Abstract
Purpose
Presentation of a rare lesion: a case of upper eyelid lipoma,
Observations
A 76-year-old otherwise healthy woman presented with a right upper eyelid swelling. Her medical history was recorded. On ophthalmologic examination a soft, non-ulcerated and not well-circumscribed mass was evident. An ultrasonography examination was carried out showing a hyperechoic non capsulated mass situated between the superior orbital margin and the orbicularis oculi muscle.
Conclusions and Importance
Eyelid lipomas must be differentiated from herniated orbital fat, cystic lesions, tumours, and the lacrimal gland.
A pre-operative differential diagnosis of eyelid lipoma can be done through medical history, ophthalmologic, and ultrasonography examinations. Nevertheless, in case of doubt a magnetic resonance imaging (MRI) should be performed to assess a possible orbital involvement and to plan for the right surgical procedure to be performed.
Keywords: Eyelid lipoma, Eyelid lesion, Ophthalmologic examination, Lipoma, Upper eyelid, Eyelid
1. Introduction
Lipomas are soft, benign tumours, and usually present with slow growth. Histologically, they are characterized by fat lobules among fibrous septa. Lipomas are occur most commonly within the subcutaneous tissue of the back, neck, and limbs.1 Nevertheless, all areas can be affected by this kind of lesion. Herein, we present a case of a lipoma of the upper eyelid.
2. Case report
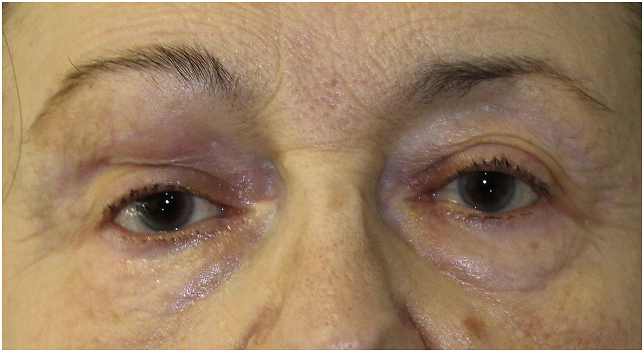
A 76-year-old otherwise healthy woman presented with a 4-year history of slow, progressive right upper eyelid swelling. She did not experience pain or other symptomatology, but only slight discomfort and an increasing size of the mass over the previous 14 days. No proptosis or resistance to retropulsion was evident (Fig. 1). On ophthalmologic examination a soft, non-ulcerated and not well-circumscribed mass was evident. The pupils were isochoric and there was not relative pupil afferent defect. An ultrasonography examination was carried out. A hyperechoic non capsulated mass was detected. The mass was located between the superior orbital margin and the orbicularis oculi muscle. The lesion measured 27 × 4 × 4.4 mm.
Fig. 1.
Preoperative picture showing a bulging mass sited in the upper eyelid. A slight ptosis can be noted in the ipsilateral eye. No proptosis is evident.
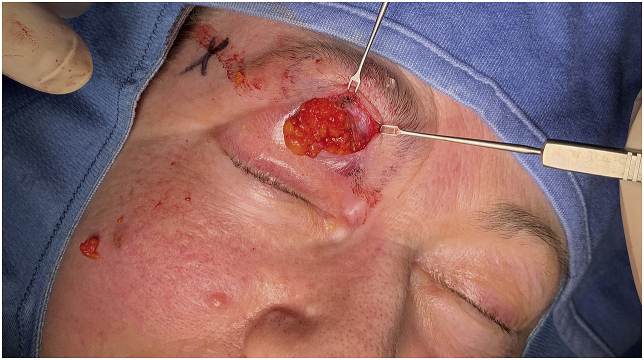
The decision was made to pursue surgical excision with biopsy. The surgery proceeded as follows, local anesthetic with 2% xylocaine with epinephrine was administered 20 minutes before surgical excision in order to facilitate hydro-dissection and to control bleeding. An upper lid skin incision was made and an irregular lobular mass under the muscular layer in the pre-septal plane was exposed. The tissue colour was lighter than the periorbital fat (Fig. 2). The lesion showed irregular margins, but it did not seem to infiltrate the orbicularis oculi muscle macroscopically. The irregular lobules were carefully excised with a Colorado® Micro-Dissection needle at 3 W coagulation in order to minimize muscle and skin damage and to control bleeding (Fig. 3).
Fig. 2.
Intraoperative picture showing the incision performed to reach the lipoma. A lobulated, sub-orbicularis oculi muscle lesion was exposed.
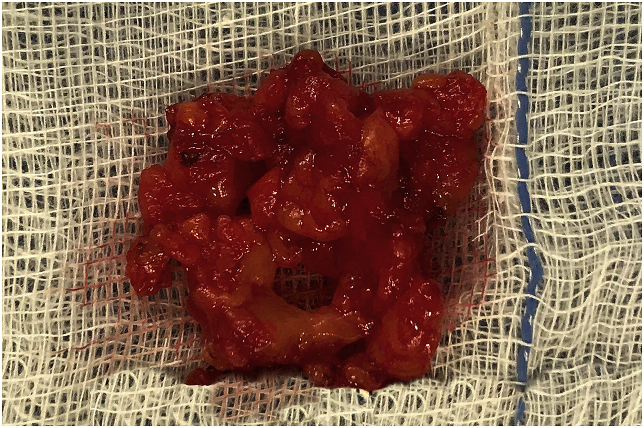
Fig. 3.
Excised eyelid lipoma.
The tumour was removed and sent for pathologic examination. The histologic section showed mature adipocytes organized in lobules divided by fibrous septa. The cells showed slight pleomorphism, but no atypia or mitotic features. No capsule and no orbicularis oculi muscle infiltration were observed.
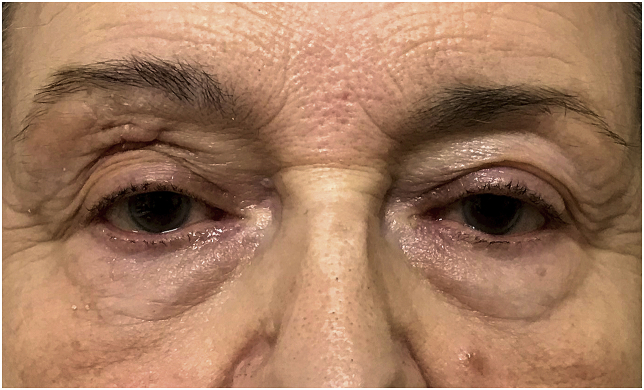
No functional deficits were detected during the post-operative period (Fig. 4). No complications were reported after a two months’ follow up.
Fig. 4.
2 weeks postoperative picture showing good healing of the surgical incision and correction of the ptosis.
3. Discussion
Although lipomas are commonly linked with a translocation between chromosome 12 and 3, the exact cause is not clear. Several cases are linked with a previous trauma in the area. Despite being the most frequent soft tissue tumours with an incidence of up to 2.1 per 100 individuals, few cases of lipomas involving the eyelid have been described in litterature.2, 3, 4, 5, 6 Different subtypes of lipomatous lesions exist and can be classified with a microscopic examination.7 They can be histologically identified on the basis of the different tissues types other than the adipose component.7 Surgical excision is very effective and recurrence rate is rare, although it is more common for intramuscular lipomas.7 Moreover, they can be a component of Nasopalpebral Lipoma-Coloboma Syndrome.8
Eyelid lipomas must be differentiated from herniated orbital fat,9 a cystic lesion10 and the lacrimal gland.
A pre-operative differential diagnosis of eyelid lipoma can be carried out through medical history and symptoms (speed of onset, pain, changes in visual acuity), and an ophthalmologic and ultrasonography examination. Nevertheless, in situations where the diagnosis remains unclear, magnetic resonance imaging can be performed to assess a possible ocular cavity involvement and to plan the right surgical procedure to be performed.
MRI is in fact a more sophisticated examination but its cost-effectiveness should be individually evaluated.
Lipomas are surgically removed daily in hospitals worldwide, but only few cases of eyelid lipoma have been described in literature. They can be frequently found in the trunk, and in the limbs where they can often be easily removed. The periorbital region represents a surgically challenging site.11 For this reason, surgical excision of the mass should be carried out with maximum care in order to minimize conjunctival and muscle tissue excision and to avoid asymmetries and scarring. Among the few cases described in literature we can identify different subtypes of lipoma, such as an osteolipoma,12 a myolipoma,2,6 a spindle-cell lipoma3 and a capsulated lipoma.1,4,5 We have described a case of non-capsulated and non-muscle-infiltrating lipoma.
4. Conclusions
Although eyelid lipomas are very rare lesions, they should be considered in the differential diagnosis for slow growing subcutaneous eyelid masses. Both ophthalmologic and ultrasonography examination should be performed to obtain a pre-operative diagnosis. In case of doubt, a magnetic resonance imaging is essential to evaluate a possible ocular cavity involvement.
Patient consent
Consent to publish this case report has been obtained from the patient in writing.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: Starnoni M., De Santis G., Pasini R., Pinelli M.
Acknowledgements
Sara Crescimbeni (sara.crescimbeni@mail.com): photo technical helper.
Scott Sanders (scott.sanders@apyxmedical.com): language reviewer.
References
- 1.Thyparampil P., Diwan A.H., Diaz-Marchan P., Grekin S.J., Marx D.P. Eyelid lipomas: a case report and review of the literature. Orbit Amst Neth. 2012;31(5):319–320. doi: 10.3109/01676830.2012.681099. [DOI] [PubMed] [Google Scholar]
- 2.Sharara N., Lee W.R., Weir C. Myolipoma of the eyelid. Graefes Arch Clin Exp Ophthal. 1998;236(8):630–634. doi: 10.1007/s004170050133. [DOI] [PubMed] [Google Scholar]
- 3.Mawn L.A., Jordan D.R., Olberg B. Spindle-cell lipoma of the preseptal eyelid. Ophthal Plast Reconstr Surg. 1998;14(3):174–177. doi: 10.1097/00002341-199805000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Maeng M.M., Godfrey K.J., Kazim M. Preseptal upper eyelid lipoma. Ophthal Plast Reconstr Surg. 2019;35(1):e2–e3. doi: 10.1097/IOP.0000000000001268. [DOI] [PubMed] [Google Scholar]
- 5.Dorello U. Simple lipoma of the eyelid. Boll Ocul. 1960;39:183–188. [PubMed] [Google Scholar]
- 6.Charles N.C., Palu R.N. Intramuscular lipoma of the eyelid. Ophthalmic Surg Laser. 2000;31(4):340–341. [PubMed] [Google Scholar]
- 7.Treatment for intramuscular lipoma frequently confused with sarcoma: a 6-year restrospective study and literature review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4276111/ [DOI] [PMC free article] [PubMed]
- 8.Chacon-Camacho O.F., Lopez-Martinez M.S., Vázquez J. Nasopalpebral lipoma-coloboma syndrome: clinical, radiological, and histopathological description of a novel sporadic case. Am J Med Genet. 2013;161A(6):1470–1474. doi: 10.1002/ajmg.a.35916. [DOI] [PubMed] [Google Scholar]
- 9.Lin C.C., Liao S.L., Liou S.W., Chen C.C., Wu Y.Y., Woung L.C. Subconjunctival herniated orbital fat mimicking adipocytic neoplasm. Optom Vis Sci Off Publ Am Acad Optom. 2015;92(10):1021–1026. doi: 10.1097/OPX.0000000000000693. [DOI] [PubMed] [Google Scholar]
- 10.Suimon Y., Kase S., Ishijima K., Kanno-Okada H., Ishida S. Clinicopathological features of cystic lesions in the eyelid. Biomed Rep. 2019;10(2):92–96. doi: 10.3892/br.2018.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pinelli M., Starnoni M., De Santis G. A simplified and practical surgical treatment for medial ectropion: a case report. Plast Reconstr Surg Glob Open. 2019;7(5) doi: 10.1097/GOX.0000000000002102. Published 2019 May 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar S., Kumar S., Kulshrestha R. Osteolipoma of the eyelid. Clin Exp Ophthalmol. 2008;36(5):473–474. doi: 10.1111/j.1442-9071.2008.01786.x. [DOI] [PubMed] [Google Scholar]