Abstract
Background/purpose
Several factors cause relapse of orthodontically de-rotated teeth after appliance removal. Circumferential supracrestal fiberotomy (CSF) may release the tension on the supra-alveolar fibers following tooth de-rotation, thereby reducing the relapse risk. However, careful identification of the amount and location of relapse enables proper clinical evaluation. We aimed to determine the amount of orthodontic relapse following CSF for de-rotated anterior teeth.
Materials and methods
Eleven patients with 90 orthodontically de-rotated anterior teeth were enrolled. CSF was performed after orthodontic treatment, during fixed retainer placement. Rotational correction and relapse were measured on three casts (preorthodontic treatment, cast 1; postorthodontic treatment + CSF, cast 2; and 12-month follow-up, cast 3). The Wilcoxon test was used to assess significant differences in the tooth rotation angles between casts 1 and 2 and casts 2 and 3. The relationship between the magnitude of relapse and pretreatment severity of rotation was assessed by the point biserial correlation test. The Mann-Whitney U test helped in identifying significant differences in the amount of relapse between maxillary and mandibular teeth.
Results
The mean amount of rotational correction was 14.05°, while the mean amount and percentage of relapse were 1.1° and 10.8%, respectively [0.81° (8%) and 1.44° (14%) for maxillary and mandibular teeth, respectively]. The relapse amount was proportional to the pretreatment rotation severity, and it was larger for the mandibular canines. There was no significant difference in the amount of relapse between the maxillary and mandibular teeth (P = 0.07).
Conclusion
Post-treatment rotational relapse of anterior teeth subjected to CSF was minimal and statistically insignificant after 1 year of follow-up. This validates the promising results of CSF when combined with appropriate mechanical retention for an adequate period.
Keywords: Cohort study, Mandibular canines, Relapse, Tooth rotation, Fiberotomy
Abbreviations: CSF, Circumferential supracrestal fiberotomy
1. Introduction
It is important to prevent the relapse of orthodontically treated teeth to their pretreatment positions for successful orthodontic treatment outcomes. Several factors may contribute to orthodontic relapse, including unfavorable skeletal growth and tissue rebound after orthodontic force release (Lovatt et al., 2008). Compared with teeth displaced in other ways, rotated teeth are more likely to relapse to their original positions after orthodontic appliance removal.
The role of the periodontium in the relapse of orthodontically rotated teeth has been extensively investigated (Lovatt et al., 2008, Redlich et al., 1996, Lv et al., 2009). Many investigators have demonstrated that relapse following orthodontic treatment is caused by the lack of reorganization and subsequent reorientation of the supracrestal periodontal fibers. Redlich et al. demonstrated tearing, ripping, disorganization, lateral spacing, and an increase in the diameter of the gingival fibers after tooth rotation and retention. The authors concluded that these patterns were incompatible with stretching (Redlich et al., 1996, Lv et al., 2009).
Several strategies have been proposed for the prevention of relapse, including a prolonged postorthodontic retention period (preferably with a fixed retainer), over-rotation in the opposite direction, and equilibration of the occlusion, which can overcome the limitations of retention (Lovatt et al., 2008). Edwards (1968) reported a simple and efficacious surgical technique that could attenuate the presumed influence of supracrestal periodontal fibers on rotational relapse. Using this technique, the gingival fibers were surgically severed after tooth rotation, followed by 2 months of mechanical retention (Edwards, 1968, Hansson, 1976). Several other studies (Retain, 1959, Beertsen, 1979) have shown that these post-treatment changes may originate in the fibrous network of the periodontium above the marginal alveolar bone. These fibers have little ability to rearrange and adapt to the corrected position, even with a long period of mechanical retention (Retain, 1959, Beertsen, 1979, Block et al., 1998). These findings led us to speculate that circumferential supracrestal fiberotomy (CSF) would release the tension on the supra-alveolar fibers following tooth rotation, thereby reducing the risk of rotational relapse (Lv et al., 2009). Further studies have validated the effect of CSF on reducing this type of relapse (Block et al., 1998, Dhingra et al., 2013, Littlewood et al., 2006). However, it is important to note the amount and location of relapse for proper clinical evaluation. The long-term stability after CFS has been documented in a few studies (Edwards, 1988, McNamara et al., 2001, Gokhale et al., 2015). Edwards evaluated the preventive effects of CSF on orthodontic relapse over a 15-year period by comparing patients who received CSF with those who did not. CSF was performed for both the maxillary and mandibular teeth. The mean amount of relapse in the CSF group was approximately 29% lesser than that in the control group, and the difference between groups was statistically significant (Edwards, 1988). To the best of our knowledge, there is little research on the magnitude of rotational relapse following CSF. The aim of this study was to determine the amount of orthodontic relapse following circumferential CSF performed for de-rotated anterior teeth.
2. Materials and methods
This study was conducted in June 2017, in accordance with the 2013 revision of the Helsinki Declaration of 1975. The protocol was approved by the Institutional Committee of Research Ethics, and permission for data collection was granted by the institutional review board. The study purpose and procedures were explained in the informed consent form, which emphasized the right to self-determination, confidentiality and anonymity, and the benefits and risks of the study procedures. All patients read this form and provided written consent to undergo the treatment, including CSF. Numerical codes replacing the participants’ names were used to ensure confidentiality.
Eleven patients (six men and five women) with a mean age of 23 years (range: 18–26 years) who had undergone corrective tooth de-rotation during orthodontic treatment at a private dental clinic in Riyadh, Saudi Arabia were recruited. None of the patients had a significant medical history, including diabetes, smoking, pregnancy, and autoimmune diseases, and all had rotated anterior teeth in either of the two arches. The exclusion criteria were as follows: buccolingual displacement, growth modification, arch expansion, unilateral extraction, extraction of one or more anterior teeth, cross bite, and/or lingual tilting of the mandibular first molar.
Orthodontic treatment involved the application of a preadjusted edgewise appliance with a 0.022-inch slot in all cases. Over-rotation was not achieved in any case. The average duration of orthodontic treatment was 24 months. All patients achieved Angle class I molar and canine relationships with preservation of the midline. A fixed retainer (0.016 Australian wire) was used with a mean retention period of 13 (range, 3–18) months. All patients were treated by the same orthodontist (N.J.) and referred to the same periodontist (A.R.) for CSF.
2.1. Surgical procedure
CSF was performed for each arch after the anteriorly rotated teeth were appropriately aligned to their ideal positions and the fixed retainer was placed. All patients had well-controlled oral hygiene and no signs of gingival inflammation or pockets around the target teeth at the time of surgery.
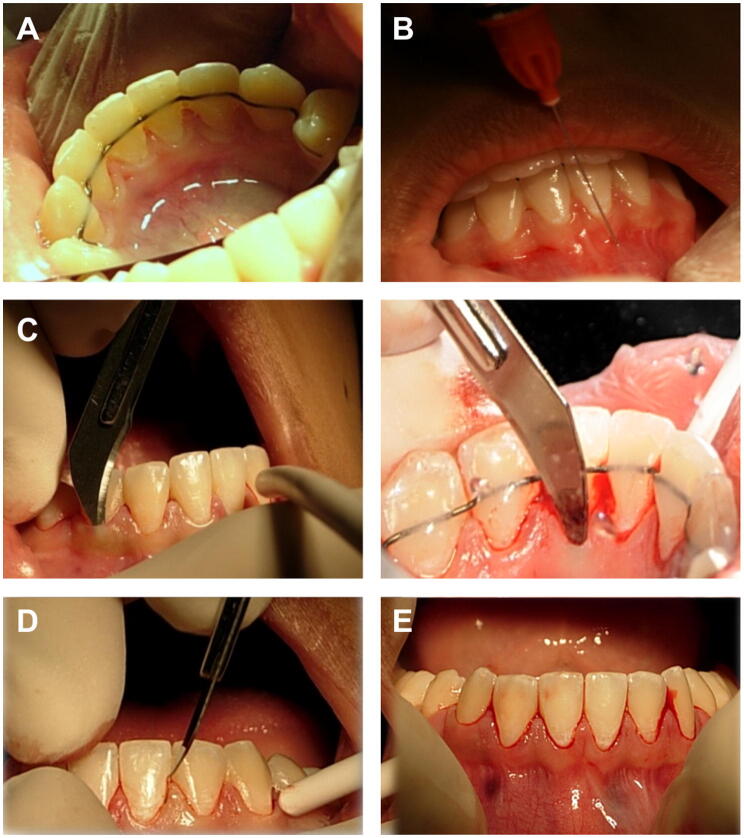
Lidocaine 5% ointment was applied to the gingiva for topical anesthesia, followed by local infiltration with lidocaine (1:100.000 epinephrine). Using a No. 15 or No. 12 blade, a crevicular (sulcular) incision was made through the gingival crevice of the aligned tooth down to the level of the alveolar crest. Keeping the blade close to the cementum and parallel to the root, the incision was extended down to the crestal bone, passing circumferentially from the labial surface to the lingual surface and including the proximal surface. All the supracrestal fibers around each de-rotated tooth were severed (Fig. 1). At the end of CSF, the teeth were irrigated with saline, followed by pressure application to the labial and lingual surfaces for 5 min using cotton gauze. Fixed retainer placement and CSF were performed at the same dental visit. No periodontal packs were used, and healing was uneventful. Postoperative follow-up evaluations were performed by the periodontist (A.R). None of the patients reported postoperative discomfort or any noticeable change in the surgical sites at the 1-week follow-up appointment.
Fig. 1.
Steps of the circumferential supracrestal fiberotomy (CSF) procedure. (A) Mandibular teeth are aligned after orthodontic treatment with the fixed retainer in place. (B) Soft tissue local anesthesia is achieved by labial and lingual infiltration. (C) No. 12 blade utilized to perform crevicular (sulcular) incision to release the supra-crestal fibers on the labial and lingual side with good wrest support. (D) proximal incision to release the trans-septal fibers. (E) Facial view of the lower teeth after the release of all supra-crestal fibers.
2.2. Casts and measurements
The following three casts were fabricated for each patient: cast 1 (pretreatment cast), obtained prior to orthodontic treatment at the initial examination visit; cast 2 (post-treatment + CSF), obtained after CSF and placement of the fixed retainer; and cast 3 (12 months after retention), obtained at the 12-month follow-up visit after removal of the fixed retainer. All casts were coded for blinding purposes.
All teeth included in the study were marked on each arch on the three casts, and a high-resolution photocopy was made for each cast in the transverse plane. To avoid distortion of the anterior teeth, each cast was confirmed to be in contact with the glass pad of the machine during photocopying. All casts were photocopied by the same operator (R.J.).
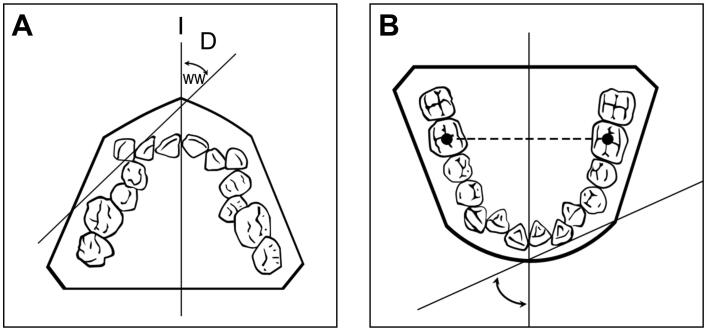
Several parameters were assessed on the copies of each cast. The degree of rotation (D) for each anterior tooth of interest in the maxillary arch was measured by using the median palatal suture line (P) as a fixed reference line and drawing an incisal line that passed through the incisal edge of each target tooth. The angle formed by the incisal line and the median palatine line determined the degree of rotation of the target tooth. Unlike the maxillary arch, the mandibular arch has no stable reproducible landmarks, so a line connecting the middle fossa of the first molar on each side was drawn to represent the intermolar width line. The treating orthodontist confirmed that this line was stable in all cases throughout the treatment period, and that it was the most stable landmark in the mandibular arch after orthodontic treatment. A line (W) perpendicular to the previous (intermolar width) line was drawn and chosen as the reference line for measurement of the mandibular anterior teeth. The incisal line for each target mandibular tooth was drawn as described above. The angle formed by the incisal line and the lower reference line determined the degree of rotation of that tooth (Fig. 2A and B).
Fig. 2.
(A) Schematic drawing illustrating maxillary tooth measurements. (B) Schematic drawing illustrating mandibular tooth measurements.
The angle of rotation of each target tooth was measured in degrees on casts 1, 2, and 3. The degree of rotational correction (C) needed to rotate the tooth from its pretreatment position into the correctly aligned position relative to the adjacent teeth was measured as the difference between the angle measured for a rotated tooth on cast 1 (D1) and that measured for the same tooth on cast 2 (D2) after alignment (i.e., C = D1 – D2). The amount of relapse (R) in each aligned tooth was determined by calculating the difference between the angle of the aligned tooth measured on cast 2 and that of the same tooth measured on cast 3 (D3) at the 12-month post-retention follow-up visit (i.e., R = D3 – D2). The percentage of relapse (R%) relative to the corrective movement was calculated as follows: R% = (R ÷ C) × 100. The mean percentage of relapse was calculated by pooling the percentage of relapse for each individual tooth.
2.3. Severity of rotation
Before treatment, the severity of rotation for each tooth was categorized according to the amount of angular change required to rotate it into an appropriate contact relationship with adjacent teeth, using the method devised by Retain et al (1959): mild (0°–10°), moderate (>10° to <20°), and severe (≥20°).
2.4. Intra-examiner reliability
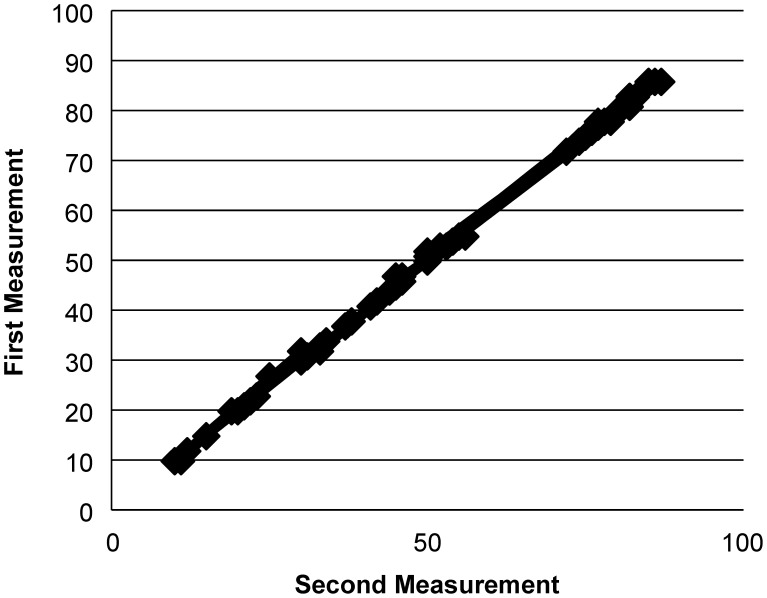
All measurements were performed by a single examiner who was blinded to the type of cast. For the assessment of intra-examiner reproducibility and reliability, the examiner measured four randomly selected casts (36 rotated teeth) on two occasions separated by a 1-week interval.
2.5. Statistical analysis
Spearman’s rank correlation test was used to estimate the correlation between the first and second readings and confirm the intra-examiner reliability. Descriptive statistical analysis was performed to determine the significance of the amount of rotational correction needed for correct alignment, the amount of post-retention relapse, and the percentage of relapse for all teeth in the overall sample, each arch, and each tooth type in each arch. The Wilcoxon test for dependent variables was used to compare the rotation angle for all teeth between pretreatment cast 1 and post-treatment cast 2. The same test was used to compare the rotation angle for all teeth between cast 2 and cast 3. The point biserial correlation test was used to assess the relationship between the magnitude of relapse and the pretreatment severity of rotation. The Mann-Whitney test was used to identify any significant difference in the amount of relapse between the maxillary and mandibular teeth. All statistical analyses were performed using SPSS for Windows version 16.0 (SPSS Inc., Chicago, IL, USA). A P-value of < 0.05 was considered statistically significant.
3. Results
The study sample comprised 90 rotated anterior (central incisors, lateral incisors, and canines) teeth (52 in 11 maxillary arches and 38 in eight mandibular arches). Eight of the 11 patients had class I malocclusion, two had class II division 1 malocclusion, and one had class III malocclusion. The severity of crowding varied among cases.
Spearman’s rank correlation test found no significant difference between the two sets of measurements obtained by the examiner (r = −0.696, n = 6, P = 0.001). Thus, the intra-examiner reliability was good (Fig. 3).
Fig. 3.
Intra-examiner reliability.
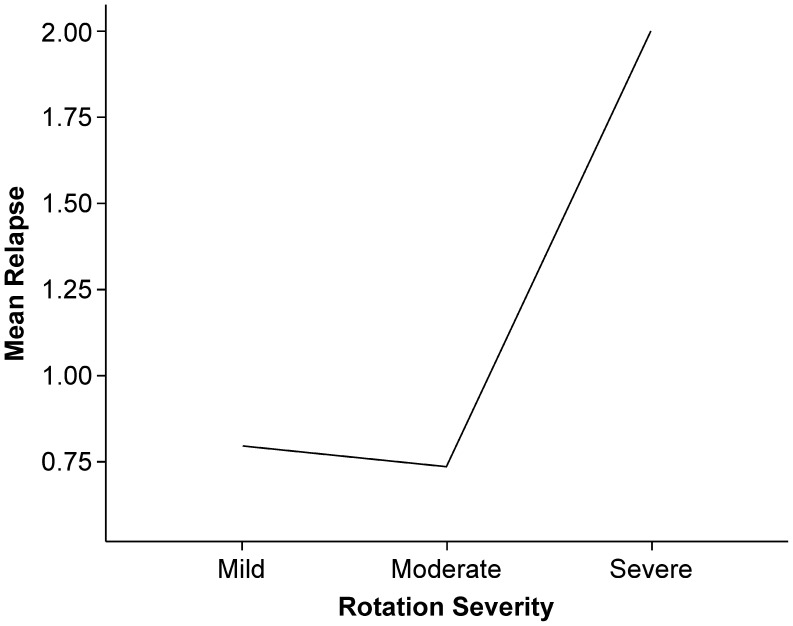
The mean degree of rotational correction of all 90 teeth was 14.05° (12.7°; range, 2°–92°), while the mean degree of post-retention rotational relapse was 1.1° (2.4°; range 0°–19°). The mean percentage of relapse relative to the original corrective movement was 10.8% (Fig. 4). There was a significant difference in the rotation angle for all teeth between casts 1 and 2 (P = 0.02; Wilcoxon test), whereas there was no significant difference between casts 2 and 3 (P = 0.19).
Fig. 4.
Representative case with an amount of post-retention relapse similar to the reported mean value of relapse. Relapse can be observed in the maxillary left central and lateral incisors on cast 3.
The pretreatment rotation was mild in 48 teeth and moderate or severe in 42 (Table 1). There was a linear relationship between the pretreatment severity of rotation and the amount of post-retention relapse; teeth with severe pretreatment rotation (≥20°) showed a greater amount of relapse during the post-retention period. However, there was no significant correlation between mild or moderate pretreatment rotation and the amount of relapse (Fig. 5).
Table 1.
Severity of rotation before treatment for all 90 teeth included in the study.
| Severity of rotation | Range | Mean | Teeth, n |
|---|---|---|---|
| Severe | 21°–92° | 33.6° | 22 |
| Moderate | 10°–19° | 13.7° | 20 |
| Mild | 0°–10° | 5.0° | 48 |
Fig. 5.
Relationship between relapse and the severity of rotation before treatment.
The mean amount of relapse for the 52 maxillary teeth was 0.81°, and the percentage of relapse relative to the original movement for these teeth was 8% (Table 2). The mean amount and percentage of relapse for the mandibular teeth were 1.44° and 14%, respectively; these were higher than the values for the maxillary teeth. There was no significant difference in the amount of relapse between the maxillary and mandibular teeth (P = 0.07).
Table 2.
Mean degree of rotational correction and rotational relapse and the percentage of relapse for each tooth type in each arch.
| Arch | Variable | C° | R° | R% |
|---|---|---|---|---|
| Maxillary* | All teeth (n = 32) | 14.59 | 0.81 | 8 |
| Canine (n = 17) | 9.4 | 0.41 | 6.1 | |
| Lateral incisor (n = 19) | 14.9 | 1 | 10.8 | |
| Central incisor (n = 16) | 19.8 | 10.6 | 7.6 | |
| Mandibular* | All teeth (n = 38) | 13.54 | 1.44 | 14 |
| Canine (n = 11) | 12.2 | 2.9 | 17.8 | |
| Lateral incisor (n = 13) | 14.5 | 0.8 | 13.9 | |
| Central incisor (n = 14) | 13.1 | 1 | 12.3 |
The mandibular canines exhibited the highest percentage of relapse, followed by the mandibular lateral and central incisors. Overall, the magnitude of relapse was lesser for the maxillary teeth.
4. Discussion
The present findings are consistent with previous reports of a significant reduction in the relapse of orthodontically rotated teeth following CSF performed as an adjunct to mechanical retention (Dhingra et al., 2013, Littlewood et al., 2006, Young et al., 2013, Pinson and Strahan, 1974, Taner et al., 2000). Interestingly, by 12 months after retention, we found a mean relapse rate of 10.8% for teeth subjected to fiberotomy; this was similar to the rate in a controlled study reported by Crum and Andreasen (Crum and Andreasen, 1974), indicating the potentially stabilizing effect of fiberotomy on orthodontically rotated teeth.
The significant reduction in postoperative relapse in the present study is similar to that in earlier reports. Pinson and Starhan demonstrated a mean relapse of 8.5° in their fiberotomy group, which represented 25.5% of the original rotation after a retention period of at least 1 year (Pinson and Strahan, 1974). However, the mean relapse in their nonsurgical group was 16°, which represented 56.5% of the original rotation. Another study reported a significantly smaller amount of relapse in the fiberotomy group than in the control group (0.42° vs 5.75°) during 30 days of observation (Taner et al., 2000).
Our findings are similar to those of another study where CSF was less effective in the mandibular anterior segment than in the maxillary anterior segment at 8–9 years after retention (Crum and Andreasen, 1974). In the present study, a smaller percentage of relapse was found in the maxillary teeth, which possibly reflects the greater complexity and multifactorial potential for relapse in the mandibular anterior arch. Furthermore, the mandibular canines showed the highest amount of relapse, possibly because of the tendency of the intercanine width to return to its pretreatment value or the anterior component of force (Jahanbin et al., 2014, Wang et al., 2003, Kalra et al., 2013).
At the 12-month post-retention follow-up, we also found that almost all teeth except one exhibited mild rotation of 0°–8°; one tooth that was severely rotated (by 24°) before treatment showed moderate rotation (by 19°) and relapse from its alignment position at the post-retention follow-up. These findings indicate that the majority of teeth with moderate or severe rotation before treatment were only slightly rotated (by 1°–2°) after the retention period. Moreover, no tooth reverted completely to the pretreatment state. Finally, similar to the finding in a previous report (Cao et al., 2015), CSF did not cause any change in the marginal or attached gingiva.
The conventional surgical approach for CSF remains an acceptable method (Proffit, 2012). However, the use of a scalpel blade during the procedure can lead to poor patient acceptance rates and adverse effects such as postoperative pain and bleeding (Fricke et al., 1990). Therefore, minimally invasive approaches have been proposed to overcome these limitations. These include, but are not limited to, low-level laser therapy and laser-aided fiberotomy (Kim et al., 2010, Miresmæili et al., 2019). A clinical trial compared the effect of Er, Cr:YSGG laser-aided CSF with that of the conventional approach and found comparable outcomes in terms of the decrease in the tendency for rotational relapse (Miresmæili et al., 2019).
Limitations of this study include a relatively short observation period after the discontinuation of mechanical retention, the lack of a control group, and the use of mechanical retention only for the purpose of comparison with fiberotomy. In addition, no clinical periodontal parameters were examined for evaluation of the periodontal status and stability before and after the procedure. Therefore, the present findings should be confirmed in a larger clinical trial that includes an appropriate control group and a longer follow-up period and assesses all orthodontic and periodontal parameters.
5. Conclusion
In conclusion, post-treatment rotational relapse of anterior teeth subjected to CSF was minimal and statistically insignificant after 1 year of follow-up. This validates the promising results of CSF when combined with appropriate mechanical retention for an adequate period. While the amount of relapse in the maxillary teeth was generally lesser than that in the mandibular teeth, the difference was statistically insignificant.
These findings will enhance the understanding of both orthodontists and periodontists in terms of the importance of adjunctive fiberotomy for improving the long-term stability of de-rotated teeth in their new positions after treatment completion. It also provides a general idea about the expected relapse that could occur after retention and facilitates comparison of this relapse with that in cases without fiberotomy.
6. Ethical considerations
This study was conducted in June 2017, in accordance with the Helsinki Declaration of 1975, as revised in 2013.The protocol used in this series was approved by the Institutional Committee of Research Ethics at the College of Dentistry Research Center, King Saud University, Riyadh, Saudi Arabia (NF 2254). Permission to collect the data used in the study was granted by the institutional review board at King Saud University.
Declarations of Competing Interest
None.
Acknowledgments
Acknowledgements
The authors are grateful to Mr. Naser Al-Maflehi for his assistance with statistical analysis of and Mrs. Wennielou Dioneda for her valuable assistance during the surgical procedures. They would also like to thank the College of Dentistry Research Center (CDRC) and the Deanship of Scientific Research at King Saud University, Riyadh, Saudi Arabia for all the support provided during this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Peer review under responsibility of King Saud University.
References
- Beertsen W. Remodeling of collagen fibers in the periodontal ligament and the supra-alveolar region. Angle. Orthod. 1979;49:218–224. doi: 10.1043/0003-3219(1979)049<0218:ROCFIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Block R.W., Kerns D.G., Regennitter F.J., Kerns L.L. The circumferential supracrestal fiberotomy. Gen. Dent. 1998;46:48–54. [PubMed] [Google Scholar]
- Cao T., Xu L., Shi J., Zhou Y. Combined orthodontic-periodontal treatment in periodontal patients with anteriorly displaced incisors. Am. J. Orthod. Dentofacial. Orthop. 2015;148:805–813. doi: 10.1016/j.ajodo.2015.05.026. [DOI] [PubMed] [Google Scholar]
- Crum R.E., Andreasen G.F. The effect of gingival fiber surgery on the retention of rotated teeth. Am. J. Orthod. 1974;65:626–637. doi: 10.1016/0002-9416(74)90257-7. [DOI] [PubMed] [Google Scholar]
- Dhingra K., Vandana K.L., Girish P.V., Cobb C. Effect of 980-nm diode laser-aided circumferential supracrestal fiberotomy on fluorosed root surfaces. Angle. Orthod. 2013;83:425–430. doi: 10.2319/052212-419.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J.G. A study of the periodontium during orthodontic rotation of teeth. Am. J. Orthod. Dentofacial. Orthop. 1968;54:441–461. doi: 10.1016/0002-9416(68)90199-1. [DOI] [PubMed] [Google Scholar]
- Edwards J.G. A long-term prospective evaluation of the circumferential supracrestal fiberotomy in alleviating orthodontic relapse. Am. J. Orthod. Dentofacial. Orthop. 1988;93:380–387. doi: 10.1016/0889-5406(88)90096-0. [DOI] [PubMed] [Google Scholar]
- Fricke L.L., Rankine C.A. Comparison of electrosurgery with conventional fiberotomies on rotational relapse and gingival tissue in the dog. Am. J. Orthod. Dentofacial. Orthop. 1990;97:405–412. doi: 10.1016/0889-5406(90)70112-P. [DOI] [PubMed] [Google Scholar]
- Gokhale S., Byakod G., Gupta G., Muglikar S., Gupta S. Effects of laser-aided circumferential supracrestal fiberotomy on relapse of orthodontically treated teeth: A pilot study. J. Dent. Lasers. 2015;9:16–22. [Google Scholar]
- Hansson C. Linder-Aronson S. Periodontal health following fibrotomy of the supra-alveolar fibers. Scand. J. Dent. Res. 1976;84:11–15. doi: 10.1111/j.1600-0722.1976.tb00455.x. [DOI] [PubMed] [Google Scholar]
- Jahanbin A., Ramazanzadeh B., Ahrari F., Forouzanfar A., Beidokhti M. Effectiveness of Er: YAG laser-aided fiberotomy and low-level laser therapy in alleviating relapse of rotated incisors. Am. J. Orthod. Dentofacial. Orthop. 2014;146:565–572. doi: 10.1016/j.ajodo.2014.07.006. [DOI] [PubMed] [Google Scholar]
- Kalra A., Jaggi N., Bansal M. Comparison of rate of canine retraction into recent extraction site with and without gingival fiberotomy: a clinical study. J. Contemp. Dent. Pract. 2013;14:419–426. doi: 10.5005/jp-journals-10024-1338. [DOI] [PubMed] [Google Scholar]
- Kim S.J., Paek J.H., Park K.H., Kang S.G., Park Y.G. Laser-aided circumferential supracrestal fiberotomy and low-level laser therapy effects on relapse of rotated teeth in beagles. Angle. Orthod. 2010;80:385–390. doi: 10.2319/051609-268.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlewood S.J., Millett D.T., Doubleday B., Bearn D.R., Worthington H.V. Orthodontic retention: a systematic review. J. Orthod. 2006;33:205–212. doi: 10.1179/146531205225021624. [DOI] [PubMed] [Google Scholar]
- Lovatt R., Goonewardenet M., Tennant M. Relapse following orthodontic rotation of teeth in dogs. Aust. Orthod. J. 2008;24:5–9. [PubMed] [Google Scholar]
- Lv T., Kang N., Wang C., Han X., Chen Y., Bai D. Biologic response of rapid tooth movement with periodontal ligament distraction. Am. J. Orthod. Dentofacial. Orthop. 2009;136:401–411. doi: 10.1016/j.ajodo.2007.09.017. [DOI] [PubMed] [Google Scholar]
- Miresmæili A.F., Mollabashi V., Gholami L., Farhadian M., Rezaei-Soufi L., Javanshir B., Malekshoar M. Comparison of conventional and laser-aided fiberotomy in relapse tendency of rotated tooth: A randomized controlled clinical trial. Int. Orthod. 2019;17:103–113. doi: 10.1016/j.ortho.2019.01.018. [DOI] [PubMed] [Google Scholar]
- McNamara J.A., Brudon W.L., Kokich V.G. Needham Press; Needham: 2001. Orthodontics and Dentofacial Orthopedics. [Google Scholar]
- Pinson R.R., Strahan J.D. The effect on the relapse of orthodontically rotated teeth of surgical division of the gingival fibers – pericision. Br. J. Orthod. 1974;1:87–91. doi: 10.1179/bjo.1.3.87. [DOI] [PubMed] [Google Scholar]
- Proffit W.R., Fields H.W., Jr, Sarver D.M. fifth ed. Elsevier; Mosby: 2012. Contemporary Orthodontics. [Google Scholar]
- Redlich M., Rahamim E., Gaft A., Shoshan S. The response of supraalveolar gingival collagen to orthodontic rotation movement in dogs. Am. J. Orthod. Dentofacial. Orthop. 1996;110:247–255. doi: 10.1016/s0889-5406(96)80007-2. [DOI] [PubMed] [Google Scholar]
- Retain K. Tissue rearrangement during retention of orthodontically rotated teeth. Angle. Orthod. 1959;29:105–113. [Google Scholar]
- Taner T.U., Haydar B., Kavuklu I., Korkmaz A. Short-term effects of fiberotomy on relapse of anterior crowding. Am. J. Orthod. Dentofacial. Orthop. 2000;118:617–623. doi: 10.1067/mod.2000.110637. [DOI] [PubMed] [Google Scholar]
- Wang, Z., Huang, C., Han, L., 2003. [Prognosis of utility of modified supracrestal fiberotomy and contact point reproximation in the treatment of anterior segment crowding]. Hua. Xi. Kou. Qiang. Yi. Xue. Za. Zhi. 21, 36-38 (Article in Chinese). [PubMed]
- Young L., Binderman I., Yaffe A., Beni L., Vardimon A.D. Fiberotomy enhances orthodontic tooth movement and diminishes relapse in a rat model. Orthod. Craniofac. Res. 2013;16:161–168. doi: 10.1111/ocr.12014. [DOI] [PubMed] [Google Scholar]