Summary
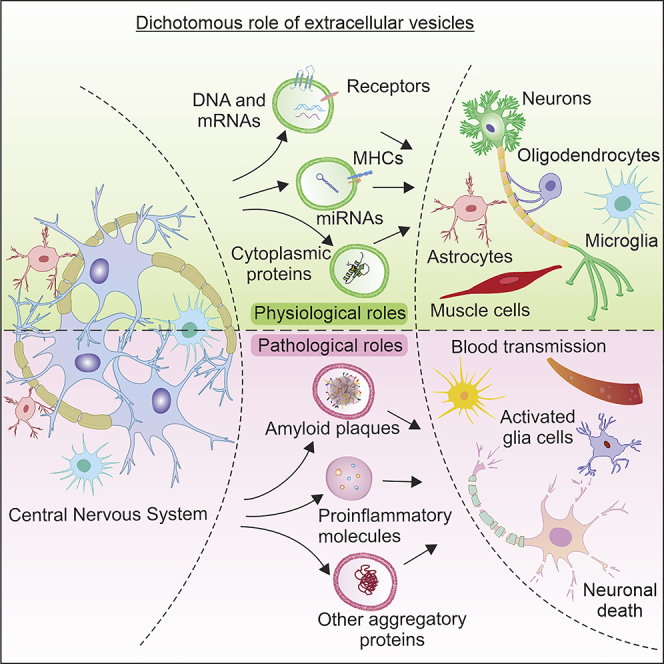
Extracellular vesicles (EVs) are important mediators of intercellular communication. Interest in the role of central nervous system (CNS)-derived EVs has been increasing; however, some skepticism of their importance has persisted because many aspects of their biology remain elusive. This ambiguity is largely due to technical barriers that hamper our ability to achieve a comprehensive understanding of their molecular components and mechanisms responsible for their transmission and uptake. However, accumulating evidence supports the notion that EVs play important roles in basic physiological processes within the CNS during neurodevelopment and synaptic plasticity. Interestingly, EVs also act to spread toxic polypeptides in neurodegenerative diseases. Developing a more profound understanding of the role that EVs play in the CNS could lead to the identification of biomarkers and potential vehicles for drug delivery. Here we highlight our current understanding of CNS EVs and summarize our current understanding of their complex role in the CNS.
Subject Areas: Neuroscience, Molecular Neuroscience, Cellular Neuroscience
Graphical Abstract
Neuroscience; Molecular Neuroscience; Cellular Neuroscience
The existence of extracellular vesicles (EVs) has become increasingly appreciated; however, their biological importance has been called into question. Historically, EVs have been defined as membrane-bound particles for shuttling cellular waste from many different cell types into the extracellular space (Harding et al., 1983; Pan et al., 1985; Trams et al., 1981). Interest in central nervous system (CNS) EVs, primarily released from neurons, have recently boomed, with a particular emphasis on the possibility that they enable intercellular communication and propagate pathological phenotypes, revealing a functional dichotomy (Vella et al., 2016; Zhang and Yang, 2018).
Neuron-to-neuron communication in the CNS has long been considered to be primarily mediated by neurotransmitters and electrical signals. Recent studies have revealed that EVs are also involved in modulating synaptic communication and neurodevelopment, thus greatly impacting the way we view intercellular CNS communication (Budnik et al., 2016). A more thorough understanding of EVs, however, has demonstrated that they play complex roles in the CNS, by propagating and exacerbating pathophysiology. Importantly, our ability to decipher the distinct roles of EVs has been limited by several significant technical barriers including their low abundance and broad size distribution. To overcome these challenges, new methods and instruments have been developed and are starting to facilitate our ability to investigate and characterize CNS EVs. In this review, we evaluate the existing literature on CNS EVs in light of our own findings while highlighting their inherent dichotomy.
EV Biogenesis and Uptake
EVs are classified primarily based on their size (40–1,000 nm in diameter) and the mechanism by which they are released from cells. There are two major EV classes: exosomes and ectosomes (also called microvesicles). Exosomes are nanosized vesicles (40–160 nm in diameter), whereas ectosomes are larger and more diverse (50 nm–1 μm in diameter) (Trams et al., 1981). Exosomes are derived from the endocytic pathway and the Golgi apparatus (Banizs et al., 2018; Nagano et al., 2019). Ectosomes, on the other hand, are formed by direct host cell liberation of the plasma membrane via outward budding and pinching (Heijnen et al., 1999). For exosome biogenesis, vesicles generated through endocytosis of the plasma membrane or Golgi apparatus fuse with endosomes and undergo inward budding. This endomembrane compartment then gives rise to multivesicular bodies (MVBs) containing intraluminal vesicles (ILVs), the intracellular precursor of exosomes (Rind et al., 2005; Roizin et al., 1967; von Bartheld et al., 1996). ILVs sequester cargo, including proteins, lipids, mRNAs, and microRNA (miRNA), from the inward budding of early endosomal membranes (Trajkovic et al., 2008). Generally, MVBs are thought to fuse either with lysosomes to facilitate catabolism, mediated by hydrolases, or with the plasma membrane to release exosomes (Johnstone et al., 1987; Karim et al., 2018). In mammalian neurons, MVBs localize predominantly to the somatodendritic compartment but have also occasionally been observed in axons (Rind et al., 2005; Roizin et al., 1967; von Bartheld et al., 1996). However, MVBs are found at presynaptic sites within nerve terminals in the Drosophila neuromuscular junction (NMJ) (Ashley et al., 2018; Franch-Marro et al., 2008; van den Heuvel et al., 1989). However, it is important to note that whereas these results provide snapshots of MVB localization patterns in neurons, EV biology is dynamic and these studies are limited by the existing technologies.
The endosomal sorting complex required for transport (ESCRT) system plays an important role in exosome biogenesis and may also be involved with releasing ectosomes. ESCRT comprises more than 30 proteins that form four different complexes (ESCRT-0, ESCRT-1, ESCRT-2, ESCRT-3), along with auxiliary proteins including Vps4, Vta1, and Alix (Schmidt and Teis, 2012). ESCRT functions in a sequential, stepwise manner, where ESCRT-0 and ESCRT-1 recruit transmembrane cargos to MVB microdomains and ESCRT-2 and ESCRT-3 play key roles in the scission of ILVs from the donor membrane (Raiborg and Stenmark, 2009; van Niel et al., 2018). Some aspects of MVB transport and exosome biogenesis also require the production of the waxy lipid ceramide, through hydrolysis of neutral type II sphingomyelins (nSMase2) (Trajkovic et al., 2008). The existence of ESCRT-independent pathways for the formation of exosomes is also supported by previous studies. For example, inhibitors of all four ESCRT complexes fail to suppress the generation of CD63-containing ILVs in MVBs (Stuffers et al., 2009). Furthermore syndecan-1, syntenin-1, and Rab proteins also contribute, to exosome biogenesis, presumably in an ESCRT-independent manner (Baietti et al., 2012; Ostrowski et al., 2010). Numerous studies in the field of virology indicate that the ESCRT system plays a critical role in viral budding (Box 1), revealing overlapping mechanisms between EVs and retroviral budding mechanisms. However, nearly all of our knowledge of EV biogenesis originates from studies using cell lines as opposed to investigating EVs in the brain. Taken together, EVs are heterogeneous in their methods of biogenesis, and although many of the general principles have been elucidated, there is still much to learn about these processes within the CNS.
Box 1. Similarities between EV Release and Viral Budding.
Emerging evidence suggests that the molecular machinery required for EV release and enveloped virus budding share many important characteristics. Viruses including herpes simplex virus 1, Ebola virus, rabies virus, and human immunodeficiency virus (HIV) have evolved the capacity to hijack host cell ESCRT machinery, which plays a key role in EV biogenesis to promote budding (Ahmed et al., 2019; Votteler and Sundquist, 2013). One particular protein that is important for the ESCRT pathway linking viral budding and EV release is Alix (also known as Pdcd6ip). Alix, which is frequently found in low abundance in EVs, is important for membrane scission, contributing to EV release, as well as virus budding (Baietti et al., 2012; Fujii et al., 2007; Hurley and Hanson, 2010).
Retroviruses, such as HIV, use protein capsids as protective barriers for genetic material to ensure robust infection and spreading. Viruses form protein capsids as protective structures to efficiently transport their genomes from cell to cell during infection. This process is mediated through the viral Group-specific antigen (Gag) polyproteins. During retroviral replication, Gags multimerize into capsid structures and sequentially bind and package viral RNA. These viral particles proceed to exit the cell by budding from the plasma membrane using ESCRT and then are capable of infecting other cells, replicating and repeating the cycle.
Similarly, the mammalian activity-regulated cytoskeleton-associated protein (Arc), which is expressed by neurons, has recently been reported to function in a manner similar to viral capsids (Campillos et al., 2006; Erlendsson et al., 2020). Arc proteins share significant homology with the retroviral Gag domain normally found in retroviruses and vestigial retrotransposon elements within the genome. However, the exact function of these analogous Gag-like structural elements of Arc protein remains unclear. Arc was found to self-assemble into oligomers, form capsid like structures, and be released from neurons in EVs (Ashley et al., 2018; Pastuzyn et al., 2018). Notably, Arc was found to encapsulate RNA and facilitate transfer to recipient cells, evocative of retroviral-like behavior. Additional evidence suggests that at the Drosophila NMJ EVs containing dArc1 also forms capsid-like structures and interacts with RNA, similarly to retroviral and retrotransposon behaviors. In addition, removing the gypsy retrotransposon-like sequence fragment in the 3′ UTR was sufficient to block intercellular transfer. Taken together, these findings reveal overlapping mechanisms between viral budding and EV formation.
Cellular uptake of EVs is an essential step in the transmission of vesicle cargo to recipient cells. Although not yet well established, several potential mechanisms for cellular uptake of EVs have been proposed (Montecalvo et al., 2012; Valadi et al., 2007). One possible mechanism is through the direct binding of proteins on the EV surface, such as CD11a, CD9, and CD81, to intercellular adhesion proteins expressed on the cells' plasma membrane (Morelli et al., 2004). Through these initial protein-protein interactions, EVs dock to cells and initiate the process of cargo transfer. Another proposed mechanism involves endocytosis, which can be clathrin dependent or caveolin mediated (Barres et al., 2010; Feng et al., 2010; Nanbo et al., 2013; Svensson et al., 2013).
Apart from receptor- and endocytosis-mediated EV uptake, other mechanisms including phagocytosis (Feng et al., 2010; Fomina et al., 2003; Prada et al., 2016), micropinocytosis (Fitzner et al., 2011), or direct membrane fusion (Jahn et al., 2003; Montecalvo et al., 2012; Parolini et al., 2009; Prada et al., 2018) have been proposed. For an in-depth description of EV uptake mechanisms, we direct readers to several previous reviews on this topic (Mulcahy et al., 2014; van Niel et al., 2018). It is important to note that these studies are limited by the currently available methods for characterizing EVs and visualizing single vesicle events (Box 2). Similar to EV biogenesis, studies investigating the mechanisms of EV uptake by recipient cells have thus far been predominantly performed on heterologous cell types; yet these mechanisms appear to extrapolate to at least some CNS cell types, but further studies are needed to confirm this hypothesis.
Box 2. Methodologies for EV Isolation and Analysis.
Efficient isolation of highly pure EVs represents a major barrier in the investigation and characterization of their cargos and functions. To overcome this barrier, many EV isolation methods have been developed, such as ultracentrifugation, ultrafiltration, size exclusion chromatography (SEC), proprietary polymer-based precipitants, density gradient-based separation, and immunoaffinity capture. Every EV isolation method has strengths and weaknesses.
Ultracentrifugation remains by far the most commonly used method to isolate EVs (Gardiner et al., 2016). This method typically involves the removal of larger vesicles by a series of slow spins, followed by 110,000 × g centrifugation to sediment EVs. However, this method isolates a heterogeneous population of EVs and lipoproteins. In an attempt to further purify exosomes, samples are subjected to sucrose or iodixanol step gradients to separate materials based on their density. In these methods, samples are centrifuged at high speeds (200,000 × g) for lengthy periods of time so that contaminating proteins are sifted through the gradient, leaving EVs resolved at an equilibrium buoyancy in the gradient (Livshits et al., 2015). Although powerful, there are several downsides to its approach, including its lengthy workflow and the requirement of an ultracentrifuge. In addition, isolation by ultracentrifugation subjects EVs to strong forces that can cause them to rupture and lose their cargos. Furthermore, these methods do not robustly remove abundant and contaminating lipoproteins. Other isolation methods such as immunoaffinity-based techniques and commercially available exosomes isolation kits are also commonly used; however, these methods have been proved to be inferior in reproducibility.
Recently, IZON has produced a convenient SEC system called qEV that utilizes gravity flow columns specific for the isolation of EVs. IZON qEV uses a matrix consisting of porous resin particles that accurately capture EVs ranging from 35–1,000 nm in a few highly enriched fractions. This instrument can isolate vesicles with about 99% purity, in a procedure requiring only 15–30 min (https://izon.com/exosomes-isolation/). This method is advantageous as it is both quick and produces intact and highly bioactive EVs. Downsides of the IZON system include the yield tending to be lower than that of other methods thus requiring a pre-concentrating step and this instrument being unable to isolate specific EVs with different protein components (i.e., CD81 versus CD9 EVs). Finally, as IZON profiles vesicles based solely on their size, the isolated vesicles may not be exclusively EVs, as other vesicles such as endosomes are similar in size.
Recently, NanoView has developed a unique and powerful instrument to immunocapture EVs and subsequently characterize them with a single analysis platform. NanoView works by passing fluid containing EVs across functional microarray chips containing antibodies specific to EV tetraspanin proteins such as CD63 and CD81 (https://www.nanoviewbio.com/). This technology is advantageous for the analysis of individual EVs and the detection of their cargo proteins. However, the EVs captured by this method are unrecoverable thus unavailable for downstream analysis.
Traditional downstream analysis following isolation typically utilizes size/morphology and immunoblotting for EV protein markers (e.g., CD81, CD9, CD63, Tsg101, Alix, flotilin). Subsequently, visualization of EVs requires high-resolution microscopy as traditional light microscopy does not suffice. To this end, electron microscopy (EM) is a commonly used technique to visualize isolated EVs. Various EM techniques have been effectively used and include transmission EM, scanning EM, and negative-staining EM. However, these methods typically only facilitate morphological measures (i.e., size) as immuno-EM requires high-affinity antibodies and epitopes that are physically accessible (Gardiner et al., 2016).
To quantify the concentration of EVs in a given sample, nanoparticle tracking analysis (NTA) is commonly used. NTA utilizes Brownian motion and light scattering to provide both size distribution and concentration of particles in solution (Filipe et al., 2010).
Although commonly used, NTA has some limitations in its ability to accurately and reliably characterize EVs. First, NTA measures any particle in a given solution; it does not selectively measure EVs, and NTA can be hindered by false-positive measurements from water marks and air bubbles.
The ability to analyze cell-specific populations of EVs is technically daunting, and new technologies are needed to accurately define these subpopulations. Interestingly, Ji et al., recently utilized a high-density microchamber and a spatially resolved antibody barcode substrate to achieve multiplexed profiling of EVs secreted from a single cell at a resolution of 1,000 per cells at a time (Ji et al., 2019). However, more advancements will be needed for the efficient isolation of EVs from a diverse set of samples.
Traditional molecular analysis of EV cargo proteins has been performed with western blotting. Although a commonly used technique, many other instruments provide more powerful and complete analysis of EV molecular cargo. NanoView, as mentioned previously, provides an immunocapture technology allowing the analysis of colocalizing proteins in EVs with potentially larger number of proteins of interest. To obtain a more systematic analysis of EV cargo proteins or RNAs high-throughput analytical strategies are required. RNA-sequencing (RNA-seq) provides global analysis of EV RNA profiles, and tandem mass spectrometry-based proteomics provides the means to rapidly identify and measure global EV protein content. It is important to note that currently both RNA-seq and proteomics are only capable of characterizing pools of EVs and provide composite measures.
EVs in Neurogenesis, Synaptogenesis, and Synaptic Plasticity
Neuronal communication in the CNS is primarily achieved through chemical neurotransmitters and electrical signals (Valenzuela et al., 2011). However, emerging evidence suggests that EVs may also play a key role in CNS intercellular communication between neurons and between neurons and glia (Figure 1). Importantly, EVs contain select proteins, RNAs, and lipids that perform important functions. Corroborating these observations, several recent studies have unexpectedly found that EVs participate in CNS biological processes such as synaptic plasticity, spine pruning, neuron-glia communication, development, and regenerative processes (Budnik et al., 2016).
Figure 1.
EV-Based Intercellular Communication at Synapses and in the CNS
(A) EVs facilitate neuronal communication through their association with important signaling proteins in both vertebrate (left) and invertebrate (right) models. At mammalian CNS synapses EVs containing EphB2 or Arc participate in retrograde synaptic communication and can modulate synaptic transmission. EVs containing EphB2 contribute to growth cone collapse and neuronal axon repulsion, whereas Arc EVs can transfer Arc mRNA. At fly NMJs, EVs containing Wnt, dArc, or Syt 4 are released from neurons and are taken up by the muscle. Wnt released in EVs from axon terminals plays a critical role in synapse development and plasticity through EVs. The role of dArc and Syt4 transferred in EVs is a topic of ongoing research.
(B) EVs function in mediating communication between multiple CNS cell types. Microglia-derived EVs contain miRNAs and enzymes. Astrocyte-derived EVs contain multiple proteins and miRNAs that contribute to neuroprotection and neurite outgrowth. Oligodendrocyte-derived EVs inhibit myelin formation, whereas neuronal EVs can block this process.
EVs participate in several dynamic CNS processes and began garnering interest in neural development when 50- to 600-nm EV-like particles were initially detected in the lumen of developing embryonic mouse brain neural tubes (Marzesco et al., 2005). These vesicles are present in the ventricular fluid at both the onset and early phases of neurogenesis and carry the stem cell marker prominin-1 (i.e., CD133), suggesting that EVs can originate from CNS cells beyond merely fully differentiated neurons during development. Furthermore, EVs enriched with the membrane attack complex are released from oligodendrocytes during the recovery phase of injury (Scolding et al., 1989). Additional studies have found that a higher amount of myeloid microvesicles are released from microglia derived from patients with multiple sclerosis compared with healthy controls (Verderio et al., 2012). Although these studies reported the presence of EV-like particle in the CNS, it was unclear if these particles played a functional role. To this end, cerebrospinal fluid (CSF) from both human and mouse embryos were found to possess nanovesicles containing miRNA and protein components of the insulin-like growth factor (IGF) pathway. Interestingly, when these EVs were applied to cultured embryonic neural stem cells, activation of the IGF-mammalian target of rapamycin complex 1 pathway was observed leading to increased proliferation, suggesting that these nanovesicles are functional (Feliciano et al., 2014). These results have gained traction and have led researchers to the consensus that EVs may serve a greater role in the CNS than originally believed. Taken together, several independent lines of investigation have found that EVs are involved with the development and signaling between different cell types in the CNS.
Several recent studies have found that EVs contribute to neurogenesis. EVs isolated from human induced pluripotent stem cells (hiPSC) increase neurogenesis through enhanced cell proliferation and differentiation of human neuronal cultures (Sharma et al., 2019). In their in vivo experiments they found that purified EVs injected into the lateral ventricle of mouse neonates increase hippocampal neurogenesis. In addition, using hiPSC models of the neurodevelopmental disorder Rett syndrome, it was found that the patient-derived cells produced abnormal EVs lacking several vital proteins for neurogenesis. Furthermore, treating Rett syndrome hiPSC neurons with EVs derived from an isogenic control successfully rescued neurodevelopmental deficits by increasing cell proliferation, synaptogenesis, synchronized firing, and neurogenesis compared with EVs derived from patient hiPSC neurons (Sharma et al., 2019). These results provide evidence for the important role that EVs have in neurogenesis.
Recent findings from invertebrate models also support the notion that EVs contribute to synaptogenesis, implying that using EVs in neurodevelopment appears to be a widely used mechanism among both vertebrate and invertebrate model organisms. For example, in Drosophila larvae, EVs have been shown to be involved in the Wnt signaling pathway, which is necessary for the proper formation of NMJs (Korkut et al., 2009, 2013). These EVs are released from glutamatergic neurons at NMJs; contain evenness disrupted, Wntless, Sprinter (Evi/Wis/Srt) proteins; and are mediated through dGRIP. Wnt- and Evi-containing EVs can also induce Wnt signaling in recipient cells of human origin (Gross et al., 2012). Intriguingly, synaptotagmins, a family of critical membrane trafficking and fusion proteins, that are yet to be linked to EV processes in mammalian cells, have been implicated in regulation of EVs at the Drosophila NMJs. In particular, evidence suggests that synaptotagmin 4 (Syt4) in neurons is essential for Syt4 to accumulate in both the neuron and muscle (Korkut et al., 2013). This finding is even more exciting as Syt4 contributes to synaptic plasticity, synapse strengthening, and learning and memory (Dean et al., 2009; Ferguson et al., 2001). These lines of evidence in concert with the findings of Sharma et al. have led to a large interest in EVs as a potential mode and regulator of CNS development.
EVs carrying important cargo have been previously shown to be released by neurons during synaptic communication. For example, depolarization of primary rodent cortical neurons by KCl, or treatment with the calcium ionophore ionomycin to induce Ca2+ influx, induces a robust release of EVs (Lachenal et al., 2011). In addition, bath application of the excitatory neurotransmitter glutamate increases EV release and antagonizing AMPA and NMDA receptors blocked this process (Goldie et al., 2014). These findings suggest that various stimuli can trigger EV release from neurons, further confirming their heterogeneity. Considering this point, future studies should investigate and decipher the possibility that different stimuli may play a key role in modifying EV cargo selection. Recent studies have revealed that EVs derived from mammalian neurons contain Arc mRNA and protein, further supporting the role of EVs in synaptic communication. Arc is an activity-regulated immediate-early gene and a key governor of synaptic plasticity in processes such as long-term potentiation and long-term depression. The Drosophila Arc1 (dArc1), which forms capsid-like structures and readily binds dArc1 mRNA, has been shown to transfer from motor neurons to muscles via EVs at NMJs (Ashley et al., 2018). In addition, the mammalian Arc protein self-assembles into capsid-like oligomers that encapsulate Arc mRNA and are released from rodent neurons via EVs (Box 1). These EVs are transferred to recipient cells where Arc mRNA undergoes activity-dependent translation (Pastuzyn et al., 2018). Taken together with the previous results linking EVs and Wnt signaling, EVs appear to be important for synaptic signaling in both vertebrate and invertebrates. These findings suggest that EVs contribute to communication between neurons and at NMJs.
Glia-derived EVs can further influence neurodevelopment. For example, astrocyte-derived EVs transfer synapsin 1 (Syn1) to neurons and contribute to neurodevelopment by promoting neurite outgrowth and survival (Wang et al., 2011). Thus EVs released from multiple cell types seem to play key roles in neurodevelopmental events (e.g., Arc and Wnt proteins associated with neuronal EVs and synapsin-1 with astrocytes). Furthermore, at least some EV characteristics seem to depend on the cellular origin. Confirming the highly dynamic nature of EVs, at later development stages, EVs have been found to negatively regulate myelination, as oligodendrocyte-derived EVs robustly downregulate myelin membrane formation, a reversible process that also requires inhibitory signals from neurons (Bakhti et al., 2011). Furthermore, in glia, EVs have been shown to be released in response to glutamate, as well as multiple inflammatory factors, such as adenosine triphosphate (ATP), interleukins (IL), and tumor necrosis factor (Datta Chaudhuri et al., 2020; Fruhbeis et al., 2013; Yang et al., 2018). These findings further suggest that EVs mediate intercellular communication between multiple CNS cell types in response to a variety of stimuli.
Several recent studies have sought to investigate the possibility that CNS EVs represent underappreciated mediators of cell type-specific intercellular communication. For example, one study discovered that neurons secrete exosomes containing discrete miRNAs using a cell-specific exosome reporter mouse model. Specifically, these exosomes contained miR124-3p that is internalized by astrocytes and drives the elevation of glutamate transporter 1 protein (Men et al., 2019). Interestingly, other miRNAs (i.e., miR-274) in microglia-derived EVs help coordinate the growth of synaptic boutons and tracheal branches in recipient neurons (Tsai et al., 2019). Further support for the possibility that EVs are key facilitators of intercellular communication in the CNS between different cell types comes from in vitro and in vivo experiments. Interestingly, when exposed to EVs purified from microglia cells, cultured neurons or neurons in mouse brains show elevated frequency of miniature excitatory postsynaptic currents. Furthermore, the mechanism underlying this process appears to require elevated levels of neuronal ceramide and sphingosine serotonin release (Antonucci et al., 2012). Additional evidence supporting the importance of glial-derived EVs from oligodendrocytes and Schwann cells has been described at length in previous reviews (Budnik et al., 2016).
EVs also contribute to axon guidance and synaptic pruning in the developing CNS-based independent results from several laboratories. Several important axon guidance factors have been found in EVs. EVs released from the glioblastoma U-251MG cell line and cultured neurons contain Eph receptor tyrosine kinases and ephrin ligands, which are important for synaptic plasticity and neuronal development (Gong et al., 2016). More so, treating cells with ephrin-Eph-containing EVs induces ephrinB1 tyrosine phosphorylation and neuronal growth cone collapse causing neuronal axon repulsion. Recently, a fragment of Nogo-A and its receptor NgR1, which play key roles in neurite outgrowth and branching, were found on exosomal membranes. Furthermore, these exosomes inhibited axonal regeneration of mechanically injured cortical neurons from mice (Sekine et al., 2020). EV-based communication between PC12 and MCG6 microglial cells can trigger rapid phagocytosis of degenerating neurites (Bahrini et al., 2015). Finally, primary human astrocytes stimulated with IL-1β release EVs that reduce neuronal outgrowth, branching, and firing (You et al., 2020). Taken together, these results show that diverse intercellular EV communication contributes to neurite dynamics in the CNS.
Neurodegeneration
The initial discovery that EVs harbor the Prion protein (PrPsc) catalyzed the hypotheses that EVs carry and spread misfolded proteins in the CNS (Fevrier et al., 2004). This is important as the mechanisms responsible for the spreading of pathology across the brain in neurodegenerative diseases such as Alzheimer disease (AD) and Parkinson disease (PD) remain largely unknown. Multiple neurodegenerative diseases including prion disease follow a predictable pattern of pathological spreading in the brain (Goedert, 2015), and numerous laboratories have reported that EVs transfer pathology to neighboring cells. However, this field is in its infancy and little is known about how EVs physically spread pathology in the human brain (Figure 2). It is currently unclear if these aberrantly misfolded proteins are bona fide EV cargos, or if they are loaded into EVs as a nonspecific last-ditch “junk removal” effort causing unintended spreading of pathology. Both mechanisms seem feasible as the concept that cells extrude misfolded proteins that are poor substrates for intracellular degradation by the ubiquitin/proteasome system (UPS) or autophagy-lysosome pathways (ALP) is intuitive. Moreover, the disposal of unwanted proteins by EVs as a mechanism to cope with the buildup of toxic proteins may be particularly important in long-lived postmitotic neurons, because they cannot be diluted through cell division. Consistently, exosomes isolated from cultured murine CNS and peripheral neuronal cell lines (i.e., CAD5 and N2A, respectively) contain PrPsc (Fevrier et al., 2004). A connection between EVs and autophagy, a key protein degradation pathway for clearing misfolded proteins in multiple neurodegenerative diseases, has been observed (Abdulrahman et al., 2018; Nah et al., 2015). Interestingly, stimulating autophagy with rapamycin has been shown to inhibit exosome-mediated release of PrPsc, whereas inhibiting autophagy stimulated the release of exosomes containing PrPsc (Abdulrahman et al., 2018). These lines of evidence suggest that EVs may spread pathology due to the failed or overrun protein degradation pathways, thus exacerbating neurodegeneration.
Figure 2.
Potential Roles of EVs in Neurodegeneration
(A) In AD, exosomes containing Aβ and tau may promote protein aggregation and spreading of pathology to neighboring cells or blood vessels.
(B) In ALS, exosomes contain and propagate both SOD1 and TDP-43.
(C) Seminal findings in the CNS revealed the presence PrPsc in EVs that can prorogate prion pathology through blood vessels. These findings represent the pioneering connection between EVs and neurodegeneration.
(D) In PD, EVs containing α-synuclein have been linked to defective ALP and increased extracellular α-synuclein.
(E) Multiple lines of evidence suggest that EVs may also play a role in regulating or spreading inflammation in the CNS, which is a key aspect of many neurodegenerative diseases.
In addition, EVs had been associated with AD, PD, amyotrophic lateral sclerosis (ALS), Huntington disease, and acute brain trauma such as traumatic brain injury and stroke (Budnik et al., 2016; Chen and Chopp, 2018; Ebrahimkhani et al., 2017; Pearce et al., 2015; Xiong et al., 2017). One common aspect shared between these diseases is the presence of neuroinflammation and oxidative stress. Features of EV cargo include multiple pro- and anti-inflammatory molecules that may modulate the CNS inflammatory burden (Gupta and Pulliam, 2014). In addition, EVs have also been associated with oxidative stress (Eldh et al., 2010). Taken together, EVs likely play diverse roles in neuronal protection, maintenance, and repair. Although these studies will only be mentioned briefly here, we point readers to several other reviews on this topic (Budnik et al., 2016; Holm et al., 2018).
Alzheimer Disease
AD is a progressive neurodegenerative condition that represents the most common form of dementia. AD is pathologically characterized by the presence of senile amyloid-beta (Aβ) plaques and neurofibrillary tangles containing hyperphosphorylated tau. AD pathophysiology is complex and depends on the interplay between protein trafficking, folding, and degradation pathways. In addition to these pathological drivers, neuroinflammation is also emerging as an important contributor to the progression of AD (Masters et al., 2015). In this section we provide a comprehensive review of EVs and their relationship to AD pathology.
Neurotoxic Aβ42 peptides are generated from amyloidogenic proteolytic cleavage of the amyloid-precursor protein (App), a type-1 transmembrane glycoprotein, by β- and γ-secretases (Chen et al., 2017). In vitro experiments have shown that full-length App is internalized from the cell surface by clathrin-mediated endocytosis (Nordstedt et al., 1993). Cleavage of App by β-secretase likely occurs in the early endosome; consequently Aβ is directed to MVBs and is released with EVs (Lah and Levey, 2000; Rajendran et al., 2006; Vassar et al., 1999). The overlapping similarities in App processing and Aβ synthesis with EV biogenesis (see sections earlier) presents the idea that these molecules may be present in EV cargo. Verifying this intuitive claim, both full-length App and App fragments appear to be constituents of EV cargo (Perez-Gonzalez et al., 2012). Consistently, pathogenic Aβ42 also localizes to MVBs in mouse, rat, and human neurons in vitro (Takahashi et al., 2002). Taken together these findings show that EVs are associated with App processing and Aβ release, which suggests they play an underappreciated role in amyloid pathology.
In addition to Aβ being associated with EVs, EVs have been linked to extracellular plaques, as the EV makers Alix and flotllin-1 have been found to be associated with Aβ plaques (Rajendran et al., 2006). Furthermore, EVs purified from postmortem AD brain are enriched with oligomeric Aβ peptides (Sardar Sinha et al., 2018). As is the case in neurodevelopment, multiple cell types release EVs that are involved in Aβ pathology and each serves diverse functions in AD pathogenesis. For example, astrocyte-derived EVs exposed to Aβ induce amyloid formation in vivo and sequentially hamper Aβ uptake by microglia and astrocytes (Dinkins et al., 2014). In addition, microglia secrete EVs containing Aβ that are toxic to cultured neurons (Joshi et al., 2014). This contributes to the growing body of evidence showing that EVs may spread amyloid pathology. Similar results have been obtained from multiple AD models and in actual human subjects with AD. Consistently, EVs isolated from a variety of AD models and human tissue are enriched with Aβ42 compared with Aβ40 (Eitan et al., 2016). These EVs are toxic because when applied to cultured neurons, they triggered apoptosis and mitochondrial dysfunction. Furthermore, administration of the ceramide synthesis GW4869 inhibitor to 5XFAD mice, or crossing 5XFAD with nSMase2 −/− mice, reduced the Aβ plaque load (Dinkins et al., 2014, 2016). These results suggest that EVs contribute to the Aβ burden and therefore could represent a potential target for therapeutics.
Clearance of toxic polypeptides represents an early line of cellular defense for mitigating pathology in multiple neurodegenerative diseases including AD (Malik et al., 2019; Wolfe et al., 2013). Consistently, pharmacological and genetic inhibition of lysosomal activity leads to increased levels of Aβ42 in EVs (Eitan et al., 2016). However, further research is needed to expand on these initial findings to determine the relationship between impaired Aβ42 degradation and its secretion through EVs. Interestingly, extracellular Aβ levels are elevated by synaptic activity and decreased synaptic transmission dramatically reduces Aβ levels in brain interstitial fluid (ISF) (Cirrito et al., 2005). This process has been shown to require endocytosis because inhibition of this process led to a rapid 70% decrease of Aβ in ISF. As cleavage and processing of pathogenic Aβ occurs via the endocytic pathway, and neuronal activity increases Aβ in an endocytosis-dependent manner (Cirrito et al., 2008), activity-dependent release of EVs could be one mechanism responsible for spreading Aβ pathology.
Although there is abundant evidence showing that EVs exacerbate Aβ pathology, other evidence suggests that EVs help to reduce Aβ levels. Aβ-degrading enzymes such as neprilysin (NEP) and insulin-degrading enzymes (IDE) are major regulators of Aβ peptide levels in the brain. EVs from N2a neuroblastoma and microglia BV-2 cells have been shown to promote degradation of Aβ through EV-associated IDEs (Bulloj et al., 2010; Tamboli et al., 2010). More specifically, EVs from human adipose tissue-derived mesenchymal stem cells (ADSCs) contain enzymatically active NEP that can potentially degrade Aβ (Katsuda et al., 2013). Similarly, intracerebral injection of ADSC-derived EVs reduced Aβ plaque burden in APP/PS1 AD model mice (Elia et al., 2019). Neuron-derived EVs have been shown to facilitate Aβ uptake and degradation by microglia by promoting conformational changes of Aβ nontoxic fibrils (Yuyama et al., 2012). These results point to EVs playing a two-sided role in amyloid pathology; on one side, by propagating and spreading Aβ peptides, whereas on the other side by mitigating amyloid load in the brain by promoting clearance of Aβ. These results provide an interesting framework for the apparently complex role of EVs in AD pathology and highlight the dynamic and contrasting nature of EVs.
Neurofibrillary tangles composed of hyperphosphorylated tau correlate with the progression of AD pathology (Serrano-Pozo et al., 2011). Tau pathology is thought to occur downstream or in parallel with Aβ effects, occurs before the onset of AD cognitive deficits, and spreads throughout the brain in a predictable manner. Given EVs' role in the spreading of neurodegenerative disease pathology, the hypothesis that EVs facilitate tau spreading has been put forth. Evidence from multiple laboratories supports this possibility as EVs derived from the human AD extracts and cultured neurons carry misfolded tau as cargo (Saman et al., 2012; Wang et al., 2017). Further studies suggest that microglia-derived EVs specifically propagate tau pathology, as cultured microglia phagocytose tau proteins and release tau-containing EVs when stimulated with lipopolysaccharides, ATP, or KCl. These findings further the notion that multiple stimuli trigger EV release. Future studies should investigate the possibility that these stimuli regulate EV cargo selection and function. Additional evidence for the role of microglia in tau pathology comes from their findings that inhibiting ceramide production with GW4869, knocking down Smase2 expression with small interfering RNAs (siRNAs), or depleting the microglia pool all reduce tau pathology (Asai et al., 2015; Wang et al., 2017). Consistent with these findings, EVs containing P301L mutant tau accelerate pathological tau phosphorylation and oligomer formation but interestingly do not seed mature NFTs in ALZ17 mice (Baker et al., 2016). It is important to note, however, that several tau phosphoepitopes (AT8, AT100, and AT180), which are critical for AD pathology, were undetected and the level of tau in EVs was significantly higher in transgenic mice with pronounced tau pathology (Polanco et al., 2016). It will be important to determine if EVs containing Aβ or tau exacerbate pathology independently or in concert because both appear to be released in response to increased synaptic activity (Ittner and Götz, 2011).
Parkinson Disease
PD is a neurodegenerative disease pathologically characterized by selective loss of dopaminergic neurons and accumulation of the misfolded presynaptic protein α-synuclein in Lewy bodies (Poewe et al., 2017; Spinelli et al., 2014). Pathological Lewy body aggregates propagate in a caudorostral direction, suggesting an organized spreading mechanism (Goedert, 2015). As with AD, it has been hypothesized that EVs may contribute to PD pathophysiology by transporting toxic proteins such as α-synuclein across the brain. In fact, EVs derived from human PD plasma or CSF have been shown to contain oligomerized α-synuclein (Shi et al., 2014; Stuendl et al., 2016). However, an important caveat to these findings is that the amount of α-synuclein within EVs is minimal compared with the overall level extracellularly. Nonetheless, EVs can transfer oligomerized α-synuclein between cells (Danzer et al., 2012), and these EVs are released in a Ca2+-dependent manner and cellular uptake induces cell death (Emmanouilidou et al., 2010).
Similar to AD, UPS and ALP protein degradation pathways are hampered in PD model systems and patients (Bellomo et al., 2020), and dysfunctional protein degradation pathways can drive EV release. In a similar way, inhibition of the ALP or reducing lysosomal function results in diminished intercellular α-synuclein aggregates, but elevated extracellular α-synuclein levels (Minakaki et al., 2018; Poehler et al., 2014). These data suggest that targeting defective protein degradation pathways may offer a promising therapeutic strategy to mitigate pathological spreading in both AD and PD by EVs. Altogether these studies show that release of EVs containing α-synuclein can be exacerbated by impaired protein degradation pathways.
Amyotrophic Lateral Sclerosis
ALS is the most common neurodegenerative disease of motor neurons. The genetic alterations underlying ALS include mutations of transactive response DNA-binding protein 43 KD (TDP-43) and Cu/Zn superoxide dismutase 1 (SOD1) among a growing panel of additional genes. Mutations to these genes correlate with motor neuron degeneration and additional ALS symptoms (Hardiman et al., 2017). TDP-43 has been identified as a component of EVs in ALS and frontotemporal dementia (FTD) cell models (Nonaka et al., 2013). Furthermore, TDP-43 is located in both the EV lumen and with the outer membrane. As EVs are preferentially internalized by cells, EVs with TDP-43 exacerbate toxicity compared with purified TDP-43 protein (Feiler et al., 2015), and EVs from CSF of patients with ALS and FTD contain TDP-43 and can mediate protein aggregation (Ding et al., 2015). On the other hand, some evidence suggests that EVs play a protective role by clearing TDP-43 in EVs from neurons but not astrocytes (Iguchi et al., 2016). Blocking EV biogenesis by inhibiting ceramide synthesis or knocking down Rab27a with siRNAs in Neuro2a cells exacerbates TDP-43 aggregation, suggesting that EVs may help mitigate toxicity (Iguchi et al., 2016). The precise role of EVs in TDP-43 pathology is unclear, but the evidence suggests a highly complex process. The breadth of evidence on the relationship between SOD1 and EVs is not nearly as deep as for TDP-43, but studies suggest that EVs may contribute to worsened SOD1 prognosis. For example, wild-type and mutant SOD1 are present in EVs, and misfolded mutant SOD1 can be transferred between motor neuron-like mouse NSC-4 cells (Gomes et al., 2007). In support that EVs spread SOD1 pathology, astrocytes over-expressing mutant SOD1 secrete EVs containing mutant SOD1 that are toxic to wild-type motor neurons (Basso et al., 2013). Furthermore, conditioned media from HEK293 cells expressing human and mutant SOD1 or mouse primary spinal cord cells expressing human and wild-type SOD1 could induce SOD1 misfolding across several rounds of cell division (Grad et al., 2014). However, although these results are interesting, further studies investigating SOD1 and its relationship between EVs is necessary. Collectively these findings support a role for EVs in ALS, which are reminiscent of their contributions in PD and AD.
EVs as Liquid Biomarkers and Drug Delivering Vehicles for CNS Diseases
As a result of EVs having been shown to contain Aβ, α-synuclein, TDP-43, and SOD1, using EVs as biomarkers of neurodegenerative diseases may represent an important noninvasive and promising strategy for identifying at-risk individuals and tracking disease progression (Ding et al., 2015; Lin et al., 2015; Saman et al., 2012; Sardar Sinha et al., 2018; Shi et al., 2014; Stuendl et al., 2016). A wide range of biological fluids including blood, CSF, and urine, have been used as source material to isolate EVs, and these convenient avenues for EV isolation could provide key early indicators of disease progression or successful therapeutic interventions.
EVs could also be used as potential vehicles for the targeted delivery of drugs combatting various CNS aliments. The blood-brain barrier (BBB) is composed of several different cell types acting as a selective barrier to protect the brain, and many peptides, proteins, and small molecules are impermeable (Zlokovic, 2008). Consequently, the BBB significantly hampers our ability to efficiently deliver drugs to the brain (Pardridge, 2005). EVs, however, are able to cross the BBB, thus representing a promising candidate for cell type-specific drug delivery in the CNS (Zheng et al., 2019). The mechanism by which EVs pass the BBB seems to depend on EV surface ligands, and their receptors expressed endothelial cell plasma membranes. For example, naive macrophage-derived exosomes can pass the BBB using lymphocyte function-associated antigen 1 or intercellular adhesion molecule 1 with carbohydrate-binding C-type lectin receptors on brain endothelial cells (Yuan et al., 2017). Importantly, other proteins on EV surfaces are involved and additional BBB entry mechanisms exist that have been covered extensively in other reviews (Zheng et al., 2019). Adding to the possibility to utilize EVs as potential drug delivery vehicles, EVs also offer the advantage of being synthesized and potentially loaded by the cellular machinery in vitro. This is a clear advantage compared with liposomes or polymeric nanoparticles prepared in test tubes, as EVs may have higher biocompatibility and longer circulation times with low immunogenicity and toxicity (Zheng et al., 2019).
Several recent studies attempted to use EVs as a therapeutic strategy to mitigate pathology in mouse models of neurodegenerative disease. In one study, exosomes isolated from dendritic cells were packaged with BACE1 siRNAs and subsequently reduced BACE1 gene expression (Alvarez-Erviti et al., 2011). In an additional study exosomes isolated from blood were loaded with dopamine and could target the striatum and substantia nigra elevating the overall dopamine levels (Qu et al., 2018). To date, the most compelling evidence that EVs can be used to modulate neurodegeneration comes from several studies on PD and include delivery of EVs containing antioxidants, neurotrophic factors, and α-synuclein siRNAs (Cooper et al., 2014; Haney et al., 2015; Zhao et al., 2014).
Recently, the exciting possibility that EVs can be used to deliver therapeutic cargo to the CNS in a cell-type specific manner has been explored. Cell type-specific directed therapeutics represents a promising strategy for many reasons including the ability to specifically target degenerating neurons (e.g., mid-brain dopaminergic neurons in PD) or promoting a specific desired innate cellular response (e.g., microglia phagocytosis of toxic proteins). Several lines of evidence suggest that different CNS cell types exhibit discrete signaling via EVs. For example, EVs released from cultured neurons preferentially bind to neurons but do not bind to the surface of microglia and astrocytes (Chivet et al., 2014). Another study found that neuroblastoma N2a cells selectively loaded mutant APP into a subset of EVs lacking CD63 that preferentially bind to neuronal dendrites (Laulagnier et al., 2018). In addition, some cells specifically release EVs that contain the major histocompatibility class II proteins, which preferentially bind to microglia (Fitzner et al., 2011).
Although these studies show great potential for using EVs in targeted delivery of drugs to specific cell types, several major technical barriers remain. Among the barriers, it is currently unknown which cells are most appropriate to use to synthesize EVs and how to effectively load them with drugs. Our knowledge of the underlying mechanism is still in its infancy; however, these results are exciting and support the possibility that someday EVs may facilitate drug delivery to discrete CNS cells.
Conclusion
The presented evidence highlights our current understanding of EVs in the CNS during healthy and neurodegenerative conditions, and emphasizes the complexity of EV biology. Although our understanding of these elusive nanovesicles is still in its infancy, we expect that future studies, facilitated by emerging technological advancements will continue to accelerate our ability to determine the precise role of these CNS EVs. Ultimately it will be exciting to see if EVs can be used as effective biomarkers or drug delivery vehicles for neurodegenerative diseases.
Acknowledgments
Exosome research in the Savas Lab is supported by R01 AG061787. We thank Samuel Smukowski and members of the lab for their constructive suggestions.
Author Contributions
D.R.G., Y.-Z.W, A.U., and J.N.S wrote the paper and constructed the figures.
References
- Abdulrahman B.A., Abdelaziz D.H., Schatzl H.M. Autophagy regulates exosomal release of prions in neuronal cells. J. Biol. Chem. 2018;293:8956–8968. doi: 10.1074/jbc.RA117.000713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed I., Akram Z., Iqbal H.M.N., Munn A.L. The regulation of Endosomal Sorting Complex Required for Transport and accessory proteins in multivesicular body sorting and enveloped viral budding - an overview. Int. J. Biol. Macromol. 2019;127:1–11. doi: 10.1016/j.ijbiomac.2019.01.015. [DOI] [PubMed] [Google Scholar]
- Alvarez-Erviti L., Seow Y., Yin H., Betts C., Lakhal S., Wood M.J.A. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat. Biotechnol. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- Antonucci F., Turola E., Riganti L., Caleo M., Gabrielli M., Perrotta C., Novellino L., Clementi E., Giussani P., Viani P. Microvesicles released from microglia stimulate synaptic activity via enhanced sphingolipid metabolism. EMBO J. 2012;31:1231–1240. doi: 10.1038/emboj.2011.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asai H., Ikezu S., Tsunoda S., Medalla M., Luebke J., Haydar T., Wolozin B., Butovsky O., Kügler S., Ikezu T. Depletion of microglia and inhibition of exosome synthesis halt tau propagation. Nat. Neurosci. 2015;18:1584–1593. doi: 10.1038/nn.4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashley J., Cordy B., Lucia D., Fradkin L.G., Budnik V., Thomson T. Retrovirus-like Gag protein Arc1 binds RNA and traffics across synaptic boutons. Cell. 2018;172:262–274.e11. doi: 10.1016/j.cell.2017.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahrini I., Song J.H., Diez D., Hanayama R. Neuronal exosomes facilitate synaptic pruning by up-regulating complement factors in microglia. Sci. Rep. 2015;5:7989. doi: 10.1038/srep07989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baietti M.F., Zhang Z., Mortier E., Melchior A., Degeest G., Geeraerts A., Ivarsson Y., Depoortere F., Coomans C., Vermeiren E. Syndecan–syntenin–ALIX regulates the biogenesis of exosomes. Nat. Cell Biol. 2012;14:677–685. doi: 10.1038/ncb2502. [DOI] [PubMed] [Google Scholar]
- Baker S., Polanco J.C., Gotz J. Extracellular vesicles containing P301L mutant tau accelerate pathological tau phosphorylation and oligomer formation but do not seed mature neurofibrillary tangles in ALZ17 mice. J. Alzheimers Dis. 2016;54:1207–1217. doi: 10.3233/JAD-160371. [DOI] [PubMed] [Google Scholar]
- Bakhti M., Winter C., Simons M. Inhibition of myelin membrane sheath formation by oligodendrocyte-derived exosome-like vesicles. J. Biol. Chem. 2011;286:787–796. doi: 10.1074/jbc.M110.190009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banizs A.B., Huang T., Nakamoto R.K., Shi W., He J. Endocytosis pathways of endothelial cell derived exosomes. Mol. Pharm. 2018;15:5585–5590. doi: 10.1021/acs.molpharmaceut.8b00765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barres C., Blanc L., Bette-Bobillo P., Andre S., Mamoun R., Gabius H.J., Vidal M. Galectin-5 is bound onto the surface of rat reticulocyte exosomes and modulates vesicle uptake by macrophages. Blood. 2010;115:696–705. doi: 10.1182/blood-2009-07-231449. [DOI] [PubMed] [Google Scholar]
- Basso M., Pozzi S., Tortarolo M., Fiordaliso F., Bisighini C., Pasetto L., Spaltro G., Lidonnici D., Gensano F., Battaglia E. Mutant copper-zinc superoxide dismutase (SOD1) induces protein secretion pathway alterations and exosome release in astrocytes: implications for disease spreading and motor neuron pathology in amyotrophic lateral sclerosis. J. Biol. Chem. 2013;288:15699–15711. doi: 10.1074/jbc.M112.425066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellomo G., Paciotti S., Gatticchi L., Parnetti L. The vicious cycle between α-synuclein aggregation and autophagic-lysosomal dysfunction. Mov. Disord. 2020;35:34–44. doi: 10.1002/mds.27895. [DOI] [PubMed] [Google Scholar]
- Budnik V., Ruiz-Canada C., Wendler F. Extracellular vesicles round off communication in the nervous system. Nat. Rev. Neurosci. 2016;17:160–172. doi: 10.1038/nrn.2015.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulloj A., Leal M.C., Xu H., Castano E.M., Morelli L. Insulin-degrading enzyme sorting in exosomes: a secretory pathway for a key brain amyloid-beta degrading protease. J. Alzheimers Dis. 2010;19:79–95. doi: 10.3233/JAD-2010-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campillos M., Doerks T., Shah P.K., Bork P. Computational characterization of multiple Gag-like human proteins. Trends Genet. 2006;22:585–589. doi: 10.1016/j.tig.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Chen G.-F., Xu T.-H., Yan Y., Zhou Y.-R., Jiang Y., Melcher K., Xu H.E. Amyloid beta: structure, biology and structure-based therapeutic development. Acta Pharm. Sin. 2017;38:1205–1235. doi: 10.1038/aps.2017.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Chopp M. Exosome therapy for stroke. Stroke. 2018;49:1083–1090. doi: 10.1161/STROKEAHA.117.018292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chivet M., Javalet C., Laulagnier K., Blot B., Hemming F.J., Sadoul R. Exosomes secreted by cortical neurons upon glutamatergic synapse activation specifically interact with neurons. J. Extracell Vesicles. 2014;3:24722. doi: 10.3402/jev.v3.24722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirrito J.R., Kang J.E., Lee J., Stewart F.R., Verges D.K., Silverio L.M., Bu G., Mennerick S., Holtzman D.M. Endocytosis is required for synaptic activity-dependent release of amyloid-beta in vivo. Neuron. 2008;58:42–51. doi: 10.1016/j.neuron.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirrito J.R., Yamada K.A., Finn M.B., Sloviter R.S., Bales K.R., May P.C., Schoepp D.D., Paul S.M., Mennerick S., Holtzman D.M. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo. Neuron. 2005;48:913–922. doi: 10.1016/j.neuron.2005.10.028. [DOI] [PubMed] [Google Scholar]
- Cooper J.M., Wiklander P.B., Nordin J.Z., Al-Shawi R., Wood M.J., Vithlani M., Schapira A.H., Simons J.P., El-Andaloussi S., Alvarez-Erviti L. Systemic exosomal siRNA delivery reduced alpha-synuclein aggregates in brains of transgenic mice. Mov. Disord. 2014;29:1476–1485. doi: 10.1002/mds.25978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danzer K.M., Kranich L.R., Ruf W.P., Cagsal-Getkin O., Winslow A.R., Zhu L., Vanderburg C.R., McLean P.J. Exosomal cell-to-cell transmission of alpha synuclein oligomers. Mol. Neurodegener. 2012;7:42. doi: 10.1186/1750-1326-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datta Chaudhuri A., Dasgheyb R.M., DeVine L.R., Bi H., Cole R.N., Haughey N.J. Stimulus-dependent modifications in astrocyte-derived extracellular vesicle cargo regulate neuronal excitability. Glia. 2020;68:128–144. doi: 10.1002/glia.23708. [DOI] [PubMed] [Google Scholar]
- Dean C., Liu H., Dunning F.M., Chang P.Y., Jackson M.B., Chapman E.R. Synaptotagmin-IV modulates synaptic function and long-term potentiation by regulating BDNF release. Nat. Neurosci. 2009;12:767–776. doi: 10.1038/nn.2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding X., Ma M., Teng J., Teng R.K., Zhou S., Yin J., Fonkem E., Huang J.H., Wu E., Wang X. Exposure to ALS-FTD-CSF generates TDP-43 aggregates in glioblastoma cells through exosomes and TNTs-like structure. Oncotarget. 2015;6:24178–24191. doi: 10.18632/oncotarget.4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinkins M.B., Dasgupta S., Wang G., Zhu G., Bieberich E. Exosome reduction in vivo is associated with lower amyloid plaque load in the 5XFAD mouse model of Alzheimer's disease. Neurobiol. Aging. 2014;35:1792–1800. doi: 10.1016/j.neurobiolaging.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinkins M.B., Enasko J., Hernandez C., Wang G., Kong J., Helwa I., Liu Y., Terry A.V., Jr., Bieberich E. Neutral sphingomyelinase-2 deficiency ameliorates Alzheimer's disease pathology and improves cognition in the 5XFAD mouse. J. Neurosci. 2016;36:8653–8667. doi: 10.1523/JNEUROSCI.1429-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahimkhani S., Vafaee F., Young P.E., Hur S.S.J., Hawke S., Devenney E., Beadnall H., Barnett M.H., Suter C.M., Buckland M.E. Exosomal microRNA signatures in multiple sclerosis reflect disease status. Sci. Rep. 2017;7:14293. doi: 10.1038/s41598-017-14301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eitan E., Hutchison E.R., Marosi K., Comotto J., Mustapic M., Nigam S.M., Suire C., Maharana C., Jicha G.A., Liu D. Extracellular vesicle-associated Aβ mediates trans-neuronal bioenergetic and Ca(2+)-handling deficits in Alzheimer's disease models. NPJ Aging Mech. Dis. 2016;2:16019. doi: 10.1038/npjamd.2016.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldh M., Ekstrom K., Valadi H., Sjostrand M., Olsson B., Jernas M., Lotvall J. Exosomes communicate protective messages during oxidative stress; possible role of exosomal shuttle RNA. PLoS One. 2010;5:e15353. doi: 10.1371/journal.pone.0015353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elia C.A., Tamborini M., Rasile M., Desiato G., Marchetti S., Swuec P., Mazzitelli S., Clemente F., Anselmo A., Matteoli M. Intracerebral injection of extracellular vesicles from mesenchymal stem cells exerts reduced abeta plaque burden in early stages of a preclinical model of Alzheimer's disease. Cells. 2019;8:1059. doi: 10.3390/cells8091059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmanouilidou E., Melachroinou K., Roumeliotis T., Garbis S.D., Ntzouni M., Margaritis L.H., Stefanis L., Vekrellis K. Cell-produced α-synuclein is secreted in a calcium-dependent manner by exosomes and impacts neuronal survival. J. Neurosci. 2010;30:6838–6851. doi: 10.1523/JNEUROSCI.5699-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erlendsson S., Morado D.R., Cullen H.B., Feschotte C., Shepherd J.D., Briggs J.A.G. Structures of virus-like capsids formed by the Drosophila neuronal Arc proteins. Nat. Neurosci. 2020;23:172–175. doi: 10.1038/s41593-019-0569-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feiler M.S., Strobel B., Freischmidt A., Helferich A.M., Kappel J., Brewer B.M., Li D., Thal D.R., Walther P., Ludolph A.C. TDP-43 is intercellularly transmitted across axon terminals. J. Cell Biol. 2015;211:897–911. doi: 10.1083/jcb.201504057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feliciano D.M., Zhang S., Nasrallah C.M., Lisgo S.N., Bordey A. Embryonic cerebrospinal fluid nanovesicles carry evolutionarily conserved molecules and promote neural stem cell amplification. PLoS One. 2014;9:e88810. doi: 10.1371/journal.pone.0088810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng D., Zhao W.L., Ye Y.Y., Bai X.C., Liu R.Q., Chang L.F., Zhou Q., Sui S.F. Cellular internalization of exosomes occurs through phagocytosis. Traffic. 2010;11:675–687. doi: 10.1111/j.1600-0854.2010.01041.x. [DOI] [PubMed] [Google Scholar]
- Ferguson G.D., Vician L., Herschman H.R. Synaptotagmin IV: biochemistry, genetics, behavior, and possible links to human psychiatric disease. Mol. Neurobiol. 2001;23:173–185. doi: 10.1385/MN:23:2-3:173. [DOI] [PubMed] [Google Scholar]
- Fevrier B., Vilette D., Archer F., Loew D., Faigle W., Vidal M., Laude H., Raposo G. Cells release prions in association with exosomes. Proc. Natl. Acad. Sci. U S A. 2004;101:9683–9688. doi: 10.1073/pnas.0308413101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipe V., Hawe A., Jiskoot W. Critical evaluation of Nanoparticle Tracking Analysis (NTA) by NanoSight for the measurement of nanoparticles and protein aggregates. Pharm. Res. 2010;27:796–810. doi: 10.1007/s11095-010-0073-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzner D., Schnaars M., van Rossum D., Krishnamoorthy G., Dibaj P., Bakhti M., Regen T., Hanisch U.-K., Simons M. Selective transfer of exosomes from oligodendrocytes to microglia by macropinocytosis. J. Cell Sci. 2011;124:447–458. doi: 10.1242/jcs.074088. [DOI] [PubMed] [Google Scholar]
- Fomina A.F., Deerinck T.J., Ellisman M.H., Cahalan M.D. Regulation of membrane trafficking and subcellular organization of endocytic compartments revealed with FM1-43 in resting and activated human T cells. Exp. Cell Res. 2003;291:150–166. doi: 10.1016/s0014-4827(03)00372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franch-Marro X., Wendler F., Guidato S., Griffith J., Baena-Lopez A., Itasaki N., Maurice M.M., Vincent J.P. Wingless secretion requires endosome-to-Golgi retrieval of Wntless/Evi/Sprinter by the retromer complex. Nat. Cell Biol. 2008;10:170–177. doi: 10.1038/ncb1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fruhbeis C., Frohlich D., Kuo W.P., Amphornrat J., Thilemann S., Saab A.S., Kirchhoff F., Mobius W., Goebbels S., Nave K.A. Neurotransmitter-triggered transfer of exosomes mediates oligodendrocyte-neuron communication. PLoS Biol. 2013;11:e1001604. doi: 10.1371/journal.pbio.1001604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujii K., Hurley J.H., Freed E.O. Beyond Tsg101: the role of Alix in 'ESCRTing' HIV-1. Nat. Rev. Microbiol. 2007;5:912–916. doi: 10.1038/nrmicro1790. [DOI] [PubMed] [Google Scholar]
- Gardiner C., Di Vizio D., Sahoo S., Thery C., Witwer K.W., Wauben M., Hill A.F. Techniques used for the isolation and characterization of extracellular vesicles: results of a worldwide survey. J. Extracell Vesicles. 2016;5:32945. doi: 10.3402/jev.v5.32945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goedert M. Alzheimer’s and Parkinson’s diseases: the prion concept in relation to assembled Aβ, tau, and α-synuclein. Science. 2015;349:1255555. doi: 10.1126/science.1255555. [DOI] [PubMed] [Google Scholar]
- Goldie B.J., Dun M.D., Lin M., Smith N.D., Verrills N.M., Dayas C.V., Cairns M.J. Activity-associated miRNA are packaged in Map1b-enriched exosomes released from depolarized neurons. Nucleic Acids Res. 2014;42:9195–9208. doi: 10.1093/nar/gku594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomes C., Keller S., Altevogt P., Costa J. Evidence for secretion of Cu,Zn superoxide dismutase via exosomes from a cell model of amyotrophic lateral sclerosis. Neurosci. Lett. 2007;428:43–46. doi: 10.1016/j.neulet.2007.09.024. [DOI] [PubMed] [Google Scholar]
- Gong J., Körner R., Gaitanos L., Klein R. Exosomes mediate cell contact–independent ephrin-Eph signaling during axon guidance. J. Cell Biol. 2016;214:35–44. doi: 10.1083/jcb.201601085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grad L.I., Yerbury J.J., Turner B.J., Guest W.C., Pokrishevsky E., O'Neill M.A., Yanai A., Silverman J.M., Zeineddine R., Corcoran L. Intercellular propagated misfolding of wild-type Cu/Zn superoxide dismutase occurs via exosome-dependent and -independent mechanisms. Proc. Natl. Acad. Sci. U S A. 2014;111:3620–3625. doi: 10.1073/pnas.1312245111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross J.C., Chaudhary V., Bartscherer K., Boutros M. Active Wnt proteins are secreted on exosomes. Nat. Cell Biol. 2012;14:1036–1045. doi: 10.1038/ncb2574. [DOI] [PubMed] [Google Scholar]
- Gupta A., Pulliam L. Exosomes as mediators of neuroinflammation. J. Neuroinflammation. 2014;11:68. doi: 10.1186/1742-2094-11-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haney M.J., Klyachko N.L., Zhao Y., Gupta R., Plotnikova E.G., He Z., Patel T., Piroyan A., Sokolsky M., Kabanov A.V. Exosomes as drug delivery vehicles for Parkinson's disease therapy. J. Control Release. 2015;207:18–30. doi: 10.1016/j.jconrel.2015.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardiman O., Al-Chalabi A., Chio A., Corr E.M., Logroscino G., Robberecht W., Shaw P.J., Simmons Z., van den Berg L.H. Amyotrophic lateral sclerosis. Nat. Rev. Dis. Primers. 2017;3:17071. doi: 10.1038/nrdp.2017.71. [DOI] [PubMed] [Google Scholar]
- Harding C., Heuser J., Stahl P. Receptor-mediated endocytosis of transferrin and recycling of the transferrin receptor in rat reticulocytes. J. Cell Biol. 1983;97:329–339. doi: 10.1083/jcb.97.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heijnen H.F., Schiel A.E., Fijnheer R., Geuze H.J., Sixma J.J. Activated platelets release two types of membrane vesicles: microvesicles by surface shedding and exosomes derived from exocytosis of multivesicular bodies and alpha-granules. Blood. 1999;94:3791–3799. [PubMed] [Google Scholar]
- Holm M.M., Kaiser J., Schwab M.E. Extracellular vesicles: multimodal envoys in neural maintenance and repair. Trends Neurosci. 2018;41:360–372. doi: 10.1016/j.tins.2018.03.006. [DOI] [PubMed] [Google Scholar]
- Hurley J.H., Hanson P.I. Membrane budding and scission by the ESCRT machinery: it's all in the neck. Nat. Rev. Mol. Cell Biol. 2010;11:556–566. doi: 10.1038/nrm2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iguchi Y., Eid L., Parent M., Soucy G., Bareil C., Riku Y., Kawai K., Takagi S., Yoshida M., Katsuno M. Exosome secretion is a key pathway for clearance of pathological TDP-43. Brain. 2016;139:3187–3201. doi: 10.1093/brain/aww237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ittner L.M., Götz J. Amyloid-β and tau — a toxic pas de deux in Alzheimer's disease. Nat. Rev. Neurosci. 2011;12:67–72. doi: 10.1038/nrn2967. [DOI] [PubMed] [Google Scholar]
- Jahn R., Lang T., Sudhof T.C. Membrane fusion. Cell. 2003;112:519–533. doi: 10.1016/s0092-8674(03)00112-0. [DOI] [PubMed] [Google Scholar]
- Ji Y., Qi D., Li L., Su H., Li X., Luo Y., Sun B., Zhang F., Lin B., Liu T. Multiplexed profiling of single-cell extracellular vesicles secretion. Proc. Natl. Acad. Sci. U S A. 2019;116:5979–5984. doi: 10.1073/pnas.1814348116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnstone R.M., Adam M., Hammond J.R., Orr L., Turbide C. Vesicle formation during reticulocyte maturation. Association of plasma membrane activities with released vesicles (exosomes) J. Biol. Chem. 1987;262:9412–9420. [PubMed] [Google Scholar]
- Joshi P., Turola E., Ruiz A., Bergami A., Libera D.D., Benussi L., Giussani P., Magnani G., Comi G., Legname G. Microglia convert aggregated amyloid-beta into neurotoxic forms through the shedding of microvesicles. Cell Death Differ. 2014;21:582–593. doi: 10.1038/cdd.2013.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim M.A., Samyn D.R., Mattie S., Brett C.L. Distinct features of multivesicular body-lysosome fusion revealed by a new cell-free content-mixing assay. Traffic. 2018;19:138–149. doi: 10.1111/tra.12543. [DOI] [PubMed] [Google Scholar]
- Katsuda T., Tsuchiya R., Kosaka N., Yoshioka Y., Takagaki K., Oki K., Takeshita F., Sakai Y., Kuroda M., Ochiya T. Human adipose tissue-derived mesenchymal stem cells secrete functional neprilysin-bound exosomes. Sci. Rep. 2013;3:1197. doi: 10.1038/srep01197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkut C., Ataman B., Ramachandran P., Ashley J., Barria R., Gherbesi N., Budnik V. Trans-synaptic transmission of vesicular Wnt signals through Evi/Wntless. Cell. 2009;139:393–404. doi: 10.1016/j.cell.2009.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkut C., Li Y., Koles K., Brewer C., Ashley J., Yoshihara M., Budnik V. Regulation of postsynaptic retrograde signaling by presynaptic exosome release. Neuron. 2013;77:1039–1046. doi: 10.1016/j.neuron.2013.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachenal G., Pernet-Gallay K., Chivet M., Hemming F.J., Belly A., Bodon G., Blot B., Haase G., Goldberg Y., Sadoul R. Release of exosomes from differentiated neurons and its regulation by synaptic glutamatergic activity. Mol. Cell Neurosci. 2011;46:409–418. doi: 10.1016/j.mcn.2010.11.004. [DOI] [PubMed] [Google Scholar]
- Lah J.J., Levey A.I. Endogenous presenilin-1 targets to endocytic rather than biosynthetic compartments. Mol. Cell Neurosci. 2000;16:111–126. doi: 10.1006/mcne.2000.0861. [DOI] [PubMed] [Google Scholar]
- Laulagnier K., Javalet C., Hemming F.J., Chivet M., Lachenal G., Blot B., Chatellard C., Sadoul R. Amyloid precursor protein products concentrate in a subset of exosomes specifically endocytosed by neurons. Cell Mol Life Sci. 2018;75:757–773. doi: 10.1007/s00018-017-2664-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., Li J., Huang B., Liu J., Chen X., Chen X.M., Xu Y.M., Huang L.F., Wang X.Z. Exosomes: novel biomarkers for clinical diagnosis. ScientificWorldJournal. 2015;2015:657086. doi: 10.1155/2015/657086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livshits M.A., Khomyakova E., Evtushenko E.G., Lazarev V.N., Kulemin N.A., Semina S.E., Generozov E.V., Govorun V.M. Isolation of exosomes by differential centrifugation: theoretical analysis of a commonly used protocol. Sci. Rep. 2015;5:17319. doi: 10.1038/srep17319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik B.R., Maddison D.C., Smith G.A., Peters O.M. Autophagic and endo-lysosomal dysfunction in neurodegenerative disease. Mol. Brain. 2019;12:100. doi: 10.1186/s13041-019-0504-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzesco A.M., Janich P., Wilsch-Brauninger M., Dubreuil V., Langenfeld K., Corbeil D., Huttner W.B. Release of extracellular membrane particles carrying the stem cell marker prominin-1 (CD133) from neural progenitors and other epithelial cells. J. Cell Sci. 2005;118:2849–2858. doi: 10.1242/jcs.02439. [DOI] [PubMed] [Google Scholar]
- Masters C.L., Bateman R., Blennow K., Rowe C.C., Sperling R.A., Cummings J.L. Alzheimer's disease. Nat. Rev. Dis. Primers. 2015;1:15056. doi: 10.1038/nrdp.2015.56. [DOI] [PubMed] [Google Scholar]
- Men Y., Yelick J., Jin S., Tian Y., Chiang M.S.R., Higashimori H., Brown E., Jarvis R., Yang Y. Exosome reporter mice reveal the involvement of exosomes in mediating neuron to astroglia communication in the CNS. Nat. Commun. 2019;10:4136. doi: 10.1038/s41467-019-11534-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minakaki G., Menges S., Kittel A., Emmanouilidou E., Schaeffner I., Barkovits K., Bergmann A., Rockenstein E., Adame A., Marxreiter F. Autophagy inhibition promotes SNCA/alpha-synuclein release and transfer via extracellular vesicles with a hybrid autophagosome-exosome-like phenotype. Autophagy. 2018;14:98–119. doi: 10.1080/15548627.2017.1395992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montecalvo A., Larregina A.T., Shufesky W.J., Stolz D.B., Sullivan M.L., Karlsson J.M., Baty C.J., Gibson G.A., Erdos G., Wang Z. Mechanism of transfer of functional microRNAs between mouse dendritic cells via exosomes. Blood. 2012;119:756–766. doi: 10.1182/blood-2011-02-338004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morelli A.E., Larregina A.T., Shufesky W.J., Sullivan M.L., Stolz D.B., Papworth G.D., Zahorchak A.F., Logar A.J., Wang Z., Watkins S.C. Endocytosis, intracellular sorting, and processing of exosomes by dendritic cells. Blood. 2004;104:3257–3266. doi: 10.1182/blood-2004-03-0824. [DOI] [PubMed] [Google Scholar]
- Mulcahy L.A., Pink R.C., Carter D.R. Routes and mechanisms of extracellular vesicle uptake. J. Extracell Vesicles. 2014;3 doi: 10.3402/jev.v3.24641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagano M., Toshima J.Y., Siekhaus D.E., Toshima J. Rab5-mediated endosome formation is regulated at the trans-Golgi network. Commun. Biol. 2019;2:419. doi: 10.1038/s42003-019-0670-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nah J., Yuan J., Jung Y.K. Autophagy in neurodegenerative diseases: from mechanism to therapeutic approach. Mol. Cells. 2015;38:381–389. doi: 10.14348/molcells.2015.0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanbo A., Kawanishi E., Yoshida R., Yoshiyama H. Exosomes derived from Epstein-Barr virus-infected cells are internalized via caveola-dependent endocytosis and promote phenotypic modulation in target cells. J. Virol. 2013;87:10334–10347. doi: 10.1128/JVI.01310-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonaka T., Masuda-Suzukake M., Arai T., Hasegawa Y., Akatsu H., Obi T., Yoshida M., Murayama S., Mann D.M., Akiyama H. Prion-like properties of pathological TDP-43 aggregates from diseased brains. Cell Rep. 2013;4:124–134. doi: 10.1016/j.celrep.2013.06.007. [DOI] [PubMed] [Google Scholar]
- Nordstedt C., Caporaso G.L., Thyberg J., Gandy S.E., Greengard P. Identification of the Alzheimer beta/A4 amyloid precursor protein in clathrin-coated vesicles purified from PC12 cells. J. Biol. Chem. 1993;268:608–612. [PubMed] [Google Scholar]
- Ostrowski M., Carmo N.B., Krumeich S., Fanget I., Raposo G., Savina A., Moita C.F., Schauer K., Hume A.N., Freitas R.P. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nat. Cell Biol. 2010;12:19–30. doi: 10.1038/ncb2000. 11-13. [DOI] [PubMed] [Google Scholar]
- Pan B.T., Teng K., Wu C., Adam M., Johnstone R.M. Electron microscopic evidence for externalization of the transferrin receptor in vesicular form in sheep reticulocytes. J. Cell Biol. 1985;101:942–948. doi: 10.1083/jcb.101.3.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardridge W.M. The blood-brain barrier: bottleneck in brain drug development. NeuroRx. 2005;2:3–14. doi: 10.1602/neurorx.2.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parolini I., Federici C., Raggi C., Lugini L., Palleschi S., De Milito A., Coscia C., Iessi E., Logozzi M., Molinari A. Microenvironmental pH is a key factor for exosome traffic in tumor cells. J. Biol. Chem. 2009;284:34211–34222. doi: 10.1074/jbc.M109.041152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastuzyn E.D., Day C.E., Kearns R.B., Kyrke-Smith M., Taibi A.V., McCormick J., Yoder N., Belnap D.M., Erlendsson S., Morado D.R. The neuronal gene arc encodes a repurposed retrotransposon Gag protein that mediates intercellular RNA transfer. Cell. 2018;172:275–288.e18. doi: 10.1016/j.cell.2017.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce M.M.P., Spartz E.J., Hong W., Luo L., Kopito R.R. Prion-like transmission of neuronal huntingtin aggregates to phagocytic glia in the Drosophila brain. Nat. Commun. 2015;6:6768. doi: 10.1038/ncomms7768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Gonzalez R., Gauthier S.A., Kumar A., Levy E. The exosome secretory pathway transports amyloid precursor protein carboxyl-terminal fragments from the cell into the brain extracellular space. J. Biol. Chem. 2012;287:43108–43115. doi: 10.1074/jbc.M112.404467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poehler A.M., Xiang W., Spitzer P., May V.E., Meixner H., Rockenstein E., Chutna O., Outeiro T.F., Winkler J., Masliah E. Autophagy modulates SNCA/alpha-synuclein release, thereby generating a hostile microenvironment. Autophagy. 2014;10:2171–2192. doi: 10.4161/auto.36436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poewe W., Seppi K., Tanner C.M., Halliday G.M., Brundin P., Volkmann J., Schrag A.-E., Lang A.E. Parkinson disease. Nat. Rev. Dis. Primers. 2017;3:17013. doi: 10.1038/nrdp.2017.13. [DOI] [PubMed] [Google Scholar]
- Polanco J.C., Scicluna B.J., Hill A.F., Gotz J. Extracellular vesicles isolated from the brains of rTg4510 mice seed tau protein aggregation in a threshold-dependent manner. J. Biol. Chem. 2016;291:12445–12466. doi: 10.1074/jbc.M115.709485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prada I., Amin L., Furlan R., Legname G., Verderio C., Cojoc D. A new approach to follow a single extracellular vesicle-cell interaction using optical tweezers. Biotechniques. 2016;60:35–41. doi: 10.2144/000114371. [DOI] [PubMed] [Google Scholar]
- Prada I., Gabrielli M., Turola E., Iorio A., D'Arrigo G., Parolisi R., De Luca M., Pacifici M., Bastoni M., Lombardi M. Glia-to-neuron transfer of miRNAs via extracellular vesicles: a new mechanism underlying inflammation-induced synaptic alterations. Acta Neuropathol. 2018;135:529–550. doi: 10.1007/s00401-017-1803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu M., Lin Q., Huang L., Fu Y., Wang L., He S., Fu Y., Yang S., Zhang Z., Zhang L. Dopamine-loaded blood exosomes targeted to brain for better treatment of Parkinson's disease. J. Control Release. 2018;287:156–166. doi: 10.1016/j.jconrel.2018.08.035. [DOI] [PubMed] [Google Scholar]
- Raiborg C., Stenmark H. The ESCRT machinery in endosomal sorting of ubiquitylated membrane proteins. Nature. 2009;458:445–452. doi: 10.1038/nature07961. [DOI] [PubMed] [Google Scholar]
- Rajendran L., Honsho M., Zahn T.R., Keller P., Geiger K.D., Verkade P., Simons K. Alzheimer's disease β-amyloid peptides are released in association with exosomes. Proc. Natl. Acad. Sci. U S A. 2006;103:11172–11177. doi: 10.1073/pnas.0603838103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rind H.B., Butowt R., von Bartheld C.S. Synaptic targeting of retrogradely transported trophic factors in motoneurons: comparison of glial cell line-derived neurotrophic factor, brain-derived neurotrophic factor, and cardiotrophin-1 with tetanus toxin. J. Neurosci. 2005;25:539–549. doi: 10.1523/JNEUROSCI.4322-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roizin L., Nishikawa K., Koizumi J., Keoseian S. The fine structure of the multivesicular body and their relationship to the ultracellular constituents of the central nervous system. J. Neuropathol. Exp. Neurol. 1967;26:223–249. doi: 10.1097/00005072-196704000-00004. [DOI] [PubMed] [Google Scholar]
- Saman S., Kim W., Raya M., Visnick Y., Miro S., Saman S., Jackson B., McKee A.C., Alvarez V.E., Lee N.C. Exosome-associated tau is secreted in tauopathy models and is selectively phosphorylated in cerebrospinal fluid in early Alzheimer disease. J. Biol. Chem. 2012;287:3842–3849. doi: 10.1074/jbc.M111.277061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sardar Sinha M., Ansell-Schultz A., Civitelli L., Hildesjö C., Larsson M., Lannfelt L., Ingelsson M., Hallbeck M. Alzheimer’s disease pathology propagation by exosomes containing toxic amyloid-beta oligomers. Acta Neuropathol. 2018;136:41–56. doi: 10.1007/s00401-018-1868-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt O., Teis D. The ESCRT machinery. Curr. Biol. 2012;22:R116–R120. doi: 10.1016/j.cub.2012.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scolding N.J., Morgan B.P., Houston W.A.J., Linington C., Campbell A.K., Compston D.A.S. Vesicular removal by oligodendrocytes of membrane attack complexes formed by activated complement. Nature. 1989;339:620–622. doi: 10.1038/339620a0. [DOI] [PubMed] [Google Scholar]
- Sekine Y., Lindborg J.A., Strittmatter S.M. A proteolytic C-terminal fragment of Nogo-A (reticulon-4A) is released in exosomes and potently inhibits axon regeneration. J. Biol. Chem. 2020;295:2175–2183. doi: 10.1074/jbc.RA119.009896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano-Pozo A., Frosch M.P., Masliah E., Hyman B.T. Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect. Med. 2011;1:a006189. doi: 10.1101/cshperspect.a006189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma P., Mesci P., Carromeu C., McClatchy D.R., Schiapparelli L., Yates J.R., 3rd, Muotri A.R., Cline H.T. Exosomes regulate neurogenesis and circuit assembly. Proc. Natl. Acad. Sci. U S A. 2019;116:16086–16094. doi: 10.1073/pnas.1902513116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi M., Liu C., Cook T.J., Bullock K.M., Zhao Y., Ginghina C., Li Y., Aro P., Dator R., He C. Plasma exosomal alpha-synuclein is likely CNS-derived and increased in Parkinson's disease. Acta Neuropathol. 2014;128:639–650. doi: 10.1007/s00401-014-1314-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli K.J., Taylor J.K., Osterberg V.R., Churchill M.J., Pollock E., Moore C., Meshul C.K., Unni V.K. Presynaptic alpha-synuclein aggregation in a mouse model of Parkinson's disease. J. Neurosci. 2014;34:2037–2050. doi: 10.1523/JNEUROSCI.2581-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuendl A., Kunadt M., Kruse N., Bartels C., Moebius W., Danzer K.M., Mollenhauer B., Schneider A. Induction of alpha-synuclein aggregate formation by CSF exosomes from patients with Parkinson's disease and dementia with Lewy bodies. Brain. 2016;139:481–494. doi: 10.1093/brain/awv346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuffers S., Sem Wegner C., Stenmark H., Brech A. Multivesicular endosome biogenesis in the absence of ESCRTs. Traffic. 2009;10:925–937. doi: 10.1111/j.1600-0854.2009.00920.x. [DOI] [PubMed] [Google Scholar]
- Svensson K.J., Christianson H.C., Wittrup A., Bourseau-Guilmain E., Lindqvist E., Svensson L.M., Mörgelin M., Belting M. Exosome uptake depends on ERK1/2-heat shock protein 27 signaling and lipid raft-mediated endocytosis negatively regulated by caveolin-1. J. Biol. Chem. 2013;288:17713–17724. doi: 10.1074/jbc.M112.445403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi R.H., Milner T.A., Li F., Nam E.E., Edgar M.A., Yamaguchi H., Beal M.F., Xu H., Greengard P., Gouras G.K. Intraneuronal Alzheimer abeta42 accumulates in multivesicular bodies and is associated with synaptic pathology. Am. J. Pathol. 2002;161:1869–1879. doi: 10.1016/s0002-9440(10)64463-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamboli I.Y., Barth E., Christian L., Siepmann M., Kumar S., Singh S., Tolksdorf K., Heneka M.T., Lutjohann D., Wunderlich P. Statins promote the degradation of extracellular amyloid {beta}-peptide by microglia via stimulation of exosome-associated insulin-degrading enzyme (IDE) secretion. J. Biol. Chem. 2010;285:37405–37414. doi: 10.1074/jbc.M110.149468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trajkovic K., Hsu C., Chiantia S., Rajendran L., Wenzel D., Wieland F., Schwille P., Brugger B., Simons M. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science. 2008;319:1244–1247. doi: 10.1126/science.1153124. [DOI] [PubMed] [Google Scholar]
- Trams E.G., Lauter C.J., Salem N., Jr., Heine U. Exfoliation of membrane ecto-enzymes in the form of micro-vesicles. Biochim. Biophys. Acta. 1981;645:63–70. doi: 10.1016/0005-2736(81)90512-5. [DOI] [PubMed] [Google Scholar]
- Tsai Y.W., Sung H.H., Li J.C., Yeh C.Y., Chen P.Y., Cheng Y.J., Chen C.H., Tsai Y.C., Chien C.T. Glia-derived exosomal miR-274 targets Sprouty in trachea and synaptic boutons to modulate growth and responses to hypoxia. Proc. Natl. Acad. Sci. U S A. 2019;116:24651–24661. doi: 10.1073/pnas.1902537116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valadi H., Ekström K., Bossios A., Sjöstrand M., Lee J.J., Lötvall J.O. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- Valenzuela C.F., Puglia M.P., Zucca S. Focus on: neurotransmitter systems. Alcohol Res. Health. 2011;34:106–120. [PMC free article] [PubMed] [Google Scholar]
- van den Heuvel M., Nusse R., Johnston P., Lawrence P.A. Distribution of the wingless gene product in Drosophila embryos: a protein involved in cell-cell communication. Cell. 1989;59:739–749. doi: 10.1016/0092-8674(89)90020-2. [DOI] [PubMed] [Google Scholar]
- van Niel G., D'Angelo G., Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat. Rev. Mol. Cell Biol. 2018;19:213–228. doi: 10.1038/nrm.2017.125. [DOI] [PubMed] [Google Scholar]
- Vassar R., Bennett B.D., Babu-Khan S., Kahn S., Mendiaz E.A., Denis P., Teplow D.B., Ross S., Amarante P., Loeloff R. Beta-secretase cleavage of Alzheimer's amyloid precursor protein by the transmembrane aspartic protease BACE. Science. 1999;286:735–741. doi: 10.1126/science.286.5440.735. [DOI] [PubMed] [Google Scholar]
- Vella L.J., Hill A.F., Cheng L. Focus on extracellular vesicles: exosomes and their role in protein trafficking and biomarker potential in alzheimer's and Parkinson's disease. Int. J. Mol. Sci. 2016;17:173. doi: 10.3390/ijms17020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verderio C., Muzio L., Turola E., Bergami A., Novellino L., Ruffini F., Riganti L., Corradini I., Francolini M., Garzetti L. Myeloid microvesicles are a marker and therapeutic target for neuroinflammation. Ann. Neurol. 2012;72:610–624. doi: 10.1002/ana.23627. [DOI] [PubMed] [Google Scholar]
- von Bartheld C.S., Byers M.R., Williams R., Bothwell M. Anterograde transport of neurotrophins and axodendritic transfer in the developing visual system. Nature. 1996;379:830–833. doi: 10.1038/379830a0. [DOI] [PubMed] [Google Scholar]
- Votteler J., Sundquist W.I. Virus budding and the ESCRT pathway. Cell Host Microbe. 2013;14:232–241. doi: 10.1016/j.chom.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Cesca F., Loers G., Schweizer M., Buck F., Benfenati F., Schachner M., Kleene R. Synapsin I is an oligomannose-carrying glycoprotein, acts as an oligomannose-binding lectin, and promotes neurite outgrowth and neuronal survival when released via glia-derived exosomes. J. Neurosci. 2011;31:7275–7290. doi: 10.1523/JNEUROSCI.6476-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Balaji V., Kaniyappan S., Kruger L., Irsen S., Tepper K., Chandupatla R., Maetzler W., Schneider A., Mandelkow E. The release and trans-synaptic transmission of Tau via exosomes. Mol. Neurodegener. 2017;12:5. doi: 10.1186/s13024-016-0143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe D.M., Lee J.H., Kumar A., Lee S., Orenstein S.J., Nixon R.A. Autophagy failure in Alzheimer's disease and the role of defective lysosomal acidification. Eur. J. Neurosci. 2013;37:1949–1961. doi: 10.1111/ejn.12169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong Y., Mahmood A., Chopp M. Emerging potential of exosomes for treatment of traumatic brain injury. Neural Regen. Res. 2017;12:19–22. doi: 10.4103/1673-5374.198966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Boza-Serrano A., Dunning C.J.R., Clausen B.H., Lambertsen K.L., Deierborg T. Inflammation leads to distinct populations of extracellular vesicles from microglia. J. Neuroinflammation. 2018;15:168. doi: 10.1186/s12974-018-1204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You Y., Borgmann K., Edara V.V., Stacy S., Ghorpade A., Ikezu T. Activated human astrocyte-derived extracellular vesicles modulate neuronal uptake, differentiation and firing. J. Extracellular Vesicles. 2020;9:1706801. doi: 10.1080/20013078.2019.1706801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan D., Zhao Y., Banks W.A., Bullock K.M., Haney M., Batrakova E., Kabanov A.V. Macrophage exosomes as natural nanocarriers for protein delivery to inflamed brain. Biomaterials. 2017;142:1–12. doi: 10.1016/j.biomaterials.2017.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuyama K., Sun H., Mitsutake S., Igarashi Y. Sphingolipid-modulated exosome secretion promotes clearance of amyloid-beta by microglia. J. Biol. Chem. 2012;287:10977–10989. doi: 10.1074/jbc.M111.324616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang G., Yang P. A novel cell-cell communication mechanism in the nervous system: exosomes. J. Neurosci. Res. 2018;96:45–52. doi: 10.1002/jnr.24113. [DOI] [PubMed] [Google Scholar]
- Zhao Y., Haney M.J., Gupta R., Bohnsack J.P., He Z., Kabanov A.V., Batrakova E.V. GDNF-transfected macrophages produce potent neuroprotective effects in Parkinson's disease mouse model. PLoS One. 2014;9:e106867. doi: 10.1371/journal.pone.0106867. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Zheng M., Huang M., Ma X., Chen H., Gao X. Harnessing exosomes for the development of brain drug delivery systems. Bioconjug. Chem. 2019;30:994–1005. doi: 10.1021/acs.bioconjchem.9b00085. [DOI] [PubMed] [Google Scholar]
- Zlokovic B.V. The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron. 2008;57:178–201. doi: 10.1016/j.neuron.2008.01.003. [DOI] [PubMed] [Google Scholar]




