Abstract
Metastatic pulmonary calcification is a metabolic lung disease that occurs due to a prolonged hypercalcemic state where calcium salts precipitate into numerous foci or nodules of fluffy calcifications in the lung apices, usually bilaterally. Calcifications can also occur in other organs such as in the stomach and the kidneys. It is often underdiagnosed and is usually associated with end stage renal failure and resultant secondary hyperparathyroidism. Nevertheless, it is rarely reported in the postcardiac surgery status and cardiac transplant patients. We present a case of a 15-year-old male patient with a recent history of cardiac transplant due to a complex congenital heart disease where findings of extensive metastatic pulmonary calcifications were seen a routine follow-up chest radiograph. Clinical manifestations of metastatic pulmonary calcifications can range from having no symptoms or mild dyspnea on exertion to fulminant respiratory failure. Therefore, early recognition of imaging features and initiation of proper management is crucial to the patient's outcome.
Keywords: Metastatic pulmonary calcification, Congenital heart disease, Cardiac transplant, Chest radiography, Computed tomography, Metabolic disease
Introduction
Metastatic pulmonary calcification (MPC) is considered to be a metabolic lung disease with disturbance in the calcium /phosphorus metabolism and its etiology is subdivided into benign and malignant causes [1], [2], [3]. It is seen most commonly in patients undergoing hemodialysis due to end stage renal disease and is often an underdiagnosed condition as almost 60-75% of patients on hemodialysis appear to have MPC at autopsy [4,5]. Metastatic pulmonary calcifications can also be seen in patients with orthotopic liver transplantation and primary hyperparathyroidism and in malignant etiologies such as in patients with multiple myeloma and osteoblastic metastatic tumors to the lungs [6]. Nevertheless it has been rarely described in cardiac transplant patients [7,8]. We present a case of a 15-year-old male patient who underwent a recent cardiac transplant surgery with an incidental finding of metastatic pulmonary calcification on plain chest radiograph and serial computed tomography images showing the progression of the disease.
Case report
A 15-year-old middle-eastern male patient presented to the outpatient clinic complaining of facial heaviness, nasal stuffiness and headache. He was a known case of severely dilated cardiomyopathy due to complex congenital heart disease with a recent cardiac transplant done abroad 11 months prior. He also had a previous history of Still's disease treated with interleukin I antagonists.
The patient had traveled abroad to the United States for a cardiac transplant after worsening of his cardiomyopathy related symptoms. During the perioperative period he was intubated and mechanically ventilated but continued to deteriorate despite biventricular assistant device placement and had required veno-arterial extra corporeal membrane oxygenation. He had more than 1 episode of intrathoracic hemorrhage postoperatively causing tamponade and required evacuation of hematoma formation twice. He had also required prolonged periods of mechanical ventilation and was finally extubated 2 months later.
The perioperative course was also complicated by episodes of sepsis requiring broad spectrum antibiotics but the patient eventually made a complete recovery and after discharge from the hospital had remained asymptomatic from respiratory point of view.
On clinical examination, he was oriented to time and place. Vitals were stable and oxygen saturation was 100% on room air. He did not have cyanosis. Chest auscultation was clear with no evidence of fine crepitations or rhonchi. Heart sounds were normal. Abdomen was soft and no pedal edema was observed.
Given the history of post-transplant immunocompromised state and ongoing sinus symptoms, the patient was admitted for further investigation. After a paranasal sinus computed tomography (CT) scan and ENT examination a fungal infection was ruled out and the patient was treated for acute sinusitis only.
However, during the work up his routine chest X-ray showed extensive bilateral ground glass haziness with fluffy foci of minute calcifications mainly in the upper and middle lung zones.
His lungs had appeared normal in the pretransplant chest radiograph at our hospital almost a year ago (Fig. 1A and B).
Fig. 1.
Postero-anterior chest radiograph (A) Pretransplant image showing enlarged cardiac shadow. Lungs and costophrenic angles appear clear. (B) Eleven months post-transplant image showing extensive ground glass haziness bilaterally with multiple fluffy foci of minute calcifications more pronounced in the upper and middle zones.
The laboratory work-up including complete blood count, renal and liver function tests were unrevealing. Corrected calcium, Vitamin D, and the parathyroid hormone levels were also within the normal limits. Venous blood gas at the time of admission was also unremarkable.
The pulmonary function tests were consistent with a pattern of restrictive lung disease changes.
A contrast enhanced CT scan of the chest in 1.5 mm axial cuts with reformatted sagittal and coronal reconstructions was done and showed bilateral predominantly upper lobe ground glass haziness with extensive minute foci of calcification giving Hounsfield units of approximately 680. Upon retrospective review of the perioperative images, the 2-week post-transplant chest CT done abroad showed early evidence of calcification in the lungs which has progressed further on the 2-month follow-up CT and was significantly worse in the subsequent CT done at our facility at 11 months post-transplant (Figs. 2 and 3).
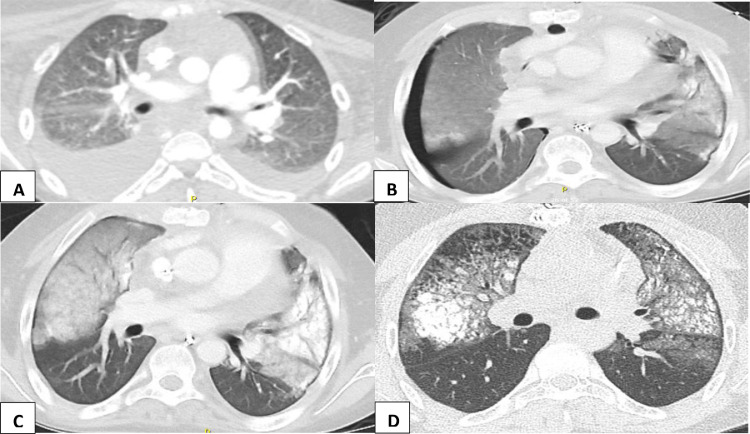
Fig. 2.
Axial contrast-enhanced CT scan of the chest in lung window at the level of the aortic root. (A) Preoperative state showing bilateral pleural effusion. No evidence of pulmonary ground glass opacities or calcification. (B) Two weeks post-transplant showing right-sided pneumothorax. Bilateral areas of ground glass haziness and minimal development of subpleural parenchymal calcification. (C) Two months post-transplant showing dense consolidation and an increase in the parenchymal calcifications. (D) Eleven months post-transplant showing further interval progression of the parenchymal metastatic calcifications.
Fig. 3.
(A-C) Sagittal, axial and coronal CT scan of the chest in bone window showing fluffy scattered calcifications in the upper lobes and superior aspect of the lower lobes bilaterally.
The imaging features were consistent with the diagnosis of metastatic pulmonary calcification. The patient was treated for acute sinusitis and then discharged with close monitoring and follow-up by the respiratory team .
Discussion
Pulmonary calcifications in postcardiac surgery patients are not uncommon and are usually dystrophic, focal or asymmetrically distributed as a sequela of respiratory infections, hemorrhage or even infarction in the perioperative period. However, metastatic pulmonary calcification has also been reported rarely in this patient population [1].
The exact pathogenesis of these calcific deposits is not known [8]. However, it is hypothesized that calcium salts crystalize and precipitate in the alveolar septa, blood vessels, bronchi and bronchioles [7,9]. Calcification of chest wall vasculature has also been frequently observed and aids in the diagnosis of MPC [1,2]. The metastatic calcifications can also occur in other organs such as in the stomach and kidneys but are most commonly seen involving the lungs [4,9]. Several theories have been proposed as to the aggravating factors of this disease, all of which include an elevated blood calcium level. Nevertheless, metastatic calcifications have been reported in patients with normal or low serum calcium levels [6].
Prolonged hypercalcemia can occur in the postcardiac transplant setting either due to a transient episode of acute renal failure or after receiving large amounts of blood products which increases plasma citrate levels causing hypocalcemia and in turn stimulating an increased secretion of parathyroid hormone causing secondary hyperparathyroidism and high calcium levels. Also, during cardiac surgery in pediatric patients the ionized calcium levels are kept at higher levels of normal of a value of approximately 1.3-1.6 mmol/l [7].
The pattern of deposition which favors the upper lobes could be partly explained due to the higher ventilation-perfusion ratio in the lung apices leading to a lesser arterial blood partial pressure of carbon dioxide and a higher alkalinity (higher pH) providing a favorable setting for calcium deposition [1]. Similarly prolonged intubation with assisted ventilation also raises the alkalinity and promote calcium crystallization and can be one of the contributing factors for the development of MPC in our patient [7].
Most patients with MPC are either asymptomatic or present with mild shortness of breath and a nonproductive cough . Although a more fulminant course with hypoxemia and acute respiratory failure has also been reported [2,5]. Pulmonary function tests are initially normal but might show restrictive lung functions later on in the disease as the lung vital capacity is inversely proportional to the severity of lung calcifications [4,9].
The routine chest X-ray is not sensitive in early disease and may be normal however a dual energy X-ray has better sensitivity and higher diagnostic yield at detecting mild MPC [5,10]. Patchy and confluent air space opacities or diffuse nodules with or without foci of calcifications are the usual findings on the X-ray imaging. Suspicion of metastatic pulmonary calcifications in the setting of hypercalcemia should be raised if the chest X-ray findings persist and do not resolve with time [1,2,10].
High resolution computed tomography of the chest in 1-mm sections (mediastinal window) is more specific and sensitive than chest radiography in visualizing the calcifications in MPC [2]. The main role of HRCT is early recognition of pulmonary calcifications in high risk individuals, thereby narrowing the differential diagnosis and precluding the necessity for surgical biopsy [2,6].
Calcific foci are usually observed bilaterally and most commonly in the upper and middle lobes [7,2]. Dual-energy computed tomography with pulmonary calcium suppression technique could also aid in the diagnosis and confirmation of MPC. [11].
Different patterns of MPC may be appreciated on HRCT scan of the lungs and include the presence of numerous diffuse calcified nodules, patchy ground glass opacification or confluent hyperdense consolidation [1], [2], [3].
Technetium 99m Methylene Diphosphonate nuclear scan (TC-99m MDP) may a be a useful tool in early detection of this metabolic disease which usually shows intense uptake of the tracer in the involved lung parenchyma [3,4,8]. 99mTc MDP scintigraphy can evaluate metastatic calcification in other organs concurrently. Although the scintigraphy appears to be more sensitive at detecting MPC, CT scan has the added advantage of evaluating the whole thorax and lung parenchyma in detail and so may help identify any alternate diagnosis [6].
As for most lung diseases, magnetic resonance imaging does not have a major role in the diagnosis of MPC. Calcifications appear hypointense on T1 and isointense on T2 and the signal is somewhat variable depending on the calcium concentration [4].
The main differential diagnosis of MPC includes pulmonary microlithiasis and hypersensitivity pneumonitis in addition to occupational lung diseases, calcific metastases and a previous history of varicella lung infection [1,8].
The management of MPC involves correcting the underlying etiology, especially the elevated calcium levels [1]. Complete resolution of the calcifications has been reported in a small number of cases after a few months of treatment for the secondary causes of hyperparathyroidism while some cases are reported to follow more a fulminant course [4,9]. Hence, early diagnosis and initiation of proper management is crucial to the patient's prognosis and may also aid in avoiding unnecessary procedures and therapeutic errors [7,2].
In conclusion, metastatic pulmonary calcifications in a pediatric postcardiac transplant setting is extremely rare. It has been reported in four other case reports where MPC was attributed to therapy with large doses of calcium and postsurgical acute renal failure [7,5,10,12]. Our patient was asymptomatic at presentation with no history of acute renal failure, however occult or undetected transient hypercalcemia in the perioperative period cannot be ruled out as a causative factor. Recognizing early imaging features on plain radiography and computed tomography is essential for diagnosis and initiation of the proper treatment.
Consent
Obtained from patient.
Footnotes
Conflicts of interest: The authors declare no conflicts of Interest.
Contributor Information
Dana AlNuaimi, Email: dr.danas@hotmail.com.
Mahmoud ElKaissi, Email: elkaism@clevelandclinicabudhabi.ae.
Ali Wahla, Email: wahlaa@clevelandclinicabudhabi.ae.
Irfan Shafiq, Email: shafiqi@clevelandclinicabudhabi.ae.
Shareefa Abdulghaffar, Email: sabdulghaffar@dha.gov.ae.
References
- 1.Belém LC, Zanetti G, Souza AS, Hochhegger B, Guimarães MD, Nobre LF. Metastatic pulmonary calcification: state-of-the-art review focused on imaging findings. Respir Med. 2014;108(5):668–676. doi: 10.1016/j.rmed.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 2.Belém LC, Souza CA, Souza AS, Jr, Escuissato DL, Hochhegger B, Nobre LF. Metastatic pulmonary calcification: high-resolution computed tomography findings in 23 cases. Radiologia Brasileira. 2017;50(4):231–236. doi: 10.1590/0100-3984.2016-0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torres PPTES. Metastatic pulmonary calcification: contribution of imaging to noninvasive diagnosis. Radiol Bras. 2017;50(5) doi: 10.1590/0100-3984.2017.50.5e2. VII–VIII. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peungjesada S, Baskin MH, Winer-Muram HT. Metastatic pulmonary calcification. Appl Radiol. 2016;45(1):31–33. [Google Scholar]
- 5.Berezowska S, Poellinger A, Ulmer F, Trippel M. Respiratory failure due to rapidly progressive metastatic lung calcifications after heart transplantation in a 6-year-old girl. Am J Respir Crit Care Med. 2019;01;200(9):1177–1178. doi: 10.1164/rccm.201812-2321IM. [DOI] [PubMed] [Google Scholar]
- 6.Chan ED, Morales DV, Welsh CH, McDermott MT, Schwarz MI. Calcium deposition with or without bone formation in the lung. Am J Respir Crit Care Med. 2002;165(12):1654–1669. doi: 10.1164/rccm.2108054. [DOI] [PubMed] [Google Scholar]
- 7.Sonavane S, Guleria S, Crowe DR, Steenwyk B, Singh S. Progressive lung calcification after orthotopic heart transplant. Pediatr Radiol. 2015;45(1):124–128. doi: 10.1007/s00247-014-3023-z. [DOI] [PubMed] [Google Scholar]
- 8.Yatera K, Kawanami T, Ishimoto H, Mukae H. Progressive metastatic pulmonary calcification after successful renal transplantation. Eur Respirat Rev. 2013;22(127):98–99. doi: 10.1183/09059180.00007712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bein M, Lee D, Mink J, Dickmeyer J. Unusual case of metastatic pulmonary calcification. Am J Roentgenol. 1979;132(5):812–816. doi: 10.2214/ajr.132.5.812. [DOI] [PubMed] [Google Scholar]
- 10.Mani TM, Lallemand D, Corone S, Mauriat P. Metastatic pulmonary calcifications after cardiac surgery in children. Radiology. 1990;174(2):463–467. doi: 10.1148/radiology.174.2.2404318. [DOI] [PubMed] [Google Scholar]
- 11.Fehrmann A, Borrega J, Holz J, Shapira N, Doerner J, Boell B. Metastatic pulmonary calcification: first report of pulmonary calcium suppression using dual-energy CT. Radiol Case Rep. 2020;15(7):900–903. doi: 10.1016/j.radcr.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morrison ML, Casey F, Paterson A, Shields M. Postoperative pulmonary calcification in a child with truncus arteriosus. BMJ Case Rep. 2013;2013(bcr2013009793):1–3. doi: 10.1136/bcr-2013-009793. [DOI] [PMC free article] [PubMed] [Google Scholar]