Abstract
Traumatic hemorrhage of the bilateral basal ganglia is an extremely rare event in severe closed head injuries. Its mechanism remains poorly understood. This report describes the rare case of bilateral traumatic basal ganglia hemorrhage in a 33-year-old man, who had been a victim of violent head trauma. Magnetic resonance imaging and serial computed tomography revealed small hemorrhages in the bilateral basal ganglia as well as nonhemorrhagic diffuse axonal injury in the bilateral internal capsules. The patient was discharged without neurologic deficits following conservative management. Overall, this case report highlights that shearing injury is a potential cause of bilateral traumatic basal ganglia hemorrhage.
Keywords: Basal ganglia, Hematoma, Traumatic, Bilateral
Introduction
Traumatic basal ganglia hemorrhage (TBGH) is relatively uncommon, but a serious complication resulting from head injury [1]. TBGH is defined as an intracerebral hemorrhage located in the basal ganglia and adjacent structures, such as the thalamus and internal capsule [2]. Bilateral TBGH is an extremely rare occurrence [3,4]. Although the pathophysiology remains unclear, it is considered to arise from shearing injury to the lenticulostriate or anterior choroidal vessels secondary to the acceleration-deceleration forces at the time of head trauma [2,3]. To the best of my knowledge, this is the first case report describing bilateral TBGH with nonhemorrhagic diffuse axonal injury (DAI) involving the bilateral internal capsule. This report shows serial computed tomographic (CT) and magnetic resonance imaging (MRI) findings and provides a discussion of the possible mechanisms.
Case presentation
A 33-year-old man was admitted to the emergency department with a complaint of headache after 1 hour of head injury, having sustained an assault to his head by an unknown person in a drunken state. There was no medical history of bleeding disorders, hypertension, or diabetes. His blood pressure was 100/60 mm Hg on admission and was within a normal range during the 4 weeks of hospitalization. The prothrombin time was 15 seconds (normal range: 11.6-14.5 seconds) on admission and normalized over the period of hospitalization. The other laboratory results were all within normal ranges, including activated partial thromboplastin time, liver function tests, platelet count, and blood glucose levels. The Glasgow coma scale score was 15. The initial noncontrast CT scan of the head showed hyperdense acute basal ganglia hematomas bilaterally, 0.9 × 0.8 cm on the right and 0.8 × 0.6 cm on the left (Fig. 1). Other findings included parietal and occipital bone fractures and a bilateral traumatic subarachnoid hemorrhage. The follow-up CT scan, obtained 2 days later, showed new hypodense lesions in the bilateral internal capsule (Fig. 2). The MRI performed 3 days after trauma revealed acute hematoma of the bilateral globi pallidi with surrounding edema. Symmetric signal abnormalities were noted in the bilateral internal capsule, without signal drop out on a gradient echo image, suggestive of nonhemorrhagic DAI (Fig. 3). The patient was conservatively managed and discharged at 28 days after head trauma without focal neurologic deficit. A follow-up CT scan, at 7 months after the injury, revealed encephalomalacia in the bilateral basal ganglia and internal capsules (Fig. 4), and his neurological status was normal.
Fig. 1.
The initial brain computed tomographic image shows small hyperdense acute hematomas in the bilateral basal ganglia, measuring less than 1 cm in diameter each
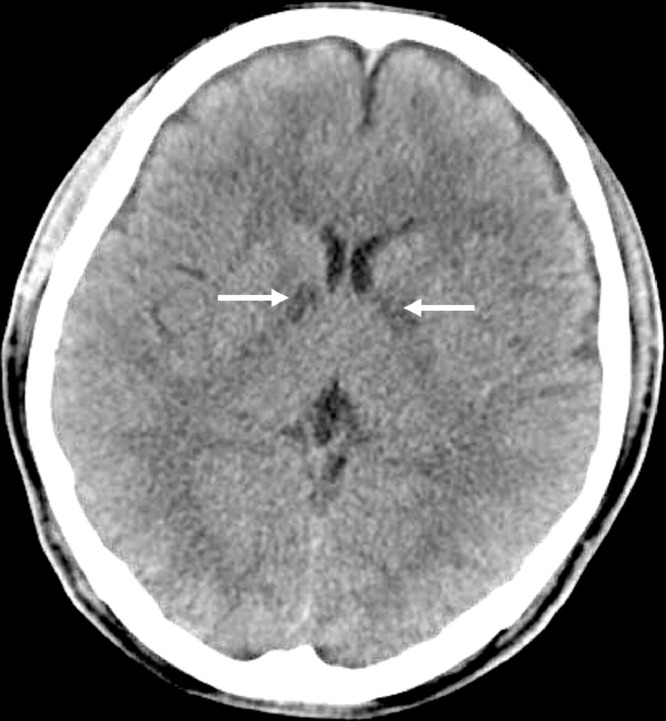
Fig. 2.
A follow-up brain computed tomographic image obtained 2 days after trauma shows new hypodense lesions in bilateral internal capsule (arrows)
Fig. 3.
Brain magnetic resonance imaging taken at 3 days after trauma. The axial fluid-attenuated inversion recovery (FLAIR) image (A) and gradient echo (GRE) sequence (B) depict acute hematoma with surrounding edema in the bilateral basal ganglia. Hyperintensity on the FLAIR image (C) and no blooming on the GRE sequence (D) in the bilateral internal capsule are compatible with nonhemorrhagic diffuse axonal injuries
Fig. 4.
A follow-up brain computed tomographic image obtained 7 months after injury shows well-defined hypodense areas with decreased parenchymal volume in the bilateral basal ganglia (A) and the internal capsule (B), suggestive of encephalomalacia
Discussion
TBGH is a relatively uncommon incidence, observed in only approximately 3% of the patients with a closed head injury. In autopsy series, the incidence is higher, ranging between 10% and 12% [2,[5], [6], [7]. Relatively, bilateral TBGH is even more rare and limited number of cases are reported to date [1], [2], [3], [4],8]. This case study describes bilateral TBGH with serial CT and MRI findings.
DAI results from axonal stretch or shear stress, arising from rotational as well as translational injuries, and can be hemorrhagic or nonhemorrhagic [9]. Characteristic locations include the gray–white matter junction, corpus callosum, internal capsules, dorsal midbrain, and pons [9]. The present case shows a signal change in the bilateral internal capsule, without evidence of blooming on the gradient echo sequence, suggestive of nonhemorrhagic DAI.
Whether deeply located hematomas, such as those of the basal ganglia, are spontaneous or traumatic in origin is an important and potentially crucial medicolegal matter [2,8]. Spontaneous hematomas of the basal ganglia region are usually unilateral [1]. Moreover, as basal ganglia hematomas can result from nontraumatic causes, such as hypertension or coagulation disorders, it is often challenging to determine the precise cause in patients that have severe head trauma history and hematoma simultaneously [2,3]. However, in this case, there was a clear history of head trauma and blood pressure had been within normal ranges throughout the hospital stay. Although the patient showed slightly prolonged prothrombin time on admission, it was normalized following the admission period and the other laboratory results were within normal ranges. Brain CT and MRI disclosed a fracture of the skull, bilateral traumatic subarachnoid hemorrhages, subdural hematoma, and nonhemorrhagic DAI. Therefore, based on his clinical history and radiologic findings, the patient was diagnosed with bilateral TBGH.
The exact mechanism of injury leading to basal ganglia hematoma after trauma has not yet been revealed. However, a possible mechanism of TBGH may be the sudden acceleration or deceleration of forces that turn into shear stress over the lenticulostriate or anterior choroidal arteries and lead to hemorrhage of the basal ganglia [10]. Specifically, when high velocity impact is delivered to the head and directed towards the tentorium, it can shift the brain through the tentorium notch and produce a stretch as well as tear of the vessels from the shearing forces. This may result in bilateral hemorrhages in the basal ganglia region [2,3]. TBGH can be classified as “small” when less than 2 cm in diameter, or as “large” when more than 2 cm in diameter [6]. Small lesions have been described as a part of DAI [2]. The present patient demonstrated bilateral basal ganglia hematoma of diameter less than 2 cm that were classified as small hemorrhages. Therefore, according to the imaging findings of small bilateral TBGH combined with nonhemorrhagic DAI in the bilateral internal capsules, the shearing injury in the ganglionic region can be considered as the most probable mechanism of TBGH in this patient.
Various treatment options have been used for patients with TBGH, including open surgery, stereotactic aspiration, and conservative management [3]. Boto et al has previously recommended the surgical evacuation of hematoma for all lesions of a volume of more than 25 mL [7]. Similarly, the prognosis of TBGH has also been reported to be variable. TBGH is considered to be associated with a worse prognosis than other types of post-traumatic intracranial hemorrhages [8]. The larger the size of the hematoma–associated with coagulation disorders, DAI, and intraventricular or brainstem hemorrhage—the greater the indication of poorer outcomes [2]. The existence of associated DAI after severe closed head injury is also strongly related to worse prognosis [7]. Although surgically treated patients commonly experienced poor outcomes [3,7], a previous study has reported favorable results following TBGH [5].
Additionally, bilateral TBGH can be considered a marker of poor prognosis [3]. However, some previous reports have highlighted successful outcomes in bilateral TBGH without surgical interventions [4,8]. As the current patient had small-sized basal ganglia hematomas, he was managed conservatively. Additionally, he was discharged with no neurological deficit, despite showing nonhemorrhagic DAI in the bilateral internal capsules and bilateral involvement of TBGH.
In conclusion, bilateral TBGH with DAI is extremely rare. It can show favorable recovery if the hematomas are small and can be managed conservatively. In the present case, shear stress in the ganglionic region after the head injury may have played an important role in the bilateral TBGH with adjacent DAI.
Footnotes
Competing Interests: The author declares that he has no conflict of interest.
Funding: There was no funding support for the research.
Authors' contribution: Byung Hoon Lee; design of the study, patient enrollment, data acquisition, data analysis/interpretation, and manuscript preparation.
Patient consent statement: This study has got an ethical review exemption from the Institutional Review Board of author’s institution, which waived the requirement for written informed consent from the participant.
References
- 1.Jain S.K., Sundar I.V., Sharma V., Prasanna K.L., Kulwal G., Tiwari R.N. Bilateral large traumatic basal ganglia haemorrhage in a conscious adult: a rare case report. Brain Inj. 2013;27(4):500–503. doi: 10.3109/02699052.2013.765597. PubMed: 23472761. [DOI] [PubMed] [Google Scholar]
- 2.Bhargava P., Grewal S.S., Gupta B., Jain V., Sobti H. Traumatic bilateral basal ganglia hematoma: a report of two cases. Asian J Neurosurg. 2012;7(3):147–150. doi: 10.4103/1793-5482.103725. PubMed: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pandey N., Mahapatra A., Singh P.K. Bilateral large traumatic hemorrhage of the basal ganglion. Asian J Neurosurg. 2014;9(4):240. doi: 10.4103/1793-5482.146644. PubMed: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kankane V.K., Gupta T.K., Jaiswal G. Traumatic bilateral basal ganglia bleed: a report of rare two cases and review of the literature. Asian J Neurosurg. 2016;11(4):457. doi: 10.4103/1793-5482.175646. PubMed: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katz D.I., Alexander M.P., Seliger G.M., Bellas D.N. Traumatic basal ganglia hemorrhage: clinicopathologic features and outcome. Neurology. 1989;39(7):897–904. doi: 10.1212/wnl.39.7.897. PubMed: [DOI] [PubMed] [Google Scholar]
- 6.Adams J.H., Doyle D., Graham D.I., Lawrence A.E., McLellan D.R. Deep intracerebral (basal ganglia) haematomas in fatal non-missile head injury in man. J Neurol Neurosurg Psychiatry. 1986;49(9):1039–1043. doi: 10.1136/jnnp.49.9.1039. PubMed: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boto G.R., Lobato R.D., Rivas J.J., Gomez P.A., de la Lama A., Lagares A. Basal ganglia hematomas in severely head injured patients: clinicoradiological analysis of 37 cases. J Neurosurg. 2001;94(2):224–232. doi: 10.3171/jns.2001.94.2.0224. PubMed: [DOI] [PubMed] [Google Scholar]
- 8.Jang K.J., Jwa C.S., Kim K.H., Kang J.K. Bilateral traumatic hemorrhage of the basal ganglia. J Korean Neurosurg Soc. 2007;41(4):272–274. doi: 10.3340/jkns.2007.41.4.272. PubMed: [DOI] [Google Scholar]
- 9.Schweitzer A.D., Niogi S.N., Whitlow C.T., Tsiouris A.J. Traumatic brain injury: imaging patterns and complications. Radiographics. 2019;39(6):1571–1595. doi: 10.1148/rg.2019190076. PubMed: [DOI] [PubMed] [Google Scholar]
- 10.Ogrenci A., Eksi M.S., Gun B., Koban O. Traumatic basal ganglia hematoma following closed head injuries in children. Childs Nerv Syst. 2016;32(7):1237–1243. doi: 10.1007/s00381-016-3060-z. PubMed: [DOI] [PubMed] [Google Scholar]