Abstract
Aim
Osteoporotic vertebral compressive fractures (VCFs) are known to be commonly missed in X-rays indicated for pulmonary or heart diseases. In this study, we investigated the underreporting status of VCF in back pain clinic patients when the spine was the focus of interest.
Materials and methods
This is a retrospective analysis of 105 female cases (mean: 72 years, range: 55–93 years) from a tertiary hospital in China (facility A, FA). The patients with back and/or leg pain were referred for a spine X-ray. The images were retrieved and transferred to a central reading facility (facility B, FB), where images were double-read by two readers experienced in evaluating osteoporotic vertebral compressive deformity (VCD)/VCF. A qualitative VCD with <20%, 20–25%, 25–40%, and >40% vertebral body height loss was recorded as minimal, mild, moderate, and severe grades, respectively. A VCD coexisted with endplate/cortex fracture (ECF) was VCF. FB readings were considered as the reference.
Results
There were 34 true negative cases where FA and FB had a consensus. In 7 cases with minimal VCD, 3 cases with ECF, and 7 cases with minimal or mild VCFs, the FA readings were false negative. No standalone singular moderate or severe VCD/VCF in a patient was missed in FA's reports. In 25 FA reading positive cases with multiple VCFs, one VCF was missed in 8 cases, more than one VCF was missed in 15 cases, and one additional ECF was missed in 2 cases. In 14 cases, FA and FB had VCF number agreement, with the term ‘vertebral fracture’ was used appropriately in FA reports. In 15 cases, FA and FB had agreement in VCF number; however, the appropriate term ‘vertebral fracture’ was not used in FA reports; instead the terms of ‘compressive change’ or ‘wedging change’ were used. In most VCFs, severity grading was not given in FA. In 13 VCFs where grading was reported, all were marked as ‘mild’, including seven mild VCFs, five moderate VCFs, and even one severe VCF.
Conclusion
Among the patients with VCD/VCF, the false negative rate among was 23.9% (17/71), but the missed cases were all minimal or mild grades. One or more VCFs were missed in 32.4% (23/71) of the cases with multiple VCFs. Appropriate severity grading was not reported for most cases.
The translational potential of this article
The underreporting rate of osteoporotic vertebral compressive fracture in back pain clinic patients in a typical tertiary hospital setting in China compared favorably with literature reports. However, there is a general lack of awareness of vertebral endplate/cortex fracture sign and vertebral fracture severity grading, while minimal and mild VCD with endplate/cortex fracture may have clinical significance. Moreover, after one VCF is spotted in a patient, it is highly advisable to carefully check the whole spine so that multiple VCFs will not be missed.
Keywords: Osteoporosis, Radiographic diagnosis, Underreporting, Vertebral fractures, X-ray
Introduction
Osteoporosis is characterized by low bone mass and micro-architectural deterioration, which leads to bone fragility and consequent increase in fracture risk. Vertebral compressive fracture (VCF) is the most common osteoporotic fracture. A VCF, after minor trauma, is a hallmark of osteoporosis. Prevalent VCFs increase the risk of future vertebral and non-vertebral osteoporotic fractures independent of bone mineral density (BMD) [[1], [2], [3]]. The presence of a VCF increases the relative risk of future VCF by 4.4-fold and the risk of hip fracture by twofold [4]. VCFs are associated with poor life quality, impaired bending and rising, difficulties in the activities of daily living, frailty, higher risk of hospitalization, and higher mortality [[4], [5], [6], [7]]. Appropriate interventions for VCF can reduce the occurrence of hip fractures, preventing further VCF, reducing pain and related disabilities [1,8,9], It is important to identify and report VCF accurately and clearly, so that appropriate investigation and treatment can be instigated.
In clinical practice, osteoporotic vertebral fracture (VCF) remains under-recognized and undertreated [[10], [11], [12], [13], [14], [15], [16], [17], [18]]. For example, VCFs are often unrecognized on chest X-rays, especially when the X-rays were not primarily ordered for skeletal conditions. In one study, a review of 100 frontal and lateral view chest X-rays of patients aged ≥60 years in the emergency department of a tertiary hospital in the United States revealed a 22% prevalence of moderate-to-severe VCFs, and 45% of them were unrecognized [11]. Moreover, a follow-up of 500 patients aged ≥60 years who had frontal and lateral view chest X-rays in an emergency department in the United States showed that one-sixth of the patients had moderate-to-severe VCFs, but only 43% of the cases were reported, and only 25% of the cases were clinically diagnosed or treated [12]. Recent reports show that similar underreporting exists in China [[15], [16], [17]]. In a retrospective study, Yu et al. [15] reported that, of 1638 hospitalized patients aged 50 years and older, 64% of patients with vertebral fractures (inclusive of mild VCF) found on routine frontal and lateral view chest X-rays were undiagnosed in the original radiology reports. In an analysis of lateral chest X-ray of 3216 female patients 50 years of age and older, Li et al. [16] reported that 66.8% of patients with severe or moderate vertebral fractures were undiagnosed in the original radiology reports.
Despite this issue of underreporting of VCF is a known fact, it was shown that the situation has not improved in the last 10 years [18]. This underreporting can be due to a lack of awareness by radiologists of clinical implications of incidental VCFs, and also some radiologists tend to focus their report only on the clinical indication of the X-ray exam, and thus tend to not perform an accurate analysis of the spine while reading chest X-rays when the clinical indication is pulmonary or heart diseases. In this study, we looked at this issue from a different angle. We studied that, for patients with suspected spine pathologies, and when radiologists did pay attention to the spine, whether VCFs are properly recognized and reported in a typical tertiary hospital setting in China.
Materials and methods
This is a retrospective analysis with the 107 cases of The Second Hospital of Wenzhou Medical University, China (facility A, FA), which is a tertiary academic hospital with a good reputation for spine care. The institutional ethics committee approved this study, and the informed consent was waivered. These patients were referred, from 1 January 2017 to 31 March 2018, to the Department of Radiology for X-ray examination of the spine. Both lateral and frontal X-rays were obtained. All included cases were female aged ≥55 years, and therefore were all high-risk subjects for VCF. Patients with notable recent trauma history or spine surgery were excluded. The referring departments included the general orthopedics department, spine surgery department, pain department, rheumatology department, and endocrinology department. The main complaints of the patients included thoracic/upper back pain, lower back pain, and/or leg pain. The purpose of the spine X-ray examination was to see whether vertebral fracture, spine tumor, infection/inflammation, spine scoliosis, or spondylolisthesis existed. To evaluate VCF, the recommendation was to screen the T4-L4 vertebrae. For the clinical cases in this study, the X-ray was targeted toward the region with pain, and the lower L-spine was not filmed in 11 cases. However, in all cases, the VCF high-risk region of the middle thoracic spine and thoracolumbar junctions were included.
The images were transferred to a central reading facility (facility B, FB) at the Department of Imaging and Interventional Radiology, The Chinese University of Hong Kong, Hong Kong SAR, in DICOM format for reassessment. In FB, all X-rays were initially read by a trained radiographer and then read again by a radiologist. When there was an initial disagreement, the consensus was reached. Both readers at facility B were experienced in reading osteoporotic vertebral compressive deformity and/or fracture (VCD/VCF) and were blinded to the radiological reports from reading FA during image interpretation. All vertebrae demonstrated on the radiograph were read, primarily on the lateral view, and frontal views were also used for supplementary information. The reading was performed with the consideration of the Genant's semi-quantitative (SQ) method [19,20], the Wang's modified SQ method (mSQ) [21], and endplate and/or cortex fracture (ECF) [[22], [23], [24]]. Congenital or acquired non-osteoporotic vertebral deformities, which may mimic VCD in appearances, were systematically excluded [19,23]; thus, VCD/VCF was considered after excluding other potential causes. A definite VCD with <20% vertebral body (VB) height loss was recorded as minimal grade VCD. A VCD with 20–25% VB height loss was recorded as a mild grade, 25–40% as a moderate grade, and >40% as severe grade [19,21]. The diagnosis of VCD was qualitative; whereas, for severity grading, a measurement was taken to evaluate percentage VB height loss. ECF was noted only when it was unambiguous. A VCD vertebra without ECF is recorded as VCD. When VCD coexisted with ECF, the vertebra is recorded to have VCF. It has been noted that, in elderly females, VCD with >34% height loss is always associated with radiographically identifiable ECF [25,26]. ECF was particularly carefully assessed with the spine considered to be without VCD. However, when multiple VCFs (i.e., ≥2 definite VCF) exist, ECF was no longer summarized; as in these cases, identifying more ECF might not further change the clinical management approach.
The radiological reports from FA and the assessment results from FB were compared, with the latter considered as the reference. Comparing the reporting radiologists at FA, the readers at FB had the following advantages: (1) they were well aware of the clinical relevance of reporting VCD/VCF; (2) they had experience in VCD/VCF evaluation and grading; (3) probably they spent more time reading the images.
Results
There were two cases with substantial scoliosis, and, according to FB, proper assessment of VCD/VCF was not permitted. However, in one case, it was strongly suspected that at least one moderate grade VCD existed, but VCD was not noted in the FA reporting. Thus, in total, 105 patients were included in this study.
There were 34 true negative cases (34/105, 32.3%), whether both FA reading and FB reading had a consensus that there was no VCD/VCF.
Seventy-one cases had positive VCD/VCF reading at FB. Six cases of minimal VCDs and one case of mild VCD (9.8%, 7/71) were missed (Figure 1). In three cases, definite endplate fracture was missed (4.2%, 3/71). Taking together, all endplate fracture only and minimal VCD only cases were missed. In seven cases with VCF (9.8%), the report was false negative (Figure 2, Figure 3, Figure 4). All these seven cases were of minimal/mild VB height loss but with positive ECF signs. The total false negative rate was 16.2% for all cases (17/105) or 23.9% for VCD/VCF positive cases (17/71). However, no standalone singular moderate or severe VCD/VCF in a patient was missed in FA's reports.
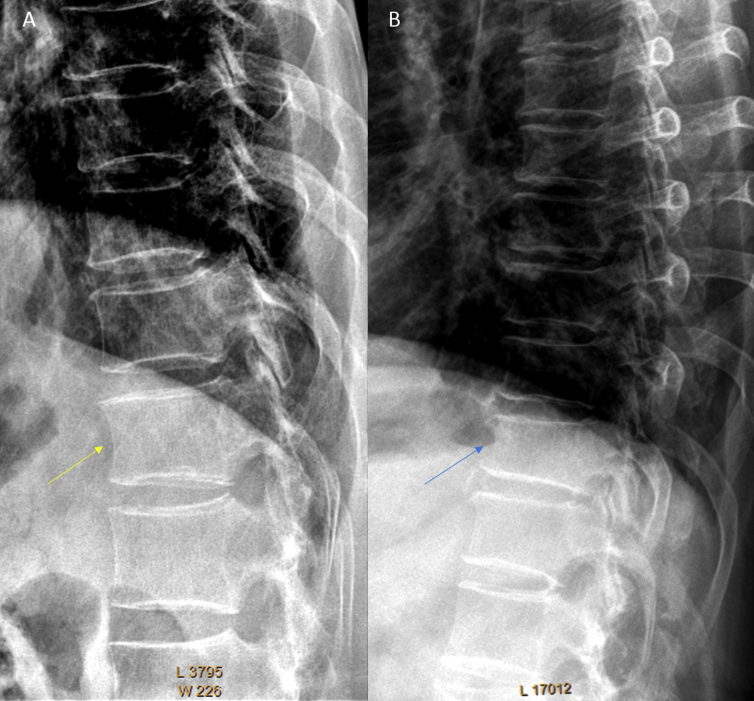
Figure 1.
Two cases of minimal/mild vertebral compressive deformity (VCD) missed in the reports of facility A. A: arrow indicates a minimal VCD in T12; B: arrow indicates a mild VCD in T11.
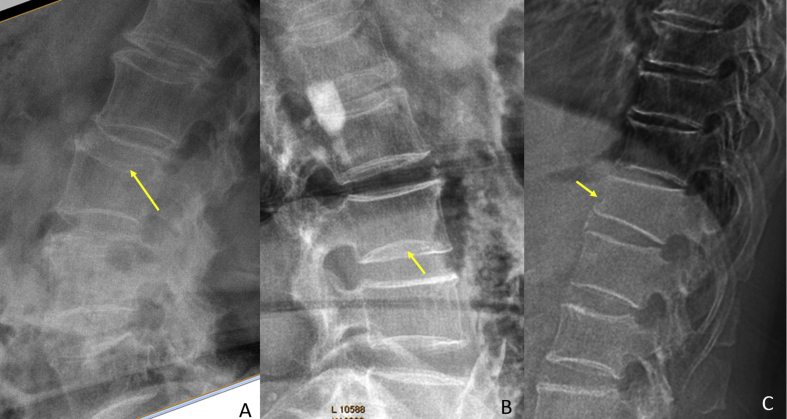
Figure 2.
Three cases of VCF with false negative report. A: a L2 VCF with middle height loss and upper endplate fracture (arrow); B: a case of standalone L3 lower endplate fracture (arrow) without apparent vertebral height loss; C: T12 mild wedged deformity and anterior cortex buckling (arrow).
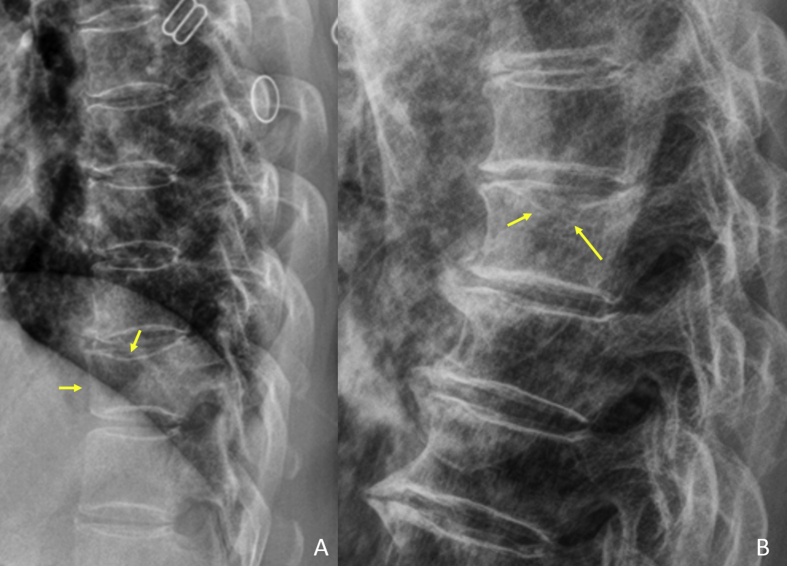
Figure 3.
Two cases of VCF with false negative report. A: T11 mild deformity and upper endplate fracture (arrows); B: T7 mild deformity and upper endplate fracture (arrows).
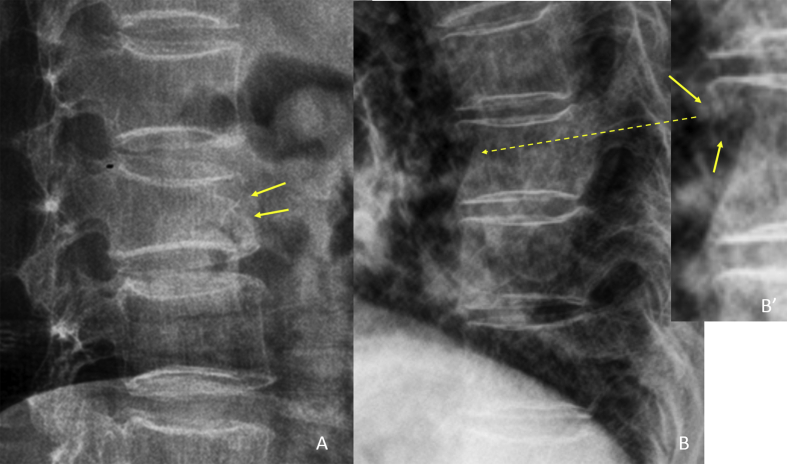
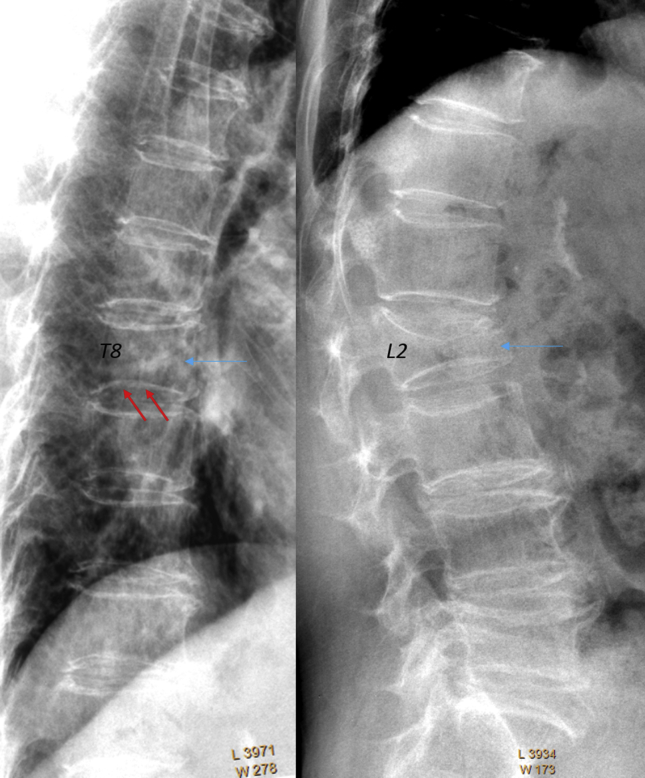
Figure 4.
Two cases of VCF with false negative report. A: L2 deformity with anterior cortex fracture; B: T8 fracture with its anterior cortex disrupted. B′ is the enlarged image of T8 anterior cortex showing disruption (arrows).
In eight FA-reported positive cases with multiple VCFs, one VCF was missed in reporting (Figure 5). The missed VCFs were of four mild grade severity and four moderate grade severity. According to FB's reading, with these 8 cases, 4, 1, 1, and 2 cases had 2, 3, or 5 VBs involvement, respectively.
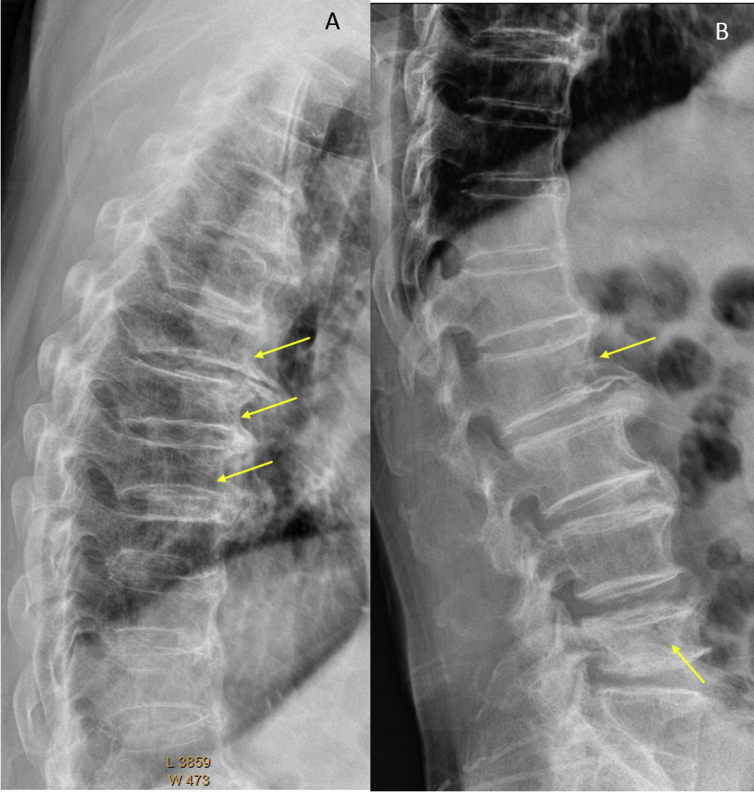
Figure 5.
A case with two VCFs. In addition to severe L2 VCF, there is a minimal VCF with lower endplate fracture at T8 which was missed in the radiological report. The lower endplate fracture of T8 can be noted by comparing the lower endplates of T7, T8, and T9, with the lower endplate of T8 showing a depression.
In 15 FA-reported positive cases with multiple VCFs, more than one VCF was missed in reporting (Figure 6). According to FB's reading, in these 15 cases, the mean VCF number was 6 (range: 3–10 vertebrae) per subject, and the mean missed VCFs were 3.8 (range: 2–8 vertebrae) per subject.
Figure 6.
A case of multiple VCFs. Only L4 ‘compressive change’ was reported, while T6, T7, T8, and L1 VCFs were missed in the radiological report.
In one case with three severe VCFs, one additional vertebra with ECF was missed. In one case with one moderate VCF and one severe VCF, two additional vertebrae with ECF were missed.
In 14 cases, with one VCF per subject for eight cases, and two VCFs for per subject for six cases, the FA report and FB reading had agreement in VCF number. The term ‘vertebral fracture’ was used in the radiological reports.
In 15 cases with VCF, FA report and FB reading had agreement in VCF number; however, the term ‘vertebral fracture’ was not used in the radiological reports. Instead, the terms of ‘vertebral compressive change’ or ‘vertebral wedging change’ were used. In this group, 10 cases, 3 cases, and 1 case had 1 VB, 2 VBs, and 3 VBs involvement, respectively. One case had 9 VBs involvement, and this subject was reported to have ‘multiple vertebral compressive changes’. In one case, a T8 VCF was mislabeled as a T7 VCF.
In most cases, severity grading was not given. For 13 VCFs where grading was reported, all were marked as ‘mild’, including seven mild VCFs, five moderate VCFs, and one severe VCF.
Discussion
Prevention of further new fracture is of paramount importance for patients with existing VCF. Fragility VCF is one of the indications for the initiation of anti-osteoporosis drug therapy. Several drug therapies have proved to reduce the risk of future fracture risk [8,9,27]. Osteoporosis pharmacotherapy should be strongly considered for patients with an osteoporotic VCF of more recent, higher grade, or multiple fractures. The early detection of a VCF can lead to further investigation and appropriate therapy that decreases the risk of future fractures. Many patients with VCF do not have BMD T-scores in the osteoporotic range and would not be selected for pharmacological therapy based on BMD scores alone [2,28,29]. This reflects alterations in the micro–macro architecture that are not captured by dual-energy X-ray absorptiometry (DXA) measurement.
Recent reports emphasize the importance of identifying osteoporotic ECF [or ABQ fracture as defined by Jiang et al. [22]. In the MsOS (Hong Kong) study, it was shown that, compared with vertebrae without Genant SQ-VCD, ECF(−) mild and moderate VCDs did not have a higher short-term (4 years) future risk for new incident VCD; however, these vertebrae with deformity had a higher risk of short-term future turning to ECF(+) [26]. Within the same mild/moderate VCD grades, compared with the subjects without ECF, the subjects with ECF are associated with a higher short-term future risk of VCD progression and new incident VCD. Although mild VCDs may not have immediate fragility fracture consequence, they may be a risk factor further developing ECF, thus indicating that they are a biomarker of compromised bone quality [26]. It is known that VCD/VCF does not necessarily have a height loss. Wang [21] proposed that vertebrae can be radiographically classified into the following: (1) grade 0: without VCD, without ECF; (2) mild VCD: qualitative VCD and VB height loss <20%, mild VCF: mild VCD together with ECF; (3) moderate VCD: VCD with 20–34% VB height loss, moderate VCF: moderate VCD together with ECF; (4) severe VCF: >34% vertebral height loss, always with ECF. Thus, it is less than 1/5 VB height loss being mild grade and more than 1/3 VB height loss being severe grade, and those in-between being moderate grade [21]. In this study, we adopted a compromise of Genant's SQ criteria, Jiang et al.'s ABQ criteria, and Wang's mSQ criteria. ECF sign was checked, and VCD was classified into four categories, thus that mSQ's mild VCD would be minimal VCD in this study, the criteria for Genant SQ's mild, moderate, and severe grades' height loss were kept unchanged, and those with ECF were recorded as VCF while those without ECF were recorded as VCD. This approach would potentially allow our results to be compared with historical results used as Genant's SQ criteria. It has to be noted that, while SQ's mild grade was initially described to require a 20–25% height loss, in real practice, VCDs with less than 20% height loss were also commonly graded as Genant SQ grade 1. These examples can be seen in both Genant's 1993 original paper (Fig. 2A of reference 19, mild VCD with less than 20% height loss) and international osteoporosis foundation’s teaching materials (slide 14 at https://www.iofbonehealth.org/what-we-do/training-and-education/educational-slide-kits/vertebral-fracture-teaching-program, accessed on May 31, 2019). Therefore, some previously reported SQ mild VCD would be actually minimal VCDs with the criteria in this study. The Scientific Advisory Council of Osteoporosis Canada and the Canadian Association of Radiologists suggested that it is to patients' benefit that radiologists report all VCDs evident on radiograph, particularly for VDs occurring at the typical location of VCF, such as at T11-L2 levels, and for females [30]. BMD testing should be considered if a VCD/VCF is found without the diagnosis of osteoporosis having already been confirmed. For acute patients with acute pain, it should be also noted that VB with VCF may appear only as minimal deformity or to be ‘normal’ during initial X-ray [31]. In these cases, reporting minimal VCD deformity may alert further investigations such as fat-suppressed T2-weighted magnetic resonance (MR) imaging [23,32]. If patients' results of other tests (e.g., BMD) do not warrant antiresorptive therapy, it would be advisable to consider them to be at high risk of fracture and further tests should be carried out again in 1–2 years.
With the data from a tertiary academic hospital in China, this study shows the radiological report for back pain clinic patients for whom the spine was the focus of interest, had a false negative rate of 10% for minimal or mild VCF, 4.3% for ECF, and 10% for minimal VCD, which compared favorably with other similar reports [10,33]. This also contrasts with previous publications that >40% of the moderate/severe VCDs/VCF were missed in the report when the focus was not spine such as the chest X-rays when indicated for pulmonary or heart pathologies [[11], [12], [13], [14], [15], [16], [17]]. However, this study shows that several aspects should also be improved with FA's reporting. In addition to the false negative reporting, the first is that VCD/VCF severity was not provided for most cases. Moreover, five moderate VCFs and even one severe VCF were wrongly labelled as ‘mild’. Actually, when the grading was given in the reports, it was always ‘mild’. The awareness of the existing grading schemes can be improved for the reporting radiologists. It is known that the greater the severity of prevalent VCFs, the greater the risk of future fractures [30,33,34]. The precise reporting of the grading, particularly being moderate/severe, is likely to capture the attention of referring physicians.
Of the 71 VCD/VCF positive cases, 56.7% [(17 + 23)/71] of the cases had one or more VCFs missed in the report. This was more common when multiple VCFs (n = 23) existed. It is known that the greater the number of prevalent VCFs, the greater the risk of future fractures [26,33,34]. Patients with two or more previous fragility fractures should be considered as affected by severe osteoporosis, regardless of BMD values, particularly if the vertebral deformities are moderate or severe [2].
In most of the FA reports, the specific term of vertebral fracture was not used. Instead, the vague terms of ‘vertebral wedging change’ or ‘vertebral compressive change’ were used. When the diagnose is clear, the more firm term ‘vertebral fracture’ should be favored to alert the referring physician [10]. Theoretically, ‘vertebral wedging’ can be aging-related, degenerative, or osteoporotic VCD-related; whereas, ‘vertebral compressive changes’ are likely to be interpreted as ‘compressive deformity’ (i.e., VCD). It is possible that, for many cases, the reporting radiologists might not feel conformable to using the term ‘fracture’ when what he/she saw a VCD. In these cases, to look for ECF signs may help. A definite ECF sign can lead to the diagnosis of VCF. As noted, no ECF was reported in this study series, and the reporting radiologists might be relatively unfamiliar with the ECF concept. The recently published educational materials may help in this aspect [23,24]. After excluding the known physiological congenital and congenital changes, these VCD/VCFs are by far most likely to be caused by osteoporosis, and the radiologist may report ‘VCD/VCFs, suggestive of osteoporotic nature’. In the end, osteoporotic VCD/VCF should be a clinical diagnosis after considering all contributing factors.
There are a few limitations to this study. We used the conventional radiographic technique for obtaining spine X-ray, and in a number of cases, the lower lumbar vertebrae were not included. X-ray cone beam may cause geometric distortion of vertebrae located at extremities of the scans, and therefore the accuracy of the diagnosis of VCFs could be reduced at the upper thoracic and lower lumbar levels. A complete medical record review was not performed so that whether or not osteoporosis was diagnosed and treated by the referring clinicians remained unclear. There was no golden standard for minimal and mild VCD, and the reading results at FB were used as the reference. Standalone minimal and mild VCD may, or may not be, clinically significant at an individual patient's level [35,36]. Additional tests or X-ray follow-up may be considered for these cases. These data were from elderly females. It is known that VCDs/VCFs of elderly men and elderly women have distinctly different features [[37], [38], [39]]. For example, mild VCD is more likely to be associated with ECF in females than in males [37], and minimal and mild VDs in males are of less clinical relevance [21,40,41]. How the results of this study can be applied in elderly males remains unknown. Moreover, it should be noted that though the patients in this study were referred for spine X-ray because of back/leg pain, the actual cause of the back/leg pain would be difficult to ascertain [42]. In fact, 3/4 of the elderly females with osteoporotic VCF may not have back pain [43].
In conclusion, 105 cases of spine X-rays acquired at the back pain clinic patients of a tertiary Chinese hospital in China were reassessed at a central reading facility. Among the patients with positive VCD/VCF findings, the false negative cases included 10% for minimal or mild grade VCFs, 4.3% for standalone ECFs, and 10% for minimal VCDs. One or more VCFs were missed in 32.4% (23/71) of the FA-reported positive cases with multiple VCFs. Of particular concern is that appropriate grading was not reported for most cases. As the clinical management can be facilitated by precise reporting as to the grade of VCD/VCF and the segmental level or levels involved, radiologists should be trained and sensitized in VCD/VCFs identification; thus, by precise VCD/VCF reporting, radiologist can play an important role in the clinical care of patients with osteoporosis [44, 45].
Conflict of interest
The authors have no conflicts of interest to disclose in relation to this article.
Funding/support
The authors have no acknowledgements to disclose and they received no funding for the work described in this article.
Acknowledgements
We thank Dr Daniele Diacinti and Dr Yebin Jiang for advice in checking cases with minimal vertebral compressive deformity.
Contributor Information
Zhi-Han Yan, Email: yanzhihanwz@163.com.
Yi Xiang J. Wang, Email: yixiang_wang@cuhk.edu.hk.
References
- 1.Black D.M., Cummings S.R., Karpf D.B., Cauley J.A., Thompson D.E., Nevitt M.C. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 2.Nuti R., Brandi M.L., Isaia G., Tarantino U., Silvestri S., Adami S. New perspectives on the definition and the management of severe osteoporosis: the patient with two or more fragility fractures. J Endocrinol Investig. 2009;32:783–788. doi: 10.1007/BF03346537. [DOI] [PubMed] [Google Scholar]
- 3.Jager P.L., Jonkman S., Koolhaas W., Stiekema A., Wolffenbuttel B.H., Slart R.H. Combined vertebral fracture assessment and bone mineral density measurement: a new standard in the diagnosis of osteoporosis in academic populations. Osteoporos Int. 2011;22:1059–1068. doi: 10.1007/s00198-010-1293-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klotzbuecher C.M., Ross P.D., Landsman P.B., Abbott T.A., 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 5.Kendler D.L., Bauer D.C., Davison K.S., Dian L., Hanley D.A., Harris S.T. Vertebral fractures: clinical importance and management. Am J Med. 2016;129 doi: 10.1016/j.amjmed.2015.09.020. 221.e1-10. [DOI] [PubMed] [Google Scholar]
- 6.Kanis J.A., Oden A., Johnell O., De Laet C., Jonsson B. Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int. 2004;15:108–112. doi: 10.1007/s00198-003-1516-y. [DOI] [PubMed] [Google Scholar]
- 7.Wang Y.X. Senile osteoporosis is associated with disc degeneration. Quant Imaging Med Surg. 2018;8:551–556. doi: 10.21037/qims.2018.07.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wells G.A., Cranney A., Peterson J., Boucher M., Shea B., Robinson V. Etidronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008:CD003376. doi: 10.1002/14651858.CD003376.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells G.A., Cranney A., Peterson J., Boucher M., Shea B., Robinson V. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008:CD001155. doi: 10.1002/14651858.CD001155.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Delmas P.D., van de Langerijt L., Watts N.B., Eastell R., Genant H., Grauer A. IMPACT Study Group. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005;20(4):557–563. doi: 10.1359/JBMR.041214. [DOI] [PubMed] [Google Scholar]
- 11.Kim N., Rowe B.H., Raymond G., Jen H., Colman I., Jackson S.A. Underreporting of vertebral fractures on routine chest radiography. Am J Roentgenol. 2004;182:297–300. doi: 10.2214/ajr.182.2.1820297. [DOI] [PubMed] [Google Scholar]
- 12.Majumdar S.R., Kim N., Colman I., Chahal A.M., Raymond G., Jen H. Incidental vertebral fractures discovered with chest radiography in the emergency department. Arch Intern Med. 2005;165:905–909. doi: 10.1001/archinte.165.8.905. [DOI] [PubMed] [Google Scholar]
- 13.Lansdown D., Bennet B., Thiel S., Ahmed O., Dixon L., Vokes T.J. Prevalence of vertebral fractures on chest radiographs of elderly African American and Caucasian women. Osteoporos Int. 2011;22:2365–2371. doi: 10.1007/s00198-010-1452-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gehlbach S.H., Bigelow C., Heimisdottir M., May S., Walker M., Kirkwood JR. Recognition of vertebral fracture in a clinical setting. Osteoporos Int. 2000;11:577–582. doi: 10.1007/s001980070078. [DOI] [PubMed] [Google Scholar]
- 15.Yu W., Yao J.P., Lin Q., Mou W.B. Cause analysis of missing diagnosis for vertebral fracture on lateral chest radiography. Chin J Radiol. 2010;44:504–507. [Google Scholar]
- 16.Li Y., Yan L., Cai S., Wang P., Zhuang H., Yu H. The prevalence and under-diagnosis of vertebral fractures on chest radiograph. BMC Muscoskelet Disord. 2018;19:235. doi: 10.1186/s12891-018-2171-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang H.T., Chen C.K., Chen C.W., Lin M.H., Peng L.N., Chang C.Y. Unrecognized vertebral body fractures (VBFs) in chest radiographic reports in Taiwan: a hospital-based study. Arch Gerontol Geriatr. 2012;55:301–304. doi: 10.1016/j.archger.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 18.Bartalena T., Rinaldi M.F., Modolon C., Braccaioli L., Sverzellati N., Rossi G. Incidental vertebral compression fractures in imaging studies: lessons not learned by radiologists. World J Radiol. 2010;2:399–404. doi: 10.4329/wjr.v2.i10.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Genant H.K., Wu C.Y., van Kuijk C., Nevitt M.C. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137–1148. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 20.Genant H.K., Jergas M. Assessment of prevalent and incident vertebral fractures in osteoporosis research. Osteoporos Int. 2003;14(Suppl 3):S43–S55. doi: 10.1007/s00198-002-1348-1. [DOI] [PubMed] [Google Scholar]
- 21.Wang Y.X. A modified semi-quantitative (mSQ) grading scheme for osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg. 2019;9:146–150. doi: 10.21037/qims.2019.02.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang G., Eastell R., Barrington N.A., Ferrar L. Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int. 2004;15:887–896. doi: 10.1007/s00198-004-1626-1. [DOI] [PubMed] [Google Scholar]
- 23.Wang Y.X., Santiago R.F., Deng M., Nogueira-Barbosa M.H. Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg. 2017;7:555–591. doi: 10.21037/qims.2017.10.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y.X., Deng M., He L.C., Che-Nordin M.N., Santiago R.F. Osteoporotic vertebral endplate and cortex fractures: a pictorial review. J Orthop Translat. 2018;15:35–49. doi: 10.1016/j.jot.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deng M., Kwok T.C.Y., Leung J.C.S., Leung P.C., Wáng Y.X. All osteoporotically deformed vertebrae with >34% height loss have radiographically identifiable endplate/cortex fracture. J Orthop Translat. 2018;14:63–66. doi: 10.1016/j.jot.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Y.X., Che-Nordin N., Deng M., Leung J.C., Kwok A.W.L., He L.C. Osteoporotic vertebral deformity with endplate/cortex fracture is associated with higher further vertebral fracture risk: the Ms. OS (Hong Kong) study results. Osteoporos Int. 2019;30:897–905. doi: 10.1007/s00198-019-04856-4. [DOI] [PubMed] [Google Scholar]
- 27.Harvey N.C.W., McCloskey E.V., Mitchell P.J., Dawson-Hughes B., Pierroz D.D., Reginster J.Y. Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int. 2017;28:1507–1529. doi: 10.1007/s00198-016-3894-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schuit S.C., van der Klift M., Weel A.E., de Laet C.E., Burger H., Seeman E. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone. 2004;34:195–202. doi: 10.1016/j.bone.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 29.Wainwright S.A., Marshall L.M., Ensrud K.E., Cauley J.A., Black D.M., Hillier T.A. Hip fracture in women without osteoporosis. J Clin Endocrinol Metab. 2005;90:2787–2793. doi: 10.1210/jc.2004-1568. [DOI] [PubMed] [Google Scholar]
- 30.Lentle B.C., Brown J.P., Khan A., Leslie W.D., Levesque J., Lyons D.J. Scientific Advisory Council of Osteoporosis Canada; Canadian Association of Radiologists. Recognizing and reporting vertebral fractures: reducing the risk of future osteoporotic fractures. Can Assoc Radiol J. 2007;58:27–36. [PubMed] [Google Scholar]
- 31.Pham T., Azulay-Parrado J., Champsaur P., Chagnaud C., Legre V., Lafforgue P. “Occult” osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine. 2005;30:2430–2435. doi: 10.1097/01.brs.0000184303.86932.77. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 32.Diacinti D., Guglielmi G. How to define an osteoporotic vertebral fracture? Quant Imaging Med Surg. 2019;9:1485–1494. doi: 10.21037/qims.2019.09.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Diacinti D., Vitali C., Gussoni G., Pisani D., Sinigaglia L., Bianchi G. Research Department of FADOI. Misdiagnosis of vertebral fractures on local radiographic readings of the multicentre POINT (Prevalence of Osteoporosis in INTernal medicine) study. Bone. 2017;101:230–235. doi: 10.1016/j.bone.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 34.Delmas P.D., Genant H.K., Crans G.G., Stock J.L., Wong M. Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone. 2003;33:522–532. doi: 10.1016/s8756-3282(03)00241-2. [DOI] [PubMed] [Google Scholar]
- 35.Wang Y.X., Che-Nordin N. Informed communication with study subjects of radiographically detected osteoporotic vertebral deformity. Quant Imaging Med Surg. 2018;8:876–880. doi: 10.21037/qims.2018.09.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yoshida T., Nanba H., Mimatsu K., Kasai T. Treatment of osteoporotic spinal compression fractures. Conservative therapy and its limitation. Clin Calcium. 2000;10:53–58. [Google Scholar]
- 37.Deng M., Zeng X.J., He L.C., Leung J.C.S., Kwok A.W.L., Griffith J.F. Osteoporotic vertebral fracture prevalence in elderly Chinese men and women: a comparison of endplate/cortex fracture-based and morphometrical deformity-based methods. J Clin Densitom. 2019;22:409–419. doi: 10.1016/j.jocd.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 38.Szulc P., Munoz F., Marchand F., Delmas P.D. Semiquantitative evaluation of prevalent vertebral deformities in men and their relationship with osteoporosis: the MINOS study. Osteoporos Int. 2001;12:302–310. doi: 10.1007/s001980170120. [DOI] [PubMed] [Google Scholar]
- 39.Che-Nordin N., Deng M., Griffith J.F., Leung J.C.S., Kwok A.W.L., Zhu Y.Q. Prevalent osteoporotic vertebral fractures more likely involve the upper endplate than the lower endplate and even more so in males. Ann Transl Med. 2018;6:442. doi: 10.21037/atm.2018.10.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Waterloo S., Søgaard A.J., Ahmed L.A., Damsgård E., Morseth B., Emaus N. Vertebral fractures and self-perceived health in elderly women and men in a population-based cross-sectional study: the Tromsø Study 2007-08. BMC Geriatr. 2013;13:102. doi: 10.1186/1471-2318-13-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Y.X., Che-Nordin N., Deng M., Griffith J.F., Leung J.C.S., Kwok A.W.L. Elderly males with or without existing osteoporotic vertebral fracture have much lower future vertebral fracture risk than elderly females: the MrOS (Hong Kong) year-4 follow-up spine radiograph study. Osteoporos Int. 2019 Sep 2 doi: 10.1007/s00198-019-05136-x. [DOI] [PubMed] [Google Scholar]
- 42.Wang Y.X., Wu A.M., Ruiz Santiago F., Nogueira-Barbosa M.H. Informed appropriate imaging for low back pain management: a narrative review. J Orthop Translat. 2018;15:21–34. doi: 10.1016/j.jot.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fink H.A., Milavetz D.L., Palermo L., Nevitt M.C., Cauley J.A., Genant H.K., Fracture Intervention Trial Research Group What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res. 2005;20:1216–1222. doi: 10.1359/JBMR.050314. [DOI] [PubMed] [Google Scholar]
- 44.Zhang Y., Guo J., Duanmu Y., Zhang C., Zhao W., Wang L. Quantitative analysis of modified functional muscle-bone unit and back muscle density in patients with lumbar vertebral fracture in Chinese elderly men: a case-control study. Aging Clin Exp Res. 2019;31:637–644. doi: 10.1007/s40520-018-1024-8. [DOI] [PubMed] [Google Scholar]
- 45.Guglielmi G., Balzano R.F., Cheng X. What is changed in the diagnosis of osteoporosis: the role of radiologists. Quant Imaging Med Surg. 2018;8:1–4. doi: 10.21037/qims.2018.02.04. [DOI] [PMC free article] [PubMed] [Google Scholar]