Abstract
Sacropelvic is a complex junctional area owing to the complex regional anatomy and higher biomechanical stress. However extension of construct is indicated in cases with complex deformities, high grade spondylolisthesis, and complex fractures. The challenges remain which includes pseudoarthrosis and fixation failures. The fixation techniques have constantly evolved over time with better results with iliac screws and S2-alar-iliac screws. This article gives background on evolution, biomechanics, and recent update of use of robotics for sacropelvic fixation.
Keywords: Sacropelvic, Robotics, S2AI, Deformity, Fixation, Pelvic
1. Introduction
The uniqueness of lumbosacral junction with its complexity has led to a continuous stride in the evolution of management strategies for pathologies involving fixation in and around the junctional area. The big challenge is the complex anatomy, and higher amounts of biomechanical forces acting at this junctional area. The distal lumbosacral articulation is composed of steeply angled discs,1 most mobile segment in the sagittal axis, and least mobile in coronal axis.2The cumulative forces acting in this area create highest transitional forces in the spine.3,4 In addition, the bone density of sacrum is low which adds to the cumulative factors causing higher rates of non union and instrumentation failure at this segment.5
Nonetheless the area is explored for various indications to maintain sagittal, coronal balance, stronger construct and to achieve solid fusion. To overcome this, surgeons’ have been trying to devise new methods to add to their armamentarium aimed at reducing these complications with better fusion rates and clinical results. This review aims to update and outline the different available modalities with advantages and disadvantages of each.
2. Anatomy and biomechanics
It is of paramount importance to understand the relevant anatomy of the sacropelvic junction prior to performing any procedures in this area. The fifth lumbar vertebra articulates with the sacrum. The sacrum is a constitution of 5 vertebrae, the transverse processes of which form the sacral alae. The anterior division of the four sacral nerves exit from the sacral neural foramina.6 The sacroiliac joints transmit all the forces from spine to the lower extremities.
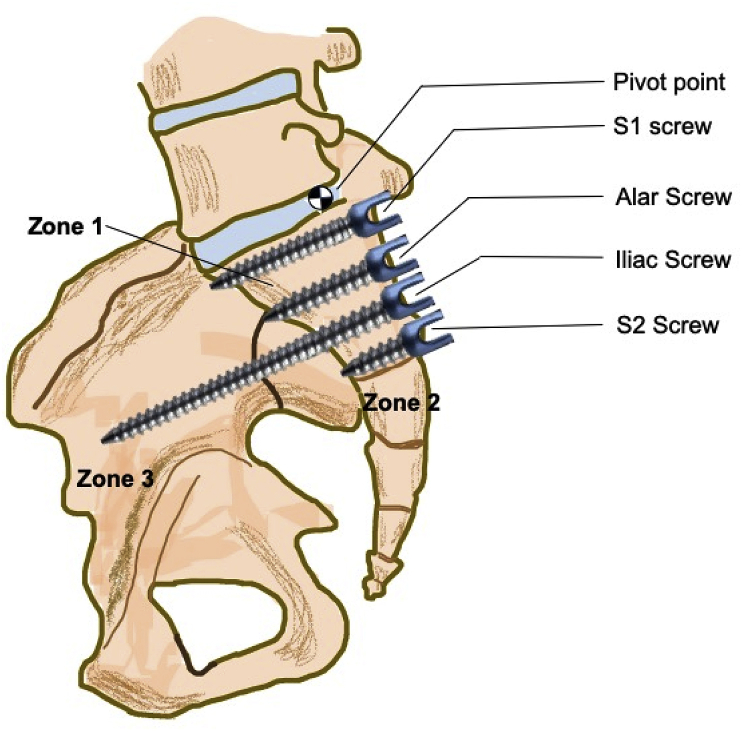
The lumbosacral junction is subject to high amounts of forces which may go to 100 N with some activities.7 McCord et al. introduced the concept of pivot point across lumbosacral area8 with the central axis of the pivot acting along the middle osteo-ligamentous column between the last lumbar vertebrae and sacrum. The study concluded that construct stability increases as the fixation progresses more ventral to the pivot point.8
This was followed by Zone concept by O’Brien et al.9 to stratify the strength of the sacropelvic constructs further. They divided the sacral fixation areas into 3 zones. Zone 1 constituted the S1 vertebral body with cephalad alae. Zone 2 is from the S2 vertebral body to the tip of coccyx with caudal sacral alae. Zone 3 constitutes the ilia. The construct stability improves as the fixation extends caudally with more anchor points and is further increased if instrumentation is through zone 3 with fixation points anterior to the lumbosacral pivot.
The significance of these zones is with respect to the stability of the construct. Fixation in Zone 1 with S1 screws or rods is biomechanically the least stable. The most common associated complications are high risk of facet fracture and higher screw pull out.10,11 The disadvantage with Zone II fixations is low bone density with anatomic constraints. The different options of this zone are either to augment S1 screws or to extend the fixation distally. Fixations which include the iliac wings of Zone III are probably, biomechanically, the most stable.12, 13, 14 (Fig. 1).
Fig. 1.
Zones of O’Brien and McCord’s pivot point.
Such complex biomechanics and anatomy across the lumbosacral junction make it imperative for the modern-day spine surgeon to restore the pelvic parameters to get a good clinical and functional result. In order to achieve this goal a thorough knowledge of different options of fixation in the sacropelvic area becomes very important.
2.1. Indications of sacropelvic instrumentation
| Long fusions | Adult degenerative Scoliosis, Neuromuscular Scoliosis, Paralytic curves. |
| Spondylolisthesis | High grade slips |
| Deformity | Kyphotic deformity especially in cases of Ankylosed spine, Pelvic obliquity |
| Fractures | Sacral and sacropelvic fractures |
| Osteotomy | Osteotomies in lower lumbar spine |
| Others | Pseudarthrosis, Tumors, Lumbosacral dislocations, Osteomyelitis |
2.2. Historical perspective
Historically before the dawn of spinal instrumentation, sacropelvic pathologies were managed using whole body casting. This modality had high failure rates owing to complications like inadequate correction, pseudoarthrosis, immobility and sores.15 R. Hibbs had first postulated lumbosacral junction as a “point of greatest strain” in the spine and he advocated lumbosacral fusions in selective cases in 1924.16
In 1947, Paul Harrington devised the first instrumentation system for treatment of scoliosis in patients suffering from polio which was further improvised with an extension to lumbosacral junction.17 Pseudoarthrosis was reported to be as high as 40% with this technique.18,19 Other late complications were sacral hook dislodgement and flat back syndrome.20
In order to combat the fallout of Harrington system, Eduardo Luque in 1970’s introduced the concept of “segmental instrumentation” which was based on multiple fixation points and improved pelvic fixation allowing better correction.21 The advantage of the system was that it gave a correction in coronal and sagittal planes. The rate of pseudoarthrosis was reported to be as low as 6% to as high as 41%.22,23
In mid-1980’s Cotrel-Dubousset technique used screws in caudal part of lumbosacral spine24 in combination with hooks.25 The advantage was of multiple fixation points with 3 dimensional correction in patients with scoliosis.26 Also, the corrections in cases with pelvic obliquity was higher with minimal loss of correction on follow up. Despite the technology and advancement, the rate of pseudoarthrosis reported was as high as 33% and pedicle screw pull out as high as in 44% of the cases.27
Allen and Ferguson in 1983 in an attempt to increase the fusion rates introduced the landmark Galveston technique.28 It involved inserting contoured rods in “L” shape through the paraspinal muscles into ilium from posterior superior iliac spine (PSIS). This increased the stability of the construct in flexion and side bending. The fusion rates were reported to be increased to as high as 94%.28,29 The complications associated with this technique were primarily mechanical in nature. Implant prominence at PSIS was the most unacceptable complication.30, 31, 32 Along with this “windshield wiper” effect was seen radiographically.
2.3. Sacral screws
The different options for sacral fixation include S1 pedicle, S2 pedicle, sacral promontory and sacral alar screws. The S1 screws are directed medially 30–40° parallel to the superior end plate. The wide S1 pedicle is able to accommodate large amounts of medialization of screw, but the overhang of the iliac crest frequently poses a challenge to obtain an adequately medial trajectory. Lehman et al. introduced the “tricortical” purchase concept in order to increase the pull-out strength of the sacral pedicle screws. These screws are inserted in a similar fashion but aim at a cortical purchase in the sacral promontory.33The path of the screw is again 30–40° medially and 15° cephalad. The tricortical trajectory doubles the insertional torque of the bicortical screw inserted parallel to the S1 end plate. The use of S1 pedicle screws alone is not recommended in long constructs because of high failure rates reported to be as high as 44%.34
The S2 pedicle screw insertion raises a theoretical possibility of increasing the strength of fixation by supplementing S1 pedicle screws, but they are not recommended as it doesn’t offer any significant advantage. S2 pedicles are dorsal to the sacral pivot and hence are unable to give any biomechanical advantage.8 Sacral alar screws are usually unicortical screws taking the purchase laterally in the cancellous sacral ala. Alar screws are used as supplemental fixations by many surgeons.
2.4. Iliac screws
Iliac screw fixation is one of the most common modality used for sacropelvic fixation. The primary advantage is higher pull out strength in comparison to the Galveston rods.35 The basis of higher pull out strength is the different plane (coronal) of fixation as compared to the rest of the construct along with cancellous threads and divergence of screws. It also obviates the need of contoured rods in comparison to Galveston technique. The other advantage is increased comfort of the surgeon owing to high amount of freedom in choosing the entry point which is between iliac tubercle and posterosuperior iliac spine (PSIS). This requires usage of connector to connect these screws to the proximal construct. It also gives the advantage of possibility of insertion of multiple iliac screws increasing the strength of the construct.
The insertion technique of iliac screws involves dissection to expose the posterior superior iliac spine (PSIS) subperiosteally. The entry point is classically anterior to the PSIS. The standard process is to create a small osseous depression for screw head accommodation. Anatomically this recess is 1.5 cm cephalad and medial to PSIS. If such space is not created the screw head will lay prominent creating mechanical complications and discomfort to the patient. Two different trajectories in which the screws can be directed are either towards anterior inferior iliac spine (AIIS) or the superior portion of acetabulum. The preferred path is from PSIS to AIIS which is made using a probe directing it 25° lateral and 30° caudal. The screw lengths can be decided based on intra operative imaging but are typically 8 mm in diameter and 80–100 mm in length (Fig. 2, Fig. 3). The advantage of screws directed towards AIIS is insertion of longer screws along with decreased chances of breech of wall of acetabulum.36
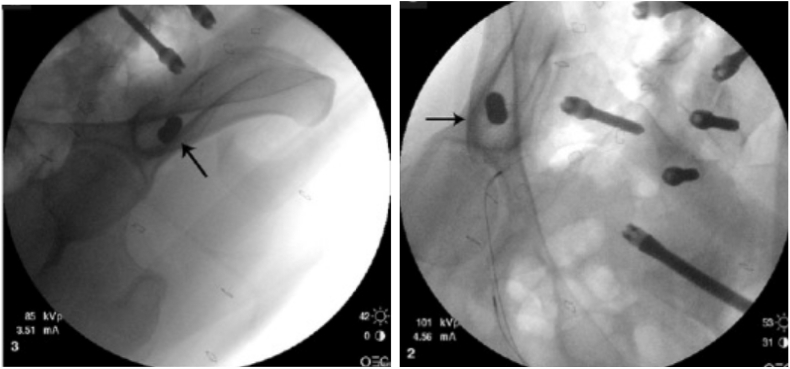
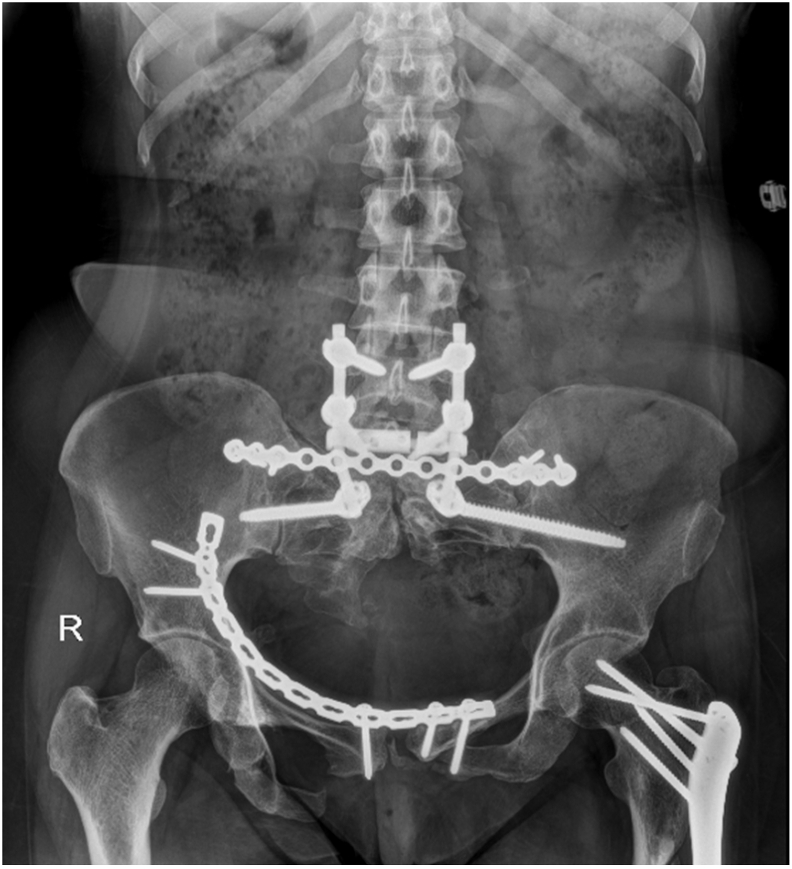
Fig. 2.
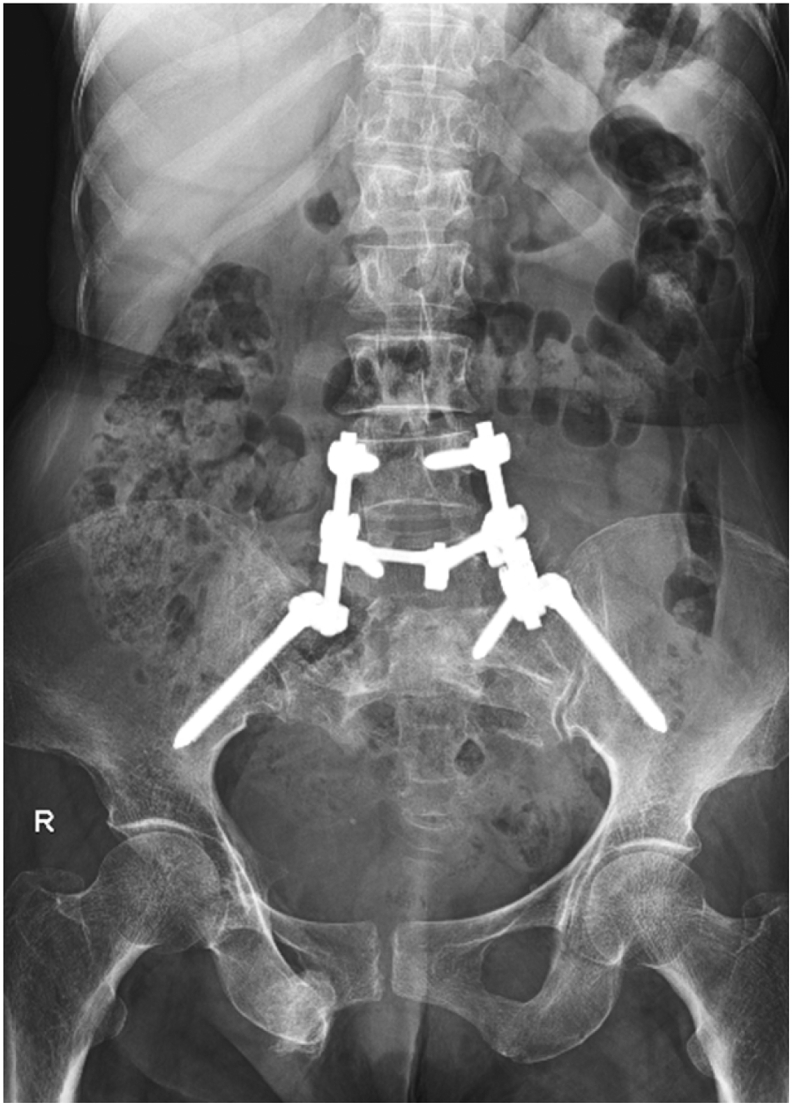
Use of bilateral iliac screws for lumbosacral fusion in a 56year old female having a sacral fracture involving the right L5-S1 facet.
Fig. 3.
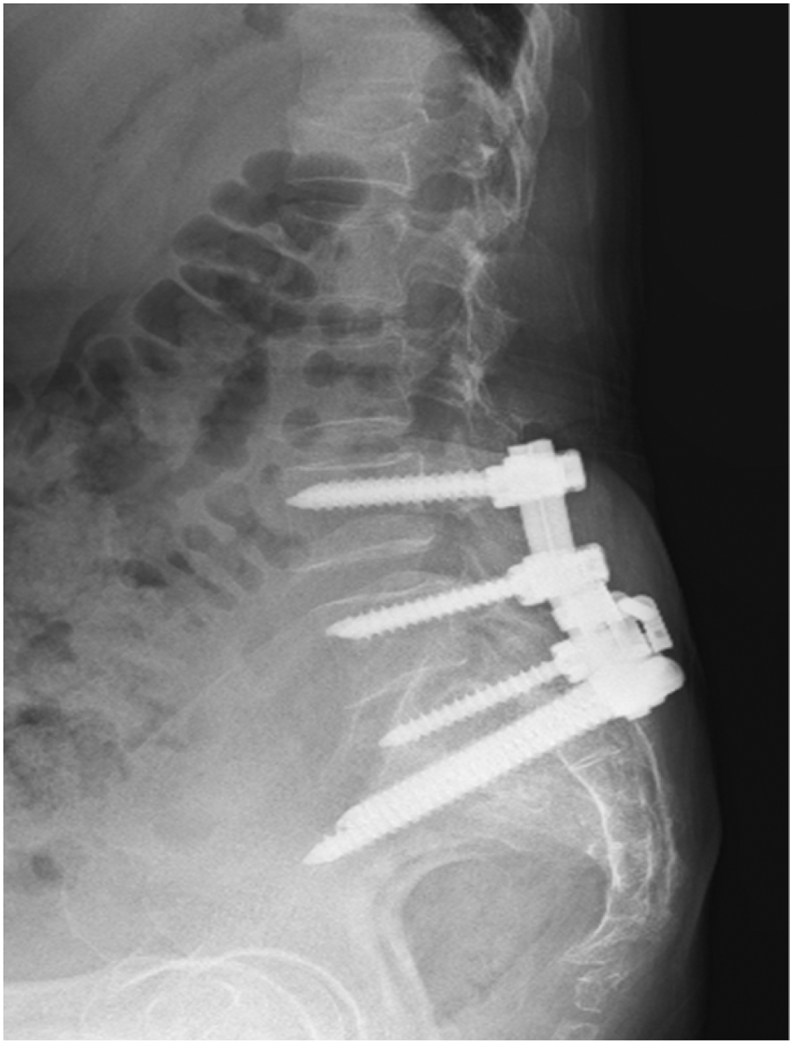
Lateral view showing bilateral iliac screws lumbosacral fusion in a 56 year old female having a sacral fracture involving the right L5-S1 facet.
The insertion of these screws puts structures in sciatic notch at risk of iatrogenic damage (superior gluteal artery and sciatic nerve). The insertion of screws needs far lateral dissection and exposure increasing the risks of surgical site infections to 4%.37 The entry point of the screws is too superficial causing mechanical complications leading to almost 34% patients needing implant removal.38
2.4.1. Multiple rods technique
This technique was described by Shen et al in 2006 in an attempt to reduce the incidence of screw pull-out and rod breakage during lumbopelvic fixations.39 The technique involved inserting two iliac screws on each side and then connecting them with two separate rods to lumbar pedicle screws at different levels on each side. This technique using multiple rods was proven to be biomechanically better as compared to the standard two rods and was recommended only for complex lumbopelvic reconstructions like total sacrectomy.
However, the technique is challenging as it needs very precise placement of lumbar pedicle screws to create an offset between two contiguous level screws to facilitate two rods to be placed side by side. Moreover, this technique leads to compromised purchase of the lumbar pedicle screws and usually requires additional lumbar levels to be involved in the fusion construct.
2.4.2. Percutaneous iliac screws (Cannulated)
The prerequisite for these screws is a good radiolucent table with a good C-arm technician. It is important to localize sciatic notch to prevent any injury to sciatic nerve. A diagonal stab incision is made overlying PSIS. Jamshidi needle is docked into superficial aspect of PSIS moving it ventromedially. The entry point can be flexible as per the trajectory aimed for. As described above recess is created for screw head. Jamshidi needle is advanced further up to 2 cm after which it is replaced with a K wire. It is recommended to tap prior to insertion of these screws. It is of paramount importance to be vigilant in osteoporotic bone, as breech with such technique is easier.
2.4.3. S2-ALAR-ILIAC screws (S2AI)
The S2-alar-iliac screw was first described in 2007 by Sponseller and Kebaish40 to combat the shortcomings and limitations of iliac screw fixation techniques. They are primarily used in the cases of paediatric and adult deformities. The distinct advantages of S2AI screws are that they align in line with S1 screws, therefore obviating the need for an extensive lateral dissection or a separate incision. The screws fall in line with the cephalad construct, this makes rod insertion easier with no need of rod connectors.41 Other advantages include adding to the stability of the construct and lesser implant prominence.
S2AI technique: The authors prefer the free hand technique for S2AI screws. The starting point is in between S1 and S2 foramen, medial to the lateral crest (Fig. 4). Once the entry point is defined, a drill or probe is used to fashion the screw trajectory. It is recommended to use intra-operative imaging to optimize screw trajectory. Once entry is confirmed either a 2.5 mm drill or a probe is used to define the path. The direction of the drill should be laterally with an inclination of 40° in the horizontal plane and 20–30° caudally depending on the pelvic tilt42, 43 (Fig. 5, Fig. 6). These values may slightly differ with pelvic tilt and sacral anatomy.43 Intraoperative fluoroscopy should demarcate the sciatic notch clearly in anteroposterior view. The drill should be aimed within an area span of 20 mm proximal to the sciatic notch and towards anteroinferior iliac spine. A tear drop C arm image helps to confirm the anteroposterior trajectory within ilium (rule out any cortical breach) once the drill/probe crosses SI joint (Fig. 7). The gearshift technique is important in creating this trajectory. Initially the probe is directed posteriorly until SI joint is reached. Ball tip is used to confirm the intra osseous trajectory. Once that is confirmed, probe is reinserted and rotated 180° to face anteriorly, creating the rest of the screw path (Fig. 8). This hole should be verified by a ball tip sound to palpate 5 bony walls-medial, lateral, superior, inferior and anterior/bottom. A k wire is inserted through this pilot hole to determine the length of the hole. A polyaxial screw of 80–90 mm length and of 7–9 mm should be inserted. Intra operative C arm images confirm the trajectory of the screw. It is important to rule out any violation of sciatic notch, acetabulum or the pelvic cavity (Fig. 9).
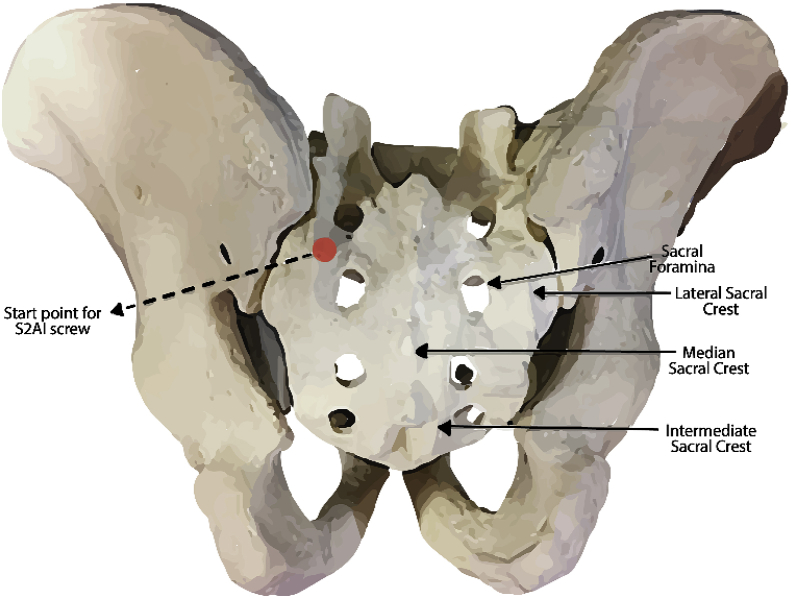
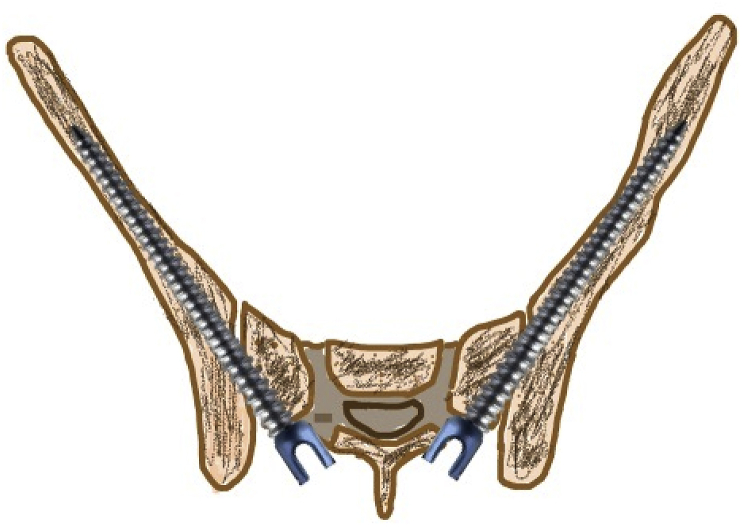
Fig. 4.
Entry point S2AI screw (Between S1 and S2 foramen medial to the lateral sacral creast).
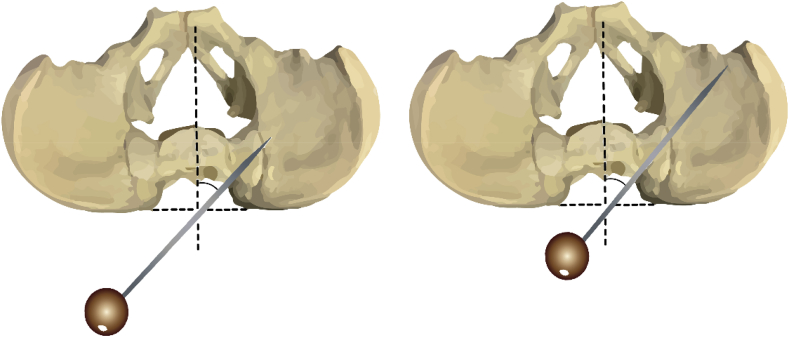
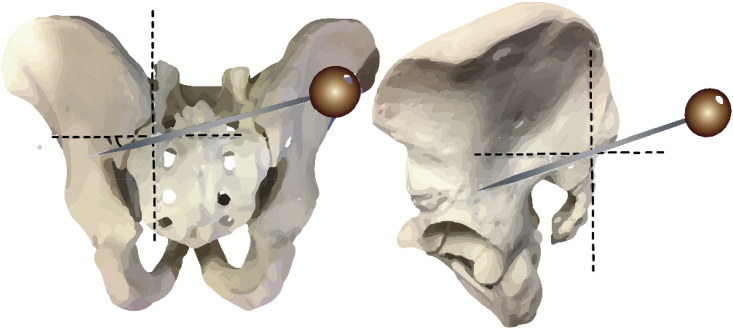
Fig. 5.
The inclination in the axial plane.
Fig. 6.
The trajectory is within 20 mm of sciatic notch.
Fig. 7.
A and B- Obturator oblique view showing screw tips within the tear drop.
Source of image: Vilela MD, Braga BP, Pedrosa HAS. Fluoroscopy only for the placement of long iliac screws: A study on 14 patients. Surg Neurol Int. 2018; 9:108. Published 2018 May 25. https://doi.org/10.4103/sni.sni_59_18.
Fig. 8.
Steps of insertion of S2AI screws.
A- Gearshift technique in which to avoid the anterior cortex breach, the probe is rotated. B- Once no breach is confirmed, k wire is inserted. C- Tapping and size of screw is determined. D- Finally, the screw is inserted.
Fig. 9.
Final position of S2AI screws.
Smith44 et al. reported a prevalence of 10.4% of asymptomatic translucency on follow up in a study of S2AI screws. Mazur et al.45 reported a revision rate of around 4% in S2AI fixations. Martin et al.46 published their work on percutaneous insertion of S2AI screws. They reported less blood loss, lesser infection and faster post-operative recovery. Though the complication profile of S2AI screws is lesser in comparison to iliac screws, the etiology of loosening is different. Short term acute failures were reported to be higher with S2AI screws by Guler et al47 Higher amount of stresses at the junction of screw head and shaft creating an acute angle was thought to be the cause. This caused the failure when these screws crossed the sacroiliac joint. Higher loosening rates of S2AI screws were reported in osteoporotic bone by Enercan et al48 They hypothesized that the cause of failure was instability of proximal part of the screw in the osteoporotic sacral alar bone.
Sacroiliac joint pain (SIJP) is a known complication of multisegmented fusions. It is hypothesized that since S2AI screws cross the sacroiliac joint, it may lead to degeneration and eventually SIJP. Literature reports that fixations extending to sacrum have higher chances of SIJP whereas the ones extending to pelvis rarely have SIJP. Unoki et al.49 had hypothesized that if the S2AI screws were not anchored in the sacroiliac joint properly and are associated with loosening, this will lead to SIJP.
With the usage of S2AI screws, the sacroiliac joint is transfixed. Hence S2AI screws hold the advantage of least incidence of SIJP possibly.49
2.4.4. Navigation and robotic technique
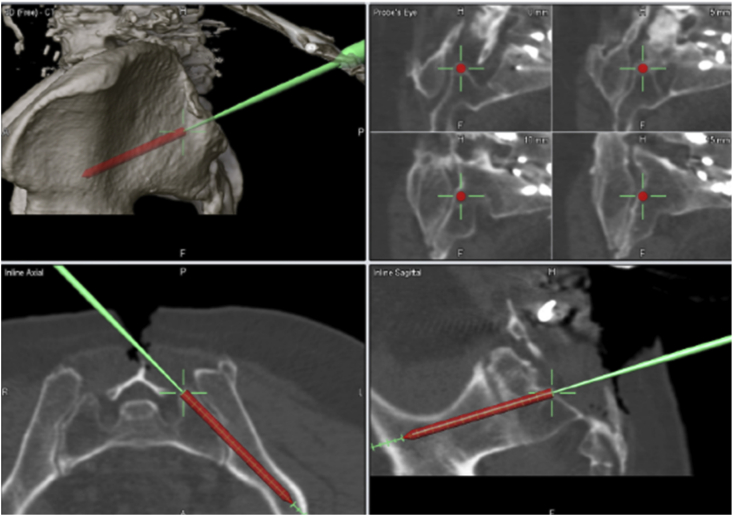
Prior to the dawn of robotics, computer assisted optical navigation system was a new development for pedicle screw placement, including S2AI screws. It involves pre-operative planning with specific drill, positioning guide, trajectory planning for accurate screw placement (Fig. 10). Ray et al.50 in their navigation series reported successful use of navigation for S2AI screw placement. There was a single breech amongst 36 reported screws. This patient required repositioning of screw owing to anterior breach.
Fig. 10.
Intra op navigation guidance and trajectory for S2AI screws
Source- Phan, Kevin & Li, Julian & Giang, Gloria & Teng, Ian & Phan, Steven & Chang, Nicholas & Mobbs, Ralph. (2017). Technical note A novel technique for placement of sacro-alar-iliac (S2AI) screws by K-wire insertion using intraoperative navigation. Journal of Clinical Neuroscience. 45. 10.1016/j.jocn.2017.08.049.
Navigation requires use of stereotactic frame. This frame is mounted on the spinous process of the lumbar vertebrae. The entry point has to be determined on a CT scan preoperatively or intraoperatively and is same as that with free hand technique. Errors are minimized using the metallic frame attached to the spinous process. It is of paramount importance that the screw size and trajectory is determined on the CT scan. Phan et al.51 used K wire and Jamshidi needle to create the trajectory that was determined on the CT scan. Once the track is created, screw is inserted.
For robotics, preoperatively, CT scan with 1 mm cuts is a prerequisite. This CT scan must be uploaded in the planning software. The vertebral bodies are segmented individually so that the change in position doesn’t change the registration done. Planning also involves determining the screw trajectory and position. After determining the entry point for S2AI screw (between S1 and S2 foramen, medial to the lateral crest) the screws must be directed laterally in the sacral ala across the sacro iliac joint into the ilium. After positioning, C arm images are used to synchronize the position with the preoperative CT scan. This completes the registration process. The robot is set into position with the required bridge platform. The predetermined arms are fixed to the robot and drill tube is inserted. Once drilling is complete ball tip may be used to confirm the integrity of bony walls. Once confirmed, adequate size screw is inserted.
Bederman et al.52 reported their experience of 31 S2AI screws with robotic guidance. Even though the trajectories were accurate, there were 20 screws protruding the ilium distally by less than 2 mm, 1 screw by 2–4 mm, and 10 screws by 4 mm or more. There was no associated sciatic notch breech, intrapelvic breech, proximal breech, neurovascular damage. Shillingford et al.53 compared free hand vs robotic placement of S2AI screws. They reported no significant difference with respect to accuracy and complications.
One of the primary concerns with the use of robot is breech in the cortex of the bone. Hu and Libermann54 assessed 35 screws and confirmed no breeches. They also reported minimal deviation from the original plan of S2AI screw with the use of robotic technology. Similarly, Laratta et al.55 reported 95.7% accuracy with breech in two screws. This study is more specific since they confirmed the cortical breech with intra operative CT scan. No other study to our knowledge assessed breech on CT scans.
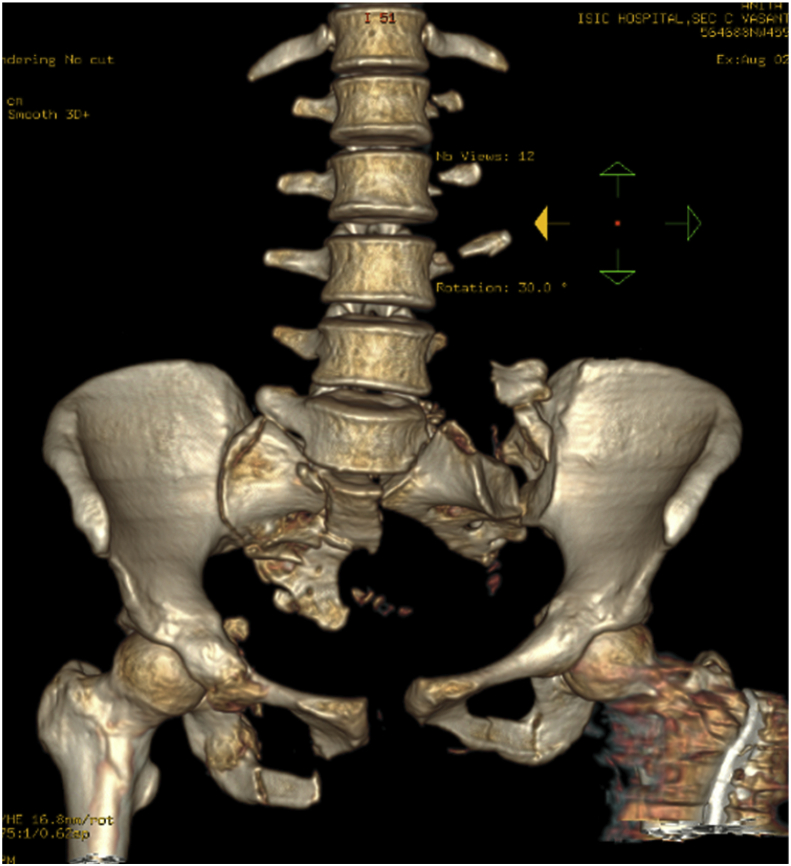
From the case series of the authors (Fig. 11, Fig. 12, Fig. 13, Fig. 14).
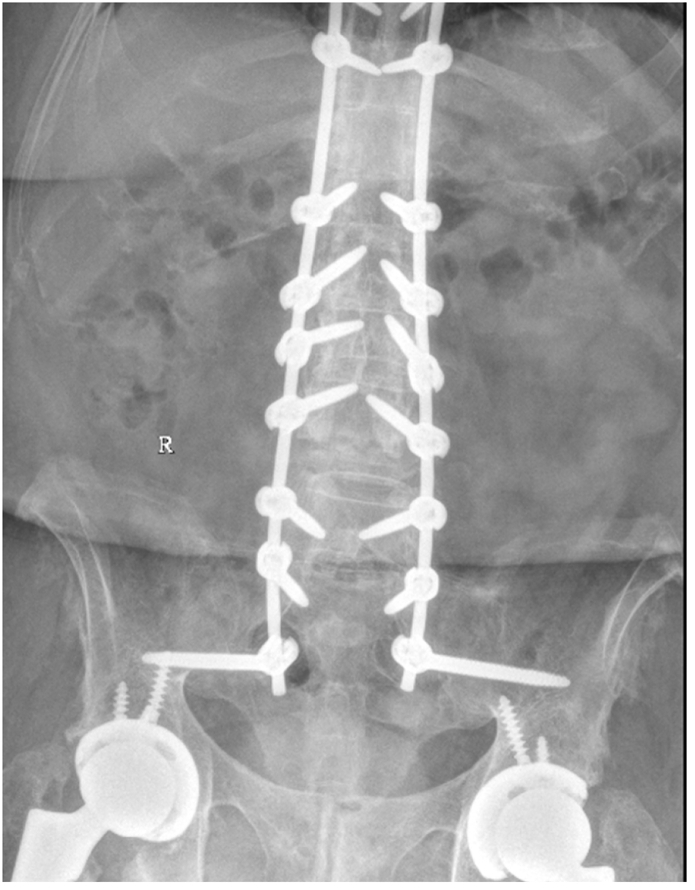
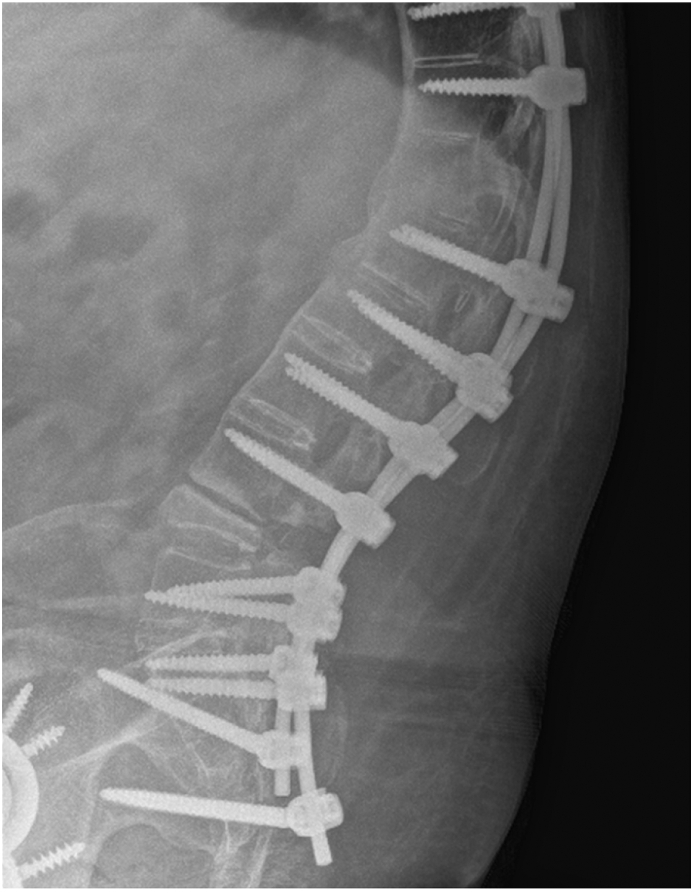
Fig. 11.
3D reconstruction of a Traumatic sacral fracture in a 39year old female with left sacroiliac dissociation.
Fig. 12.
The patient was treated with a Lumbosacral construct with S2AI screws.
Fig. 13.
A 38/M with Ankylosing spondylitis treated with PSO at L4 for kyphotic deformity correction with horizontal gaze. The construct is supplemented with S2AI screws for better stability.
Fig. 14.
Lateral view showing S2AI screws in the same case.
2.4.5. S2AI screws vs iliac screws
Multiple studies over the time have favoured the use of S2AI screws over iliac screws with the advantages of less infections/wound dehiscence, revisions, failures, postoperative pain.56, 57, 58, 59 Level 1 study by Keorochana et al.60 compared S2AI screws with iliac screws in paediatric and adult population. They concluded that iliac screw fixation was associated with higher complications and increased rates of revisions. There was no difference in the VAS scores between the two groups. The findings were similar in adult and paediatric population.
De la Garza Ramos et al.61 reported their meta-analysis on five, level III evidence studies. S2AI were reported to have lesser incidence of biomechanical failure and lesser complications as compared to iliac screws. Their analysis was based on adult spine. However, none of these studies commented on cost of surgery, quality of life, satisfaction levels, quality of life and cost efficacy analysis.
Hasan et al.62 did a meta-analysis with a primary intent to compare post-operative complications between Iliac and S2AI screw. On one hand, they concluded that S2AI screws with a lower profile have made a significant impact in reducing complications associated with conventional iliac screws but on the other hand, they highlighted one of the concerns with S2AI screws which is sacroiliac joint violation. They also brought out that modifications of iliac screw insertion technique could reduce complications associated with screw prominence. Elder et al.56 reported similar incidence of proximal junctional failure, Sacro iliac joint pain, pseudoarthrosis in both groups.
Mazur et al.58 advocated S2AI screws primarily because of greater cortical purchase and obviation of use of connectors which as used in cases of iliac screws acts as a potential site of failure. Lee et al.63 reported lower incidence of implant failure with S2AI screws as compared to iliac screws. This difference was nullified with the usage of cross links in iliac screw construct. Perrault et al. reported that use of lateral connectors adds to the loads and stress on iliac screws. They concluded a 17% decrease in toggle movement on screws if the screws were inserted from sacrum instead of standard iliac crests as the entry point.64
Ilyas et al in 2015 compared clinically and radiologically iliac and S2AI screws.57 They reported statistically better outcomes with respect to implant loosening, acute infections, late pain, revision surgery because of implant loosening and delayed wound complications with usage of S2AI screws compared with iliac screws. Sponseller et al. reported better pelvic obliquity corrections with S2AI screws.65
Hoernschemeyer et al.’s66 biomechanical study compared the stiffness between S2AI and iliac screws on cadaver models. They reported less stiffness in iliac screws. These results were not statistically significant. O’Brien et al.67 evaluated the strength of S2AI and iliac screws biomechanically. They concluded that constructs ending at S1 are less stable as compared to S2AI and iliac screw construct. However, there was no difference between S2AI and iliac screws constructs. Furthermore, different sizes of S2AI screws (65, 80, 90 mm) are biomechanically similar strength wise.
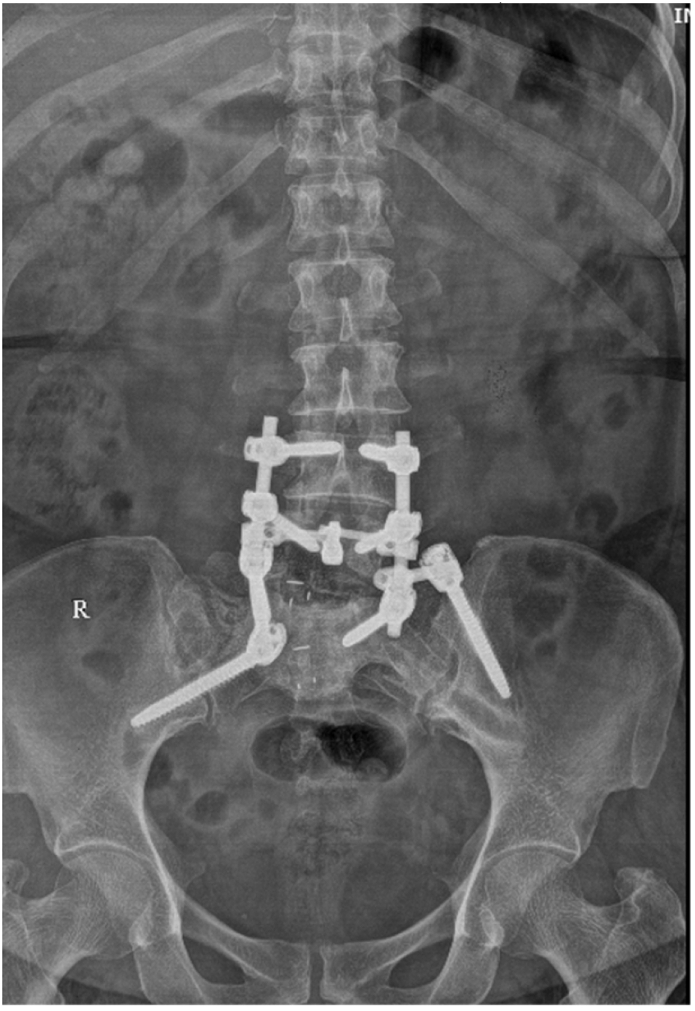
Example from authors case series - Sacropelvic fusion in a case of L5-S1 pseudarthrosis using Left iliac screw and right sided S2AI screw for better stability of the construct (Fig. 15, Fig. 16)
Fig. 15.
An example of Sacropelvic fusion in a case of L5-S1 pseudarthrosis using left iliac screw and right sided S2AI screw for better stability of the construct.
Fig. 16.

Lateral view with left iliac screw and right sided S2AI screw.
2.4.6. S1-ALAR-ILIAC screws (S1AI)
S1AI screws are a salvage option in cases with a failed promontory screw. They also are preferred by surgeons who are concerned with soft tissue dissection for S2 pedicle screws. The entry point is at the same landmark as that of entry of S1 pedicle. The entry point should not be too lateral or too medial. Lateral entry won’t give adequate purchase in sacrum and if excessively medially, it will deviate from the construct cranially. The angulation is 35–45° caudally and 20° horizontally in the coronal plane. The aim is to target ipsilateral greater trochanter with oblique views confirming the trajectory.68
2.4.7. Combined S1AI and S2AI screws
Mattei et al in 2013 described salvage technique in cases of pseudoarthrosis and severe deformities or failed fixation.69 They advocated usage of combination of S1AI with S2AI screws for biomechanically stronger fixation and better union. It is also important to mention that they reported no significant radiolucency or infections in their follow up.
2.4.8. S3- ALAR- ILIAC screws (S3AI)
Mattei in the year 2020 has described S3AI70 as salvage technique in complex deformities as a bail out procedure. The entry point of S3AI screws is located at the midpoint of S2 and S3 foramina, 2 mm medial to the lateral iliac crest. Mattei et al. expressed their reservation on free hand insertion of these screws in view of proximity to the sciatic notch. They advocate usage of navigation systems for such screws.
2.4.9. Advancments in screw design
There have been newer designs of screws which are indicated for fixation around sacroiliac area.
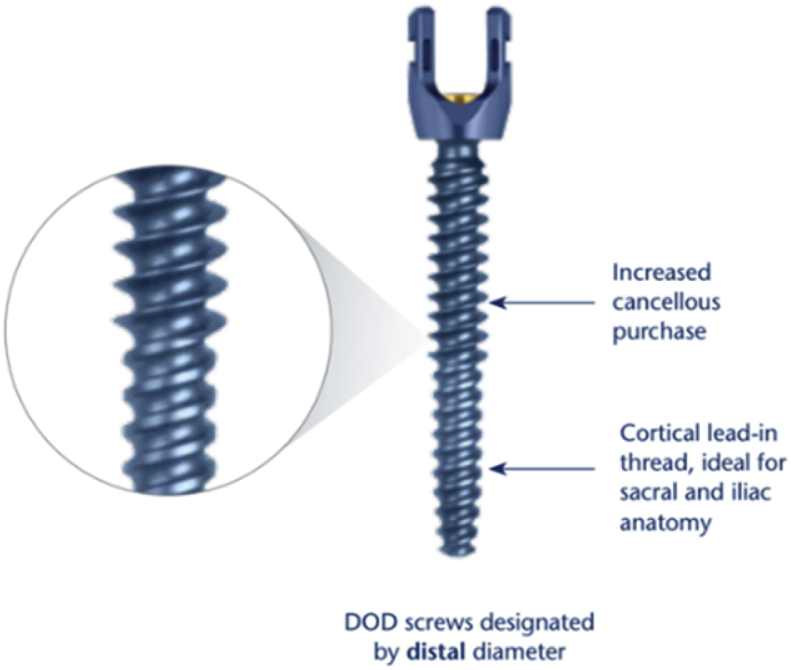
Dual outer diameter (DOD) screws: These screws have nominal diameter at distal end which helps for deeper insertion into Ilium without perforating. They are designed primarily for better fixation in sacrum, ilium and osteoporotic bones. The diameter of distal and proximal is in various combinations. The advantage is for better purchase in cancellous as well as cortical bone (Fig. 17).
Fig. 17.
Dual outer diameter screws.
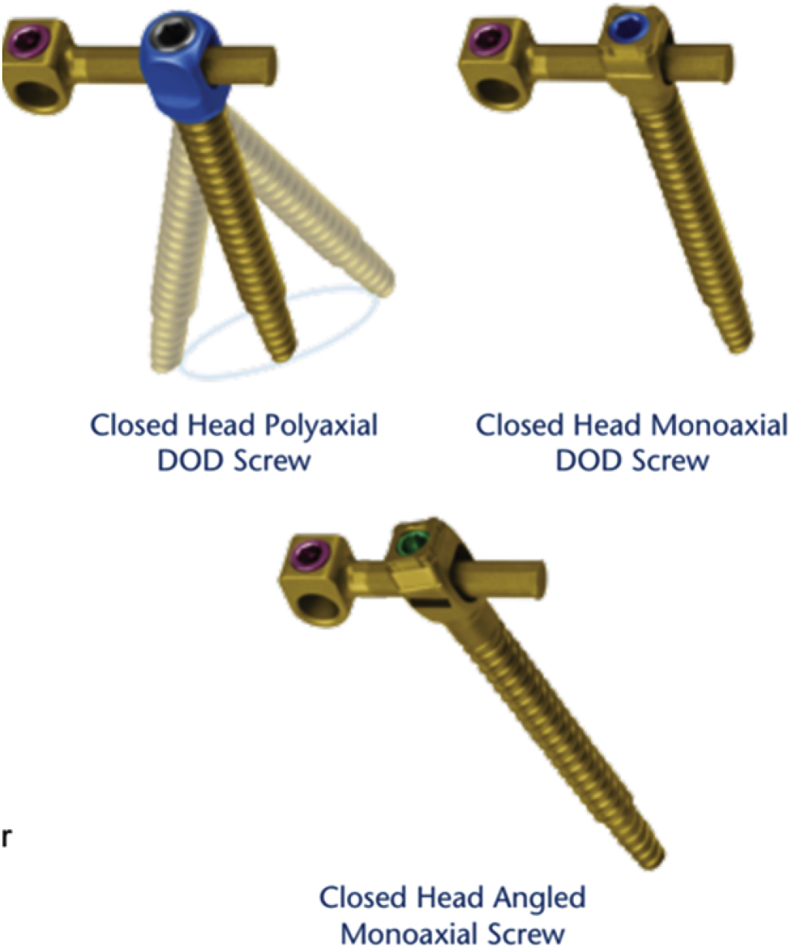
Closed head dual outer diameter (DOD) screws: These screws were designed with primary indication of fixation in ilium. They have better purchase in cancellous bone. The screws taper distally for better piloting between the cortical walls. The strength is maintained with maintained core diameter. These closed screw heads provide better security and better profile. It accepts round, faceted, D shaped offset. These screws may be polyaxial (provide 30° angulation in all planes), monoaxial or angled monoaxial screws (fixed tilf of 15° for easy placement) (Fig. 18).
Fig. 18.
Closed head DOD polyaxial, Monoaxial, Angled Monoaxial screws.
3. Summary
The sacropelvic fixation modalities have evolved over time with respect to technique and indications. With the current availability of multiple techniques, the preferred technique remains S2AI and iliac screws. However, S2AI screws have the edge owing to lesser complications with respect to implant and to soft tissue.
References
- 1.Goodwin CR, Kosztowski TA, Elder BD, et al. Complex lumbosacropelvic fixation techniques. In: Steinmetz MP, Benzel EC, editors. Benzel’s Spine Surgery: Techniques, Complication Avoidance, and Management. Philadelphia, PA: Elsevier; 2017760e767.e2.
- 2.Panjabi M.M., White A.A., III Basic biomechanics of the spine. Neurosurgery. 1980;7:76e93. doi: 10.1227/00006123-198007000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Dietrich M., Kurowski P. The importance of mechanical factors in the etiology of spondylolysis. A model analysis of loads and stresses in human lumbar spine. Spine (Phila Pa 1976) 1985;10:532e42. doi: 10.1097/00007632-198507000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Colombini D., Occhipinti E., Grieco A. Estimation of lumbar disc areas by means of anthropometric parameters. Spine (Phila Pa 1976) 1989;14:51e5. doi: 10.1097/00007632-198901000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Zheng Y., Lu W.W., Zhu Q. Variation in bone mineral density of the sacrum in young adults and its significance for sacral fixation. Spine (Phila Pa 1976) 2000;25:353e7. doi: 10.1097/00007632-200002010-00016. [DOI] [PubMed] [Google Scholar]
- 6.Terry R.J.H. Osteology. In: Schaeffer J.P., editor. Morris’ Human Anatomy. Blakiston; Philadelphia, PA: 1947. p. 77e265. [Google Scholar]
- 7.Kornblatt M.D., Casey M.P., Jacobs R.R. Internal fixation in lumbosacral spine fusion. Clin Orthop Relat Res. 1986;203:141–150. [PubMed] [Google Scholar]
- 8.McCord D.H., Cunningham B.W., Shono Y. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976) 1992;17(8 Suppl):S235–S243. doi: 10.1097/00007632-199208001-00004. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien M.F. Sacropelvic fixation in spinal deformity. In: DeWald R.L., editor. Spinal Deformities: The Comprehensive Text. Thieme; New York: 2003. pp. 601–614. [Google Scholar]
- 10.O’Brien M.F., Kuklo T.R., Lenke L.G. Sacropelvic instrumentation: anatomic and biomechanical zones of fixation. Semin Spine Surg. 2004;16:76e90. [Google Scholar]
- 11.McCarthy R.E., Dunn H., McCullough F.L. Luque fixation to the sacral ala using the Dunn-McCarthy modification. Spine (Phila Pa 1976) 1989;14:281e3. doi: 10.1097/00007632-198903000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Ebraheim N.A., Lu J., Yang H. Anatomic considerations of the second sacral vertebra and dorsal screw placement. Surg Radiol Anat. 1997;19:353e7. doi: 10.1007/BF01628500. [DOI] [PubMed] [Google Scholar]
- 13.Leong J.C.Y., Lu W.W., Zheng Y. Comparison of the strengths of lumbosacral fixation achieved with techniques using one and two triangulated sacral screws. Spine (Phila Pa 1976) 1998;23:2289e94. doi: 10.1097/00007632-199811010-00008. [DOI] [PubMed] [Google Scholar]
- 14.Louis R. Fusion of the lumbar and sacral spine by internal fixation with screw plates. Clin Orthop Relat Res. 1986;203:18e33. [PubMed] [Google Scholar]
- 15.Balderston R.A., Winter R.B., Moe J.H. Fusion to the sacrum for nonparalytic scoliosis in the adult. Spine (Phila Pa 1976) 1986;11:824e9. doi: 10.1097/00007632-198610000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Hibbs R.A. A report of fifty-nine cases of scoliosis treated by the fusion operation. By Russell A. Hibbs, 1924. Clin Orthop Relat Res. 1988;(229):4–19. [PubMed] [Google Scholar]
- 17.Harrington P.R. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44:591–610. [PubMed] [Google Scholar]
- 18.Kostuik J.P. Treatment of scoliosis in the adult thoracolumbar spine with special reference to fusion to the sacrum. Orthop Clin N Am. 1988;19:371–381. [PubMed] [Google Scholar]
- 19.Devlin V.J., Asher M.A. Biomechanics and surgical principles of long fusions to the sacrum. Spine State Art Rev. 1996;10:515–544. [Google Scholar]
- 20.Balderston R.A., Winter R.B., Moe J.H. Fusion to the sacrum for nonparalytic scoliosis in the adult. Spine. 1986;11:824–829. doi: 10.1097/00007632-198610000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Luque E.R., Cardoso A. Segmental correction of scoliosis with rigid internal fixation, a preliminary report. Orthop Trans. 1977;1:136–137. [Google Scholar]
- 22.Boachie-Adjei O., Lonstein J.E., Winter R.B. Management of neuromuscular spinal deformities with Luque segmental instrumentation. J Bone Joint Surg Am. 1989;71(4):548–562. [PubMed] [Google Scholar]
- 23.Kostuik J.P., Errico T.J., Gleason T.F. Techniques of internal fixation for degenerative conditions of the lumbar spine. Clin Orthop Relat Res. 1986;203:219–231. [PubMed] [Google Scholar]
- 24.Cotrel Y., Dubousset J., Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10e23. [PubMed] [Google Scholar]
- 25.CotrelY Dubousset J. New segmental posterior instrumentation of the spine. Orthop Trans. 1985;9:118. [Google Scholar]
- 26.Camp J.F., Caudle R., Ashmun R.D. Immediate complications of Cotrel-Dubousset instrumentation to the sacro-pelvis. A clinical and biomechanical study. Spine. 1990;15:932–941. doi: 10.1097/00007632-199009000-00018. [DOI] [PubMed] [Google Scholar]
- 27.Camp J.F., Caudle R., Ashmun R.D. Immediate complications of Cotrel-Dubousset instrumentation to the sacro-pelvis. A clinical and biomechanical study. Spine (Phila Pa 1976) 1990;15:932e41. doi: 10.1097/00007632-199009000-00018. [DOI] [PubMed] [Google Scholar]
- 28.Allen B.L., Jr., Ferguson R.L. The Galveston experience with L-rod instrumentation for adolescent idiopathic scoliosis. Clin Orthop Relat Res. 1988;229:59e69. [PubMed] [Google Scholar]
- 29.Gau Y.L., Lonstein J.E., Winter R.B. Luque-Galveston procedure for correction and stabilization of neuromuscular scoliosis and pelvic obliquity: a review of 68 patients. J Spinal Disord. 1991;4:399e410. doi: 10.1097/00002517-199112000-00001. [DOI] [PubMed] [Google Scholar]
- 30.Saer E.H., III, Winter R.B., Lonstein J.E. Long scoliosis fusion to the sacrum in adults with nonparalytic scoliosis. An improved method. Spine (Phila Pa 1976) 1990;15:650e3. doi: 10.1097/00007632-199007000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Allen B.L., Jr., Ferguson R.L. L rod instrumentation for scoliosis in cerebral palsy. J Pediatr Orthop. 1982;2:87–96. [PubMed] [Google Scholar]
- 32.Broom M.J., Banta J.V., Renshaw T.S. Spinal fusion augmented by Luque-rod segmental instrumentation for neuromuscular scoliosis. J Bone Joint Surg Am. 1989;71:32–44. [PubMed] [Google Scholar]
- 33.Lehman R.A., Jr., Kuklo T.R., Belmont P.J., Jr. Advantage of pedicle screw fixation directed into the apex of the sacral promontory over bicortical fixation: a biomechanical analysis. Spine. 2002;27:806–811. doi: 10.1097/00007632-200204150-00006. [DOI] [PubMed] [Google Scholar]
- 34.Devlin V.J., Boachie-Adjei O., Bradford D.S. Treatment of adult spinal deformity with fusion to the sacrum using CD instrumentation. J Spinal Disord. 1991;4:1e14. [PubMed] [Google Scholar]
- 35.Schwend R.M., Sluyters R., Najdzionek J. The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine (Phila Pa 1976) 2003;28:542–547. doi: 10.1097/01.BRS.0000049925.58996.66. [DOI] [PubMed] [Google Scholar]
- 36.Berry J.L., Stahurski T., Asher M.A. Morphometry of the supra sciatic notch intrailiac implant anchor passage. Spine (Phila Pa 1976) 2001;26:E143e8. doi: 10.1097/00007632-200104010-00002. [DOI] [PubMed] [Google Scholar]
- 37.Kuklo T.R., Bridwell K.H., Lewis S.J. Minimum 2- year analysis of sacropelvic fixation and L5–S1fusion using S1 and iliac screws. Spine (Phila Pa1976) 2001;26 doi: 10.1097/00007632-200109150-00007. 1976–83. [DOI] [PubMed] [Google Scholar]
- 38.Tsuchiya K., Bridwell K.H., Kuklo T.R. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976) 2006;31(3):303–308. doi: 10.1097/01.brs.0000197193.81296.f1. [DOI] [PubMed] [Google Scholar]
- 39.Shen F.H., Harper M., Foster W.C. A novel ‘‘four rod technique’’ for lumbo-pelvic reconstruction: theory and technical considerations. Spine. 2006;31(12):1395–1401. doi: 10.1097/01.brs.0000219527.64180.95. [DOI] [PubMed] [Google Scholar]
- 40.Sponseller P.D. The S2 portal to the ilium. Roundtables Spine Surg. 2007;2(2):83–87. [Google Scholar]
- 41.O’Brien J.R., Yu W.D., Bhatnagar R. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976) 2009;34:E439e42. doi: 10.1097/BRS.0b013e3181a4e3e4. [DOI] [PubMed] [Google Scholar]
- 42.Kebaish K.M., Dafrawy M. Sacropelvic fixation. In: Vaccaro A.R., Baron E., editors. Operative Techniques: Spine Surgery. Elsevier; Philadelpia: 2016. pp. 240–254. [Google Scholar]
- 43.Zhu F., Bao H.D., Yuan S. Posterior second sacral alar iliac screw insertion: anatomic study in a Chinese population. Eur Spine J. 2013;22(7):1683–1689. doi: 10.1007/s00586-013-2734-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith E.J., Kyhos J., Dolitsky R. S2 alar iliac fixation in long segment constructs, a two- to five-year follow-up. Spine Deform. 2018;6:72e8. doi: 10.1016/j.jspd.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 45.Mazur M.D., Mahan M.A., Shah L.M. Fate of S2-alar-iliac screws after 12-month minimum radiographic follow-up: preliminary results. Neurosurgery. 2017;80:67e72. doi: 10.1227/NEU.0000000000001322. [DOI] [PubMed] [Google Scholar]
- 46.Martin C.T., Witham T.F., Kebaish K.M. Sacropelvic fixation: two case reports of a new percutaneous technique. Spine (Phila Pa 1976) 2011;36(9):E618–E621. doi: 10.1097/BRS.0b013e3181f79aba. [DOI] [PubMed] [Google Scholar]
- 47.Guler Uo C.E., Yaman O., Pellise F. European Spine Study Group. Sacropelvic fixation in adult spinal deformity (ASD); a very high rate of mechanical failure. Eur Spine J. 2015;24:1085–1091. doi: 10.1007/s00586-014-3615-1. [DOI] [PubMed] [Google Scholar]
- 48.Enercan M M, Kahraman S, Gokcen B. et al. Radiological outcomes and complications of S2 alariliac fixation in adult patients with osteoporotic spine. Poster Presented at Euro Spine October 2014.
- 49.Unoki E., Miyakoshi N., Abe E. Sacropelvic fixation with S2 alar iliac screws may prevent sacroiliac joint pain after multisegment spinal fusion. Spine (Phila Pa 1976) 2019;44(17):E1024–E1030. doi: 10.1097/BRS.0000000000003041. [DOI] [PubMed] [Google Scholar]
- 50.Ray Wilson, Ravindra Vijay, Schmidt Meic, Dailey Andrew. Stereotactic navigation with the O-arm for placement of S-2 alar iliac screws in pelvic lumbar fixation. J Neurosurg Spine. 2013;18 doi: 10.3171/2013.2.SPINE12813. [DOI] [PubMed] [Google Scholar]
- 51.Phan Kevin, Li Julian, Giang Gloria. Technical note A novel technique for placement of sacro-alar-iliac (S2AI) screws by K-wire insertion using intraoperative navigation. J Clin Neurosci. 2017;45 doi: 10.1016/j.jocn.2017.08.049. [DOI] [PubMed] [Google Scholar]
- 52.Bederman S.S., Hahn P., Colin V., Kiester P.D., Bhatia N.N. Robotic guidance for S2-alar-iliac screws in spinal deformity correction. Clin Spine Surg. 2017;30(1):E49–E53. doi: 10.1097/BSD.0b013e3182a3572b. [DOI] [PubMed] [Google Scholar]
- 53.Shillingford J.N., Laratta J.L., Park P.J. Human versus robot: a propensity-matched analysis of the accuracy of free hand versus robotic guidance for placement of S2 alar-iliac (S2AI) screws. Spine (Phila Pa 1976) 2018;43(21):E1297–E1304. doi: 10.1097/BRS.0000000000002694. [DOI] [PubMed] [Google Scholar]
- 54.Hu X., Lieberman I.H. Robotic-guided sacro-pelvic fixation using S2 alar-iliac screws: feasibility and accuracy. Eur Spine J : Off. Publ.Eur.Spine.Soc. Eur.Spinal Deformity Soc Eur.Sect.Cervical Spine Res. Soc. 2017 Mar;26(3):720–725. doi: 10.1007/s00586-016-4639-5. [DOI] [PubMed] [Google Scholar]
- 55.Laratta J.L., Shillingford J.N., Lombardi J.M. Accuracy of S2 alar-iliac screw placement under robotic guidance. Spine Deform. 2018;6(2):130–136. doi: 10.1016/j.jspd.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 56.Elder B.D., Ishida W., Lo S.L. Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation. Spine (Phila Pa 1976) 2017;42:E142e9. doi: 10.1097/BRS.0000000000001722. Level 4. [DOI] [PubMed] [Google Scholar]
- 57.Ilyas H., Place H., Puryear A. A comparison of early clinical and radiographic complications of iliac screw fixation versus s2 alar iliac (S2AI) fixation in the adult and pediatric populations. J Spinal Disord Tech. 2015;28 doi: 10.1097/BSD.0000000000000222. Level 3. [DOI] [PubMed] [Google Scholar]
- 58.Mazur M.D., Ravindra V.M., Schmidt M.H. Unplanned reoperation after lumbopelvic fixation with S-2 alar-iliac screws or iliac bolts. J Neurosurg Spine. 2015;23:67e76. doi: 10.3171/2014.10.SPINE14541. [DOI] [PubMed] [Google Scholar]
- 59.Shabtai L., Andras L.M., Portman M. Sacral alar iliac (SAI) screws fail 75% less frequently than iliac screws in neuromuscular scoliosis. J Pediatr Orthop. 2017;37 doi: 10.1097/BPO.0000000000000720. Level 3. [DOI] [PubMed] [Google Scholar]
- 60.Keorochana G., Arirachakaran A., Setrkraising K., Kongtharvonskul J. Comparison of complications and revisions after sacral 2 alar iliac screw and iliac screw fixation for sacropelvic fixation in pediatric and adult populations: systematic review and meta-analysis. World Neurosurg. 2019;132:408–420. doi: 10.1016/j.wneu.2019.08.104. [DOI] [PubMed] [Google Scholar]
- 61.De la Garza Ramos R., Nakhla J., Sciubba D.M., Yassari R. Iliac screw versus S2 alar-iliac screw fixation in adults: a meta-analysis. J Neurosurg Spine. 2018;30(2):253–258. doi: 10.3171/2018.7.SPINE18710. [DOI] [PubMed] [Google Scholar]
- 62.Hasan M.Y., Liu G., Wong H.K., Tan J.H. Postoperative complications of S2AI versus iliac screw in spinopelvic fixation: a meta-analysis and recent trends review. Spine J. 2020;20(6):964–972. doi: 10.1016/j.spinee.2019.11.014. [DOI] [PubMed] [Google Scholar]
- 63.Lee M.C., Jarvis C., Solomito M.J. Comparison of S2-Alar and traditional iliac screw pelvic fixation for pediatric neuromuscular deformity. Spine J. 2018;18:648e54. doi: 10.1016/j.spinee.2017.08.253. [DOI] [PubMed] [Google Scholar]
- 64.Desrochers-Perrault F., Aubin C.E., Wang X., Schwend R.M. Biomechanical analysis of iliac screw fixation in spinal deformity instrumentation. Clin Biomech (Bristol, Avon) 2014;29:614–621. doi: 10.1016/j.clinbiomech.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 65.Sponseller P.D., Zimmerman R.M., Ko P.S. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine. 2010;35:1887–1892. doi: 10.1097/BRS.0b013e3181e03881. [DOI] [PubMed] [Google Scholar]
- 66.Hoernschemeyer D.G., Pashuck T.D., Pfeiffer F.M. Analysis of the S2 alar-iliac screw as compared with the traditional iliac screw: does it increase stability with sacroiliac fixation of the spine? Spine J. 2017;17:875e9. doi: 10.1016/j.spinee.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 67.O’Brien J.R., Yu W., Kaufman B.E., Bucklen B., Salloum K., Khalil S. Biomechanical evaluation of S2 alar-iliac screws: effect of length and quad-cortical purchase as compared with iliac fixation. Spine (Phila Pa. 1976;38 doi: 10.1097/BRS.0b013e31829e17ff. E1250– E12552013. [DOI] [PubMed] [Google Scholar]
- 68.Wang Z., Boubez G., Shedid D., Yuh S.J., Sebaaly A. Is S1 alar iliac screw a feasible option for lumbosacral fixation?: a technical note. Asian Spine J. 2018;12(4):749–753. doi: 10.31616/asj.2018.12.4.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mattei Tobias A., Fassett Daniel R. Combined S-1 and S-2 sacral alar-iliac screws as a salvage technique for pelvic fixation after pseudarthrosis and lumbosacropelvic instability. J Neurosurg Spine. 2013;19(3):321–330. doi: 10.3171/2013.5.SPINE121118. [DOI] [PubMed] [Google Scholar]
- 70.Mattei T.A. S3 sacral-alar iliac (S3AI) screw, a salvage technique for pelvic fixation in complex deformity surgery: technical note. World Neurosurgery. 2020 Mar doi: 10.1016/j.wneu.2020.03.025. [DOI] [PubMed] [Google Scholar]