Abstract
Objective
Provide an update on minimal invasive surgery (MIS) techniques for surgical management of pediatric spine.
Methods
Minimal Invasive surgery for pediatric spine deformity has evolved significantly over the past decade. We include updated information about the surgical management of patients with adolescent idiopathic and Early Onset Scoliosis through MIS techniques. We take into consideration the implementation of this technique in Low-to-Middle Income Countries (LMICs).
Results
Although MIS began as a technique in adult and degenerative spine, recent publications on MIS in pediatric spine cases report benefits of decreased blood loss and infection incidence, and cosmetic advantages from fewer incision numbers. Adoption of MIS techniques in pediatric spine can be facilitated with pre- and intraoperative use of pertinent medical systems.
Conclusion
With appropriate considerations and training, MIS is a safe procedure for pediatric spine correction surgery and can be applicable in LMICs.
Keywords: Minimal invasive surgery, Adolescent idiopathic scoliosis, Early onset scoliosis
1. Introduction
Early Onset Scoliosis (EOS) is a pediatric spine deformity that includes all children below 10 years of age regardless of etiology,1 according to the Scoliosis Research Society (SRS), pediatric orthopedic Society of North America (POSNA), Growing Spine Study Group (GSSG) definition. The adolescent type is called Adolescent Idiopathic Scoliosis (AIS) with an age range of 10–16 years2 and is the most common type of pediatric spine deformities.
From the early 1960s, surgery became the golden standard of management for progressive adolescent idiopathic spine deformity, and open posterior spinal fusion is now considered the popular procedure for these cases. With regard to EOS, however, the treatment concept changed from fusion and instrumentation to spine growth preservation techniques to allow for maximum thoracic cavity and lung growth.3 In recent years, there has been a shift to MIS for degenerative spine disorders including scoliosis.4,5 The MIS technique have shown advantages in reducing blood loss, decreasing infection incidence, reducing hospital stays, and shortening rehabilitation.6
Trials for implementing the MIS technique for pediatric spine deformity began slowly only in the last decade due to the associated technical challenges related to pediatric spine deformity. Challenges toward implementing MIS in pediatric spine deformity include the instrumentation of more levels, difficulty in inserting screws due to rotation of the vertebrae, and limitation of access to the field. This makes facetectomy and fusion as a primary procedure more challenging. Furthermore, increased radiation exposure from putting multiple levels of pedicular screws under fluoroscopy control would add significant risk to children.
With the surgeon’s acknowledgment of the associated complications, MIS can be applied to avoid the complications related to the open technique. Mastering the MIS technique for these children would make this procedure safer. Despite the literature on MIS for pediatric spine deformity being limited and in small subset of patients, the results are promising. This article discusses updates in MIS for pediatric spine deformity.
2. Adolescent idiopathic scoliosis and MIS
2.1. Muscle sparing or Wiltse approach
This approach is an old technique, mainly for muscle sparing with decreased blood loss. It approaches the lumbar facet joints through blunt dissection between the medial multifidus and lateral longissimus muscles, providing access to pedicular screws during scoliosis correction, and is considered MIS for AIS surgeries.7 A retrospective study by Street et al. comparing the results of 385 patients done with midline surgical approach and Wiltse approach found that the latter has advantages in reducing the incidence of infection, blood loss, and adjacent segment failure than the midline approach.8
2.2. MIS with 3 small incisions
This is a surgical technique done for correction of adolescent idiopathic scoliosis with 3 incisions, as opposed to the standard open Posterior Spinal Fusion technique (Fig. 1) Vishai Sarwahi et al. suggested this MIS technique to be done for patients with major curve cobb angle <70° and flexibility >50% on side bending films.9 It includes 3 small midline incisions, usually about 5 cm each. Two to three levels are instrumented per incision with 1–2 intervening segments between instrumented vertebraes. At each level, a stab wound is done one cm or one fingerbreadth lateral to the spinous process, bluntly separate the muscle to reach the facet joint.
Fig. 1.
3 incisions were done for scoliosis correction.
In this technique, facetectomy is done under direct vision followed by pedicle screw insertion with the freehand technique, and is an important step the surgeon should be aware of since it is the main arthrodesis procedure. Some surgeons are more attached to the minimal or less invasive surgery techniques that distract them from the main point of fusion and from the necessity to perform facetectomy at every level exposed by the surgeon. Underestimating this step would increase instability of the screws and would increase the incidence of screws dislodgment and or rod breakage.
Some surgeons prefer to use the sequential retractors and tubular dilators to put the screws, avoiding excessive soft tissue distractions and the possibility of excessive angulation of the screwdriver with severe deformity. However, this is not always available for many centers in limited resources areas. In the authors’ experience in limited resource countries, they put most of the screws without using the tubes by angulating the table in a way that will get the appropriate angle without difficulty to put the screw, especially on the concave side. The procedure is done on both sides according to the preoperative plan. Rods are pre-contoured to correct the sagittal profile. The rods are placed from distal to proximal going under the soft tissue and the skin bridges to fit the screw tabs, or seated within the tulips of the pedicle screw. All standard procedures for correction, including rod de-rotation, compression, distraction, and in-situ bending are to be performed.7,9 (Fig. 2).
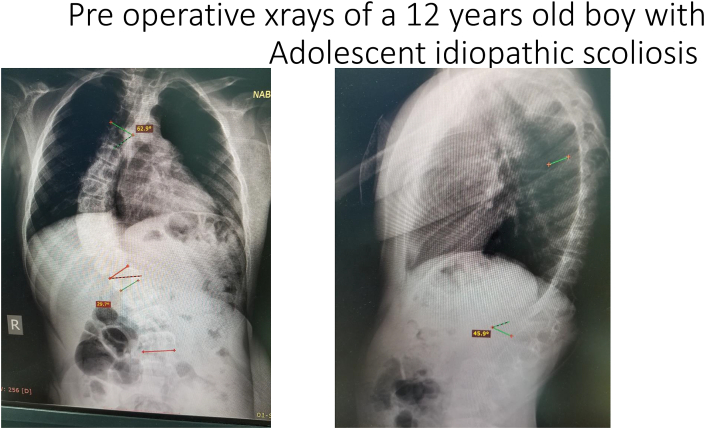
Fig. 2a.
Pre operative x rays of a 12 years old boy with Adolescent idiopathic scoliosis.
Fig. 2b.
Post operative x ray with clear correction of the scoliosis correction of the deformity coronal and sagittal.
Advantages of MIS over the traditional posterior spine instrumentation are mainly related to intraoperative blood loss, reduced hospital stays, and lower infection rate. However, traditional spine posterior fusion can have better curve correction, less operative time, and lower post-operative complications.10
Though the data related to outcomes of the MIS9 had similar deformity correction, screw placement accuracy, and fusion status when compared with the PSF group, it had lower blood transfusion rate, shorter fusion, and fewer pedicle screws. MIS shows real potential in the short term over traditional open posterior instrumentation (Fig. 3).
Fig. 3.
Pre and post operative with good correction and compensation with less invasive technique.
There remains a need to have longer term prospective studies, focusing on fusion rates, and this is a main goal in AIS surgical management.
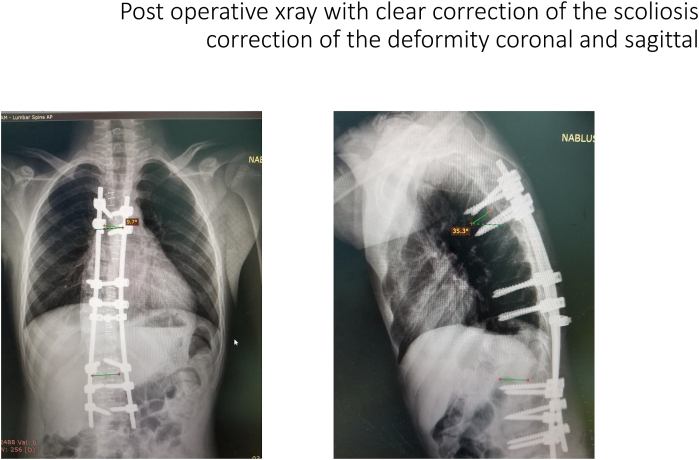
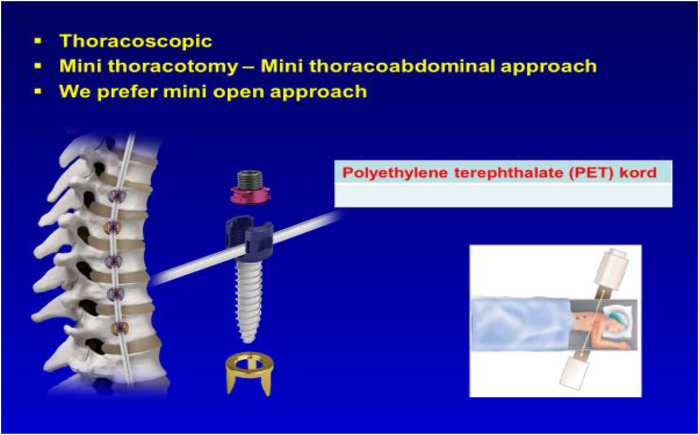
2.3. Minimal invasive technique by anterior fusion and instrumentation
Open Anterior Spinal Fusion and Instrumentation has been one of the traditional methods for correction of AIS. With the dissemination of the MIS, a mini open thoracotomy approach is used for anterior fusion and instrumentation in AIS (Fig. 4). The procedure is done with the patient lying on their side with the convex part up. A lateral 8 cm skin incision is made on the rib most proximal to the vertebrae to be instrumented, with not more than 5 vertebrates to be instrumented with the same incision (Fig. 5). The remainder of the surgical procedure for exposing the spine, correcting the deformity, and putting the screws with the rod is the same as the traditional open technique11 (Fig. 6).
Fig. 4.
Mini thoracotomy for anterior instrumentation with Permission from Professor Azmi HamzaOglu.
Fig. 5.
Minimal incisions for anterior instrumentation in AISwith Permission from Professor Azmi HamzaOglu.
Fig. 6.
Putting screws in the same way as open technique with Permission from Professor Azmi HamzaOglu.
With the ongoing interest in MIS, there is growing interest in thoracoscopic anterior instrumentation and fusion. This surgical technique is done with the patient in the decubitus position with the convex side up. Access to the spine is done with thoracoscopic technique through 4–6 portals of entry. Discectomy is performed before screw instrumentation with 4.5 rod put, with correction done through cantilever effect and compression.12
There is some worry about pulmonary function post-operatively with the anterior procedure. However, recent studies show that while the vital capacity decreases 28% within the first 3 weeks postoperatively, it returns to normal with the last follow up.13 Other pulmonary complications with this procedure include hemothorax, pneumothorax, and atelectasis. Implant related and vascular complications are also detected.13
The advantages of this technique relate mainly cosmetic wound, fewer instrumented levels, and less time staying in the intensive care unit.14 However, this comes at the cost of longer operative time and perioperative pulmonary complications. In addition, since this MIS process is technically challenging, it needs to be performed with highly trained surgeons, limited to smaller curves, or with an adjunct to posterior fusion and instrumentation in larger curves.
3. MIS in early onset scoliosis patients
EOS includes all spinal deformities in children below 10 years of age regardless of etiology (1), according to the Scoliosis Research Society (SRS), pediatric orthopedic Society of North America (POSNA), Growing Spine Study Group (GSSG) definition. EOS can be etiologically classified as idiopathic (infantile and juvenile), neuromuscular, syndromic, or congenital. On the contrary to AIS management, the treatment of EOS may be a life-saving measure. A past belief that straight and short spine is better than a long and deformed one led to spine fusion with maximum correction as the main surgical management.15 However, after realizing the morbidity of early spine fusion due to lung growth restriction, treatment concept changed to spine growth preservation techniques like Traditional growing rods, Mathe genetically Controlled growing rods, allowing for maximum thoracic cavity and lung growth.3
MIS is not popular in EOS, even in comparison with AIS. This is mainly due to the heterogenicity, difficulty of the cases, small pedicles, osteoporotic bone, severely deformed vertebrae and their pedicles, and the need to go every 6 months for distraction. The pulmonary insufficiency is also a major factor restricting anterior endoscopic approach for these patients, except for juvenile idiopathic ones.
The literature discussing MIS techniques in EOS is limited. However, there is potential for applying MIS in early onset scoliosis cases with a minimal anterior and posterior approach, including through the anterior vertebral tethering technique for juvenile idiopathic scoliosis through a mini incision or thoracoscopic technique. This technique is used for children who have juvenile idiopathic scoliosis with curves between 35 and 60° and 50% of flexibility.16 The main concept it uses is tethering through anterior approach with pedicular screws and a flexible polypropylene tethering band. The hypothesis is that modulation of the vertebra will happen because of the tethering of the convex side, maintaining the disc viability, unlike the vertebral body stapling.
This technique began with a case report published in 201017 with an 8 year old boy who has juvenile idiopathic scoliosis. Although it was done by mini thoracotomy, it involved the same principle of putting pedicular screws on the convex side anteriorly at the midpoint of the body just anterior to the rib heads, securing the tethering band on the screws’ heads, and applying compression of the screws.
Good results were reported, with a 4 year follow up with a modulation of the 6 tethered vertebrae and 1.4° correction/level/year. Additional articles were later published with the same tethering principle, but with the use of the thoracoscopic technique. All published papers were confined to juvenile idiopathic type of EOS cases. The results indicated that this procedure is a safe and effective option in the treatment of the growing spine17 (Fig. 7).
Fig. 7.
Efficiency of anterior tethering in Juvenile idiopathic scoliosis with Permission from Professor Azmi HamzaOglu.
Although this technique demands a high skill level, it has cosmetic advantages and includes limited incisions leading to less intraoperative bleeding and reduced infection rate. The contraindications for using this technique are severe curvature more than 60°, non-flexible curve, pulmonary insufficiency associated with the scoliosis, kyphosis more than 40°, and neuromuscular, syndromic, and congenital scoliosis. This surgical technique shares many similarities with the previously discussed thoracoscopic anterior fusion, but without fusion and replacing the rod with the polypropylene band.16
3.1. Minimal invasive technique with 2 incisions through a posterior approach
This category of MIS includes performing 2 incisions instead of doing one big incision for EOS cases. Reports in the literature18 on myelomeningocele associated with severe kyphosis show that it avoids the scarred tissue from previous surgery of the myelomeningocele, through having proximal incision to put proximal anchors and distal incisions in the iliac areas to put iliac screws.
The rod is put sub facially or subcutaneously through a chest tube to add safety to the procedure from proximal to distal and avoid pathological skin. This procedure can be done in other EOS cases than the myelomeningocele and would decrease the intraoperative bleeding incidence, decrease infection incidence, and provide cosmetically enhanced results.
3.2. Percutaneous pedicle screw fixation
This technique is well known for degenerative and spine trauma, but it is not popular for scoliosis surgery due to the need for long instrumentations that require many small incisions, even though the straight midline incision is cosmetically better.
The way that percutaneous screw fixation as a MIS technique is to be used is with limited levels, good awareness to the deformity in the vertebrae, and preoperative appropriate pedicles assessment. This is even more mandatory in EOS, considering the age of the patient, the deformity, and bone weakness.
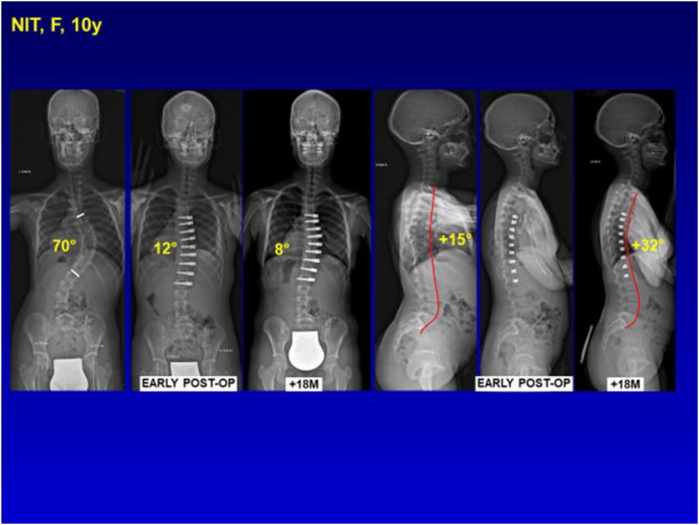
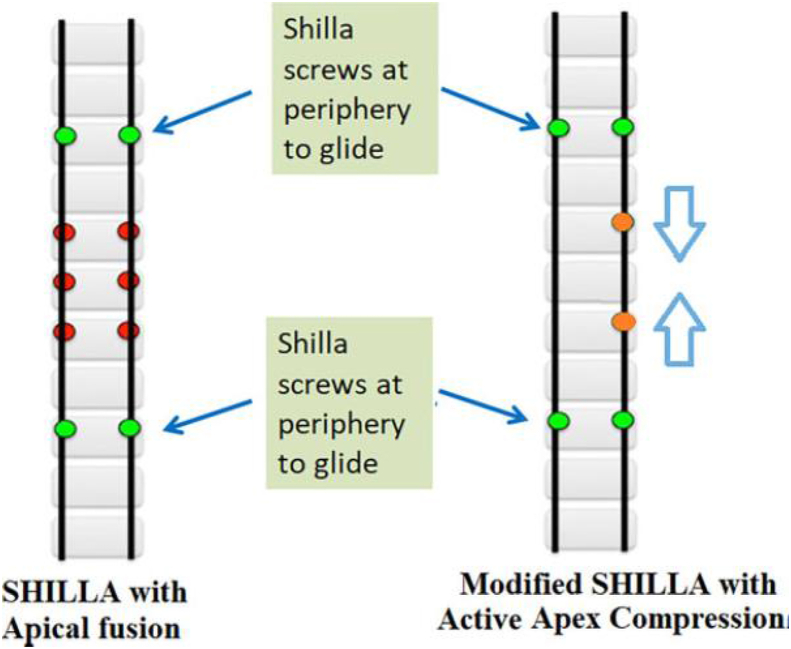
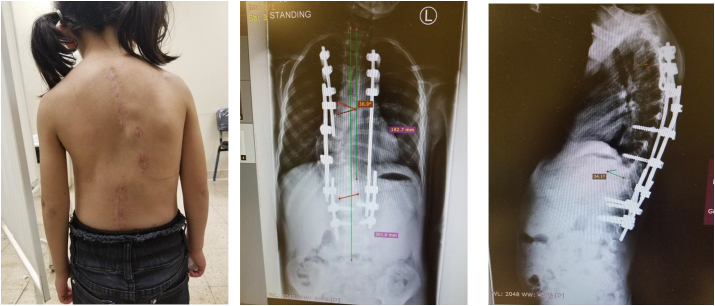
The author is accomplished in performing surgeries for EOS with the Active Apex Correction (APC) technique that includes tethering of the convex part of the apex through putting 2 screws above and below the most wedged vertebrae. The APC surgical procedure is a modified version of SHILLA (Fig. 8), using either the rod to SHILLA screws (Medtronic, MN, USA) with a sliding mechanism or the analogous rod to domino (4.5 or 5.5 mm rod in 5.5 mm domino hole) sliding mechanism.19
Fig. 8.
With the difference in concept between the SHILLA and APC.
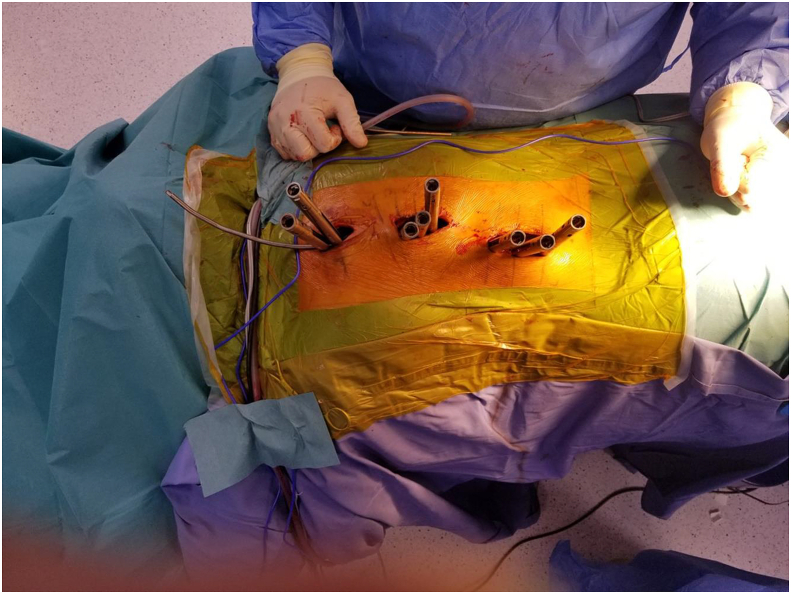
In recent studies by the author these 2 screws are put percutaneously and connected with a small 5.5 rod for tethering to decrease the tissue damage and the fusion incidence in the apex, hence promoting the modulation process (Fig. 9, Fig. 10). In this modified technique, the most wedged vertebra are selected, followed by the insertion of pedicle screws percutaneously in the convex side above and below the wedged vertebrae. No screws are placed on the concave side of the apex. The rod 5.5 is put subfascial connecting the 2 screws with compression of the screws on the convex side.19 The tethered rod is connected proximally and distally with rods through dominos, with sliding of the proximal and distal rods to avoid the 6 months lengthening surgeries. All surgeries are performed under an intraoperative neuromonitor and a C-arm. Additionally, no cast or brace is used for these patients postoperatively.
Fig. 9.
Years old female with early onset scoliosis increased despite brace treatment.
Fig. 10.
With correction of the deformity with APC technique with the arrows showing the percutaneous screws site in the Apex.
4. Discussion
Surgical management with minimal invasive surgery (MIS) techniques in the spine is well known and has become increasingly popular over the past two decades. However, most of the MIS in spine cases are related to degenerative spine problems and disc hernia, with the technique less popular in pediatric spine deformity surgeries due to instrumentation being mostly around 10 levels. The instrumentation levels make it very hard and not realistic to perform the surgery with the MIS technique without many short wounds needed on both sides (mostly around 20 stab wound), and so it is better to have 3 small midline noncontiguous incisions to give better cosmetic results for the patients. Additionally, the deformity of the pedicles and the rotation of the vertebrae make it harder and less safe to put the screws percutaneously.
The golden standard of scoliosis surgery used to be a posterior approach with instrumentation and fusion for AIS and non-fusion for EOS. Nonetheless, in the last decade, trials began to correct scoliosis with less invasive techniques through anterior and posterior approaches. Scoliosis correction in children with spine deformity with MIS technique through anterior approach became possible with the evolution of the thoracoscopic techniques. This includes both the fusion and non-fusion techniques.
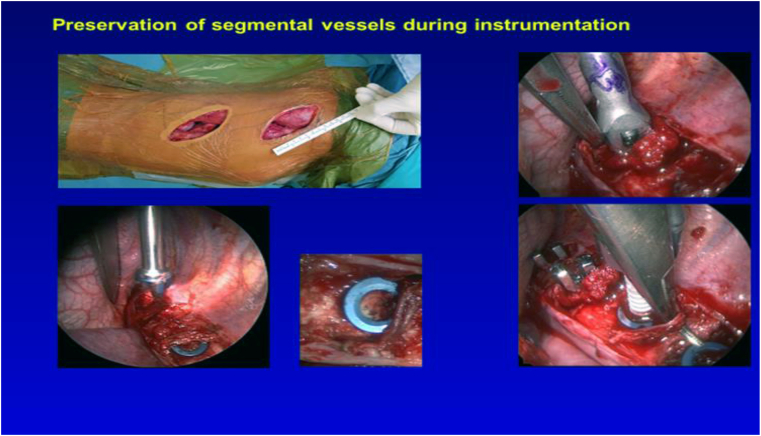
Gradually, there has been a paradigm shift from the subperiosteal resection and excessive muscle retraction to soft tissue dilatation using the sequential dilators and tubular retractors (Fig. 11). This improves the MIS techniques in spine surgery through a posterior approach.20 In addition, the involvement of the 3D radiology machines and the O arm in the operating room have increased the safety in putting screws percutaneously in deformed pedicles. This technology has opened the door to more involvement in the MIS techniques in scoliosis through the posterior approach.
Fig. 11.
The use of tubular dilators during less invasive technique in AIS.
Despite the scarcity of the published papers about the surgical minimal invasive techniques in pediatric spine deformity, there are clear advantages related to the reduced blood loss, infection rate, and easiness with mastering this technique.
3 studies compared the safety and efficacy of minimally invasive surgery (MIS) for the surgical management of adolescent idiopathic scoliosis (AIS) to the standard open posterior approach (PSF) (Table 1).
Table 1.
Comparison of outcomes between MIS and Open posterior fusion in AIS surgery in 3 studies.
| Vishal Sarwahi et al. |
Firoz Miyanji et al. |
Wiktor Urbanski et al. |
||||
|---|---|---|---|---|---|---|
| MIS | Open | MIS | Open | MIS | Open | |
| Percent major Curve Correction | 79% | 85% | 63% | 68% | 68% | 78% |
| Thoracic kyphosis (degrees) | 24 | 21 | 21 | 17 | 26 | 32 |
| EBL (ml) | 600 | 800 | 277 | 388 | 138 | 450 |
| Length of surgery (hours) | 9 | 7 | 7.4 | 5.8 | 4.8 | 4.00 |
| LOS (days) | 8 | 7 | 4.6 | 6.2 | 3.8 | 7.00 |
Retrospective controlled study done by Vishal Sarwahi et al.9 compared the results of MIS with open posterior fusion.
For surgical deformity correction the difference between MIS and open posterior fusion in correction of scoliosis or kyphosis and screw displacement was no statistically significant, but there were less instrumented levels and less screws in MIS that were statistically significant (0.046, 0.015 respectively).
For the perioperative results, estimated blood loss was more in open technique than MIS (800 cc, 600 cc respectively), with nearly half of the open fusion needed postoperative blood transfusion with no MIS patients needed post-operative transfusion, but the anesthesia and surgery time was less than MIS that was statistically significant.
Complications in general were higher in open posterior fusion than MIS (86%, 71% respectively) with no statistical significance.
In Wiktor Urbanski et al. study, results of AIS Lenke 5 correction with MIS,21 good correction of the scoliosis (68%, p < 0.001), estimated blood loss was 138 ml, with 4.8 h operative time.
Firoz Miyanji et al. study,22 results were similar to previous 2 results with Post-op major Cobb 63% correction in those treated with MIS and 68% in those treated with open surgery. Both estimated blood loss and length of stay (LOS) were significantly less in the MIS group (277 mL, 4.63 days) compared to the open group (388 mL, 6.19 days); however OR time was significantly longer in the MIS group (444 min) compared to the open group (350 min).
MIS is still a relatively new technique and that makes it technically demanding, but an appropriate assessment of the vertebral body and pedicles preoperatively through a 3D CT scan and the increased use of the 3D intraoperative radiation machines will facilitate the adoption of this technique in the future.
Begin with the most popular approach for scoliosis surgery. It is followed by performing less invasive techniques such as the three small incisions for AIS, then putting screws percutaneously in short small curve beginning on the convex side like with the APC technique discussed. The technique relies on good C arm image intensifier and sliding the bed to overcome the difficulty of putting the screws without having the tubes or navigation.
For anterior approach in LMICs, the surgeon can do the MIS with small incisions, whether for thoracic or lumbar curves, instead of thoracoscopic technique, which might not be available.
Additional retrospective data from different experiences in MIS for pediatric spine deformity correction and longer follow up through multicenter studies could make the MIS technique become the standard in developed countries. In developing countries, more participation from the local surgeons will be needed to make MIS for pediatric spine correction the standard surgical technique and to overcome the lack of technology in their hospitals.
5. Conclusion
MIS for spine deformity should achieve results comparable to open surgeries. Major goals of MIS for spine deformity include appropriate coronal and sagittal deformity correction through minimal soft tissue disruption, minimal blood loss, maximal fusion for fusion surgeries, and return to normal activities sooner comparable to open surgeries.
The MIS techniques are spreading in use by the scoliosis surgeons who are now familiar with the new sets of instruments, such as those working in a restricted space through expandable tubular tools, putting pedicular screws percutaneously, through endoscopic surgery or with the help of the chest endoscopic surgeon. In addition, new image guidance tools like intraoperative navigation and CT guided imaging have increased the safety and accuracy of putting the pedicular screws in scoliosis surgery in severely deformed and rotated vertebrae.
Publications about complications in MIS for pediatric spine deformity and life quality are scarce in comparison to the MIS in adult spine surgery, but there is more evidence that complications are 50% less with MIS in comparison with open surgery.23
Less ideal technology within the context in LMICs would give a wrong assumption that MIS for pediatric spine deformity is more difficult to implement in these resource poor regions. On the contrary, MIS has a great potential to develop in LMICs, considering the decreased rate of complications that would remove a big burden on the weak health systems.
References
- 1.El-Hawary R., Akbarnia B.A. Early onset scoliosis - time for consensus. Spine Deformity. 2015;3(2):105–106. doi: 10.1016/j.jspd.2015.01.003. Mar. [DOI] [PubMed] [Google Scholar]
- 2.Reamy Brian V., Joseph B. SLAKEY- adolescent idiopathic scoliosis:review and current concepts. Am Fam Physician. 2001;64:111–116. [PubMed] [Google Scholar]
- 3.Hell A.K., Campbell R.M., Hefti F. The vertical expandable prosthetic titanium rib implant for the treatment of thoracic insufficiency syndrome associated with congenital and neuromuscular scoliosis in young children. J Pediatr Orthop B. 2005;14:287e293. doi: 10.1097/01202412-200507000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Anand N., Baron E.M., Thaiyananthan G. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech. 2008;21:459–467. doi: 10.1097/BSD.0b013e318167b06b. [DOI] [PubMed] [Google Scholar]
- 5.Anand N., Rosemann R., Khalsa B. Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus. 2010;28:E6–E13. doi: 10.3171/2010.1.FOCUS09272. [DOI] [PubMed] [Google Scholar]
- 6.Wang M.Y., Mummaneni P.V. Minimally invasive surgery for thoracolumbar spinal deformity: initial experience with clinical and radiographic outcomes. Neurosurg Focus. 2010;28:E9–E16. doi: 10.3171/2010.1.FOCUS09286. [DOI] [PubMed] [Google Scholar]
- 7.Guiroy A., Surgical Neurology International . 2018. 9:38 How to perform the Wiltse posterolateral spinal approach. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Street J., Glennie A., Dea N. A comparison of the Wiltse versus midline approaches in degenerative conditions of the lumbar spine. J Neurosurg Spine. 2016;25:332–338. doi: 10.3171/2016.2.SPINE151018. [DOI] [PubMed] [Google Scholar]
- 9.Sarwahi Vishal, Jonathan J., Horn B.S., Preethi M., Kulkarni M.D. Minimally invasive surgery in patients with adolescent idiopathic scoliosis is it better than the standard approach? A 2-year follow-up study. Clin Spine Surg. 2016;29(Number 8) doi: 10.1097/BSD.0000000000000106. October. [DOI] [PubMed] [Google Scholar]
- 10.Firoz Miyanji M.D., Desai Sameer. BScb. Minimally invasive surgical options for adolescent idiopathic scoliosis. Semin Spine Surg. 2015;2(7) 3 9 – 4 4. [Google Scholar]
- 11.Qiu Yong, Zhu Feng, Wang Bin. Mini-open anterior instrumentation with diaphragm sparing for thoracolumbar idiopathic scoliosis: its technique and clinical results. Eur Spine J. 2011;20:266–273. doi: 10.1007/s00586-010-1654-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Padhye Kedar, Soroceanu Alexandra, Russell David. Thoracoscopic anterior instrumentation and fusion as a treatment for adolescent idiopathic scoliosis: a systematic review of the literature. Spine Deformity. 2018;6:384–390. doi: 10.1016/j.jspd.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 13.Lonner B.S., Scharf C., Antonacci D. The learning curve associated with thoracoscopic spinal instrumentation. Spine. 2005;30:2835–2840. doi: 10.1097/01.brs.0000192241.29644.6e. [DOI] [PubMed] [Google Scholar]
- 14.Perez-Caballero M.C., Burgos Flores J., Martos Sanchez I. Early postoperative complications of thoracoscopy versus thoracotomy in pediatric idiopathic scoliosis. An Pediatr. 2006;65:569–572. doi: 10.1157/13095850. [DOI] [PubMed] [Google Scholar]
- 15.Winter R.B., Moe J.H. The results of spinal arthrodesis for congenital spinal deformity in patients younger than five years old. J Bone Joint Surg Am. 1982;64:419–432. [PubMed] [Google Scholar]
- 16.Samdani Amer F., Ames Robert J., Kimball Jeff S. Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J. 2015;24:1533–1539. doi: 10.1007/s00586-014-3706-z. [DOI] [PubMed] [Google Scholar]
- 17.Crawford C.H., 3rd, Lenke L.G. Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: a case report. J Bone Joint Surg Am. 2010;92(1):202–209. doi: 10.2106/JBJS.H.01728. [DOI] [PubMed] [Google Scholar]
- 18.Alaaeldin A. Ahmad Treatment of spinal deformity associated with myelomeningocele in young children with the use of the four-rib construct. J Pediatr Orthop B. 2013;22(6):595–601. doi: 10.1097/BPB.0b013e3283633150. Nov. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal Aakash, Aker Loai, Ahmad Alaaeldin Azmi. Active apex correction with guided growth technique for controlling spinal deformity in growing children: a modified SHILLA technique. Global Spine J. 2019 doi: 10.1177/2192568219859836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kulkarni Arvind Gopalrao, Patel Ravish Shammi, Dutta Shumayou. Asian Spine J. 2016;10(6):1000–1006. doi: 10.4184/asj.2016.10.6.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Urbanski Wiktor, Zaluski Rafał, Kokaveshi Anis. Minimal invasive posterior correction of Lenke 5C idiopathic scoliosis: comparative analysis of minimal invasive vs. open surgery. Arch Orthop Trauma Surg. 2019;139:1203–1208. doi: 10.1007/s00402-019-03166-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miyanji Firoz, Samdani Amer, Ghag Arvindera. Minimally invasive surgery for AIS: an early prospective comparison with standard open posterior surgery. J Spine. 2013;S5 [Google Scholar]
- 23.Wang M.Y., editor. Minimally Invasive Spinal Deformity Surgery. © Springer-Verlag Wien; 2014. p. 393. [DOI] [Google Scholar]