Abstract
Purpose
To report diagnostic and management challenges of a case of WHO Grade III glioma of the optic nerve occurring in an unusually young patient with more than 7 years of survival without recurrence.
Observations
An 18-year-old woman reported rapidly progressive vision loss in the right eye in the setting of a right optic nerve lesion, central retinal artery occlusion, central retinal vein occlusion, and neovascularization of the optic disc. An orbital MRI with contrast demonstrated enhancement of the intraocular, intraorbital, and intracanalicular portion of the right optic nerve. Biopsy of a portion of the intraorbital optic nerve was negative, however, biopsy of the intracranial optic nerve confirmed WHO Grade III glioma (anaplastic astrocytoma). Although the tumor was excised, there remained positive margins at the optic chiasm. The patient was then managed with a combination of radiation and temozolomide. Postoperatively, the initial neovascularization of the optic nerve that had resolved, re-emerged with gliosis. In this setting a concern for intraorbital tumor arose and the globe was enucleated, definitively ruling out neoplasm. The patient has remained tumor free seven years after resection.
Conclusions and importance
Malignant optic pathway glioma is rare and carries a high 5-year mortality rate. Diagnosis can be elusive given orbital MRI with contrast often appears to be non-specific. Inflammatory changes can be confounding such that a biopsy in the respective area will yield a negative pathologic result. Repeat biopsy is recommended if clinical suspicion is high. Combination treatment of optic nerve tumor resection, temozolomide and radiation has been effective in treating this patient who continues to be followed closely and has had no clinical or radiographic evidence of recurrence in over 7 years. The re-emergence of neovascularization with gliosis/fibrosis of the optic nerve, was driven by ischemia and further precipitated by radiation. To our knowledge this patient represents the youngest reported case of malignant optic nerve glioma with the longest reported survival in the literature to date (over seven years).
Keywords: Malignant optic nerve glioma, Temozolomide, Neovascularization of the optic nerve, Remission, Radiation
1. Introduction
Malignant optic pathway gliomas in adults were first described in 1973 by Hoyt.1 Since then over 70 cases have been reported in the literature.2, 3, 4 These tumors represent approximately one percent of all intracranial gliomas and affect women and men in a fairly equal distribution. Mean onset is in the sixth decade of life with the youngest case reported being age 22 years.3,4 Malignant optic pathway gliomas arise de novo from astrocytes within the optic nerve, the optic chiasm, or optic tracts and are quite challenging to diagnose and treat. Patients typically present with rapidly progressive unilateral vision loss of unclear etiology. Their clinical and radiologic features can mimic common entities such as optic neuritis, neurosarcoidosis, optic neuropathy, or retinal vascular occlusion,5 further delaying diagnosis and proper treatment of this condition. MRI findings include thickening of the optic nerve with contrast enhancement on T1-weighted images6; however, T2-weighted signal changes are relatively heterogeneous without a consistent pattern. Tissue biopsy is critical to confirm the diagnosis. The World Health Organization (WHO) classifies these malignant lesions according to their pathologic appearance, which include anaplastic astrocytomas (WHO grade III) and glioblastoma multiforme (WHO grade IV). Management includes surgical resection, chemotherapy, and radiation. Despite treatment, the mortality rate is extremely high with death usually within 1 year and the longest reported survival of 20 months.2, 3, 4
We share a challenging case of an 18-year-old woman who presented with vision loss in the setting of a WHO grade III optic pathway glioma. She remains tumor free seven years after optic nerve tumor resection, chemotherapy, and radiation. To our knowledge this patient represents the youngest reported case of malignant optic pathway glioma and the longest reported survival in the literature to date.
2. Case report
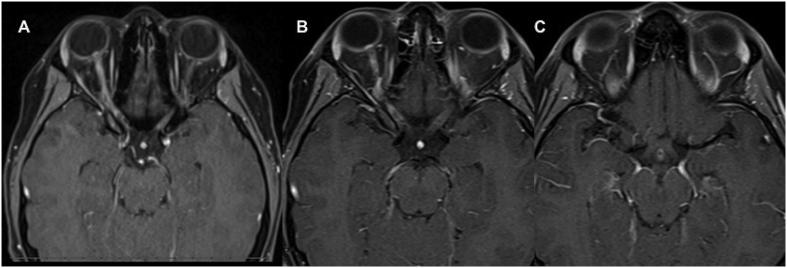
An 18-year-old woman with no significant past medical history presented to the neuro-ophthalmology clinic for a second opinion to evaluate rapidly progressive vision loss in her right eye. Symptoms began 3 months prior with difficulty focusing and photophobia in the affected eye. These symptoms progressed to complete vision loss within one month of their onset. Her cerebrospinal fluid and serologic evaluation at the time was exhaustive and inconclusive. Serum Epstein Barr IgG was elevated. Pertinent negative labs included ACE, ANA, Toxoplasmosis IgG, and NMO antibodies. MRI of the orbits showed enhancement of the intraocular, intraorbital and intracanalicular right optic nerve extending to the right chiasm without significant T2 hyperintensity (Fig. 1). She was treated with multiple courses of IV and oral steroids without effect.
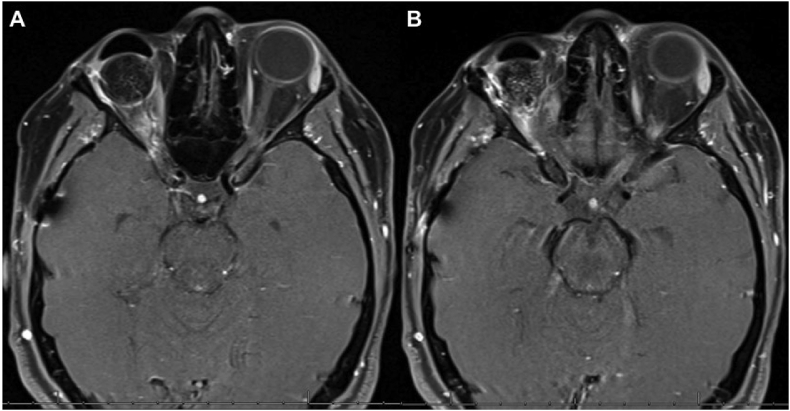
Fig. 1.
Sequential axial T1 weighted, fat saturated MRI with gadolinium images (A–C) on presentation demonstrating enhancement of the intraocular, intraorbital and intracanalicular right optic nerve extending toward the right chiasm.
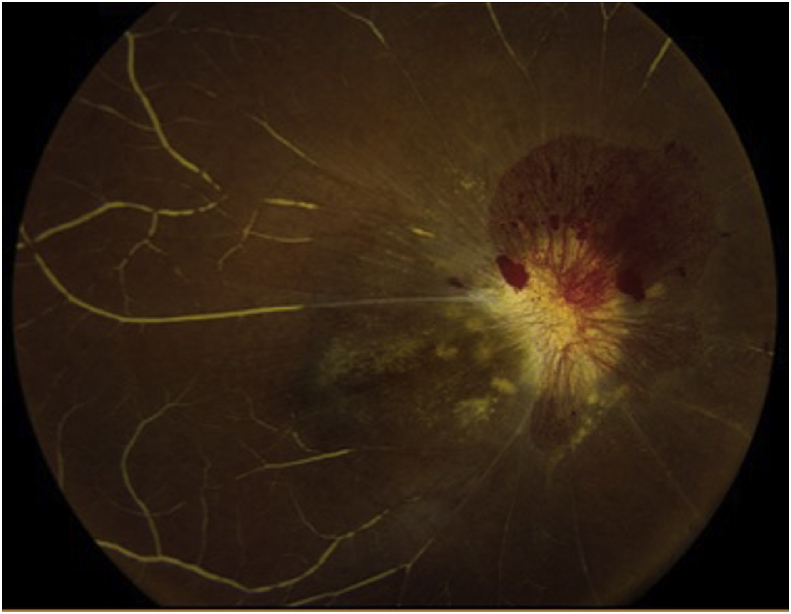
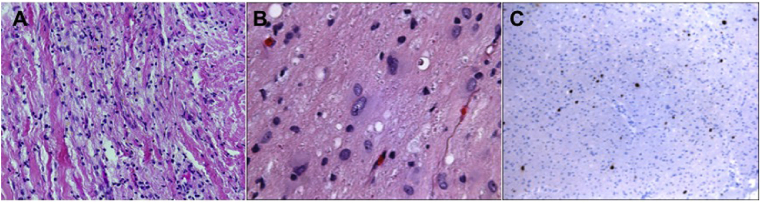
Examination confirmed NLP vision in the right eye with an amaurotic pupil. A pale, infiltrated, edematous right optic nerve was evident with neovascularization of the optic disc and absence of perfusion of the central retinal artery and vein (Fig. 2). Examination of the left eye was normal. A right optic nerve biopsy was performed through a transconjunctival orbitotomy, and pathology disclosed inflammation. Given high suspicion for malignancy, the intracranial optic nerve was biopsied through a superior craniotomy yielding a diagnosis of anaplastic astrocytoma (WHO Grade III). Globe sparing resection of the optic nerve was then undertaken using the technique described by Shriver et al.7 Tumor was identified in the intracranial and intracanalicular portions of the optic nerve (Fig. 3), but not intraorbital. Posterior margins at the level of the anterior optic chiasm were positive for malignant astrocytoma.
Fig. 2.
Right optic nerve upon presentation showing optic nerve edema, pallor, neovascularization, central retinal artery occlusion and central retinal vein occlusion, hyalinization of vessels, and cotton wool spots.
Fig. 3.
Hematoxylin and Eosin staining of initial intraorbital optic nerve biopsy specimen (A) showing lymphocytes consistent with chronic inflammation. Hematoxylin and Eosin staining of the intracranial optic nerve from subsequent craniotomy (B) demonstrates tumor consistent with anaplastic astrocytoma (WHO grade III) and Ki67 staining (C) showed an index of 4–5% at the chiasmal margin.
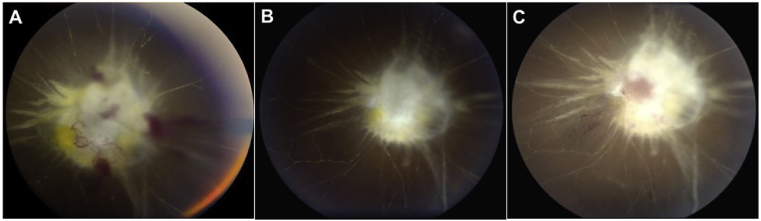
The patient underwent chemotherapy (6 month course of temozolomide) and radiation (60 Gray in 30 fractions). Serial examinations showed regression of neovascularization of the right optic nerve at postoperative month 3 (Fig. 4A) and postoperative month 6 (Fig. 4B) visits and MRI confirmed absence of disease. One year after surgical resection, the patient presented with intraocular optic nerve thickening and new hemorrhage at the level of the intraocular optic nerve (Fig. 4C). In light of concern for intraocular malignancy, the globe was enucleated. Review of pathology did not reveal intraocular tumor. The fornix was then rehabilitated with an ocular prosthesis. The patient has been followed clinically and with serial MRIs of the orbit (Fig. 5) for seven years without evidence of disease recurrence and with 20/20 vision and a full field of vision in her contralateral eye.
Fig. 4.
Optic nerve photos 3 months (A) and 6 months (B) after tumor resection showing regression of the neovascularization of the disc and glial fibrosis at the optic nerve head. The photo 12 months post resection (C) demonstrates the reappearance of neovascularization at the optic nerve head with more prominent fibrosis.
Fig. 5.
Post-operative sequential axial T1 weighted, fat saturated MRI with gadolinium images (A,B) showing a right orbital implant and absence of disease at the level of the chiasm 7 years after surgical resection, chemotherapy, and radiation.
3. Discussion
This youngest reported case of malignant optic pathway glioma with the longest reported survival highlights unique challenges of the disease process. In line with previously reported cases of malignant optic pathway gliomas, this patient presented with painless, subacute, unilateral vision loss, accompanied by an extensive, non-revealing serologic work up and neuroimaging that appeared consistent with a myriad of optic nerve pathologies, including but not limited to infectious, inflammatory, and neoplastic causes. Her initial treatment was also similar to previous reports in that a presumptive inflammatory optic nerve process was managed using steroid. Given the lack of response and findings on the MRI, an intraorbital approach to the optic nerve biopsy was deemed appropriate. Gross examination of the optic nerve intraoperatively was notable for black grainy material encasing the nerve within the optic nerve sheath, suggestive of a distant hemorrhagic event. The biopsy of this lesion only showed mild inflammation which was perplexing. Though a cause for a negative biopsy may result from a biopsy that includes only the dural sheath, the biopsy specimen contained optic nerve tissue. Given a raised index of suspicion, an intracranial biopsy was performed allowing for the diagnosis of a WHO grade III optic pathway glioma. Indeed, the importance of pursuing a re-biopsy diagnosing malignant optic nerve glioma to establish a definitive diagnosis cannot be overemphazied.
Resection of the intraorbital, intracanalicular, and prechiasmal optic nerve also confirmed that there was no tumor in the intraorbital portion of the optic nerve. Intralesional hemorrhage within optic pathway gliomas, though rare, has been reported in WHO grade I and II lesions,8, 9, 10, 11, 12 and less so in WHO grade III and IV lesions. This is in contrast to malignant gliomas in other locations which are known to hemorrhage as the tumors outgrow their blood supply and necrose or invade into a vessel. An intralesional bleed within the intracranial portion of the optic nerve, extending within the dural sheath of the intraorbital portion of the optic nerve may explain the preoperative MRI findings (diffuse enhancement and thickening of the optic nerve on T1 images with gadolinium) and the clinical findings of optic nerve head thickening, central retinal artery occlusion and central retinal vein occlusion.
Review of the permanent slides of the tumor pathology revealed anaplastic astrocytoma (WHO grade III) with positive microscopic margins at the posterior margins of the resection at the level of the anterior optic chiasm. This was in contrast to the clear margins obtained during intraoperative frozen section analysis. The Ki67 index at the posterior margin was 4–5%, suggesting a low mitotic rate. Ki-67, a nuclear antigen expressed during proliferative phases of the cell cycle, is useful in understanding the biologic behavior of tumors.13 In patients 18 years and younger with low grade gliomas, cause specific survival was significantly higher in patients with an average Ki-67 index less than 5%.14
Until recently, the mainstay of treatment after surgical resection of intracranial malignant gliomas is 54–60 Gray radiation to the surgical bed. The discovery of temozolomide, an oral alkylating agent found to have efficacy against malignant gliomas,15, 16, 17, 18 has provided a very effective therapy for malignant gliomas. The addition of temozolomide to radiation further potentiates tumoricidal activity in-vitro19 leading to increased survival in-vivo20 in patients with glioblastoma multiforme (WHO grade IV). Two year survival rates were 26.5% in the combined temozolomide and radiation group compared to 10.4% in the radiation alone group.
Several considerations were taken in determining the next step in management of our patient. Further resection would address residual tumor but would be associated with the morbidity of repeat intracranial surgery and the likelihood of permanent vision loss in the patient's only seeing eye as the resection encroaches on the optic chiasm. The low Ki-67 index in the microscopic positive margin prompted the team to proceed with temozolomide and radiation with plan for close monitoring.
The patient did remarkably well after surgical excision with eventual resolution of neovascularization at the optic nerve head at postoperative month 6. At postoperative year 1 visit, the recurrent neovascularization at the optic nerve head and worsening gliosis raised concern for intraocular tumor involvement despite the fact that the pathology from the previous surgical resection confirmed absence of tumor at the level of the intraorbital optic nerve. Intraocular malignant glioma has been described in the literature21 (albeit without pathological confirmation) presenting with a similar appearance to our patient, including a combined central retinal artery and vein occlusion with peripapillary changes. In close consultation with the patient, enucleation was advised given the vision was no light perception in this eye. This confirmed absence of intraocular tumor and supported the theory that the neovascularization was driven by ischemia which was further potentiated by her recent radiation treatment.
4. Conclusions
This case affirms malignant optic pathway gliomas often masquerade as other entities on both clinical exam and neuroimaging, making timely diagnosis challenging. When an initial biopsy is negative, pursuit of a repeat biopsy in a different location is prudent, particularly when clinical suspicion is high. Surgical resection is best supplemented with adjuvant chemotherapy. Temozolomide plus radiation was successful in clearing a positive posterior margin in this particular tumor which had a low Ki-67 index. The re-emergence of neovascularization with gliosis/fibrosis of the optic nerve, was driven by ischemia and further precipitated by radiation. To our knowledge this patient represents the youngest reported case of malignant optic pathway glioma and the longest reported survival in the literature to date (over seven years).
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
Supported by NIH Center Core Grant P30EY014801 and Research to Prevent Blindness Unrestricted Grant
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures or personal conflicts of interest: CRA, VSS, TAE, LLS, BLL.
Acknowledgements/Disclosures
All procedures performed in this study involving a human participant adhered to the 1964 Declaration of Helsinki and its later amendments. Collection of information in this report complied with the Health Insurance Portability and Accountability Act of 1996.
Financial Support: NIH Center Core Grant P30EY014801, RPB Unrestricted Award and Career Development Awards, Department of Defense (DOD- Grant#W81XWH-09-1-0675).
References
- 1.Hoyt W.F., Meshel L.G., Lessell S., Schatz N.J., Suckling R.D. Malignant optic glioma of adulthood. Brain. 1973;96(1):121–132. doi: 10.1093/brain/96.1.121. [DOI] [PubMed] [Google Scholar]
- 2.Mastorakos P., Hays M.A., Caruso J.P. Transtentorial dissemination of optic nerve glioblastoma: case report. J Neurosurg. 2018;128(2):406–413. doi: 10.3171/2016.10.JNS161443. [DOI] [PubMed] [Google Scholar]
- 3.Traber G.L., Pangalu A., Neumann M. Malignant optic glioma - the spectrum of disease in a case series. Graefes Arch Clin Exp Ophthalmol. 2015;253(7):1187–1194. doi: 10.1007/s00417-015-3045-8. [DOI] [PubMed] [Google Scholar]
- 4.Wabbels B., Demmler A., Seitz J., Woenckhaus M., Bloss H.G., Lorenz B. Unilateral adult malignant optic nerve glioma. Graefes Arch Clin Exp Ophthalmol. 2004;242(9):741–748. doi: 10.1007/s00417-004-0905-z. [DOI] [PubMed] [Google Scholar]
- 5.Miller N.R. Primary tumours of the optic nerve and its sheath. Eye (Lond) 2004;18(11):1026–1037. doi: 10.1038/sj.eye.6701592. [DOI] [PubMed] [Google Scholar]
- 6.Millar W.S., Tartaglino L.M., Sergott R.C., Friedman D.P., Flanders A.E. MR of malignant optic glioma of adulthood. AJNR Am J Neuroradiol. 1995;16(8):1673–1676. [PMC free article] [PubMed] [Google Scholar]
- 7.Shriver E.M., Ragheb J., Tse D.T. Combined transcranial-orbital approach for resection of optic nerve gliomas. Ophthalmic Plast Reconstr Surg. 2012;28(3):184–191. doi: 10.1097/IOP.0b013e3182232395. [DOI] [PubMed] [Google Scholar]
- 8.Applegate L.J., Pribram H.F. Hematoma of optic nerve glioma--a cause for sudden proptosis. Magnetic resonance imaging findings. J Clin Neuro Ophthalmol. 1989;9(1):15–19. [PubMed] [Google Scholar]
- 9.Charles N.C., Nelson L., Brookner A.R., Lieberman N., Breinin G.M. Pilocytic astrocytoma of the optic nerve with hemorrhage and extreme cystic degeneration. Am J Ophthalmol. 1981;92(5):691–695. doi: 10.1016/s0002-9394(14)74663-x. [DOI] [PubMed] [Google Scholar]
- 10.Schneider R.C., Kriss F.C., Falls H.F. Prechiasmal infarction associated with intrachiasmal and suprasellar tumors. J Neurosurg. 1970;32(2):197–208. doi: 10.3171/jns.1970.32.2.0197. [DOI] [PubMed] [Google Scholar]
- 11.Maitland C.G., Abiko S., Hoyt W.F., Wilson C.B., Okamura T. Chiasmal apoplexy. Report of four cases. J Neurosurg. 1982;56(1):118–122. doi: 10.3171/jns.1982.56.1.0118. [DOI] [PubMed] [Google Scholar]
- 12.van Baarsen K., Roth J., Serova N. Optic pathway-hypothalamic glioma hemorrhage: a series of 9 patients and review of the literature. J Neurosurg. 2018;129(6):1407–1415. doi: 10.3171/2017.8.JNS163085. [DOI] [PubMed] [Google Scholar]
- 13.Patsouris E., Stocker U., Kallmeyer V., Keiditsch E., Mehraein P., Stavrou D. Relationship between Ki-67 positive cells, growth rate and histological type of human intracranial tumors. Anticancer Res. 1988;8(4):537–544. [PubMed] [Google Scholar]
- 14.Fisher B.J., Naumova E., Leighton C.C. Ki-67: a prognostic factor for low-grade glioma? Int J Radiat Oncol Biol Phys. 2002;52(4):996–1001. doi: 10.1016/s0360-3016(01)02720-1. [DOI] [PubMed] [Google Scholar]
- 15.Bower M., Newlands E.S., Bleehen N.M. Multicentre CRC phase II trial of temozolomide in recurrent or progressive high-grade glioma. Canc Chemother Pharmacol. 1997;40(6):484–488. doi: 10.1007/s002800050691. [DOI] [PubMed] [Google Scholar]
- 16.Newlands E.S., Stevens M.F., Wedge S.R., Wheelhouse R.T., Brock C. Temozolomide: a review of its discovery, chemical properties, pre-clinical development and clinical trials. Canc Treat Rev. 1997;23(1):35–61. doi: 10.1016/s0305-7372(97)90019-0. [DOI] [PubMed] [Google Scholar]
- 17.Stupp R., Gander M., Leyvraz S., Newlands E. Current and future developments in the use of temozolomide for the treatment of brain tumours. Lancet Oncol. 2001;2(9):552–560. doi: 10.1016/S1470-2045(01)00489-2. [DOI] [PubMed] [Google Scholar]
- 18.Yung W.K. Temozolomide in malignant gliomas. Semin Oncol. 2000;27(3 Suppl 6):27–34. [PubMed] [Google Scholar]
- 19.Wedge S.R., Porteous J.K., Glaser M.G., Marcus K., Newlands E.S. In vitro evaluation of temozolomide combined with X-irradiation. Anti Canc Drugs. 1997;8(1):92–97. doi: 10.1097/00001813-199701000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Stupp R., Mason W.P., van den Bent M.J. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 21.Dumas-Stoeckel S., Gambrelle J., Cornut P.L., El Chehab H., Vighetto A., Denis P. [Central retinal vein and artery occlusions related to intraocular involvement of an anaplastic optochiasmatic glioma] J Fr Ophtalmol. 2010;33(8):564–567. doi: 10.1016/j.jfo.2010.06.014. [DOI] [PubMed] [Google Scholar]