Abstract
Temporary balloon occlusion techniques have been described to redirect blood flow during hepatic chemo- and radioembolization. A 69 years old male with pathologically proven multifocal hepatocellular carcinoma involving all the liver segments except segments 2 and 3. We temporarily occlude segment 2/3 branch with the microvascular plug (MVP) to safely deliver the Y90 glass microspheres through the multiple small segment 4 branches. Distal occlusion using MVP may provide a valuable, cheaper and readily available tool in cases of unfavorable anatomy to divert blood flow and avoid non target delivery of Chemo or Radioembolic agents.
Keywords: Temporary occlusion, Balloon, Microvascular plug, Radioembolization
Introduction
Radioembolization has gained wide acceptance in the management of hepatocellular carcinoma. Selective delivery of the radioactive microspheres to the tumor supplying vessels aims to maximize therapeutic effectiveness and reduce treatment related complications. Catheterization and selection of target hepatic arteries supplying the tumor is not always feasible. Temporary balloon occlusion techniques have been described to redirect blood flow during Hepatic chemo- and radioembolization [1], [2], [3]. We describe an occlusion technique using microvascular plug (MVP) to reduce flow to a vascular territory to protect normal hepatic parenchyma and avoid non target delivery of radioactive microspheres.
Case Presentation
This case report was compliant with the Health Insurance Portability and Accountability Act and approved by the institutional review board with a waiver of informed consent. A 69 years old male with pathologically proven multifocal hepatocellular carcinoma, hepatitis C, and hemochromatosis, presented to our interventional radiology department for radiomebolization. The patient presented with multifocal HCC involving all the liver segments except segments 2 and 3. Diagnostic hepatic angiogram of the left liver revealed multiple small segment 4 branches at a common origin of the segment 2/3 branch. Following 99-TC macro-aggregated albumin injection, SPECT/CT was performed and confirmed eligibility for Y90 glass microspheres treatment. The plan was made to temporarily occlude segment 2/3 branch with the MVP on the day of treatment. The dose was calculated using partition model.
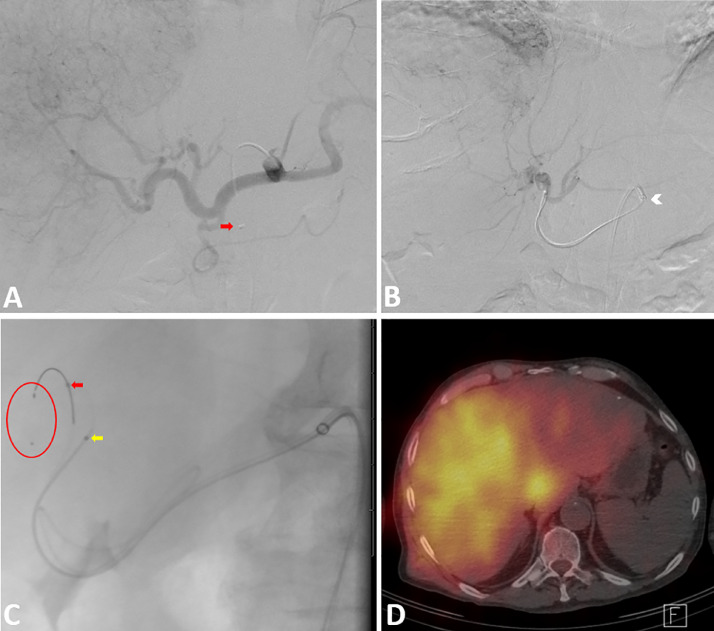
Through a femoral arterial access, a 5-F Chaung B catheter (Cook, Bloomington, IN) was used to select the celiac artery. A celiac angiogram was performed (Fig. 1A). Following this, a 6-French Ansel 1 guiding sheath (Cook, Bloomington, IN) was used to engage the celiac artery (Fig. 1B). A microcatheter was advanced into the right hepatic artery and the Y90 glass microspheres administration was performed in its entirety. Next, The microcatheter and 5-French catheter were removed. Two 2.7-F microcatheters (Renegade HI-FLO; Boston scientific, Natick, MA) were advanced parallel the 6-French guide sheath and used to select the common hepatic artery. One of the catheters was advanced into the segment 2/3 branch of the Left hepatic artery. The second microcatheter was advanced into the proximal left hepatic artery (Fig. 1C).
Fig. 1.
(A) Celiac angiogram showing large tumor blush supllied by branches from Left and Right hepatic arteries . Note the 5F catheter is through the 6F guiding sheath (Red arrow). (B) Left hepatic Angiogram showing multiple segment 4 branches supplying the tumor originating at the same level of the segment 23 branches. Note the 6F guiding sheath is engaged in the celiac artery (white arrow head). (C) left anterior oblique view showing 2 microcatheters advanced side-by-side through the 6 French guiding sheath. Note the MVP device (red circle) is deployed but not released through the microcatheter in segment 2/3 branch (red arrow). The tip of the second microcatheter is in the left hepatic artery (yellow arrow). (D) Post-treatment SPECT/CT showing selective distribution of the radioactive microspheres into the tumors and selective sparing of segments 2 and 3.
After intravenous administration of heparin (2500 IU), the 5 mm microvascular plug (MVP, Medtronic, Minneapolis, MN) was deployed into the common trunk of the segment 2/3 branch (Fig. 1C). The MVP e was deployed but not released. On left hepatic angiography, the blood flow was redirected to segment 4 branches. Subsequently from the proximal left hepatic artery, Y90 glass microspheres administration was performed in its entirety. The MVP and microcatheters were removed. Completion celiac angiogram demonstrates persistent flow in the Right and left hepatic arteries. Post administration SPECT/CT Bremsstrahlung imaging (Fig. 1D) was performed. MIM Y90 SurePlan software (Cleveland, OH) for normal and tumor voxel dosimetry was performed. The calculated mean dose to the normal liver in segment 4 and segments 2/3 were 63 and 35 Gy, respectively. The dominant tumor achieved a mean dose of 133 Gy. Imaging seven month post treatment demonstrated decrease in size of the dominant lesion from 12 to 9.3 cm with multiple sites of necrosis. Segments 2 and 3 also demonstrated interval hypertrophy from 680 ml to 810 ml.
Discussion
The use of temporary occlusion techniques has been described [1], [2], [3]. Itagaki et al [3] applied the same concept using neurovascular balloon microcatheter. In his 2 cases of hepatic chemoembolization, a neurovascular balloon microcatheter was placed distally into the main or a division of the right hepatic artery to protect the vessel and chemoembolization was performed proximally through a single injection. Both procedures were uneventful [3].
The rigidity of the microcatheter (balloon or regular) with possible injury of vessels, the availability and cost of the device, associated stasis and potential thrombosis, all should be considered when using temporary occlusion technique. In this case, the balloon microcatheter was not available at the time of the procedure, we used the MVP to divert the blood flow and avoid non target delivery of the radioactive microspheres. The MVP may be a more readily available device in the IR suites and less costly compared to the neurovascular balloon microcatheter. We were able to demonstrate reduced microsphere deposition and radiation dose in the segment 2/3 territory with the use of the MVP device and allow for hypertrophy of the normal liver parenchyma.
In conclusion, distal occlusion using MVP may provide a valuable tool, in cases of unfavorable anatomy, which can be used to create an artificial flow diversion and avoid non target delivery of Chemo or Radioembolic agents.
Footnotes
Disclosure: None.
References
- 1.Nakamura H., Tanaka M., Oi H. Hepatic embolization from the common hepatic artery using balloon occlusion technique. AJR Am J Roentgenol. 1985;145:115–116. doi: 10.2214/ajr.145.1.115. [DOI] [PubMed] [Google Scholar]
- 2.Matsumoto T., Endo J., Hashida K., Kojima S., Takashimizu S., Watanabe N. Balloon-occluded transarterial chemoembolization using a 1.8-French tip coaxial microballoon catheter for hepatocellular carcinoma: technical and safety considerations. Minim Invasive Ther Allied Technol. 2015;24:94–100. doi: 10.3109/13645706.2014.951657. [DOI] [PubMed] [Google Scholar]
- 3.Itagaki M.W. Temporary distal balloon occlusion for hepatic embolization: a novel technique to treat what cannot be selected. Cardiovasc Intervent Radiol. 2014;37(4):1073–1077. doi: 10.1007/s00270-013-0816-7. [DOI] [PubMed] [Google Scholar]