Abstract
With the global rise in the population of elderly along with other risk factors, spine surgeons have to encounter osteoporotic spine more often. Osteoporotic spine, however, causes problems in management, particularly where instrumentation is involved, resulting in screw loosening, pull out, pseudoarthroses or adjacent segment kyphosis. Osteoporosis alters the bio mechanics at the bone implant interface resulting in various degrees of fixation failure. Various advancements have been made in this field to deal with such issues in addition to modification of basic surgical techniques such as increasing the diameter and length of the screw, smaller pilot hole, under tapping, longer constructs, supplemental anterior fixation, sublaminar wires or laminar hooks, use of transverse connectors and triangulation techniques, among others. They include novel surgical techniques such as cortical bone trajectory, superior cortical trajectory, double screw technique, cross trajectory technique, bicortical screw technique or prophylactic vertebroplasty. Advances in the screw design include expandable screws, fenestrated screws, conical screws and coated screws. In addition to PMMA cement augmentation, other biodegradable cements have been introduced to mitigate the side effects of PMMA such as calcium phosphate, calcium apatite and hydroxyapatite. Pharmacotherapy with teriparatide can aid fusion and lower the rate of pedicle screw loosening. Many of these strategies have only bio mechanical evidence and require well designed clinical trials to establish their clinical efficacy. Though no single technique is fool proof, little modifications in the existing techniques or utilizing a combination of techniques without adding to the cost of the surgery may help to achieve a near-ideal result. Surgeons have to equip their armamentarium with all the recent advances, and should be open to novel thoughts and techniques.
Keywords: Osteoporosis, surgery; spine, surgery; Review literature; Recent advances; Evidence
1. Introduction
According to Population Census 2011 there are nearly 104 million elderly persons (aged 60 years or above) in India; 53 million females and 51 million males. A report released by the United Nations Population Fund and Help Age India suggests that the number of elderly persons is expected to grow to 173 million by 2026.1 With the growing population of older adults in India as well as globally, along with the growing incidence of other risk factors such as Vitamin D deficiency, sedentary lifestyle, smoking etc. spine surgeons have to encounter and deal with an osteoporotic spine more often.2 Also, with improvement in the anaesthetic and perioperative care, previously apprehensive patients and surgeons have become more willing for spine surgery even in the elderly.
Instrumented fusions with pedicle screw instrumentation have become the standard of care in spinal fusion surgery. Osteoporotic spine, however, complicates the management. Due to its fragile character, it often causes problems with instrumentation. Early complications such as pedicle and compression fractures and late complications such as pseudarthroses with instrumentation failure, adjacent-level disc degeneration with herniation, and progressive junctional kyphosis as a result of compression fractures have been reported after osteoporotic spine fixation.3 Hardware loosening or pull-out can occur as a result of micro-motion or injuries or excessive forces at the bone-metal boundaries.4 Pseudarthroses as a result of excessive osteoclastic activity over osteoblastic activity which happens in osteoporosis can result in longer than usual period of stress on the implant and thereby contribute to instrumentation failure.5 Adjacent level kyphosis can alter the number of levels involved in instrumentation.4 This is of particular concern when the construct ends at a kyphotic segment or at a transitional area. Even anterior instrumentation failure can occur secondary to continuous cyclic loading, cut out and subsidence of inter body devices into osteoporotic bone.6
Attempts have been made to address these concerns and there have been advancements in the variety of designs and surgical techniques, both in laboratory setting and in clinical setting to achieve optimal fixation of implant within bone of compromised quality. The purpose of this review is to outline the various advancements in osteoporotic fixation, the underlying principles, the advantages and disadvantages and the lacunae in developing a fool-proof technique of osteoporotic spine fixation.
We used MESH terms "Spine/surgery" AND "Osteoporosis" to find all the relevant articles till date. 563 articles were found of which full text articles were available for 497 articles. We accumulated all the articles which described techniques to improve the fixation strength of implants in osteoporotic spine fixation. We also went through the other similar and relevant articles. We tried to grossly divide them into advancements in screw or construct design and advancements in surgical techniques (Table 1). Finally, we added a note on the way forward in achieving a fool-proof technique or design.
Table 1.
A table summarizing the advances in osteoporotic spine fixation.
| Basic surgical techniques: |
| Increasing diameter of screw |
| Increasing length of screw |
| Small pilot hole |
| Under tapping of screw track |
| Longer construct |
| Supplemental anterior fixation |
| Use of laminar hooks or wires |
| Use of transverse connectors |
| Triangulation techniques |
| Novel surgical techniques: |
| Cortical bone trajectory |
| Superior cortical screw technique |
| Double screw technique |
| Cross screw trajectory |
| Bicortical screw technique |
| Novel screw or construct design: |
| Expandable screws |
| Fenestrated pedicle screws |
| Conical screws |
| Coated screws |
| Cement augmentation |
| Prophylactic vertebroplasty |
| Perioperative pharmacotherapy |
| Other novel strategies: |
| Biomolecular coating |
| Novel biomaterials |
| Biodegradable cements |
| Combination techniques |
2. Advancements in surgical techniques
2.1. Basic surgical techniques
Increasing the diameter and length of the screw and an insertion technique with a pilot hole size smaller than the core diameter of the screw and under tapping a pilot hole has been proposed to improve the pull out strength of pedicle screw.7 However, larger screws were found to have no effect on the fixation strength in osteoporotic bone due to the thin cortex of the pedicle.8 Other techniques such as use of longer constructs, supplemental anterior fixation, use of transverse connectors and triangulation techniques, use of laminar hooks or sub-laminar wires have been shown to contribute to the rigidity of the construct.
Increasing the number of fixation points is often recommended to dissipate stress and improve stability in an osteoporotic spine fixation. It can be either by extending the usual number of levels of fixation or by utilizing additional constructs such as laminar hooks or sub laminar wires in addition to the usual pedicle screw fixation. The laminar hook fixation is not adversely affected by osteoporosis as reported by Butler et al. in his study.9 Sub laminar hooks show superior biomechanical stability compared to wires or pedicle screws in osteoporotic thoracic spine.10 Combination of fixation techniques can help distribute stresses on the osteoporotic bone. It was reported that combination of hooks and pedicle screws, also called pediculolaminar fixation can increase the pull out strength up to 100%.11 They can also increase the stiffness of the construct and add to torsional stability in osteoporotic bone.9,10 However, clinical studies utilizing these combined techniques are limited probably because of the technical difficulties in connecting these supplemental fixation points to the rods between screws.
Regarding the number of levels of fixation, it was recommended to at least include three fixation points above and below the apex of the deformity.12 However, the optimal length of fusion is still in discussion. Also, it is preferable to avoid ending the construct at the apex of kyphotic deformity, cephalic end of the construct at L1 and caudal end of a long construct at L5 to avoid potential kyphotic collapse.13 Sagittal imbalance is a reliable and determinant predictor of clinical symptomatology in osteoporotic fractures and reestablishment of sagittal balance is supposed to be the most relevant factor for preventing junctional imbalance/failure.14 Age specific goals in adult deformity correction have been proposed lately to prevent junctional breakdown.15
Also, a circumferential fusion allows load sharing and places less stress on the posterior construct. Posterior and transforaminal lumbar interbody fusion techniques can be utilized to provide anterior column support. However, careful and meticulous end plate preparation and use of appropriate sized interbody spacer are important for successful fusion. Use of huge quantity of bone graft and preservation of the osseous end plate has been proposed by Okuda et al. for successful fusion.16 Few authors also propose removal of the osseous end plate to allow implant to rest on cancellous base which facilitates fusion.17 However, this has to be taken critically, particularly in osteoporosis, where cancellous base is weak. Also, the increased operative time, blood loss and surgical risk has to be taken into consideration for opting supplemental anterior fusion.
2.2. Cement augmentation
Frankel et al. reported an increase in the pull out strength of screws with PMMA (poly methyl methacrylate) augmentation in primary and revision surgeries by 119% and 162% respectively.18 However, the disadvantages with PMMA include its exothermic properties, the risk of neural injury in the event of extravasation, and difficulties in performing revision surgery. Hence, use of biodegradable cements was suggested. Moore et al. and Wuisman et al. reported satisfactory results utilizing calcium phosphate and calcium apatite cements respectively.19,20 Jang et al. reported that HA (Hydroxyapatite) augmentation resulted in an improved screw-bone interface, reduced the risk of angular displacement of screw constructs, and prevented subsidence at the operative level.21 This is slightly different from the HA coated screws as it enables augmentation of only the distal tip of the screw and makes extraction easy whereas HA coated screws augment the entire length of screw and create higher extraction torque.21 However, while the use of biodegradable cements certainly make screw removal less tedious when compared to PMMA, they need more time (up to 24 h) for curing and hence will not give enhanced fixation at the time of surgery.
Indirect methods such as bone cement augmentation via the disc space for percutaneous pedicle screw fixation for lumbar fusion surgeries have also been proposed as safe and economical alternatives but have yet to be established.22
In addition to cement augmentation of screws, prophylactic vertebroplasty augmentation of segments above and below the instrumented fusion levels has been studied to prevent adjacent segment fractures.23 It has also been found to reduce the risk of proximal junctional kyphosis.24 Further studies are necessary to establish its efficacy as such prophylactic augmentation techniques have also been reported to be associated with further and more severe spinal fractures in other studies.25
2.3. Cortical bone trajectory technique: (Fig. 126)
Fig. 1.
26 AP (Antero-posterior) and lateral X-ray images of a patient showing the Cortical Bone Trajectory technique for pedicle screw fixation.
Since the cancellous bone is more profoundly affected in osteoporosis compared to cortical bone and the traditional pedicle screw trajectory engages more cancellous bone than cortical bone, novel trajectory designs have been attempted to increase cortical contact. Cortical bone trajectory (CBT) screw is one such novel technique with insertion point more medial than that of a traditional pedicle screw and the trajectory oriented sagittal and cranial.27 Matsukawa et al. proposed the entry point at the junction of center of the superior articular process and 1 mm inferior to the inferior border of transverse process.28 The screw is directed cranially towards the posterior one third of the superior end plate in the sagittal plane and directed straight forward in the transverse plane. It passes through the inferior and medial corner of the proximal pedicle, then through the pedicle and then pierces the superolateral end plate of the vertebra. Iwatsuki et al. proposed an entry point at the lateral margin of the isthmus and superior margin of the intervertebral foramen.29 The CBT takes advantage of the cortically based trackI and allows for less soft tissue dissection during insertion, making it amenable to minimally invasive techniques. It was found on biomechanical studies to have a superior fixation in osteoporotic bone.
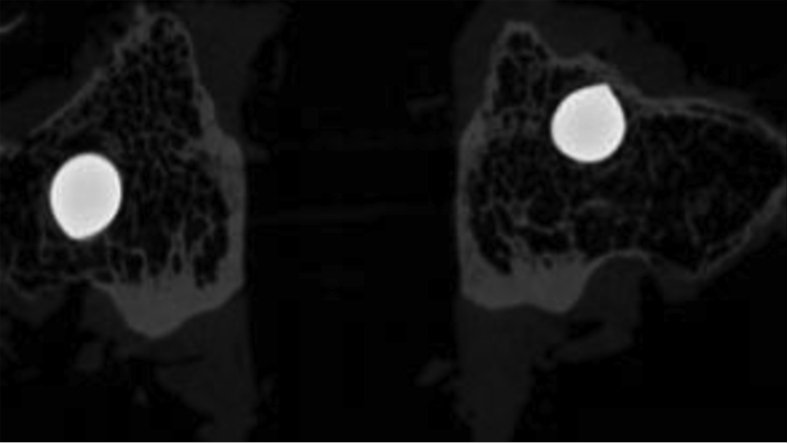
2.4. Superior cortical screw technique: (Fig. 230)
Fig. 2.
30 CT image of the pedicles showing the position of a traditional pedicle screw (left) and a superior cortical screw (right).
Since the pedicle provides roughly 60% of the pull out strength of pedicles screw and the upper third of the pedicle has the densest microstructure, a novel trajectory was attempted with entry point 3 mm above the Magerl’s point and was found to have higher pull out strength on biomechanical study by Yu et al. 30
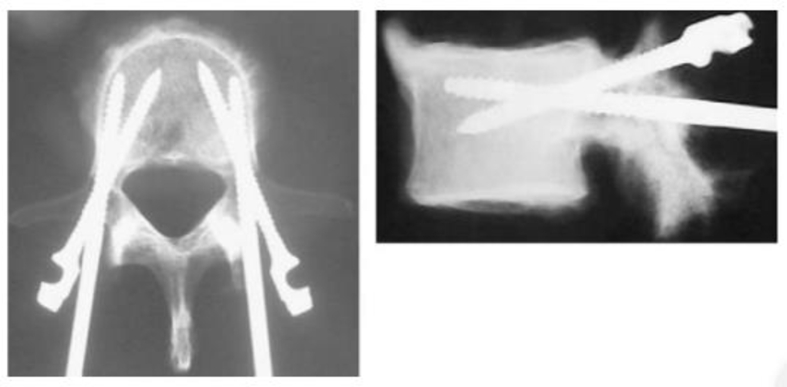
2.5. Double screw technique: (Fig. 331)
Fig. 3.
31 AP and lateral X-ray images of a patient operated by double screw technique of pedicle screw fixation.
Biomechanical feasibility studies have shown that the elliptical cross-section of the pedicle would allow the insertion of two smaller diameter pedicle screws resulting in a bony purchase superior to the standard single-screw technique.32 The safety profile has to be established before the technique can be recommended widely.
2.6. Cross trajectory technique: (Fig. 433)
Fig. 4.
33 An illustration showing the cross trajectory technique of screw insertion.
A novel double-screw technique with the combined use of traditional trajectory (TT) and CBT, by inserting two screws into an elliptical shape of a single pedicle using different transpedicular trajectories was proposed by Matsukawa et al. and found to have superior fixation strength over the TT and CBT techniques in each plane of motion.33 However, the disadvantages include a higher cost of the instrumentation as well as the technically demanding procedure with risks of neural injury and pedicle fracture.
2.7. Bicortical screw technique
Bicortical screw fixation has been proposed to increase the fixation strength by increasing the number of cortices engaged. Battula et al. recommended inserting the screw 2 mm beyond the far cortex for adequate pull out strength.34 However, this technique is limited by the risk of injuring anterior structures which include sacral sympathetic trunk, colon, vena cava and the aorta.
3. Advancements in screw/construct design
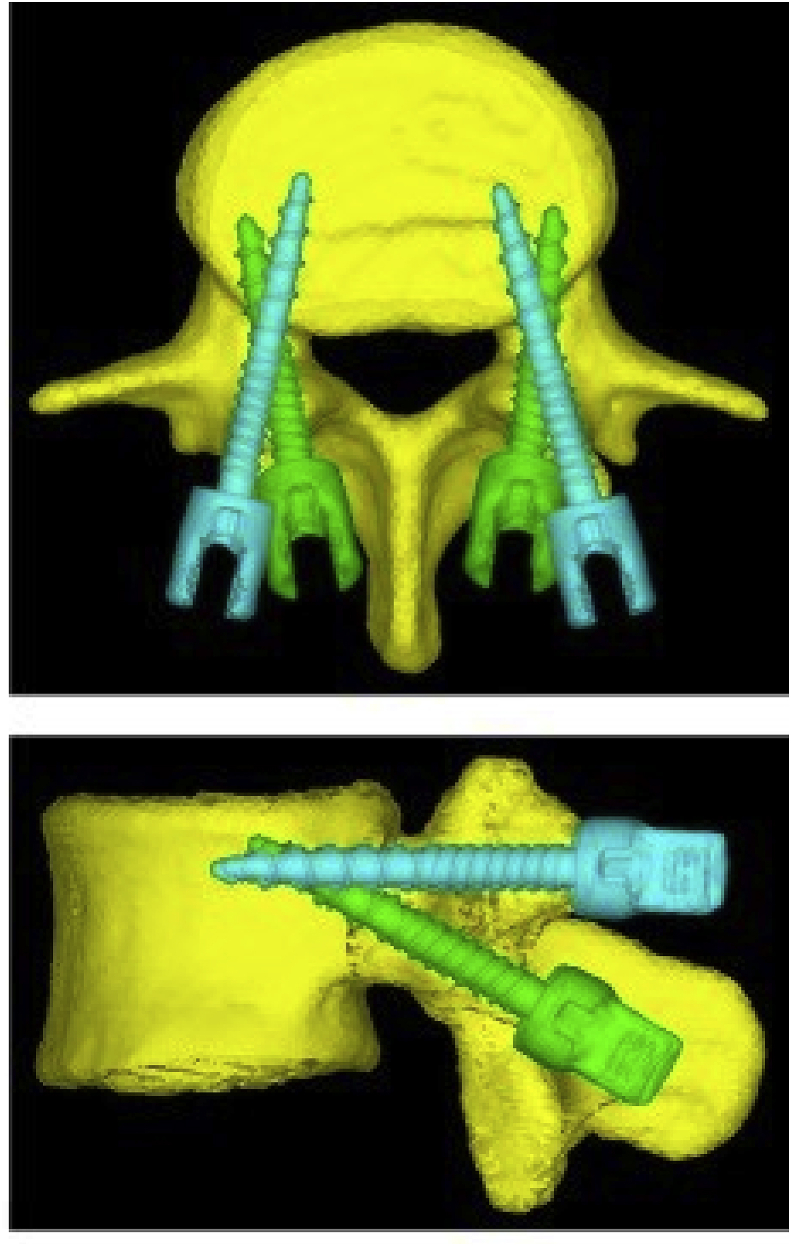
3.1. Expandable screws: (Fig. 535)
Fig. 5.
35 Image showing an expandable pedicle screw (Weigao Orthopedic Device Co. Ltd., Shandong, China).
Since increasing the size of the pedicle screw to achieve a optimal fixation may result in a pedicle fracture, screws which allow insertion into pedicle and vertebral body as a standard cylindrical screw but expand at the distal end after their insertion were developed. Several novel expandable screws have been designed in a pursuit to achieve optimal fixation in osteoporotic bone.36 Expansion of the screw compresses the bone tissues surrounding the expandable portion of the expandable screw making them denser and contributing to the fixation strength. They were shown to decrease the risk of screw loosening and improve fixation strength in prospective studies.37 Biomechanical studies showed that the pull out strength and energy of the screw is similar to a conventional pedicle screw augmented with 2 ml of bone cement.38 It avoids the risks associated with cement leakage in the latter. However, they may cause problems in removing the screw during revision procedures.
3.2. Fenestrated pedicle screws: (Fig. 639)
Fig. 6.
39 An image showing a fenestrated pedicle screw.
Use of fenestrated pedicle screws which are a special type of cannulated screw with fenestrations allowing cement to be inserted through the screw and engage the surrounding cancellous bone of the vertebral body through the fenestrations is theoretically safer in terms of avoiding inadvertent cement extravasation into the spinal canal or neural foramen. It was found that the closer the PMMA is to the pedicle and the greater the quantity of injected PMMA used (up to a point), the greater the pedicle screw stability is.40
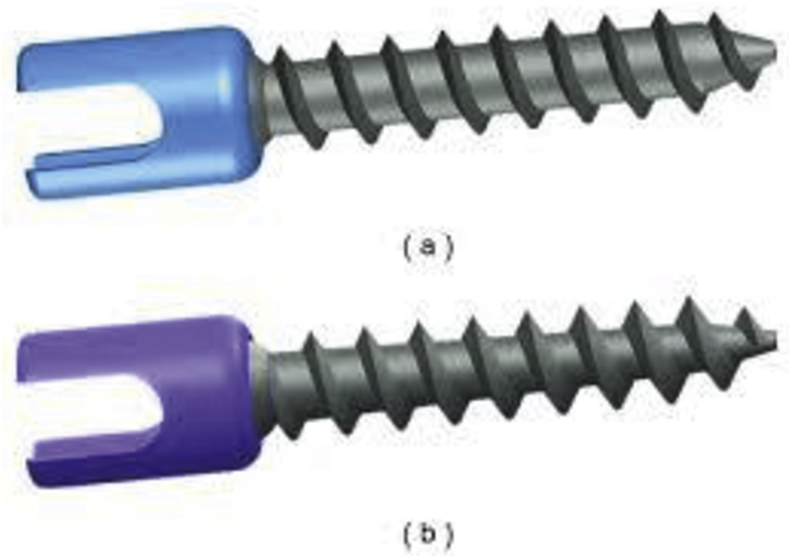
3.3. Conical screws: (Fig. 741)
Fig. 7.
41 An image showing a traditional pedicle screw (cylindrical) (a) and a conical pedicle screw(b).
Experimental and biomechanical studies have shown that pedicle screws with an outer cylindrical and inner conical configuration with a V-shaped thread may have maximum pull-out strength, regardless of bone density.42 A tapering inner core allows deeper threads with a larger surface area to engage with the poor-quality cancellous bone of the vertebral body in osteoporosis. At the same time, the conical screw design ensures that the inner core diameter remains large in the area of the pedicle where it faces the highest bending moment.
3.4. Coated screws: (Fig. 843)
Fig. 8.
43 Image showing a HA coated screw and a traditional screw.
Laboratory and clinical studies have shown that HA coating of screws results in improved fixation with reduced risk of loosening.44 It was reported to result in a significant decrease in the incidence of radiolucent zones when compared with uncoated screws.44 However, as mentioned previously, they create higher extraction torque and cause difficulties in removal. HA coated screws do not provide enhanced stability immediately, but it takes around 10 days for the HA coating to start providing enhanced stability (by gradual incorporation with the host bone).
4. Other novel strategies
Strategies targeting the complex cellular and molecular processes that occur following implantation have been developed recently. They act by altering and/or modifying the cellular recruitment and differentiation at the surgical site using biological coating or mechanical alteration of implant surfaces to enhance in-migration of bone. Titanium implants have been coated with α5β1-specific FNIII7–10 bio molecular coatings or glycine-phenylalanine-hydroxyproline-glycine-glutamate-arginine (GFOGER) collagen-mimetic peptide, selectively promoting alpha2 beta1 integrin binding, a crucial event for osteoblastic differentiation.45 Such novel biological strategies provide an interesting outlook for research in the future.
Recently, tantalum has been used in spine surgery. Inter body devices utilizing tantalum are being manufactured and used clinically. Because of the porous scaffold, superior osteoconductivity, low modulus of elasticity, excellent bio activity and bio compatibility, it has a potential role in osteoporotic spine fixation. However, the relatively high cost, the inability to produce it modularly and lower fatigue resistance compared with fully dense materials limit manufacturing screws based on these materials.
In cement augmentation techniques, in addition to vertebroplasty and kyphoplasty, Stentoplasty has been recently described where a cavity is created within the vertebral body by using a titanium device and kept in place for cement injection.46 It was found to have good to excellent results in pain improvement, quality of life and kyphosis restoration.
Biodegradable cements, developed recently to combat the problems with acrylic bone cements have been supplemented by various bioactive, osteogenic agents to promote osteogenic differentiation of progenitor cells and new bone formation. Incorporation of several bioactive ions such as strontium, magnesium, zinc, copper, and fluoride, as well as growth factors such as bone morphogenetic proteins (BMPs), basic fibroblast growth factor (bFGF), and vascular endothelial growth factor (VEGF) has been shown to improve the biological performance of biodegradable cements.47 Platelet-rich plasma (PRP) and autologous bone marrow concentrate (BMC) have also been used together with cements as autologous bone substitutes.
4.1. Role of pharmacotherapy
The role of pharmacotherapy in aiding implant fixation or fusion has been studied on bisphosphonates and teriparatide. Whereas Alendronate was found to have conflicting results in few studies on its effect in aiding fusion,48 Zolendronate was found to have non statistically significant difference. However, prospective trials showed significant advantage to teriparatide in aiding fusion and lowering the rate of pedicle screw loosening.49 Based on the available literature, it is imperative that surgeons can advise starting teriparatide before surgery and continue it through the postoperative fusion period. Though Denosumab, a RANK-L inhibitor has been approved by FDA (Food and Drug Administration) and established in the treatment of osteoporosis, its role in lumbar fusion has, yet to be evaluated.
Many of these strategies have only bio mechanical evidence and require well designed clinical trials to establish their clinical efficacy. Tremendous advancements have been made in the field of spine surgery in general. Osteoporotic spine fixation also has seen such advances. However, no technique is fool-proof and there has been no single ideal technique to achieve optimal fixation in osteoporotic bone.
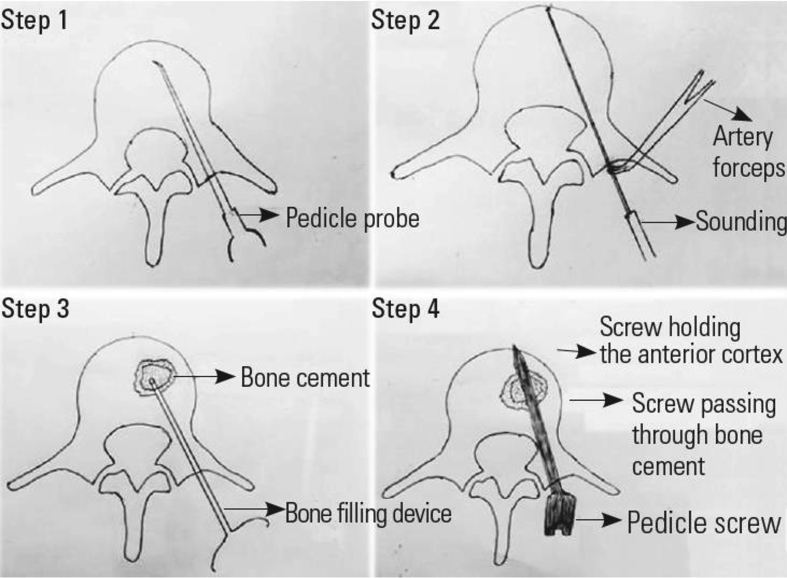
Surgeons have to be open to new advances in the field of osteoporotic spine fixation. At the same time, they should be smart enough to utilize the existing options to their advantage. Little modifications in the existing techniques or utilizing a combination of techniques without adding to the cost of the surgery may help to achieve a near-ideal result. For instance, a prospective study on the feasibility, efficacy and safety of a technique involving a combination of bi-cortical fixation with cement augmentation was performed with good results50(Fig. 9). The advantages of this technique include an increase in pull-out strength than either technique alone and a reduction in the wind-shield wiper effect. Also, there would be no extra cost compared to cement augmentation alone.
Fig. 9.
50 An illustration showing the technique of bicortical screw fixation with cement augmentation.
Spine surgeons have to be aware of the advances in the field of osteoporotic spine fixation. They have to keep all the surgical techniques in their armamentarium and make themselves well versed with the advancements in the field. They have to be open to new advances in the field and utilize them as and when necessary depending on the patient and the set up.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare no conflict of interest.
Contributor Information
Vikas Tandon, Email: vikas.spinesurgeon@gmail.com.
Jorg Franke, Email: jfranke@cubelink.de.
Kalyan Kumar Varma Kalidindi, Email: kalyanvarmambbs@gmail.com.
References
- 1.http://vikaspedia.in/social-welfare/senior-citizens-welfare/senior-citizens-status-in-india
- 2.Khadgawat R., Brar K.S., Gahlo M. High prevalence of vitamin D deficiency in Asian-Indian patients with fragility hip fracture: a pilot study. J Assoc Phys India. 2010;58:539–542. [PubMed] [Google Scholar]
- 3.DeWald C.J., Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65. Surgical considerations and treatment options in patients with poor bone quality. Spine. 2006;31:S144–S151. doi: 10.1097/01.brs.0000236893.65878.39. [DOI] [PubMed] [Google Scholar]
- 4.Hu S.S. Internal fixation in the osteoporotic spine. Spine. 1997;22(24):43S–48S. doi: 10.1097/00007632-199712151-00008. [DOI] [PubMed] [Google Scholar]
- 5.Jost B., Cripton P.A., Lund T. Compressive strength of interbody cages in the lumbar spine: the effect of cage shape, posterior instrumentation and bone density. Eur Spine J. 1998;7:132–141. doi: 10.1007/s005860050043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steffen T., Tsantrizos A., Aebi M. Effect of implant design and endplate preparation on the compressive strength of interbody fusion constructs. Spine. 2000;25:1077–1084. doi: 10.1097/00007632-200005010-00007. [DOI] [PubMed] [Google Scholar]
- 7.Chatzistergos P.E., Sapkas G., Kourkoulis S.K. The influence of the insertion technique on the pullout force of pedicle screws: an experimental study. Spine. 2010;35:E332–E337. doi: 10.1097/BRS.0b013e3181ba0b0c. [DOI] [PubMed] [Google Scholar]
- 8.Hirano T., Hasegawa K., Takahashi H.E. Structural characteristics of the pedicle and its role in screw stability. Spine. 1997;22:2504–2510. doi: 10.1097/00007632-199711010-00007. Phila Pa 1976. [DOI] [PubMed] [Google Scholar]
- 9.Butler T.E., Jr., Asher M.A., Jayaraman G., Nunley P.D., Robinson R.G. The strength and stiffness of thoracic implant anchors in osteoporotic spines. Spine. 1994;19(17):1956–1962. doi: 10.1097/00007632-199409000-00016. Phila Pa 1976. [DOI] [PubMed] [Google Scholar]
- 10.Coe J.D., Warden K.E., Herzig M.A., McAfee P.C. Influence of bone mineral density on the fixation of thoracolumbar implants: a comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine. 1990;15(9):902–907. doi: 10.1097/00007632-199009000-00012. Phila Pa 1976. [DOI] [PubMed] [Google Scholar]
- 11.Liljenqvist U., Hackenberg L., Link T., Halm H. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg. 2001;67(2):157–163. [PubMed] [Google Scholar]
- 12.De Wald C.J., Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65 surgical considerations and treatment options in patients with poor bone quality. Spine. 2006;31(Suppl 19):S144–S151. doi: 10.1097/01.brs.0000236893.65878.39. [DOI] [PubMed] [Google Scholar]
- 13.Kwon B.K., Elgafy H., Keynan O. Progressive junctional kyphosis at the caudal end of lumbar instrumented fusion: etiology, predictors, and treatment. Spine. 2006;31(17):1943–1951. doi: 10.1097/01.brs.0000229258.83071.db. Phila Pa 1976. [DOI] [PubMed] [Google Scholar]
- 14.Lattig F. Bone cement augmentation in the prevention of adjacent segment failure after multilevel adult deformity fusion. J Spinal Disord Tech. 2009;22(6):439–443. doi: 10.1097/BSD.0b013e31818d6493. [DOI] [PubMed] [Google Scholar]
- 15.Lafage R., Schwab F., Challier V. Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine. 2016;41:62–68. doi: 10.1097/BRS.0000000000001171. Phila Pa 1976. [DOI] [PubMed] [Google Scholar]
- 16.Okuda S., Oda T., Miyauchi A., Haku T., Yamamoto T., Iwasaki M. Surgical outcomes of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am. 2007;1(2):310–320. doi: 10.2106/JBJS.G.00307. [DOI] [PubMed] [Google Scholar]
- 17.Steffen T., Tsantrizos A., Aebi M. Effect of implant design and endplate preparation on the compressive strength of interbody fusion constructs. Spine. 2000;25(9):1077–1084. doi: 10.1097/00007632-200005010-00007. Phila Pa 1976. preparation on the compressive strength of interbody fusion constructs. Spine (Phila Pa 1976) 2000;25(9):1077–1084. [DOI] [PubMed] [Google Scholar]
- 18.Frankel B.M., D’Agostino S., Wang C. A biomechanical cadaveric analysis of polymethylmethacrylate augmented pedicle screw fixation. J Neurosurg Spine. 2007;7:47–53. doi: 10.3171/SPI-07/07/047. [DOI] [PubMed] [Google Scholar]
- 19.Moore D.C., Maitra R.S., Farjo L.A., Graziano G.P., Goldstein S.A. Restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine. 1997;22:1696–1705. doi: 10.1097/00007632-199708010-00003. [DOI] [PubMed] [Google Scholar]
- 20.Wuisman P.I., Van Dijk M., Staal H., Van Royen B.J. Augmentation of (pedicle) screws with calcium apatite cement in patients with severe progressive osteoporotic spinal deformities: an innovative technique. Eur Spine J. 2000;9:528–533. doi: 10.1007/s005860000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jang S.H., Lee J.H., Cho J.Y., Lee H.Y., Lee S.H. The efficacy of hydroxyapatite for screw augmentation in osteoporotic patients. Neurol Med -Chir. 2013;53(12):875–881. doi: 10.2176/nmc.oa2012-0346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park C.K., Park C.K., Lee D.C., Lee D.G. A new technique of bone cement augmentation via the disc space for percutaneous pedicle screw fixation. J Neurosurg Spine. 2016 Jan;24(1):16–19. doi: 10.3171/2015.4.SPINE141115. Epub 2015 Sep. 11. [DOI] [PubMed] [Google Scholar]
- 23.Aydogan M., Ozturk C., Karatoprak O., Tezer M., Aksu N., Hamzaoglu A. The pedicle screw fixation with vertebroplasty augmentation in the surgical treatment of the severe osteoporotic spines. J Spinal Disord Tech. 2009;22(6):444–447. doi: 10.1097/BSD.0b013e31818e0945. 57. [DOI] [PubMed] [Google Scholar]
- 24.Raman T., Miller E., Martin C.T., Kebaish K.M. The effect of prophylactic vertebroplasty on the incidence of proximal junctional kyphosis and proximal junctional failure following posterior spinal fusion in adult spinal deformity: a 5-year follow-up study. Spine J. 2017;17(10):1489–1498. doi: 10.1016/j.spinee.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 25.Fernández-Baíllo N., Sánchez Márquez J.M., Sánchez Pérez-Grueso F.J., GarcíaFernández A. Proximal junctional vertebral fracture-subluxation after adult spine deformity surgery. Does vertebral augmentation avoid this complication? A case report. Scoliosis. 2012;7(1):16. doi: 10.1186/1748-7161-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dabbous B., Brown D.V., Tsitlakidis A., Arzoglou V. Clinical outcomes during the learning curve of MIDline Lumbar Fusion (MIDLF®) using the cortical bone trajectory. Acta Neurochir. 2016;158:1413–1420. doi: 10.1007/s00701-016-2810-8. [DOI] [PubMed] [Google Scholar]
- 27.Santoni B.G., Hynes R.A., McGilvray K.C. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9:366–373. doi: 10.1016/j.spinee.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Matsukawa K., Yato Y., Nemoto O. Morphometric measurement of cortical bone trajectory for lumbar pedicle screw insertion using computed tomography. J Spinal Disord Tech. 2013;26:E248–E253. doi: 10.1097/BSD.0b013e318288ac39. [DOI] [PubMed] [Google Scholar]
- 29.Iwatsuki K., Yoshimine T., Ohnishi Y. Isthmus-guided cortical bone trajectory for pedicle screw insertion. Orthop Surg. 2014;6:244–248. doi: 10.1111/os.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu Tianming, Zhang Xuyang, Liu Junhui. Superior cortical screw in osteoporotic lumbar vertebrae: a biomechanics and microstructure-based study. Clin BioMech. 2018;53 doi: 10.1016/j.clinbiomech.2018.01.017. March 14-21. [DOI] [PubMed] [Google Scholar]
- 31.Awwad Waleed, Alahaideb Abdulaziz, Jiang Liang. Correction of severe pelvic obliquity using maximum-width segmental sacropelvic screw fixation: an analysis of 20 neuromuscular scoliosis patients. Eur J Orthop Surg Traumatol : Orthop Traumatol. 2014;25 doi: 10.1007/s00590-014-1458-4. [DOI] [PubMed] [Google Scholar]
- 32.Jiang L., Arlet V., Beckman L., Steffen T. Double pedicle screw instrumentation in the osteoporotic spine: a biomechanical feasibility study. J Spinal Disord Tech. 2007 Aug;20(6):430–435. doi: 10.1097/bsd.0b013e318030e945. [DOI] [PubMed] [Google Scholar]
- 33.Matsukawa K., Yato Y., Imabayashi H., Hosogane N., Asazuma T., Nemoto K. Biomechanical evaluation of cross trajectory technique for pedicle screw insertion: combined use of traditional trajectory and cortical bone trajectory. Orthop Surg. 2015 Nov;7(4):317–323. doi: 10.1111/os.12212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Battula S., Schoenfeld A.J., Sahai V., Vrabec G.A., Tank J., Njus G.O. The effect of pilot hole size on the insertion torque and pullout strength of self-tapping cortical bone screws in osteoporotic bone. J Trauma Acute Care Surg. 2008;64(4):990. doi: 10.1097/TA.0b013e31802bf051. [DOI] [PubMed] [Google Scholar]
- 35.Wu Z.-X., Gao M.-X., Sang H.-X. Surgical treatment of osteoporotic thoracolumbar compressive fractures with open vertebral cement augmentation of expandable pedicle screw fixation: a biomechanical study and a 2-year follow-up of 20 patients. J Surg Res. 2012;173(1):91–98. doi: 10.1016/j.jss.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 36.Wu Z.X., Cui G., Lei W., Fan Y., Wan S.Y., Ma Z.S. Application of an expandable pedicle screw in the severe osteoporotic spine: a preliminary study. Clin Invest Med. 2010;33:E1–E8. doi: 10.25011/cim.v33i6.14587. [DOI] [PubMed] [Google Scholar]
- 37.Wu Z.X., Gong F.T., Liu L., Ma Z.S., Zhang Y., Zhao X. A comparative study on screw loosening in osteoporotic lumbar spine fusion between expandable and conventional pedicle screws. Arch Orthop Trauma Surg. 2012 Apr;132(4):471–476. doi: 10.1007/s00402-011-1439-6. Epub 2011 Dec 7. [DOI] [PubMed] [Google Scholar]
- 38.Chen Y.-L. Biomechanical study of expandable pedicle screw fixation in severe osteoporotic bone comparing with conventional and cement-augmented pedicle screws. Med Eng Phys. 2014 doi: 10.1016/j.medengphy.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 39.Lubansu A., Rynkowski Michal, Abeloos Laurence, Appelboom Geoffrey, Dewitte Olivier. Minimally invasive spinal arthrodesis in osteoporotic population using a cannulated and fenestrated augmented screw: technical description and clinical experience. Minim Invasive Surg. 2012;2012:507826. doi: 10.1155/2012/507826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu Da, Sheng Jun, Luo Yang. Biomechanical comparative study on stability of injectable pedicle screw with 1 different lateral holes augmented with different volumes of polymethylmethacrylate in osteoporotic lumbar vertebrae. Spine J. 2018 doi: 10.1016/j.spinee.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 41.Shea Thomas, Laun Jake, Gonzalez-Blohm Sabrina. Designs and techniques that improve the pullout strength of pedicle screws in osteoporotic vertebrae: current status. BioMed Res Int. 2014;2014:748393. doi: 10.1155/2014/748393. open access. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim Y.-Y., Choi W.-S., Rhyu K.-W. Assessment of pedicle screw pullout strength based on various screw designs and bone densities—an ex vivo biomechanical study. Spine J. 2012;12(2):164–168. doi: 10.1016/j.spinee.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 43.Davis Timothy, Vatave Ajay, Patla James, Bernbeck Johannes, Delamarter Rick, Bae Hyun. 2020. Pedicle Screw Electrical Resistance: Hydroxyapatite Coated versus Non-coated. [Google Scholar]
- 44.Sandén B., Olerud C., Petrén-Mallmin M., Larsson S. Hydroxyapatite coating improves fixation of pedicle screws. Bone Joint J. May 2002;84(3):387–391. doi: 10.1302/0301-620X.84B3.12388. A clinical study. [DOI] [PubMed] [Google Scholar]
- 45.Reyes C.D., Petrie T.A., Burns K.L., Schwartz Z., García A.J. Biomolecular surface coating to enhance orthopaedic tissue healing and integration. Biomaterials. 2007;28(21):3228–3235. doi: 10.1016/j.biomaterials.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Heini P.F., Teuscher R. Vertebral body stenting/stentoplasty. Swiss Med Wkly. 2012;142:w13658. doi: 10.4414/smw.2012.13658. [DOI] [PubMed] [Google Scholar]
- 47.Bose S., Tarafder S. Calcium phosphate ceramic systems in growth factor and drug delivery for bone tissue engineering: a review. Acta Biomater. 2012;8:1401–1421. doi: 10.1016/j.actbio.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nagahama K., Kanayama M., Togawa D., Hashimoto T., Minami A. Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. J Neurosurg Spine. 2011;14(4):500–507. doi: 10.3171/2010.11.spine10245. [DOI] [PubMed] [Google Scholar]
- 49.Ohtori S., Inoue G., Orita S. Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine. 2012;37(23):E1464–E1468. doi: 10.1097/BRS.0b013e31826ca2a8. Phila Pa 1976. [DOI] [PubMed] [Google Scholar]
- 50.Tandon Vikas, Kalidindi Kalyan Kumar Varma, Pacha Sandesh, Bhat Mohd Rafiq. A prospective study on the feasibility, safety, and efficacy of a modified technique to augment the strength of pedicle screw in osteoporotic spine fixation. Asian Spine J. 2020 doi: 10.31616/asj.2019.0211. asj.2019.0211. Online first: January 8, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]