Abstract
Purpose
To report a case of conjunctival plaque infected from Sporothrix schenckii, which was possible transmitted from a cat.
Observations
A case of Thai woman presented with chronic painless ulcerated conjunctiva with white plaque. The lesion was not healed for one month after excision. She became concerned of getting infection from her cat because it developed chronic and multiple skin lesions on its legs. Identification of Sporothrix schenckii by PCR method was confirmed in the tissues from her conjunctiva and cat's skin.
Conclusion and Importance
The diagnosis of Sporothrix infection should be suspected in atypical conjunctival lesion in patient who had closed contact with infected cat. This brought awareness to doctors and cat owners, even though it was uncommon.
Keywords: Sporothrix schenckii, Cat transmission, Conjunctival nodule, Cat ulcer, Zoonosis, Asia
1. Introduction
Sporothrix schenckii was a dimorphic fungus, living in soil, dead wood, and hay. Infection in human occurred by accidently traumatic inoculation to the skin, for example, gardening, sporting, or outdoor activities. When mold penetrated through the traumatic skin, it will transform into blastospores, or budding cells in subcutaneous tissue. The clinical features were frequently fixed-cutaneous (painless, ulcerative-nodular lesion) or lymphocutaneous form.1,2 Hematogenous spreading (bone, lung, CNS) or disseminated form have been reported in immunocompromised host, which can progress to sepsis and multiple organ failures.3 This was a case report of conjunctival (mucosal) form of sporotrichosis in immunocompetent host which the infection was highly suspected to be transmitted from pet.
1.1. Case report
The 42-year-old Thai woman presented with chronic, painless, ulcerated lesion with whitish plaque at left lower tarsal conjunctiva after keloid-like conjunctival lesion had been excised a month ago. She complained of mild ocular irritation without visual disturbance or eye discharge. She had no fever and underlying disease. Best-corrected visual acuity was 20/20. Slit lamp examination showed ulcerated lesion size 1 × 4 mm, covering with whitish plaque and swollen edge at left lower tarsal conjunctiva (Fig. 1A). Preauricular lymph node was not palpable. She also had an itchy bump on her right hand, resemble an insect bite at the same period of eye problem. The nodule was excised three weeks ago by a general surgeon at private hospital (Fig. 2). The diagnosis was an ulcer with granuloma by histopathology.
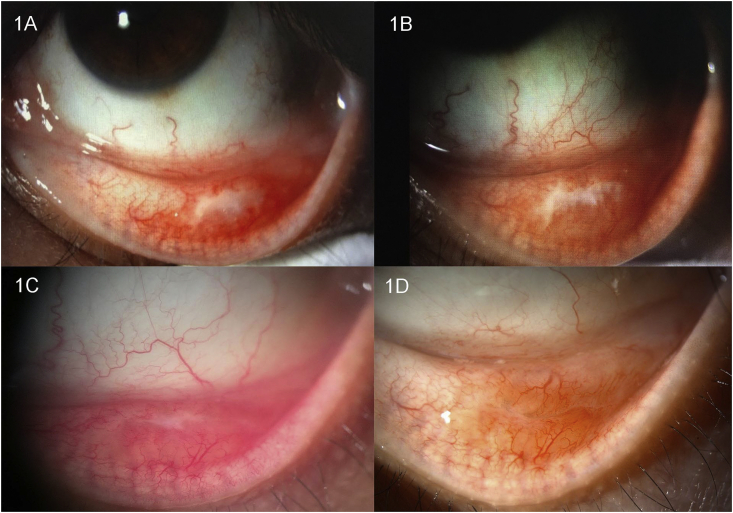
Fig. 1.
Slit-lamp photographs of the conjunctival plaque at presentation(A) ten days(B), three weeks(C), and one month(D) after treatment.
Fig. 2.
Photograph shows location of the itchy bump on her right hand post incisional biopsy.
She had three cats and slept with them in the bedroom. One of her cats developed chronic ulcerated wounds on its leg and nose (Fig. 3) three months before she had conjunctival nodule and skin lesion. Budding yeast cells were reported from the cat's histopathology staining. Our patient denied history of cat scratching or biting. The patient was referred to our center to make a definite diagnosis. Systemic examination was normal. HIV, VDRL serology, and chest x-ray were negative. Conjunctival scraping was done and sent for Gram stain, KOH stain, aerobic culture, anaerobic culture, and fungal culture. However, the results were all negative.
Fig. 3.
Photographs of the cat's ulcers starting at the elbow then get along the leg (A) and nose (B).
The biopsy tissues were reviewed and sent for PCR. The histopathology resulted from conjunctival nodule demonstrated necrotizing granulomas comprising central eosinophilic granular reactions surrounded by epithelioid histiocytes, lymphocytes, plasma cells, neutrophils, and scattered giant cells. AFB stain, GMS stain and PCR for mycobacteria showed no organisms. We also reviewed tissue from wound biopsy of the sick cat which showed non-encapsulated multilobulated mass filled with many neutrophils, plasma cells and lymphocytes in the dermis, infiltrated with macrophages that contained round yeast-like organism, size 3–8 μm with clear capsule and narrow-based buddings. The PCR using universal primers, internal transcribed spacer (ITS) 1 and ITS4 from both patient and cat's formalin-fixed paraffin embedded (FFPE) tissue showed 100% homology to Sporothrix schenckii. Therefore, we gave her a diagnosis of Sporothrix infection in ulcerative nodular form which most likely transmitted from her pet by direct contact.
The patient was treated with Terramycin (oxytetracycline hydrochloride with polymyxin B sulfate) eye ointment four times daily for 2 months. Maxitrol (neomycin sulfate with polymyxin B sulfate and dexamethasone) eye ointment at bedtime was added after day 10 and was discontinued after one month because of intraocular pressure rising. The lesion was healed (Fig. 1B, C and 1D) and resolved in two months without recurrence after follow-up for a year. The cat wounds got better by being applied gentian violet without taking any oral medications.
2. Discussion
This was the first case report in Thailand which showed sporotrichosis at conjunctiva (extracutaneous manifestation). The PCR demonstrated Sporothrix schenckii from both the patient's conjunctiva and her cat wounds. It showed high possibility that the patient caught these fungi from her infected cat. Although, she denied history of being bite or scratch from the cat, the organisms could inoculate onto her right hand and accidently passed through her conjunctiva while rubbing.
In Thailand, sporotrichosis was rare. Cutaneous sporotrichosis has been reported once in 1990 - that presented with two crusted mass at the elbow.4 The skin biopsy and culture revealed Sporothrix schenckii. Another report was found in stray cat.5 Normally, sporotrichosis found high endemic in South America e.g. Brazil and Peru.1 According to report in Brazil, 372 cats, 34 dogs, and 83 humans, were infected between year 2010 and 2016, which 35% of infected cats were dead.6 In Asia, Sporothrix infection was uncommon. There were a few report from Japan, India, China, and Malaysia.7,8 Tang MM reported case series of cutaneous sporotrichosis in Malaysia, which 68% revealed history of skin trauma and half of these trauma related to cat biting or scratching.8 Arinelli A and Aleixo A collected 26 cases of ocular sporotrichosis in Rio de Janeiro, Brazil.9 The typical characteristics were groups of shiny surface nodules surrounded by conjunctival redness and edema with eye discharge, 80% involved at tarsal conjunctiva. Adjacent lymphadenopathy was found in 77% of cases. Additionally, 96% documented the history of direct contact with an infected cat. Although there was no report of visual impairment in cases of ocular sporotrichosis in normal host, but awareness of this infection should be concerned in immunocompromised cases.
There were two routes of transmission: from plants and animals. At 25 °C, Sporothrix habitat as filamentous hyphae in plants can pass through host tissue by traumatic inoculation. Last decades, Sporotrichosis was found to be associated with occupational related plants e.g. agriculture work. Lately, closely contact by infected cats became a significant risk factor for Sporothrix infection which developed two to three weeks after deep scratches or bites.10 The gold standard for diagnosis of Sporothrix was culture positive after incubation on Sabouraud dextrose agar for 5–8 days.11 However, the infection lodge deep in host tissue, reside in cyst form, and the culture was frequently negative. Then tissue biopsy was usually required. Histopathologically, sporotrichosis showed granulomas, presence of lymphoplasmacytic cell infiltration and yeasts or asteroid bodies but identified organisms was not detected in 65%.12 Therefore, PCR from FFPE tissue processing was helpful to establish diagnosis. Sensitivity and specificity of PCR were as high as 100% and 98.7%, respectively.13 In our case, histopathological review from cat wound (demonstrated yeast-like organism), history of cat contact and location of cat's wound which developed on its nose brought us recognition of mycoses that grew at subcutaneous level. Sporothrix schenckii was detected from PCR performing.
Treatment of choices depended on clinical severity including oral itraconazole (dosage 100–400 mg/day), Potassium iodide (KI), Terbinafine, or intravenous Amphotericin B in disseminated disease.14 Before PCR result, our patient was initially started with Terramycin eye ointment which was antibiotic composed of oxytetracycline hydrochloride and polymyxin B sulfate. Zhai B suggested anticryptococcal activity of polymyxin B in vitro and in mice.15 Additionally, Hsu LH demonstrated anti-fungal activity of polymyxin B of Fusarium species in vitro.16 Our report had supported role of polymyxin B in antifungal activity. Otherwise, spontaneous recovery had been reported. In 1985, cutaneous sporotrichosis spontaneously disappeared after follow-up for 46 days in 15-month-old boy17 and in 2009, pregnant veterinarian with lymphocutaneous sporotrichosis was healed without treatment by 7 months.18
3. Conclusions
This is the first ocular Sporothrix infection in Thailand which highly possible transmitted from sick cat. Animal-to-human (zoonosis) spreading should be under awareness. PCR from tissue biopsy is helpful for diagnosis.
Patient consent
The patient consented to publication of the case in writing.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: UR, MJ, ST, WT, AC.
Acknowledgements
We thank Dr. Navaporn Worasilchai for the PCR performing and analysis.
References
- 1.Estrada-Castanon R., Chavez-Lopez G. Report of 73 cases of cutaneous sporotrichosis in Mexico. Nov/Dec 2018;93(6):907–909. doi: 10.1590/abd1806-4841.20187726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barros M.B., de Almeida Paes R., Schubach A.O. Sporothrix schenckii and sporotrichosis. Clin Microbiol Rev. Oct 2011;24(4):633–654. doi: 10.1128/CMR.00007-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moreira J.A., Freitas D.F., Lamas C.C. The impact of sporotrichosis in HIV-infected patients: a systematic review. Infection. Jun 2015;43(3):267–276. doi: 10.1007/s15010-015-0746-1. [DOI] [PubMed] [Google Scholar]
- 4.Kwangsukstith C., Vanittanakom N., Khanjanasthiti P., Uthammachai C. Cutaneous sporotrichosis in Thailand: first reported case. Mycoses. Nov-Dec 1990;33(11-12):513–517. doi: 10.1111/myc.1990.33.11-12.513. [DOI] [PubMed] [Google Scholar]
- 5.Duangkaew L., Yurayart C., Limsivilai O., Chen C., Kasorndorkbua C. Cutaneous sporotrichosis in a stray cat from Thailand. Medical mycology case reports. Mar. 2019;23:46–49. doi: 10.1016/j.mmcr.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poester V.R., Mattei A.S., Madrid I.M. Sporotrichosis in Southern Brazil, towards an epidemic? Zoonoses and public health. Nov 2018;65(7):815–821. doi: 10.1111/zph.12504. [DOI] [PubMed] [Google Scholar]
- 7.Chakrabarti A., Bonifaz A., Gutierrez-Galhardo M.C., Mochizuki T., Li S. Global epidemiology of sporotrichosis. Med Mycol. Jan 2015;53(1):3–14. doi: 10.1093/mmy/myu062. [DOI] [PubMed] [Google Scholar]
- 8.Tang M.M., Tang J.J., Gill P., Chang C.C., Baba R. Cutaneous sporotrichosis: a six-year review of 19 cases in a tertiary referral center in Malaysia. Int J Dermatol. Jun. 2012;51(6):702–708. doi: 10.1111/j.1365-4632.2011.05229.x. [DOI] [PubMed] [Google Scholar]
- 9.Arinelli A., Aleixo A. Aug 14 2019. Ocular sporotrichosis: 26 cases with bulbar involvement in a hyperendemic area of zoonotic transmission; pp. 1–8. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues A.M., de Hoog G.S., de Camargo Z.P. Sporothrix species causing outbreaks in animals and humans driven by animal-animal transmission. PLoS Pathog. Jul 2016;12(7) doi: 10.1371/journal.ppat.1005638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arenas R., Sanchez-Cardenas C.D., Ramirez-Hobak L., Ruiz Arriaga L.F. Sporotrichosis: from KOH to molecular biology. May 23 2018;4(2) doi: 10.3390/jof4020062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quintella L.P., Passos S.R., do Vale A.C. Histopathology of cutaneous sporotrichosis in Rio de Janeiro: a series of 119 consecutive cases. J Cutan Pathol. Jan 2011;38(1):25–32. doi: 10.1111/j.1600-0560.2010.01626.x. [DOI] [PubMed] [Google Scholar]
- 13.Hayashi S., Kaminaga T., Baba A. Diagnostic Value of a Nested Polymerase Chain Reaction for Diagnosing Cutaneous Sporotrichosis from Paraffin-Embedded Skin Tissue. Dec 2019;vol. 62(12):1148–1153. doi: 10.1111/myc.13004. [DOI] [PubMed] [Google Scholar]
- 14.Orofino-Costa R., Macedo P.M., Rodrigues A.M., Bernardes-Engemann A.R. Sporotrichosis: an update on epidemiology, etiopathogenesis, laboratory and clinical therapeutics. Anais brasileiros de dermatologia. Sep-Oct 2017;92(5):606–620. doi: 10.1590/abd1806-4841.2017279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhai B., Lin X. Evaluation of the anticryptococcal activity of the antibiotic polymyxin B in vitro and in vivo. Int J Antimicrob Agents. Mar 2013;41(3):250–254. doi: 10.1016/j.ijantimicag.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Hsu L.H., Wang H.F., Sun P.L., Hu F.R., Chen Y.L. The antibiotic polymyxin B exhibits novel antifungal activity against Fusarium species. Int J Antimicrob Agents. Jun 2017;49(6):740–748. doi: 10.1016/j.ijantimicag.2017.01.029. [DOI] [PubMed] [Google Scholar]
- 17.Iwatsu T., Nishimura K., Miyaji M. Spontaneous disappearance of cutaneous sporotrichosis. Report of two cases. Int J Dermatol. Oct 1985;24(8):524–525. doi: 10.1111/j.1365-4362.1985.tb05837.x. [DOI] [PubMed] [Google Scholar]
- 18.Almeida H.L., Jr., Lettnin C.B., Barbosa J.L., Dias M.C. Spontaneous Resolution of Zoonotic Sporotrichosis during Pregnancy. Revista do Instituto de Medicina Tropical de Sao Paulo. Jul-Aug 2009;vol. 51(4):237–238. doi: 10.1590/s0036-46652009000400012. [DOI] [PubMed] [Google Scholar]