle (25.6%), middle-high (22.3%), and high (12.5%) socioeconomic status.
Survey Development
The original Project EAT-I survey was developed based upon focus groups with adolescents (Neumark-Sztainer, Story, Perry, & Casey, 1999), an extensive literature review, content reviews by multidisciplinary experts and adolescents, and pilot testing. To allow for longitudinal comparisons, main items from this baseline survey and earlier survey waves (Projects EAT-II and EAT-III) were retained on the Project EAT-IV survey. Test-retest reliability was examined in a subsample of 103 participants who took the EAT-IV survey twice over a period of one to four weeks.
Measures
Outcome Variable.
Body dissatisfaction was assessed with a 10-item scale adapted from the Body Shape Satisfaction Scale (Pingitore, Spring, & Garfield, 1997). Participants responded to items asking about their satisfaction with various body parts (e.g., “How satisfied are you with your…height, weight, body shape, waist, hips, thighs, stomach, face, body build, shoulders”?) on a scale from 1 (very dissatisfied) to 5 (very satisfied), with no labels for options 2, 3, or 4. Items were reverse scored and summed for a total score, with higher scores corresponding to greater body dissatisfaction (range = 10 to 50; α = .92). This scale has demonstrated good discriminant, convergent, and predictive validity among all age and gender groups in prior studies conducted by our group (Neumark-Sztainer et al., 2006; Paxton et al., 2006). This scale has also demonstrated good test-retest reliability over two weeks (rs from .68 – .77).
Predictor Variables.
A number of psychological and environmental variables at baseline were examined as predictors of body dissatisfaction trajectory.
Depressive Symptoms.
Depressive symptoms were assessed using Kandel and Davies’ (1982) six-item scale. Participants responded to items asking about depressed mood (e.g., “During the past 12 months, how often have you been bothered or troubled by feeling unhappy, sad, or depressed?”) on a three-point scale from 1 (not at all) to 3 (very much). A total score was calculated by summing responses to all items, with higher scores indicating greater depressive symptoms (range = 6 to 18; α = .84). This measure demonstrated adequate test-retest reliability (rs from .31 – .72), and has also shown good concurrent validity (Kandel & Davies, 1982).
Self-Esteem.
Self-esteem was assessed with a six-item scale adapted from the Rosenberg Self-Esteem Scale (Rosenberg, 1965). The current study omitted two positive and two negative items from the original ten-item measure to reduce participant burden. Participants indicated how strongly they agreed with statements (e.g., “At times I think that I am no good at all”) on a scale from 1 (strongly disagree) to 4 (strongly agree). All items were reverse-scored, and a total score was calculated by summing responses to all items, with higher scores indicating higher self-esteem (range = 6 to 24; α = .85). Supporting the validity of the adapted scale, correlations between the adapted and full scales with disordered eating, perfectionism, and depressed mood were previously shown to be nearly identical (van den Berg, Mond, Eisenberg, Ackard, & Neumark-Sztainer, 2010).
Parent Dieting.
Parent dieting was assessed with four items asking participants about their perceptions of their parents’ eating habits (e.g., “My mother/father diets to lose weight or keep from gaining weight”) on a scale from 1 (not at all) to 4 (very much). A total score was calculated by averaging responses to all items, with higher scores indicating more parental dieting and encouragement from parents to diet. This measure has shown good test-retest reliability over two weeks (rs from .60 – .64), as well as good concurrent and predictive validity in associations unhealthy weight control behaviors (Neumark-Sztainer et al., 2010), and predicting future body dissatisfaction (Quick et al., 2013).
Parent Communication and Caring.
Parent communication and caring were assessed with two questions asking how comfortable participants felt talking to each of their parents and two questions asking how much they felt their parents cared about them (e.g., “How much do you feel you can talk to your mother about your problems?”) rated on a five-point scale from 1 (not at all) to 5 (very much). A total score was calculated by averaging responses to all four questions, with higher scores indicating more communication and caring from parents (range = 1 to 5; α = .69). For participants with missing data for one parent, these missing values were imputed with data from the other parent, allowing participants with data for only one parent to be included in analyses. This measure has shown good test-retest reliability over two weeks (rs from .70 – .82), as well as good concurrent and predictive validity in associations with self-esteem and depression (Ackard, Neumark-Sztainer, Story, & Perry, 2006), and predicting future body dissatisfaction (Quick et al., 2013).
Peer Dieting.
Peer dieting was assessed by asking participants how much they agreed with the statement, “Many of my friends diet to lose weight or keep from gaining weight” on a four-point scale from 1 (Not at all) to 4 (Very much) (Eisenberg, Neumark-Sztainer, Story, & Perry, 2005; Neumark-Sztainer, Wall, Story, & Perry, 2003). Higher scores indicate perceptions of more peer dieting; participants who responded “I don’t know” (n = 188, 16.6%) were included in models with a dummy variable. This measure has shown adequate test-retest reliability over two weeks (r = .40), as well as good predictive validity in predicting future binge eating and extreme weight control behaviors (Neumark-Sztainer et al., 2007).
Weight Teasing.
Weight teasing was assessed with the question, “How often are you teased about your weight?” with participants responding on a 5 point scale from 1 (Never) to 5 (At least once a week). This measure has shown good predictive validity for future obesity, binge eating, dieting, unhealthy weight control behaviors, and body dissatisfaction (Puhl et al., 2017).
Covariates and moderators.
Participants self-reported their gender, age, race/ethnicity, and socioeconomic status (SES) at baseline. Gender (male/female) and race/ethnicity (White, Black/African American, Hispanic or Latino, Asian American, Hawaiian or Pacific Islander, American Indian or Native American) were entered as categorical variables, and age was entered as a continuous variable. SES was entered as a continuous variable (low, low/medium, medium, medium/high, high) based on indicators of parent education, work status, and public assistance (e.g., free school lunches, welfare, food stamps) using a series of decision rules in classification and regression trees (Neumark-Sztainer et al., 2002). BMI was calculated according to the standard formula based on self-reported height and weight at each assessment point. Self-reported BMI and measured BMI were highly correlated in both male (r = .88) and female (r = .85) participants at baseline (Himes, Hannan, Wall, & Neumark-Sztainer, 2005), indicating that self-reported BMIs were largely accurate and valid. As BMI percentile is the standard assessment measure for children and adolescents (Kuczmarski et al., 2000; Ogden, Carroll, Kit, & Flegal, 2012), we calculated a categorical overweight status variable to maintain consistency throughout the study, based on BMI ≥ 85th percentile (Kuczmarski et al., 2000) at Time 1 and Time 2 when participants were still mostly adolescents, and as BMI ≥ 25 at Time 3 and Time 4 when all participants were adults.
Data Analytic Plan
Population Mean Body Dissatisfaction.
We first tested for changes in longitudinal trends in the population-level mean body dissatisfaction using generalized estimating equations (GEE) to account for correlation within individuals across time. We fit two longitudinal models, both including categorical time, gender, and time by gender interaction. The first model controlled for age, baseline SES, and ethnicity/race, and the second model additionally controlled for overweight status at each time point.
Body Dissatisfaction Trajectories.
Next, growth curve mixture modeling (GMM) with random intercept, slope, and quadratic terms examined trajectories of body dissatisfaction over time. This method allowed for identification of unobserved latent subclasses of individuals with similar patterns of longitudinal change in body dissatisfaction. GMMs were fit with and without controlling for overweight status at each time point. Full information maximum likelihood estimation was used to ensure all subjects, including those with some missing data, were included in the models. The best fitting number of classes in the GMM was determined based on BIC, with lower BIC indicating better model fit (Nylund, Asparouhov, & Muthén, 2007). Observed mean trajectories of body dissatisfaction from the GMM were calculated based on the most likely trajectory class membership and frequencies and proportions in each class calculated by gender.
Predictors of Body Dissatisfaction Trajectories.
Multinomial logistic regressions, using the most likely trajectory class membership as the categorical outcome, examined the association with putative baseline risk and protective factors (depressive symptoms, self-esteem, parent dieting, parent communication and caring, peer dieting, weight teasing) controlling for age, gender, SES, ethnicity/race, and overweight status. Growth mixture models were fit using Mplus 7.4 and all other analyses were performed in SAS 9.4. All analyses incorporated inverse probability weights (see below) to control for attrition.
Missing Data.
To account for missing data, because attrition from the baseline sample was not completely at random, inverse probability weighting (IPW) (Little, 1986; Seaman & White, 2011) was used for all analyses (Little, 1986). IPW is the recommended method for handling missing data in longitudinal studies, where individuals who do not respond to surveys at various assessment time points have missing values on many variables (Seaman & White, 2011). IPW minimizes potential response bias due to missing data and allows for extrapolation back to the original Project EAT-I school-based sample. Weights for IPW were derived as the inverse of the estimated probability that an individual responded at all four time points based on several Time 1 covariates including demographics, overweight status, parental living situation, and grades in school. Non-completers were more likely than completers to be male, non-white, and at baseline to be overweight. However, after weighting, there were no significant differences between the completers and the original full sample on these baseline variables or body dissatisfaction (ps > 0.20).
Results
Population Mean Body Dissatisfaction
Mean levels of body dissatisfaction across the four time points were higher for females than for males, but with average levels at each time point that were near the middle of the range (see Figure 1). Results from the first GEE model indicated that average body dissatisfaction increased slightly, but significantly, for both females (standardized beta = 0.08, 95% CI = 0.05–0.11, p < .001) and males (standardized beta = 0.09, 95% CI = 0.05–0.12, p < .001) over the 15-year period controlling for race, baseline SES, and age. This increase appeared to be largely attributable to increases in weight over the same time period; in the second GEE model average body dissatisfaction still remained high, but the trend towards increasing body dissatisfaction over time was no longer significant after adjustment for overweight status at each time point for males (p = .82) or females (p = .94). Supplemental Table S1 presents full results from both GEE models.
Figure 1.
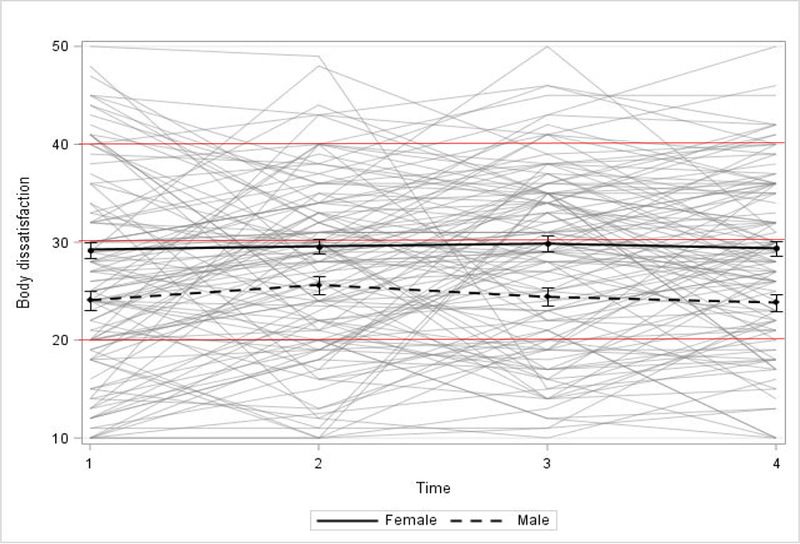
Average levels of body dissatisfaction for males and females, with 95% confidence intervals; higher scores indicate greater body dissatisfaction.
Note. Average levels of body dissatisfaction (dark black lines) are overlaid on spaghetti plots for a random subset of participants (light grey lines). Figure is adjusted for overweight status, age, socioeconomic status, and race. Body dissatisfaction was measured with a 10-item scale assessing participants’ satisfaction with various body parts; higher scores indicate greater body dissatisfaction (range = 10 – 50). On average, participants were 14.9 years old at Time 1, 19.3 at Time 2, 25.2 at Time 3, and 31.0 at Time 4.
Body Dissatisfaction Trajectories
GMM analyses with and without adjusting for overweight status supported a 4-class solution as the best fitting model based on BIC (unadjusted GMM: 2 class BIC = 39692, entropy = .477; 3 class BIC = 39689, entropy = .61; 4 class BIC = 39687, entropy = .632; 5 class BIC = 39696, entropy = .773; GMM adjusted for overweight status: 2 class BIC = 32598, entropy = .9; 3 class BIC = 32603, entropy = .873; 4 class BIC = 32592, entropy = .714; 5 class model would not converge after increasing starting values indicating possible poor fit); results of the unadjusted GMM are shown in Table 1 and Figure 2. The identified trajectories followed four patterns of body dissatisfaction (see Supplemental Table S2 for posterior probabilities of being assigned to each of the four classes). Compared to the other classes, class 1 (n = 900) exhibited the most consistently low, though slightly increasing, body dissatisfaction scores across all four time points, and was labeled “consistently low, but slightly increasing”. Class 2 (n = 46) exhibited the lowest body dissatisfaction at Time 1, but then displayed a sharp increase at Time 2, and subsequent decrease at Times 3 and 4, and was labeled “low, but increasing, then decreasing”. Class 3 (n = 58) exhibited moderately high body dissatisfaction at Time 1, but then displayed a sharp decrease, and subsequent increase, in body dissatisfaction at Times 2 and 4 (with relatively stable scores from Time 2 to Time 3), and was labeled “high, but decreasing, then increasing”. Compared to the other classes, class 4 (n = 451) exhibited high body dissatisfaction at Time 1, and maintained consistently high body dissatisfaction (with slight decreases) across all four time points, and was labeled “consistently high, but slightly decreasing.”
Table 1.
Membership in body dissatisfaction trajectories.
| n (Weighted %)a | |||
|---|---|---|---|
| Class | Overall (N = 1,455) | Female (n = 858) | Male (n = 597 |
| 1 (Consistently low, slightly increasing) | 900 (60.0%) | 444 (48.0%) | 456 (71.4%) |
| 2 (Low, but increasing, then decreasing) | 46 (4.4%) | 25 (3.6%) | 21 (5.2%) |
| 3 (High, but decreasing, then increasing) | 58 (4.2%) | 29 (3.9%) | 29 (4.5%) |
| 4 (Consistently high, slightly decreasing) | 451 (31.3%) | 360 (44.5%) | 91 (18.9%) |
Note. Classes were derived from growth curve mixture modeling of common latent body dissatisfaction trajectories.
Ns are raw sample sizes; percentages are weighted by non-response propensity weights to reflect original Time 1 sample population.
Figure 2.

Four-class model of body dissatisfaction trajectories; higher scores indicate greater body dissatisfaction.
Note. Adjusted for overweight status, age, socioeconomic status, and race. Body dissatisfaction was measured with a 10-item scale assessing participants’ satisfaction with various body parts; higher scores indicate greater body dissatisfaction (range = 10 – 50). On average, participants were 14.8 years old at Time 1, 19.3 at Time 2, 25.2 at Time 3, and 31.0 at Time 4.
As shown in Table 1, a similar proportion of females were in class 1 (consistently low, slightly increasing body dissatisfaction) and class 4 (consistently high, slightly decreasing body dissatisfaction), whereas a much higher proportion of males were in class 1 than class 4. A similar proportion of females and males were in classes 2 (low, but increasing, then decreasing body dissatisfaction) and 3 (high, but decreasing, then increasing body dissatisfaction).
Predictors of Body Dissatisfaction Trajectories
Multinomial logistic regression analyses examined predictors of membership in different body dissatisfaction trajectories. In order to reduce the number of comparisons and, thus, the potential for alpha inflation, we chose to conduct a small number of planned comparisons between classes of most theoretical interest based on results from GMM trajectory analyses. First, to examine predictors of different trajectories among individuals who started out with similarly low body dissatisfaction at baseline but subsequently followed different trajectories, we examined predictors of classification in classes 1 (consistently low, slightly increasing) and 2 (low, but increasing, then decreasing). Similarly, to examine predictors of different trajectories among individuals with comparably high body dissatisfaction at baseline but subsequently followed different trajectories, we examined predictors of classification in class 3 (high, but decreasing, then increasing) and 4 (consistently high, slightly decreasing). Finally, to determine baseline characteristics that differentiated participants following the least and most problematic trajectories, respectively, we examined predictors of classification in classes 1 and 4.
Results from these analyses found that among participants with low baseline body dissatisfaction (classes 1 and 2), peer dieting differentiated subsequent trajectories, with individuals reporting high peer dieting more likely to be in class 2 (low, but increasing, then decreasing) than class 1 (consistently low). Elevated depressive symptoms, lower self-esteem, lower parent communication and caring, more peer dieting, and more weight teasing predicted classification in class 4 (consistently high, slightly decreasing) versus class 1 (consistently low, slightly increasing). No risk or protective factors differentiated individuals who started with high body dissatisfaction, but followed subsequent trajectories (class 3 versus 4; see Table 2).
Table 2.
Predictors of body dissatisfaction trajectories.
| Pairwise Odds Ratio (95% CI) | |||
|---|---|---|---|
| Predictor | (Class 2 vs Class 1) | (Class 4 vs Class 1) | (Class 4 vs Class 3) |
| Depressive symptoms | 1.076 (0.948–1.223) | 1.261 (1.18–1.346) | 1.071 (0.949–1.209) |
| Self-esteem | 1.121 (0.944–1.331) | 0.752 (0.702–0.804) | 0.954 (0.86–1.059) |
| Parent dieting | 1.356 (0.875–2.101) | 1.217 (0.985–1.505) | 1.062 (0.707–1.596) |
| Parent communication/caring | 0.917 (0.805–1.044) | 0.874 (0.818–0.934) | 0.979 (0.868–1.104) |
| Peer dieting | 1.691 (1.155–2.474) | 1.39 (1.12–1.724) | 1.295 (0.877–1.912) |
| Peer dieting (“don’t know”) | 0.369 (0.065–2.105) | 2.020 (1.085–3.760) | 1.157 (0.327–4.094) |
| Weight teasing | 0.924 (0.626–1.365) | 1.3 (1.086–1.556) | 1.088 (0.802–1.474) |
Note. Adjusted for age, gender, socioeconomic status, race, and overweight status at Time 1. Significant odds ratios are bolded. We compared predictors of trajectories of individuals who started out with similar levels of body dissatisfaction but subsequently followed different trajectories (Class 2 vs. Class 1; Class 4 vs. Class 3), as well as the most and least problematic trajectories (Class 4 vs. Class 1). Predictors were assessed at baseline. Class 1 = consistently low, slightly increasing body dissatisfaction; class 2 = low, but increasing, then decreasing body dissatisfaction; class 3 = high, but decreasing, then increasing body dissatisfaction; class 4 = consistently high, slightly decreasing body dissatisfaction.
Discussion
The current study examined the prevalence and common trajectories of body dissatisfaction for males and females across 15 years from middle adolescence to adulthood. We identified four common patterns of change in body dissatisfaction, as well as risk and protective factors predicting membership in these groups. Examining individual patterns in the naturalistic long-term time course of body dissatisfaction, results indicated that among a diverse group of participants, body dissatisfaction remained relatively constant for the vast majority from adolescence to adulthood. When examining individual trajectories, almost two-thirds of participants experienced consistently low, though slightly increasing, levels of body dissatisfaction that reflected the unadjusted mean population time course of this variable, and approximately one-third of participants endorsed consistently high, though slightly decreasing, levels of body dissatisfaction. These results may provide somewhat encouraging information for individuals with consistently high levels of body dissatisfaction, as they indicate that this high dissatisfaction may slightly temper over time. On the other hand, individuals with consistently low levels of body dissatisfaction may experience slight increases in dissatisfaction over time. However, because the magnitude of the changes in these groups was small, these findings suggest that body dissatisfaction remains relatively stable, with some minor shifts, from middle adolescence to adulthood for nearly 95% of individuals. Even the small percentage of participants with periods of larger increases and decreases in body dissatisfaction (classes 2 and 3) during late adolescence and early adulthood later returned to their original, mid-adolescent levels of body dissatisfaction as they entered adulthood, demonstrating that severity of body dissatisfaction in adulthood is largely determined prior to middle adolescence.
It is therefore possible that, similar to other developmentally critical periods for various traits and behaviors, there is a critical period prior to mid-adolescence during which individuals develop their self-image, including body image, and learn to sense, perceive, and evaluate their bodies. Indeed, previous research documenting body image disturbances in youth (Lowes & Tiggeman, 2003; Spiel, Paxton, & Yager, 2012) suggest that a critical period for body image may actually occur earlier in adolescence, or even during childhood. Similar developmental stages have been identified as critical periods of risk for obesity in early- to mid-childhood (Dietz, 1994), and for eating disorders during puberty (Baker, Thornton, Lichtenstein, & Bulik, 2012; Klump, 2013). Results from developmental twin studies also suggest different temporal patterns of genetic and environmental influences on body satisfaction, with shared environment contributing significantly more variance to weight and shape concerns in pre-adolescence than mid-adolescence and adulthood, highlighting different developmental periods of vulnerability for development of body dissatisfaction (Klump et al., 2010). Moreover, previous body dissatisfaction trajectories derived by Rodgers and colleagues (2016) found a subgroup of early adolescents who already demonstrated persistent high body dissatisfaction across 14 months. If such a sensitive period of vulnerability for body dissatisfaction exists, this would indicate a crucial need to target body satisfaction in prevention and early intervention programs prior to mid-adolescence, especially given the wide range of negative psychosocial outcomes, such as eating disorders, obesity, and mood disturbances, associated with body dissatisfaction (Ackard, Croll, & Kearney-Cooke, 2002; Neumark-Sztainer et al., 2006; Neumark-Sztainer et al., 2010).
Moreover, as previous research has also identified common trajectories of increasing, decreasing, and consistent engagement in eating disorder behaviors during these developmental periods, targeting body dissatisfaction during childhood or early adolescence could reduce the likelihood of beginning or increasing eating disorder behaviors. In fact, research indicates that body dissatisfaction among individuals with eating disorders is remarkably resistant to change (Gusella, Butler, Nichols, & Bird, 2003; Pauli, Aebi, Metzke, & Steinhausen, 2017), suggesting that clinicians should seek to intervene upon body dissatisfaction before it becomes chronic. These findings also highlight a critical need to identify interventions that may be suitable in altering these seemingly intractable body dissatisfaction patterns. For instance, as increases in body dissatisfaction appeared closely tied to weight, promoting body acceptance at an early age may be vital in reducing body dissatisfaction.
By identifying several common time courses of body dissatisfaction, the current study also assisted in clarifying previous research that has provided discrepant information as to whether body dissatisfaction increases, decreases, or remains stable throughout adolescence and adulthood (Heatherton et al., 1997; Keel et al., 2007; Reba-Harrelson et al., 2009). Our results suggested that not all individuals, even when stratified by gender, share a similar course of body dissatisfaction severity. Rather, the analyses identified several differing trajectories of stability and change in body dissatisfaction. The analysis approach utilized here allowed us to empirically derive subgroups of individuals who may have varying prevention and intervention needs.
Individual-level factors of depression and self-esteem, as well as environmental-level factors of parent communication and caring, peer dieting, and weight teasing, seem potentially important in predicting these trajectories. These variables differentiated participants with consistently low versus high dissatisfaction, such that participants endorsing greater depression and lower self-esteem during adolescence, as well as more peer dieting and weight teasing, and less parent communication/caring, were more likely to be chronically dissatisfied with their bodies. Similarly, participants reporting more peer dieting were more likely to experience fluctuations in low body dissatisfaction rather than persistent low body dissatisfaction over time. As this trajectory showed sharp increases in body dissatisfaction during late adolescence, with subsequent decreases in adulthood, individuals in these group may be particularly affected by peer dieting, at least temporarily. Interventions aimed at reducing dieting at a group level among adolescents might be therefore be useful in reducing body dissatisfaction for this group during late adolescence. Importantly, these findings also suggest that depression, self-esteem, parent communication/caring, peer dieting, and weight-based teasing may not only be important predictors of future body dissatisfaction on average (Paxton, Eisenberg, & Neumark-Sztainer, 2006; Puhl et al., 2017; Quick et al., 2013), but also of long-term patterns of body dissatisfaction. As body dissatisfaction, self-esteem, and depressive symptomology are all facets related to self-concept and identity, these findings also bolster the idea that a sensitive window prior to middle adolescence may exist for developing a healthy self-concept, and it may be interesting for future research to consider whether trajectories of self-esteem and depression mirror those derived for body dissatisfaction in the current study. It is also possible that other variables, including those not assessed at baseline in the current study (e.g., trauma) may predict differing body dissatisfaction trajectories; however, the relatively small number of participants in classes 2 (low, but increasing, then decreasing) and 3 (high, but decreasing, then increasing) may have limited our ability to detect all but the most robust predictors. Future studies with larger sample sizes examining factors, including interactions of factors and gender differences between factors, that predict differing trajectories could provide important information about why some, but not all, individuals experience significant fluctuations in body dissatisfaction in late adolescence and early adulthood.
Results from the current study highlight the urgent need for early prevention and intervention for body dissatisfaction among both male and female youth. To this end, several prevention programs have shown promising results in reducing in body dissatisfaction. For example, New Moves, a school-based program, designed to promote positive weight-related health, which was implemented within physical education classes in high schools, significantly improved body satisfaction and self-worth among adolescent girls (Neumark-Sztainer et al., 2010). Similarly, a self-esteem enhancement program called Everybody’s Different has been shown to reduce body dissatisfaction among adolescents (O’Dea, 2004; O’Dea & Abraham, 1999). Internet-based intervention programs, such as Student Bodies, have also shown efficacy in reducing body dissatisfaction among college women at high risk for eating disorders (Taylor et al., 2006). Results of the current study suggest that these programs, which have been developed and tested in adolescence and early adulthood, should be tested with younger cohorts (e.g., childhood, early adolescence) when body dissatisfaction may be more malleable. Moreover, these results suggest that approaches further aimed at enhancing self-esteem, decreasing depression, increasing parent/child connectedness, and reducing and responding effectively to weight-based teasing and peer dieting may be particularly impactful on altering body dissatisfaction over time. Continued research examining whether existing or novel prevention programs are effective in altering long-term body dissatisfaction trajectories, or promoting consistently low body dissatisfaction trajectories, could have important clinical implications on how to intervene before body dissatisfaction becomes chronic.
This study had a number of strengths, including the use of advanced empirical modeling to classify individuals into distinct groups based on common response patterns across time. The large sample of racially, ethically, and socioeconomically diverse participants also improved the generalizability of our findings. In addition, the current study’s 15-year longitudinal design allowed us to identify trajectories of change from adolescence to adulthood, an age group that has been underrepresented in the body dissatisfaction literature. However, there were also study limitations, including study attrition from baseline to follow-up assessments. Although a large portion of attrition was due to insufficient contact information for participants based on the original cross-sectional design, response rates in the current study are in some cases lower than other longitudinal studies (e.g., 63% retention rate in Fontaine et al., 2008; 73% retention rate in Keel et at., 2007). In addition to not having collected strong contact information at baseline due to the original cross-sectional design, factors such as the young developmental stage of Project EAT participants at baseline, greater residential mobility, and distrust of research among ethically/racially diverse and lower income communities may have contributed to lower response rates in the present study. Compared to the baseline sample, participants who completed all four assessments were more likely to be female, White, and non-overweight, which may have biased the analyses. To account for any systematic differences between participants who did and did not respond to all surveys, we adjusted estimates using population weights to be more representative of the original sample. Further, many items comprising the body dissatisfaction scale (e.g., satisfaction with waist, hips, thighs, stomach, etc.) may be biased towards stereotypically feminine concerns and may not accurately assess body image in men, who may be more concerned with muscularity than thinness (Griffiths, Murray, & Touyz, 2013). Although additional items assessing male body image were included in Project EAT-IV, these were not available at earlier time points. Data collection also occurred across a time with significant societal changes, including greater internet usage and development and spread of social media, alongside increased attention to body acceptance messages (Karazsia, Murnen, & Tylka, 2017; Poushter, 2016). These environmental-level changes may be a possible factor influencing the results of the current study, such that increased access to messages on the internet and social media during development from adolescence to adulthood may have exerted unique effects on the current data that would not be present for other cohorts at different times. In addition, all data were based on self-report. Future research should use multi-method approaches, including interview and biological data, to assess the full spectrum of male and female body dissatisfaction and factors that contribute to differing trajectories of body dissatisfaction. Finally, average scores in the high body dissatisfaction group were between 30 – 40 (out of a full range of 10–50), indicating that participants in this group were more dissatisfied than satisfied (but perhaps not extremely dissatisfied). However, previous research has found that higher scores on this body dissatisfaction measure are associated with significantly worse clinical outcomes (e.g., greater eating disorder behaviors, worse depressive mood, lower self-esteem) (Neumark-Sztainer et al., 2006; Paxton et al., 2006), indicating that high scores on this measure are clinically meaningful.
The current study contributes new information about patterns of body dissatisfaction over key developmental periods. Largely, body dissatisfaction during adulthood appears to be formed and fixed prior middle adolescence, even for individuals who experience brief periods of increasing or decreasing body dissatisfaction during the transition through late adolescence and early adulthood. These findings indicate that there may be a critical period for body dissatisfaction occurring in childhood or early adolescence. Further research is needed to examine these intriguing possibilities, which could enhance our understanding of the ways in which body image is developed and maintained, as well as inform the implementation of targeted body dissatisfaction interventions for youth in critical developmental periods.
Supplementary Material
Acknowledgments
Funding: This study was supported by Grant Number R01HL116892 from the National Heart, Lung, and Blood Institute (PI: Dianne Neumark-Sztainer). Shirley B. Wang is supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-1745303. Ann F. Haynos received support from Grants T32MH082761 and K23MH112867 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute, the National Institutes of Health, the National Institute of Mental Health, or the National Science Foundation.
References
- Ackard DM, Croll JK, & Kearney-Cooke A (2002). Dieting frequency among college females: Association with disordered eating, body image, and related psychological problems. Journal of Psychosomatic research, 52(3), 129–136. [DOI] [PubMed] [Google Scholar]
- Ackard DM, Neumark-Sztainer D, Story M, & Perry C (2006). Parent–child connectedness and behavioral and emotional health among adolescents. American journal of preventive medicine, 30(1), 59–66. [DOI] [PubMed] [Google Scholar]
- Allen KL, Byrne SM, Oddy WH, & Crosby RD (2013). Early onset binge eating and purging eating disorders: Course and outcome in a population-based study of adolescents. Journal of Abnormal Child Psychology, 41(7), 1083–1096. [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American psychologist, 55(5), 469. [PubMed] [Google Scholar]
- Baker JH, Thornton LM, Lichtenstein P, & Bulik CM (2012). Pubertal development predicts eating behaviors in adolescence. International Journal of Eating Disorders, 45(7), 819–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucchianeri MM, Arikian AJ, Hannan PJ, Eisenberg ME, & Neumark-Sztainer D (2013). Body dissatisfaction from adolescence to young adulthood: Findings from a 10-year longitudinal study. Body image, 10(1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucchianeri MM, Fernandes N, Loth K, Hannan PJ, Eisenberg ME, & Neumark-Sztainer D (2016). Body dissatisfaction: Do associations with disordered eating and psychological well-being differ across race/ethnicity in adolescent girls and boys?. Cultural Diversity and Ethnic Minority Psychology, 22(1), 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz WH (1994). Critical periods in childhood for the development of obesity. The American journal of clinical nutrition, 59(5), 955–959. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Neumark-Sztainer D, & Paxton SJ (2006). Five-year change in body satisfaction among adolescents. Journal of psychosomatic research, 61(4), 521–527. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Neumark-Sztainer D, Story M, & Perry C (2005). The role of social norms and friends’ influences on unhealthy weight-control behaviors among adolescent girls. Social Science & Medicine, 60(6), 1165–1173. [DOI] [PubMed] [Google Scholar]
- Fontaine N, Carbonneau R, Barker ED, Vitaro F, Hébert M, Côté SM, … & Tremblay RE (2008). Girls’ hyperactivity and physical aggression during childhood and adjustment problems in early adulthood: a 15-year longitudinal study. Archives of General Psychiatry, 65(3), 320–328. [DOI] [PubMed] [Google Scholar]
- Griffiths S, Murray SB, & Touyz S (2013). Disordered eating and the muscular ideal. Journal of eating disorders, 1(1), 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gusella J, Butler G, Nichols L, & Bird D (2003). A brief questionnaire to assess readiness to change in adolescents with eating disorders: Its applications to group therapy. European Eating Disorders Review, 11(1), 58–71. [Google Scholar]
- Haines J, Neumark‐Sztainer D, Wall M, & Story M (2007). Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obesity, 15(11), 2748–2760. [DOI] [PubMed] [Google Scholar]
- Haynos AF, Wall MM, Chen C, Wang SB, Loth K, & Neumark‐Sztainer D (2018). Patterns of weight control behavior persisting beyond young adulthood: Results from a 15‐year longitudinal study. International Journal of Eating Disorders, 51(9), 1090–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Mahamedi F, Striepe M, Field AE, & Keel P (1997). A 10-year longitudinal study of body weight, dieting, and eating disorder symptoms. Journal of abnormal psychology, 106(1), 117. [PubMed] [Google Scholar]
- Himes JH, Hannan P, Wall M, & Neumark-Sztainer D (2005). Factors associated with errors in self-reports of stature, weight, and body mass index in Minnesota adolescents. Annals of epidemiology, 15(4), 272–278. [DOI] [PubMed] [Google Scholar]
- Holsen I, Kraft P, & Røysamb E (2001). The relationship between body image and depressed mood in adolescence: A 5-year longitudinal panel study. Journal of Health Psychology, 6(6), 613–627. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological psychiatry, 61(3), 348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, & Agras WS (2004). Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychological bulletin, 130(1), 19. [DOI] [PubMed] [Google Scholar]
- Johnson F, & Wardle J (2005). Dietary restraint, body dissatisfaction, and psychological distress: a prospective analysis. Journal of abnormal psychology, 114(1), 119. [DOI] [PubMed] [Google Scholar]
- Kandel DB, & Davies M (1982). Epidemiology of depressive mood in adolescents: An empirical study. Archives of general psychiatry, 39(10), 1205–1212. [DOI] [PubMed] [Google Scholar]
- Karazsia BT, Murnen SK, & Tylka TL (2017). Is body dissatisfaction changing across time? A cross-temporal meta-analysis. Psychological bulletin, 143(3), 293. [DOI] [PubMed] [Google Scholar]
- Keel PK, Baxter MG, Heatherton TF, & Joiner TE Jr (2007). A 20-year longitudinal study of body weight, dieting, and eating disorder symptoms. Journal of abnormal psychology, 116(2), 422. [DOI] [PubMed] [Google Scholar]
- Kim DS, & Kim HS (2009). Body-image dissatisfaction as a predictor of suicidal ideation among Korean boys and girls in different stages of adolescence: A two-year longitudinal study. Journal of Adolescent Health, 45(1), 47–54. [DOI] [PubMed] [Google Scholar]
- Klump KL, Burt SA, Spanos A, McGue M, Iacono WG, & Wade TD (2010). Age differences in genetic and environmental influences on weight and shape concerns. International Journal of Eating Disorders, 43(8), 679–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL (2013). Puberty as a critical risk period for eating disorders: A review of human and animal studies. Hormones and behavior, 64(2), 399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, … & Johnson CL (2000). CDC growth charts: United States. Advance data, (314), 1–27. [PubMed] [Google Scholar]
- Little RJ (1986). Survey nonresponse adjustments for estimates of means. International Statistical Review/Revue Internationale de Statistique, 139–157.
- Loth KA, Watts AW, Van Den Berg P, & Neumark-Sztainer D (2015). Does body satisfaction help or harm overweight teens? A 10-year longitudinal study of the relationship between body satisfaction and body mass index. Journal of Adolescent Health, 57(5), 559–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowes J, & Tiggemann M (2003). Body dissatisfaction, dieting awareness and the impact of parental influence in young children. British journal of health psychology, 8(2), 135–147. [DOI] [PubMed] [Google Scholar]
- Mond JM, & Hay PJ (2007). Functional impairment associated with bulimic behaviors in a community sample of men and women. International Journal of Eating Disorders, 40(5), 391–398. [DOI] [PubMed] [Google Scholar]
- Mond J, Mitchison D, Latner J, Hay P, Owen C, & Rodgers B (2013). Quality of life impairment associated with body dissatisfaction in a general population sample of women. BMC Public Health, 13(1), 920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond J, Van den Berg P, Boutelle K, Hannan P, & Neumark-Sztainer D (2011). Obesity, body dissatisfaction, and emotional well-being in early and late adolescence: findings from the project EAT study. Journal of Adolescent Health, 48(4), 373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer DR, Friend SE, Flattum CF, Hannan PJ, Story MT, Bauer KW, … & Petrich CA (2010). New moves—preventing weight-related problems in adolescent girls: a group-randomized study. American journal of preventive medicine, 39(5), 421–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Goeden C, Story M, & Wall M (2004). Associations between body satisfaction and physical activity in adolescents: Implications for programs aimed at preventing a broad spectrum of weight-related disorders. Eating Disorders, 12(2), 125–137. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Paxton SJ, Hannan PJ, Haines J, & Story M (2006). Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. Journal of Adolescent Health, 39(2), 244–251. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Story M, Perry C, & Casey MA (1999). Factors influencing food choices of adolescents: findings from focus-group discussions with adolescents. Journal of the American dietetic association, 99(8), 929–937. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall MM, Chen C, Larson N, Christoph M, Sherwood NE (2018). Eating, activity, and weight-related problems across the life course from adolescence to adulthood: Prevalences and trajectories. Manuscript under review [DOI] [PMC free article] [PubMed]
- Neumark-Sztainer D, Wall M, Eisenberg ME, Story M, & Hannan PJ (2006). Overweight status and weight control behaviors in adolescents: longitudinal and secular trends from 1999 to 2004. Preventive medicine, 43(1), 52–59. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer DR, Wall MM, Haines JI, Story MT, Sherwood NE, & van den Berg PA (2007). Shared risk and protective factors for overweight and disordered eating in adolescents. American journal of preventive medicine, 33(5), 359–369. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall MM, Story M, & Perry CL (2003). Correlates of unhealthy weight-control behaviors among adolescents: Implications for prevention programs. Health Psychology, 22(1), 88. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural equation modeling, 14(4), 535–569. [Google Scholar]
- O’Dea JA (2004). Evidence for a self-esteem approach in the prevention of body image and eating problems among children and adolescents. Eating disorders, 12(3), 225–239. [DOI] [PubMed] [Google Scholar]
- O’Dea JA, & Abraham S (1999). Association between self-concept and body weight, gender, and pubertal development among male and female adolescents. Adolescence, 34(133), 69–70. [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, & Flegal KM (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. Jama, 307(5), 483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauli D, Aebi M, Metzke CW, & Steinhausen HC (2017). Motivation to change, coping, and self-esteem in adolescent anorexia nervosa: a validation study of the Anorexia Nervosa Stages of Change Questionnaire (ANSOCQ). Journal of eating disorders, 5(1), 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paxton SJ, Eisenberg ME, & Neumark-Sztainer D (2006). Prospective predictors of body dissatisfaction in adolescent girls and boys: a five-year longitudinal study. Developmental psychology, 42(5), 888. [DOI] [PubMed] [Google Scholar]
- Paxton SJ, Neumark-Sztainer D, Hannan PJ, & Eisenberg ME (2006). Body dissatisfaction prospectively predicts depressive mood and low self-esteem in adolescent girls and boys. Journal of clinical child and adolescent psychology, 35(4), 539–549. [DOI] [PubMed] [Google Scholar]
- Pearson CM, & Smith GT (2015). Bulimic symptom onset in young girls: A longitudinal trajectory analysis. Journal of abnormal psychology, 124(4), 1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pingitore R, Spring B, & Garfieldt D (1997). Gender differences in body satisfaction. Obesity, 5(5), 402–409. [DOI] [PubMed] [Google Scholar]
- Poushter J (2016). Smartphone ownership and internet usage continues to climb in emerging economies. Pew Research Center, 22, 1–44. [Google Scholar]
- Presnell K, Bearman SK, & Stice E (2004). Risk factors for body dissatisfaction in adolescent boys and girls: A prospective study. International Journal of eating disorders, 36(4), 389–401. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Wall MM, Chen C, Austin SB, Eisenberg ME, & Neumark-Sztainer D (2017). Experiences of weight teasing in adolescence and weight-related outcomes in adulthood: a 15-year longitudinal study. Preventive medicine, 100, 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quick V, Eisenberg ME, Bucchianeri MM, & Neumark-Sztainer D (2013). Prospective predictors of body dissatisfaction in young adults: 10-year longitudinal findings. Emerging Adulthood, 1(4), 271–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reba-Harrelson L, Von Holle A, Hamer RM, Swann R, Reyes ML, & Bulik CM (2009). Patterns and prevalence of disordered eating and weight control behaviors in women ages 25–45. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 14(4), e190–e198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers RF, McLean SA, Marques M, Dunstan CJ, & Paxton SJ (2016). Trajectories of body dissatisfaction and dietary restriction in early adolescent girls: A latent class growth analysis. Journal of youth and adolescence, 45(8), 1664–1677. [DOI] [PubMed] [Google Scholar]
- Rosenberg M (1965). Society and the adolescent self-image (Vol. 11, p. 326) Princeton, NJ: Princeton university press. [Google Scholar]
- Rohde P, Stice E, & Marti CN (2015). Development and predictive effects of eating disorder risk factors during adolescence: Implications for prevention efforts. International Journal of Eating Disorders, 48(2), 187–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaman SR, & White IR (2013). Review of inverse probability weighting for dealing with missing data. Statistical methods in medical research, 22(3), 278–295. [DOI] [PubMed] [Google Scholar]
- Spiel EC, Paxton SJ, & Yager Z (2012). Weight attitudes in 3-to 5-year-old children: Age differences and cross-sectional predictors. Body image, 9(4), 524–527. [DOI] [PubMed] [Google Scholar]
- Stice E (2002). Risk and maintenance factors for eating pathology: a meta-analytic review. Psychological bulletin, 128(5), 825. [DOI] [PubMed] [Google Scholar]
- Stice E, & Shaw HE (2002). Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. Journal of psychosomatic research, 53(5), 985–993. [DOI] [PubMed] [Google Scholar]
- Stice E, & Whitenton K (2002). Risk factors for body dissatisfaction in adolescent girls: a longitudinal investigation. Developmental psychology, 38(5), 669. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, … & Wilfley DE (2006). Prevention of eating disorders in at-risk college-age women. Archives of general psychiatry, 63(8), 881–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiggemann M, & Lynch JE (2001). Body image across the life span in adult women: the role of self-objectification. Developmental psychology, 37(2), 243. [DOI] [PubMed] [Google Scholar]
- van den Berg PA, Mond J, Eisenberg M, Ackard D, & Neumark-Sztainer D (2010). The link between body dissatisfaction and self-esteem in adolescents: Similarities across gender, age, weight status, race/ethnicity, and socioeconomic status. Journal of Adolescent Health, 47(3), 290–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg P, & Neumark-Sztainer D (2007). Fat′ n happy 5 years later: Is it bad for overweight girls to like their bodies?. Journal of Adolescent Health, 41(4), 415–417. [DOI] [PubMed] [Google Scholar]
- Whitbourne SK, & Skultety KM (2002). Body image development: Adulthood and aging. Body image: A handbook of theory, research, and clinical practice, 83–90.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


