Abstract
Background
Alveolar bone loss can occur as a result of aggressive maneuvering due to iatrogenic trauma during teeth extraction or due to normal post-extraction socket healing. Tooth if used as a whole grafting material then successful osteoconductive remodeling can be expected because low-crystalline apatite is the main minerals in bone tissue. A study was conducted in the department of oral and maxillofacial surgery focused on the potential for osteoconduction, osteoinduction, and osteogenesis by growth factors in the tooth and related histogenesis between the tooth and bone. Radiographic evaluation of alveolar ridge preservation was performed using a 3D imaging technique as well as histologically using Autogenous fresh mineralized tooth graft prepared at the chairside.
Results
A total of 30 patients were included in the study. The data was subjected to statistical analysis and the comparison of quantitative data was done using paired t-test.
Conclusion
The outcome of this study suggests that chair side autogenous tooth graft can be used for socket survival, sinus and ridge augmentation as it is less time consuming, easy to prepare, with lower bone resorption speed, osteoinduction, osteoconduction, osteogenetic properties, and excellent primary implant stability.
Keywords: ATG (Autogenous tooth graft), CBCT (Cone beam computed tomography)
1. Introduction
Various etiologies can accompany tooth loss. Examples of such etiologies are endodontic, periodontic, advanced carious lesions, and facial injuries. Iatrogenic trauma from aggressive maneuvering can result in the alveolar bone loss while removing teeth or normal post-extraction socket healing.1 In many cases, the severity of this pattern of healing can be troublesome for the clinician: an esthetic problem is created in the manufacture of implant-supported restoration or traditional prosthesis, and implant placement is difficult if not impossible. However, to minimize such problems, ridge preservation procedures can be performed in extraction sockets using grafting materials.2 All extracted teeth are currently discarded as they are considered to be a clinical waste. Recently, few studies have been using extracted teeth to fill the same patient's alveolar defects. Cleaning, grinding, demineralization, and sterilization methods were used to treat the extracted teeth. As a resource for alveolar bone regeneration, the tooth is increasingly attracting attention. Tooth as a whole can also be used as a graft material as it contains both inorganic and organic material, and 4 forms of calcium phosphate are present in the key component of the inorganic material.12 Based on the potential for osteoconduction, osteoinduction, and osteogenesis by tooth growth factors and related histogenesis between bone and tooth, this study was conducted in the oral and maxillofacial surgery department to evaluate alveolar ridge preservation radiographically using 3D imaging technique as well as histologically using Autogenous freshly prepared mineralized chair-sided tooth graft. (see Fig. 15)
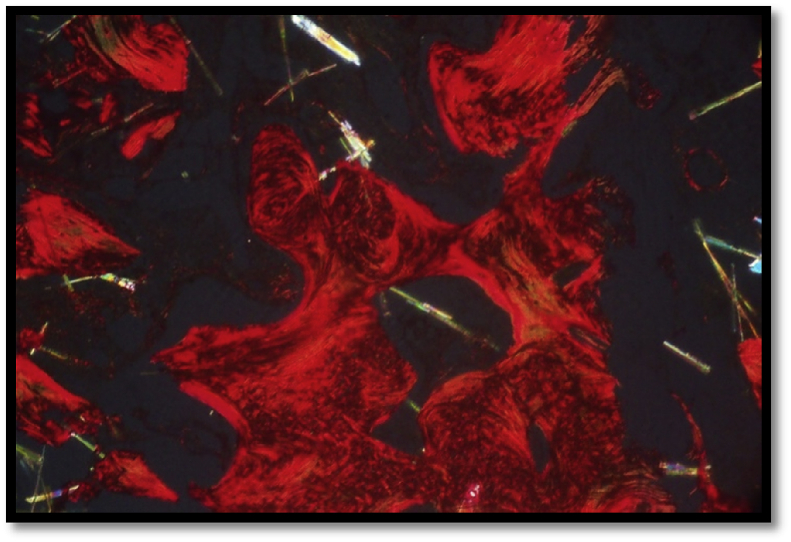
Fig. 15.
Mature lamellar bone showing orange red component under polarizing microscope.
2. Method and materials
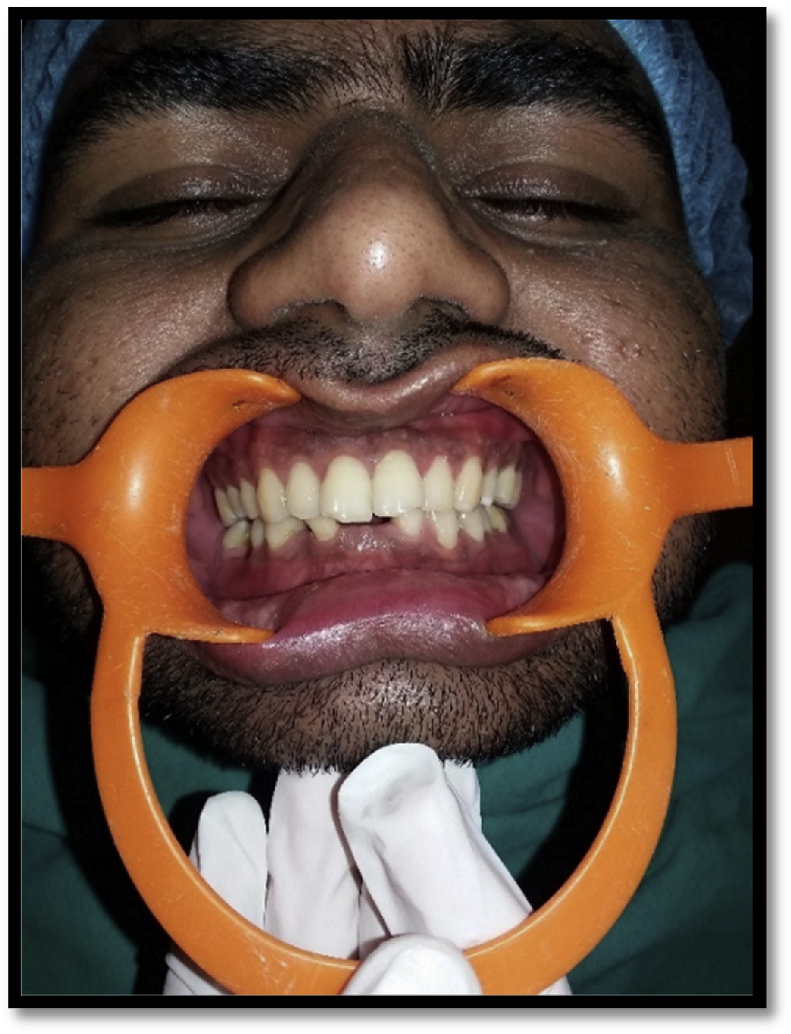
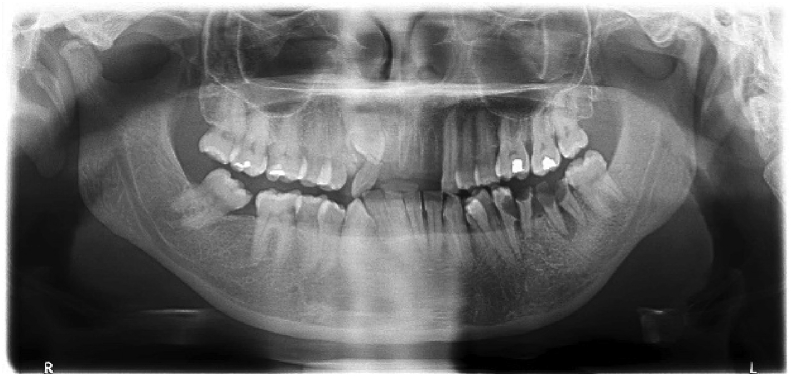
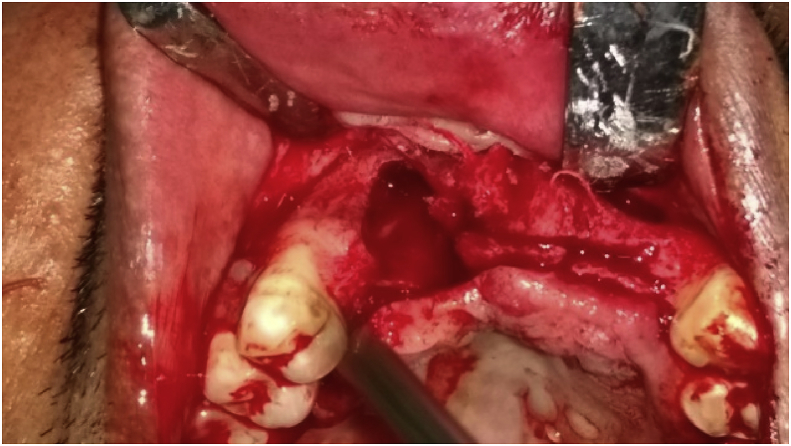
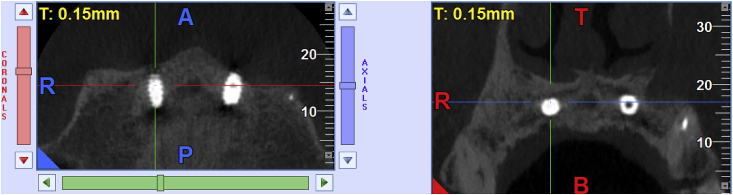
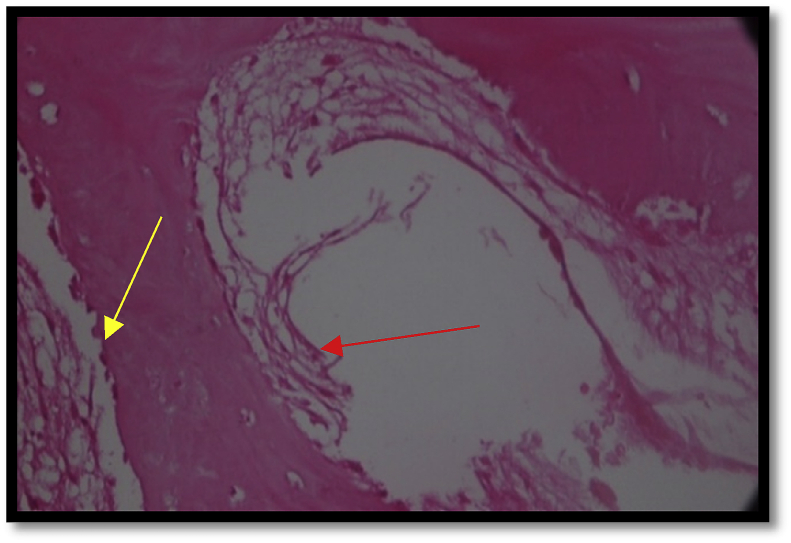
A total of 30 patients were selected on the basis of inclusion and exclusion criteria from the Department of Oral and Maxillofacial Surgery. Of all the selected subjects included in the study, a written informed consent was obtained. Ethical clearance for the study was obtained from the ITS Dental Studies and Research Center's ethical committee, Muradnagar, Ghaziabad, U·P, INDIA. It was a prospective clinical trial in which all patients in the 18-60-year age group, needing tooth extractions (for endodontic or periodontal reasons), able to give informed consent, ASA Class I and Class II patients and patients with sufficient adherence to fulfill the follow-ups were included (Fig. 1, Fig. 2, Fig. 3, Fig. 7, Fig. 8, Fig. 11). Patients more than 60 years of age, patients with severe systemic diseases (rheumatoid arthritis, osteomalacia, osteogenesis imperfecta), Psychiatric disorders, Root canal treated teeth, patients undergoing or who had undergone radiation therapy and chemotherapy to the head & neck region during 12 months, patients with para functional habits, alcoholics, Drug Abusers and heavy smokers were excluded from the study. The following parameters were recorded for each patient included in the study- CBCT evaluation for alveolar bone height before and after 4 months of placing fresh autogenous tooth particulate and histologically assessing new bone remodeling (Fig. 5, Fig. 13). After extractions, the teeth were harvested. The caries was removed using a circular carbide bur, restorations such as crowns or fillings were also removed. The teeth were cleaned dried, sterilized, and powdered after this (Fig. 4, Fig. 9, Fig. 12). The conventional grinder was used for grinding the extracted teeth with a 1500 W engine rating and a 700 rpm speed. Particulate tooth was subsequently submerged in a small glass bottle for 10 min in basic alcohol. The basic alcohol cleanser is used to defat, dissolve all organic debris, bacteria, and tooth particulate toxins as it consists of 0.5 M NaOH and 30% alcohol (v/v). All patients undergo pre and post-operative CBCT scans and follow-up till 3 years. Upon obtaining more informed written consent from the patients, the biopsy was performed in subjects where implant placement was continued for 4 months upon ridge preservation. The bone tissues were harvested with a trephine bur (3 mm in diameter). The harvested bone tissue was sent to the Department of Oral Pathology for histological analysis of new bone formation. The specimens were examined following the involvement of osteocytes in lacunae for semi-quantitative analysis of the bone formation, osteoblastic rimming, and central bone nest. Picro Sirius Red was performed to determine the orientation of collagen fibers under a polarizing microscope special stain (see Fig. 10) (see Fig. 14) (see Fig. 6) (see Fig. 15).
Fig. 1.
Intra-oral pre-operative picture.
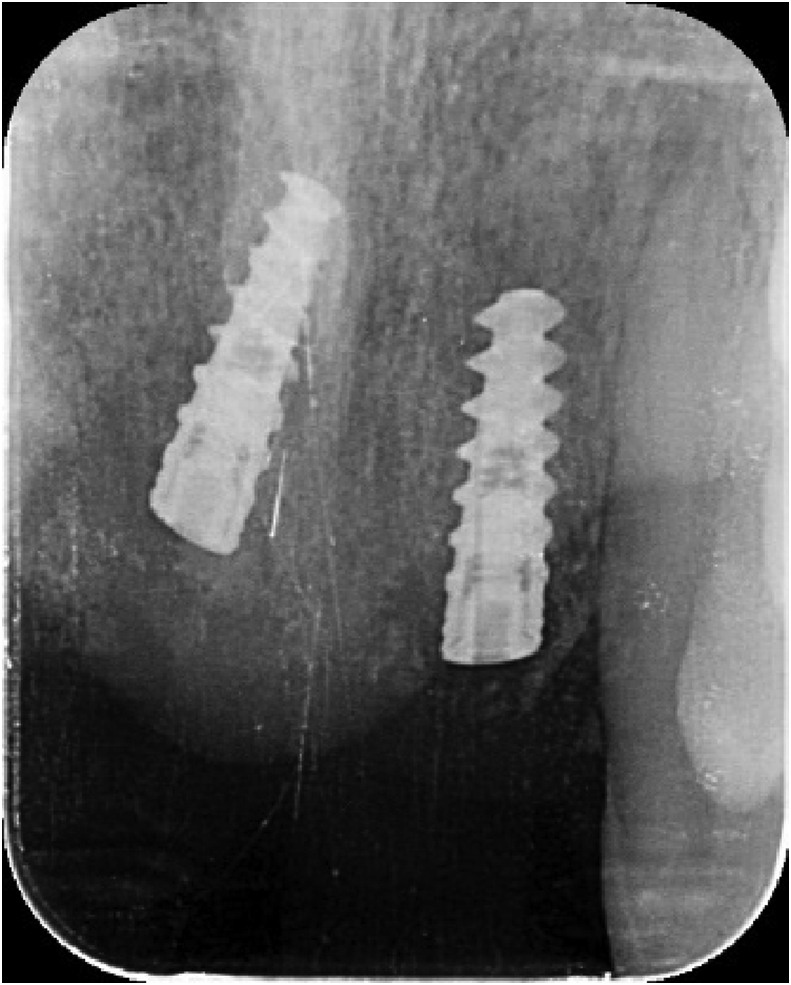
Fig. 2.
IOPA of the same patient showing the impacted canine.
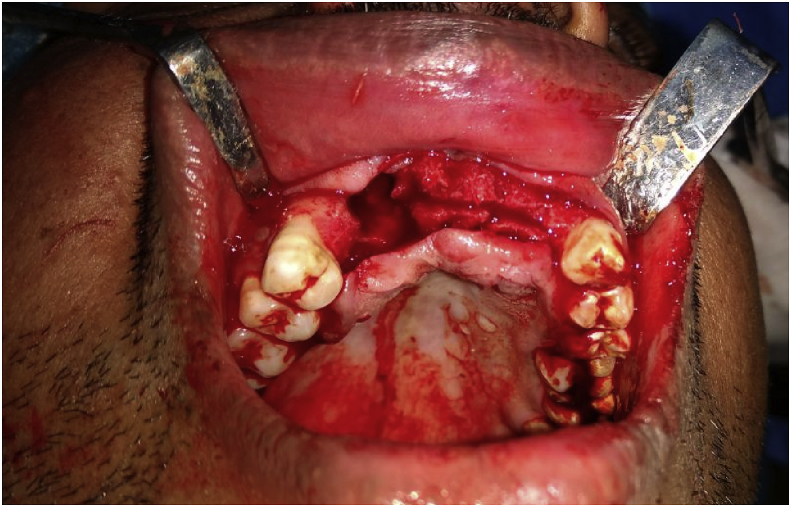
Fig. 3.
Showing the bone defect in the mandibular ridge.
Fig. 7.
OPG of the patient showing missing upper teeth with severe bone loss and impacted 13.
Fig. 8.
Showing the big bone defect in the maxillary arch.
Fig. 11.
IOPA of the patient showing fully oseteointegrated implants with complete bone formation.
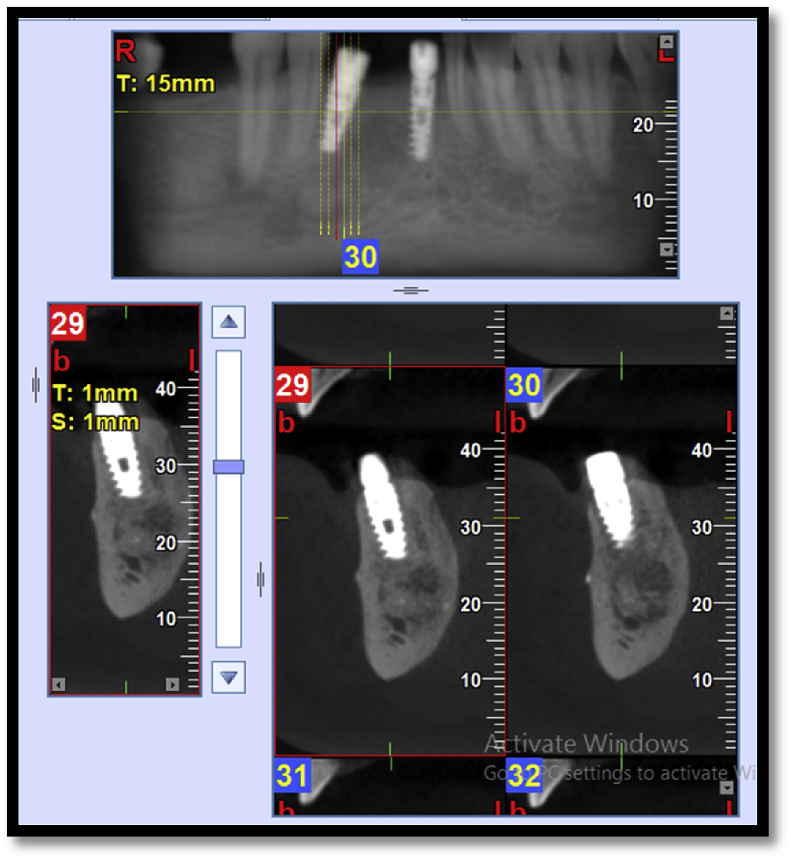
Fig. 5.
Post-operative CBCT scan with bone formation and implant placement at the same site.
Fig. 13.
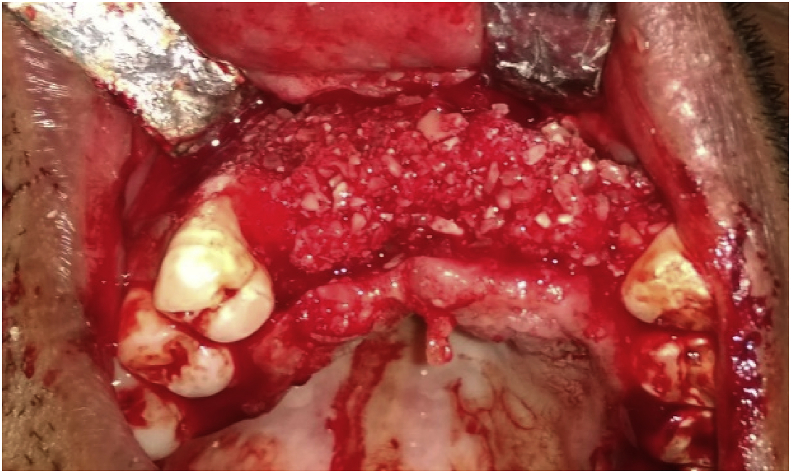
Autogenous bone graft placement.
Fig. 4.
Autogenous tooth graft in the bone defect.
Fig. 9.
Ridge split before graft placement.
Fig. 12.
Showing deficit maxillary arch.
Fig. 10.
Placement of the autogenous tooth graft.
Fig. 14.
Post-operative CBCT scan showing the implants with complete bone formation.
Fig. 6.
Follow up with final prosthesis.
3. Statistical analyses
Changes in ridge width and height measurements are compared using the paired t-test. P < 0.05 was considered significant for all the experiments. All the obtained results were plotted and described (see Fig. 16).
Fig. 16.
Showing osteoblastic rimming (yellow) & Osteocytes (red).
4. Results
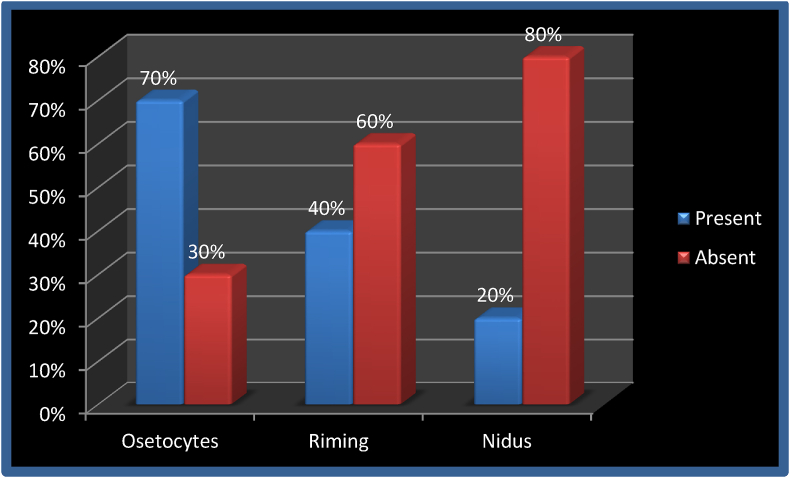
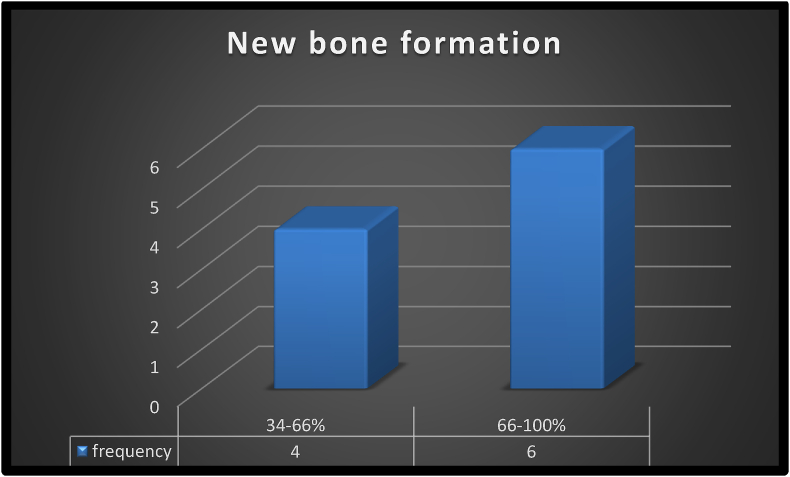
Of the 30 patients, 40% were males and 60% were females. The analysis was completed by all the patients involved. There were 70% cases of the mandibular molar region on-site distribution, 20% of cases of anterior maxillary and 10% of cases of the anterior mandibular region. Comparing the mean alveolar height and alveolar width on pre- and post-operative CBCT scans, statistically significant differences were observed with a p-value of 0.009 and 0.001 respectively (Table 1, Table 2). The histological semi-quantitative analysis revealed 34–66% of new bone formation in 40% of cases, while 67–100% of bone formation in 60% of cases. 80% of patients had collagen fibers in parallel and well-organized form and only interwoven and loosely arranged collagen fibers were present in 20% of patients. 70% of patients showed an osteocyte presence, while only 30% showed osteocyte absence. In the maximum number of patients, i.e. 60% showed no rimming, only 40% showed osteocyte rimming. Twenty percent of patients had nest formation and 80% had no nidus formation. (Graph 1, Graph 2).
Table 1.
Comparison of mean of Alveolar Height and Alveolar Width between two different time intervals by paired t-test.
| Parameter | Mean | Std. Deviation | Std. Error Mean | t | df | P value |
|---|---|---|---|---|---|---|
| Alveolar Height Post (mm.) - Alveolar Height Pre(mm.) | .6000 | .5754 | .1820 | 3.297 | 9 | .009** |
| Alveolar Width Post (mm.) - Alveolar width Pre(mm.) | .6780 | .4205 | .1330 | 5.098 | 9 | .001** |
** Highly significant p < 0.01.
Table 2.
Distribution of mean and standard deviation of Alveolar Height and Alveolar Width at two different time intervals.
| Parameter (N = 30) | Mean | Std. Deviation |
|---|---|---|
| Alveolar Height Post (mm.) | 27.562 | .7626 |
| Alveolar Height Pre(mm.) | 26.962 | .7129 |
| Alveolar Width Post (mm.) | 12.330 | .8795 |
| Alveolar width Pre(mm.) | 11.652 | 1.1073 |
Graph 1.
Percentage of osteocytes, rimming and nidus formation in 30 patients.
Graph 2.
semi-quantitative analyses of new bone formation
Semi quantitative analysis done by histological means showed 34–66% new bone formation in 40% cases, whereas 67–100% bone formation in 60% of cases.
5. Discussion
There are a lot of similarities between bone and teeth. Teeth, cartilages, muscles, and maxillofacial bones all originate from the neural crest embryologically. Most clinicians endorse the mechanism of intramembrane bone development when intraoral bone grafting is accomplished. There is an enormous amount of organic material in a tooth even though it has been left for a long time after removal, this is because the outer teeth have a strong apatite that can preserve the organic inner portion for a long time.8 If the organic portion of teeth is gradually released along with stem cells, growth factors and BMP seeded inside the teeth through an effective demineralization process, excellent bone healing can be expected.18 A new bone graft material can be developed using the inorganic and organic components of an extracted tooth as it has the properties of osteoconduction, osteoinduction, and osteogenesis.3 There are various ethical and biological issues associated with the processing of autogenous tooth graft material as the dent extracted from an individual is known as environmental waste and should be disposed of by an extracted material processor.9 Furthermore, if the patient agrees with the procedure and uses his/her own teeth, the use of autogenous bone graft is not against the rule.14 Maximum research work is mostly carried out as a bone regenerative material on the dried freeze demineralized dentin matrix.16 And there are very few case reports with a smaller sample size that used the whole tooth as a grafting product.10 We encountered more resistance to implant placement drilling and a torque of more than 40 N cm was obtained during implant insertion in 90% of patients. A study conducted by Minamizato et al (2018)4 obtained torque values of 25–40 N cm in 16 patients who were positioned using APDDM transplantation with dental implants.
In our analysis, 67–100% of new bone formation was observed in 60% of patients and 34–66% in 40% of patients with semi-quantitative histological analyzes. All this means enhancing peri-implant bone structure and mineralization which improves the stability and osseointegration of the primary implant. All of the above findings are consistent with the study conducted by Kim SE et al (2015)5 in which they found similar results in all patients within six months after grafting with the new bone formation with an even spatial pattern. Similar results with newly formed bone associated with connective tissue stroma rich in angiogenesis and infiltrated into the resorbed site of the graft material were shown in another study by Joshi et al (2016)6 discovering histology samples from ATG grafted sites.
The statistically highly significant difference was observed with a p-value of 0.009 and 0.001 respectively in our research on the comparison of mean alveolar height and alveolar width on pre- and post-operative CBCT scans.
No significant marginal bone loss, no significant post-operative reduction in bone height and restored alveolar socket anatomy was observed radiographically. Similar results were found in a study conducted by Binderman I (2014)3 in which, after regeneration, they observed increased bone density and bone level with no signs of bone resorption at the crest and concluded that autogenous dentin could be considered as the standard gold graft for socket survival, bone increase in the sinuses or bone filling. Takahashi et al (2012)7also conducted a study to determine the bone quantity of alveoli grafted in patients with alveolar clefts with autogenous particulate cancellous bone and marrow for implant placement. Bone height, bone width, and interdental alveolar crest rate were analyzed using computed tomography and found no significant loss of net bone height and width similar to the findings in our study.
Future studies should be performed on more sample size as we conducted this study on less subject and it necessitates longer follow-up to evaluate simultaneously the resorption of the graft and neo bone formation. As we have conducted pre-operative and post-operative CBCT and as CBCT provides pseudo-Hounsfield unit so that the graft density cannot be measured, CE-CT should, therefore, be performed to determine the grafted site density.
6. Conclusion
This study concludes that chair side autogenous tooth graft can be considered a gold standard for sinus augmentation, socket preservation, and ridge improvement because it is less time consuming, easy to prepare, with lower bone resorption rate osteoinduction, osteoconduction, osteogenetic properties, and excellent primary implant stability. The present study's drawback was its smaller sample size, with a larger sample size being required in a similar direction. The present study complements the literature reviewed on autogenous tooth grafting and it can be assumed that autogenous tooth grafts can be considered as the gold standard in alveolar bone grafts in the future.
Role of funding sources
None.
Ethical approval
Taken.
Informed consent
Obtained.
Declaration of competing interest
There was no conflict of interest.
Contributor Information
Anshuman Dwivedi, Email: anshumandmaxfac@gmail.com.
Manmeet Kour, Email: manmeetkour000@gmail.com.
References
- 1.Irinakis T. Rationale for socket preservation after extraction of a single-rooted tooth when planning for future implant placement. J Can Dent Assoc. 2006;72(10):917–922. [PubMed] [Google Scholar]
- 2.Irinakis T., Tabesh M. Preserving the socket dimensions with bone grafting in single sites: an esthetic surgical approach when planning delayed implant placement. J Oral Implantol. 2007;33(3):156–163. doi: 10.1563/0.824.1. [DOI] [PubMed] [Google Scholar]
- 3.Binderman I., Hallel G., Nardy C., Yaffe A., Sapoznikav L. A novel procedure to process extracted teeth for immediate grafting of autogenous dentin. Int dent African. 2014;7(1) [Google Scholar]
- 4.Minamizato T., Koga T., Takashi T. Clinical application of autogenous partially demineralized dentin matrix prepared immediately after extraction for alveolar bone regeneration in implant dentistry: a pilot study. Int J Oral Maxillofac Surg. 2018;47:125–132. doi: 10.1016/j.ijom.2017.02.1279. [DOI] [PubMed] [Google Scholar]
- 5.Kim S.K., Kim S.W., Kim K.W. Effect on bone formation of the autogenous tooth graft in the treatment of peri-implant vertical bone defects in the minipigs. Maxillofac Plast Reconstr Surg. 2015;37(1):2. doi: 10.1186/s40902-015-0002-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joshi C.P., Dani N.H., Khedkar S.U. Alveolar ridge preservation using autogenous tooth graft versus beta-tricalcium phosphate alloplast: a randomized, controlled, prospective, clinical pilot study. J Indian Soc Periodontol. 2016;20(4):429–434. doi: 10.4103/0972-124X.188335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takahashi T. Evaluation of secondary bone grafting of the alveolar cleft in adult cleft lip and palate patients. Asian J Oral Maxillofac Surg. 2011;24 10.001. [Google Scholar]
- 8.Kim Y.K., Lee J., Um I.W. Tooth-derived bone graft material. J Korean Assoc Oral Maxillofac Surg. 2013;39:103–111. doi: 10.5125/jkaoms.2013.39.3.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarala C., Chauhan M., Sandhya P.S., Dharmendra C.H., Mitra N. Autogenous tooth bone graft: ingenious bone regeneration material. Indian J Dent Sci. 2018;10:56–59. [Google Scholar]
- 10.Gual-Vaqués P., Polis-Yanes C., Estrugo-Devesa A., Ayuso-Montero R., Marí-Roig A., López-López J. Autogenous teeth used for bone grafting: a systematic review. Med Oral Patol Oral Cir Bucal. 2018 Jan 1;23(1):e112–e119. doi: 10.4317/medoral.22197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faverani L.P. Surgical techniques for maxillary bone grafting – literature review. Rev Col Bras Cir. 2014;41(1) doi: 10.1590/s0100-69912014000100012. 061-067. [DOI] [PubMed] [Google Scholar]
- 14.Kabir M.A., Murata M., Kusano K., Akazawa T., Shibata T. Autogenous demineralized dentin graft for third molar socket regeneration - a case report. Dentistry. 2015;5:343. [Google Scholar]
- 16.Calvo-Guirado J.L., Cegarra Del Pino P., Sapoznikov L., Delgado Ruiz R.A., Fernández-Domínguez M.5, Gehrke S.A. A new procedure for processing extracted teeth for immediate grafting in post-extraction sockets. An experimental study in American Fox Hound dogs. Ann Anat. 2018;217:14–23. doi: 10.1016/j.aanat.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 18.Guo W.1, He Y., Zhang X. The use of dentin matrix scaffold and dental follicle cells for dentin regeneration. Biomaterials. 2009 Dec;30(35):6708–6723. doi: 10.1016/j.biomaterials.2009.08.034. [DOI] [PubMed] [Google Scholar]