Abstract
Objective
Provide current overview of Active Apex correction as a new technique for surgical management for Early Onset Scoliosis by dynamically remodulating the apex of the deformity and mitigate loss of correction and presents a comparative correction data against the long-established systems.
Method
Summary of the surgical technique and review of the existing retrospective data on APC surgical technique and its comparison against other existing techniques.
Results
Retrospective clinical results showed the efficiency of the APC technique in active remodulation of the apex of the curve with lower incidence of implant related complications in comparison to SHILLA and Magnetically Controlled Growing Rods (MCGR). APC also showed similar results with traditional growing rods without the need for repeated distraction surgeries for 4 years.
Conclusion
Active Apex Control is safe and viable option in surgical management for Early Onset Scoliosis patients even in areas with limited resources.
Keywords: Active apex correction, Growth rod, Growth guidance, Modified SHILLA technique, Crankshafting, Adding-on
1. Background
Early onset scoliosis is a term dealing with spine deformities in children below 10 years of age. The difficulties of dealing with this group include heterogenicity, associated comorbidities, higher complications than idiopathic spine deformity, the multidisciplinary approach, and the expenses of the implants.
The main aim of surgical correction for early onset spine deformity through growth preservation techniques is to maintain a mobile growing spine with preservation of lung growth and minimal complications.
Most common surgical management of scoliosis falls under one of the three philosophies constituting of growth-guidance technology, distraction-based systems, and compression-based systems. The failure of most of these standalone techniques has shown that the concept of “one size fits all” is not applicable for the surgical management of EOS.1, 2, 3, 4, 5, 6 Therefore, newer concepts employing two or more of the above philosophies, i.e. various combinations of distraction-based, guided-growth, and compression-based approaches might be more suitable and biomechanically-speaking, a more optimal surgical intervention. One such combination currently used for surgery includes Active Apex Correction (APC).7,8.
2. Active Apex Correction
APC is a hybrid of guided-growth and compression-based philosophies for management of growing-spine deformity. The technique consists of replacing the apical fusion (of a traditional SHILLA) with a unilateral compression (applied via pedicle screws) on the convex side. Accordingly, this compression is meant to halt the growth of the most wedged vertebrae on convex side and allow the ratio of concave-to-convex height to increase overtime, thus reducing the vertebral wedging at the apex of the curve. Biomechanically, it allows for an active compression-based intervention at the apex of the curve in accordance with Hueter-Volkmann law, alongside passively restrained guided-growth height allowance of the entire scoliotic curvature. This technique also avoids the need for pedicle screw fixation on the concave side, thus circumventing the need for risky osteotomies and reducing precious surgical time.
3. Method
APC technique developed 13 years ago with control of the apex of thoracolumbar kyphosis in EOS children by putting screws posteriorly in tethering fashion.
The placement of these screws was proximal and distal to the most wedged vertebrae and compression was applied to the kyphotic (convex) side. Modulation of the wedged vertebrae was noticed at 5 years follow up with gradual correction of the kyphotic deformity without the need of osteotomies or auxiliary anterior approaches.9
Beginning 2013, APC technique was then applied to all EOS types. Results were compared with the known results of other established EOS correction technology.
4. Surgical technique
The operation is performed under general anesthesia, with the patient in the prone position. A straight longitudinal midline incision is performed as a proximal wound incision usually beginning from T2-5. In case the choice of the proximal anchors is the rib hook, the attached edge of the Trapezius and Rhomboidus major is dissected exposing the rib extraperiosteally. Two proximal hooks are placed facing downwards with distal one facing upwards in the three-rib construct. If screws are to be used as proximal anchors, it is preferable to put pedicular screws through regular spinal approach at 3 levels proximally. The choice for approaching the apex of the curve is either through continuity of the proximal incision or having a separate incision at the apex.
After identifying the peaked wedged vertebrae through MRI or 3D CT scan preoperatively, the convex side of the apex is exposed either through an open incision or minimal invasive (percutaneously) with pedicular screws inserted and connected with 5.5 rod on the convex side above and below the most wedged vertebrae [Fig. 1] to give tethering effect for modulation of the peaked wedged vertebrae. Distally, exposure of 2 distal levels previously planned through longitudinal incision and putting pedicular screws in these 2 levels or in the iliac area if the anchors are required to be more distal than the lumbar region. Proximal sliding rod (4.5 or 5.5) is used for connecting proximal anchors (convex side) to the tethering rod via domino, locking on the tethered rod.
Fig. 1.
Pedicle screws on the convex side of the apex above and below the most wedged vertebrae.
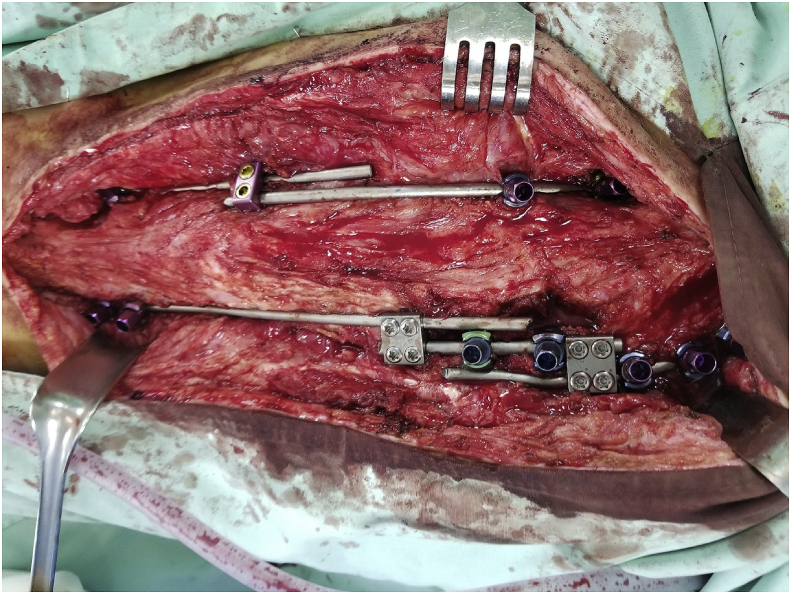
Similarly, distal rod (4.5 or 5.5) is connected via domino (unlocked for sliding) with the tethered rod (fixed with domino). [Fig. 2].
Fig. 2.
With dominos connecting the proximal and distal rods with the tethering rod on the convex side and domino connecting the proximal and distal rod on the concave side with at least 4 cm sliding rod length.
On the concave side, proximal rod is connected directly to the distal rod via domino, with one sliding rod (preferably the proximal rod) and the other fixed within the domino.
Compression of the tethered screws on the convex side should be applied with caution. Distraction must be performed on the concave side to get maximum correction; this would be achieved with maximum efficiency when holding the distraction by cross link or hook on the sliding rod.
Cross link could be used to increase the strength of fixation, but it is not mandatory. The procedure is to be done with C-arm and intraoperative neuromonitor available in the operative room. No cast or brace were used for these patients.
5. Results
Three papers are published with clinical results for children with EOS treated using APC technique and with more than 2 years of follow up.7, 8, 9 One of these papers compare the follow up results such as correction and complications of the traditional growing rods (TGR) and APC,7 indicating no statistical difference in complications, unplanned surgeries and spine length. Apical Vertebral translation improved 34 to 29, coronal balance 16 to 12, coronal cobb angle 54 to 44 and the spinal length 255 mm–281 mm. The complications for 20 patients treated with APC technique with 32 months follow up revealed 5 mechanical complications (25%) including one rod fracture. Correction with APC at 2 years follow up also revealed substantial improvement in apex wedging compared to the preoperative data.8
6. Discussion
Surgery plays major role in EOS management, and with awareness of the importance of lung growth in EOS cases, surgeons shifted to growth friendly techniques that would allow spine deformity correction with lung growth preservation. Ideal surgical management for early onset scoliosis deformity is conducting one surgery with no repeated distractions or unplanned surgeries, preserving as much spine mobility as possible with minimal autofusion, and maximum correction in the coronal plan with appropriate contouring of the sagittal plane.
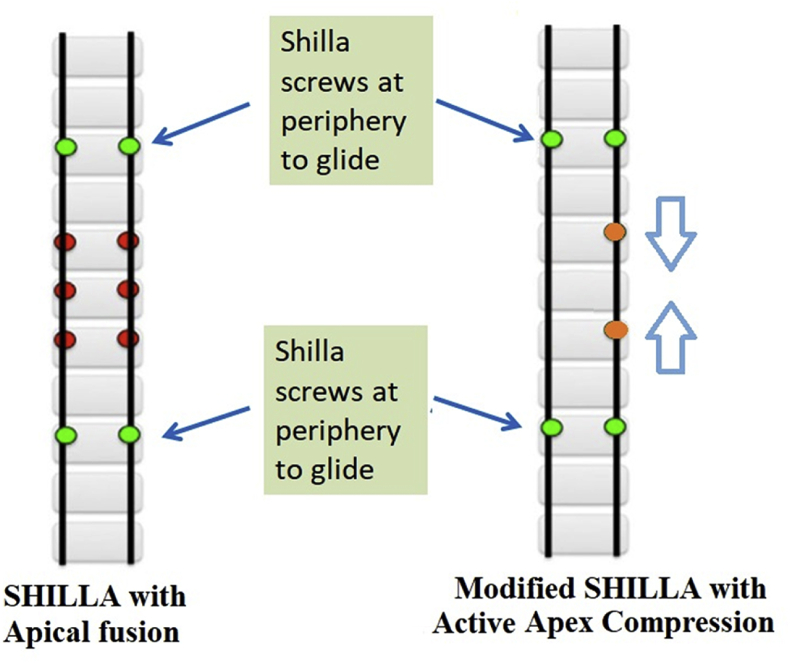
Magnetically Controlled Growing Rods (MCGR) and SHILLA are the two popular procedures allowing spinal growth with gradual correction without the need for repeated distraction surgeries. Lengthening in Magnetically Controlled Growing Rods (MCGR) is done in the outpatient clinic through transcutaneous magnetic force without the need for surgery. Follow up results showed real concerns about mechanical failure with high incidence of unplanned surgeries implant related (failure of rod distraction, rod breakage). SHILLA Growth Guidance system (SGGS) main concept is guiding growth through correction and fusion of 3–4 levels of the curve apex, with rods sliding proximally and distally through SHILLA screws without the need of recurrent surgeries. Putting screws in the apex of the curve specially on the concave side in severely deformed vertebrae is technically demanding that needs highly experienced surgeons doing it [Fig. 3].
Fig. 3.
Schematic showing key differences in established SHILLA procedure and the modified SHILLA approach used in this study. (Used with Permission).
Active Apex Correction (APC) is relatively new technique mainly considered as a modification of SHILLA with apex control through tethering the convex side allowing remodulation and reduction of vertebral wedging. Instead of apical fusion, apex compression was applied at the wedged vertebra. This in addition to allowing a foundation for fixation at the apex, traditionally sought for controlling the curve, also seeks to dynamically modify the peak of the curve. The immediate benefits of the procedure alone are avoidance of risky osteotomies, requirement to insert screws at the concave end of the apex, and more economical surgery (putting 2 screws instead of 6 at the apex of the curve) for underprivileged patients globally with no added risk over SHILLA. The results show correction in the wedging of the vertebra due to APC, in contrary to a static fusion at the apex, which have been shown to cause continued growth of deformity mostly anteriorly and thus crankshafting or adding-on.7, 8, 9 The sliding of the rods is done by connecting the tethered rod with proximal and distal rods, thereby permitting spine growth without the need of distraction under general anesthesia.
In comparison for 33 patients treated with SHILLA with 6 years follow up had 73% implant related complications of which 55% were rod breakage.14 Similarly, Bumpass et al.11 discussing the SHILLA follow up results showed 40% of rod breakage and 62% of crankshaft phenomena, increasing the incidence of unplanned surgeries. Similar results for the high incidence of the crankshaft at the apex was detected in another study.14 High incidence of rod breakage is seen more frequently adjacent to apical fusion and is highest for idiopathic EOS at 36%, with 29% breakage rate for syndromic/neuromuscular patients and 25% for congenital EOS patients.15
Concerning magnetically Controlled Growing Rods (MCGR), studies discussing the short- and medium-term mechanical complications requiring unplanned surgeries range from 47% to 75%.10,12,13 Hong Kwan et al. published results about the unplanned surgeries post MCGR showing 47% of the patients went to unplanned surgeries within 24 months of follow up.10
The main goals of having a new technique is to avoid major complications with the MCGR and SHILLA while maintaining the major advantage of avoiding repeated distraction surgeries (TGR) under GA.
Short term follow up for the APC might play a role in giving biased results comparing the mechanical complications with MCGR and SHILLA, but we hypothesize that the main concept of controlling the apex through modulation not fusion would preserve growth of the spine including the apex unlike stopping the growth by fusing the apex with continuous growth anteriorly that will increase the possibility of the Crankshaft and the implant related complications.
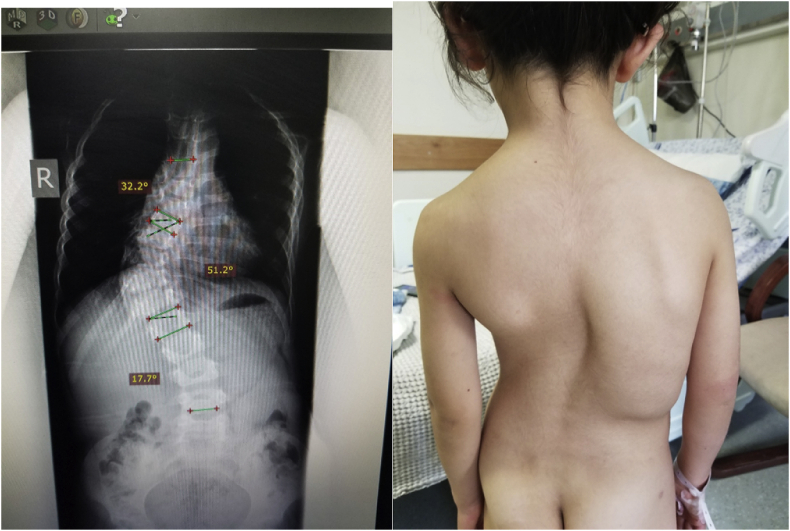
APC is easy to implement even in LMICs since it is tethering through posterior approach which is the popular approach for most spine surgeons. The procedure can be done with regular spinal implants produced from any company with no need for specific expensive implants with the ability to do hybrid fixation using rib hooks proximally if there is difficulty putting pedicle screws [Figs. 4, Fig. 5]. The technique overcomes the lack of regular follow up and the need to frequent distractions every 6 months, as the rods will slide up to 4 cm with growth.
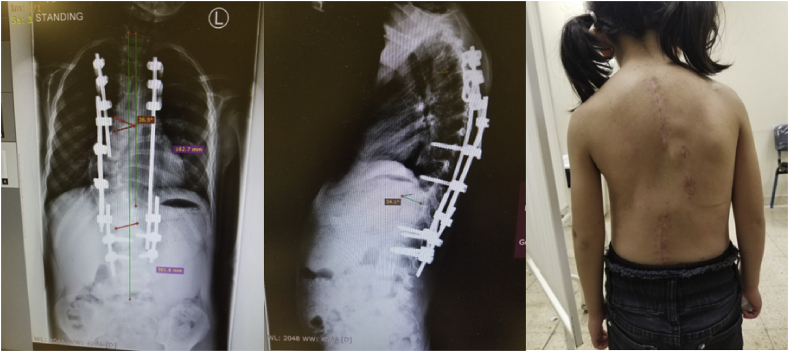
Figs. 4.
5 years old female with progressive EOS despite brace treatment.
Fig. 5.
Same patient with correction of the deformity with APC technique the tethering screws site with 5.5 rod in the Apex.
7. Future steps
Given a major deviation from the established SHILLA procedure, it was a prudent measure to limit this procedure to a few and perform a close follow up. However, given these results we are confident to carry on an open enrollment of patients with scoliosis and kyphoscoliosis. We didn’t quantify the amount of compression being applied between tethering screws, and how the magnitude of compression or lack of it altogether affects the reverse modulation in practice. We intend to quantify the amount of compression either via direct measurement or virtual setup employing Hueter Volkmann principle where a patient-specific kinetic model could be used to determine the forces based on the height gain in a given period.
One may also argue the need for a more homogeneous sample besides the presence of the same surgical team. However, it is seldom possible for the following reasons: differences in the deformity parameters at pre-op, variability between the construct even within a single surgical group (e.g., using cross-links vs not using cross-links), varied pathogenesis of scoliosis, and overall unpredictable growth and development differences among children with such pathology.
8. Conclusion
The clinical data on APC provides evidence of safe and effective reverse vertebral modulation at the apex of the curve in patients with scoliosis and kyphoscoliosis with potential to mitigate crankshafting or adding-on. The clinical data also suggested clinical equivalency with respect to correction between the two clinical procedures (APC and traditional growth rod systems) at the current follow-up period. However, the latter procedure presents an obvious disadvantage because it requires multiple surgeries to regularly distract the spine. APC can be one of the realistic surgical options for management of EOS considering the ease and safety in doing the surgery, and the availability of necessary implants with cheaper prices.
References
- 1.Agarwal A., Kelkar A., Agarwal A.G., Jayaswal D., Jayaswal A., Shendge V. Device-related complications associated with magec rod usage for distraction-based correction of scoliosis. Spine Surg Related Res. 2019;4(2):148–151. doi: 10.22603/ssrr.2019-0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bumpass D.B., McCullough L., McCarthy R.E. Shilla growth guidance—evolution of a new procedure: rate of complications in the first two years following implantation in the first 80 patients. Spine J. 2017;17(10):S106–S107. [Google Scholar]
- 3.Miyanji F., Parent S. Early Onset Scoliosis. Springer; 2018. Anterior vertebral body tethering (AVBT) for early-onset scoliosis; pp. 117–134. [Google Scholar]
- 4.Samdani A.F., Ames R.J., Kimball J.S. Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine. 2014;39(20):1688–1693. doi: 10.1097/BRS.0000000000000472. [DOI] [PubMed] [Google Scholar]
- 5.Braun J.T., Akyuz E., Ogilvie J.W., Bachus K.N. The efficacy and integrity of shape memory alloy staples and bone anchors with ligament tethers in the fusionless treatment of experimental scoliosis. JBJS. 2005;87(9):2038–2051. doi: 10.2106/JBJS.D.02103. [DOI] [PubMed] [Google Scholar]
- 6.Cebeci B.O., Ergene G., Sogunmez N., Ay B., Yilgor C., Alanay A. Non-fusion growth modulation with anterior vertebral body tethering via thoracoscopic approach for adolescent idiopathic scoliosis. Spine J. 2017;17(10):S106. [Google Scholar]
- 7.Agarwal A., Aker L., Ahmad A.A. Active apex correction (modified SHILLA technique) versus distraction-based growth rod fixation: what do the correction parameters say? Spine Surg Related Res. 2019;4(1):31–36. doi: 10.22603/ssrr.2019-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agarwal A., Aker L., Ahmad A.A. Active apex correction with guided growth technique for controlling spinal deformity in growing children: a modified SHILLA technique. Global Spine J. 2019;10(4):438–442. doi: 10.1177/2192568219859836. 2192568219859836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmad Alaaeldin A., Aker Loai, Hanbali Yahia. Growth modulation and remodeling by means of posterior tethering technique for correction of early-onset scoliosis with thoracolumbar kyphosis. Eur Spine J. 2017;26:1748–1755. doi: 10.1007/s00586-016-4910-9. [DOI] [PubMed] [Google Scholar]
- 10.Yat Hong Kwan Kenny, Ahmet Alanay, Muharrem Yazici. Unplanned reoperations in magnetically controlled growing rod surgery for early onset scoliosis with a minimum of two-year follow-up. Spine. 2017;42(24) doi: 10.1097/BRS.0000000000002297. pp E1410eE1414. [DOI] [PubMed] [Google Scholar]
- 11.Bumpass David B., Mannen Erin M., McCarthy Richard E. Implant retrieval analysis for growth guidance constructs: a mechanical analysis. Spine J. 2018;18 S70eS128. [Google Scholar]
- 12.H Teoh Kar, Winson Daniel M.G., James Stuart H. Do magnetic growing rods have lower complication rates compared with conventional growing rods? Spine J. 2016;16:S40–S44. doi: 10.1016/j.spinee.2015.12.099. [DOI] [PubMed] [Google Scholar]
- 13.Chrishan Thakar, David Christopher Kieser, Mihai Mardare, et al. Systematic review of the complications associated with magnetically controlled growing rods for the treatment of early onset scoliosis [DOI] [PubMed]
- 14.Kharrat Khalil, Sebaaly Amer, Kreichati Gaby. Shilla Proc Crankshaft Phenomenon. April 1, 2016;6(1) page(s): s-0036-1583043-s-0036-1583043. [Google Scholar]
- 15.Cryar Kipp A., Bumpass David B., McCullough Lynn. Rod breakage in shilla growth guidance constructs: when, where, and why?NASS 32 S75 nd annual meeting. Proc./Spine J. 2017;17:S41–S88. [Google Scholar]