Abstract
Difficulty in adhering to the recommended diet is a common problem in individuals with diabetes mellitus (DM). Dietary non-adherence among diabetic individuals leads to diabetes related complication and death. As far as our search established, there is a scarcity of scientific evidence of dietary non-adherence of individuals with diabetes to the recommended diet in Ethiopia, specifically in the Northwest part of the country. Hence, this study aims to assess the dietary non-adherence and associated factors among individuals with diabetes at Felege-Hiwot Referral Hospital, Bahir Dar city, Northwest Ethiopia. An institution-based cross-sectional study was conducted on 385 systematically selected individuals with diabetes following their treatment from March to April 2017. Quantitative data were collected using a pre-tested and structured questionnaire. The dependent variable association with explanatory variables was determined using logistic regression. Statistical significance was considered at p-value <0.05 with 95% CI. The overall proportion of dietary non-adherence among participants was 46.8% (95% CI: 41.1–52.0). Living rurally (AOR = 3. 75; 95% CI: 2.12–6.63), duration of diabetes less than 5 years (AOR = 2. 81; 95% CI: 1.22–6.50), did not receive nutritional education (AOR = 5. 88; 95% CI: 3.30–10.48), poor social support (AOR = 3. 84; 95% CI: 1.74–8.46) and did not make choices when eating out (AOR = 3. 49; 95% CI: 2.09–5.81) were significantly associated with dietary non-adherence. Nearly half of the individuals with diabetes involved in this study did not adhere to the recommended diet. This problem could be addressed through the provision of nutritional education and strengthening social support to adhere to diabetes dietary recommendations. Therefore, health professional and nutritional educators should take appropriate action to increase the proportion of dietary adherence of individuals with diabetes.
Keywords: Diet, Endocrine system, Food toxicology, Metabolism, Nutrition, Poultry products, Public health, Qualitative research in nutrition, Seafood, Diabetes, Dietary non-adherence, Ethiopia
Diet; Endocrine system; Food toxicology; Metabolism; Nutrition; Poultry products; Public health; Qualitative research in nutrition; Seafood; Diabetes, Dietary non-adherence, Ethiopia
1. Introduction
Diabetes is a chronic condition that occurs when the body cannot produce enough insulin or cannot use insulin and individuals present with raised levels of glucose in the blood. Due to this, accumulation of glucose in the blood over time damage to many body tissues is caused; leading to the development of debilitating and life-threatening health complications such as coronary artery and peripheral vascular diseases [1, 2].
Currently, diabetes is the most common non-communicable disease burden in the world [3]. It is the fourth or fifth leading cause of death in most high-income countries. Its prevalence is also increasing alarmingly in many low and middle-income countries [1]. Complications from diabetes result in increasing disability reduced life expectancy and increased health costs for many societies [1, 2].
According to the World Health Organization report in 2016, the number of individuals with diabetes increased from 108 million in 1980 to 422 million in 2014. In addition, the global prevalence of diabetes among adults above 18 years of age rose from 4.7% in 1980 to 8.5% in 2014 [3]. The International Diabetes Federation reported that more than 19.4 million individuals live with diabetes in Africa and this number is projected to reach 29 million by 2030, and 47 million by 2045. In Ethiopia, over 1.733 million individuals were living with diabetes in 2019 [1]. Worldwide Diabetes Mellitus (DM) is one of the most challenging health problems in the 21st century. It is also estimated that 3.2 million people worldwide die every year from complications associated with it [2, 4]. Ongoing patient self-management, education, and support are critical to prevent acute complications and to reduce the risk of long-term complications from the disease [5]. Also adherence to recommended meal plans/dietary schemes and being active can keep blood glucose level, blood pressure, and cholesterol levels within optimum ranges [6]. It follows that non-adherence to recommended diet would lead to life-threatening complications in individuals with diabetes [2].
Compliance by individuals to their recommended dietary plan could be influenced by individuals, small social groups, communities, organizations, and policies [7]. Studies conducted in different geographical regions showed that dietary non-adherence was influenced by many factors. For example, receiving nutritional education [8], level of education, family support [9], gender, age, size of family [10], income, and occupation [11] were all associated with dietary non-adherence in individuals with diabetes. In addition, factors such as receiving information on a healthy diet, making good choices when eating out, financial constraints, knowledge about the disease, adequacy, and accuracy of dietary advice [12, 13], depression, limited food choices, availability of fruits and vegetables, and consideration of the affordability of foods [14] influenced individuals with diabetes to not comply with the recommended diet.
The magnitude of dietary non-adherence among individuals with DM varies among African countries e.g. 37% in Botswana, 24% in Nigeria, and 34% in Egypt [13, 15, 16]. Previous studies conducted in Ethiopia indicated that dietary non-adherence among individuals with diabetes ranged from 51% -55% [14, 17]. However, there is a scarcity of concrete evidence on the prevalence of dietary non-adherence of individuals with diabetes and the contributing factors in Ethiopia, specifically in the Northwest part of the country. Therefore, this study aims to assess the level of dietary non-adherence and associated factors among individuals with diabetes on-treatment follow up at Felege-Hiwot Referral Hospital (FHRH) in the Northwest part of Ethiopia.
2. Methods
2.1. Study design and settings
An institution-based cross-sectional study was conducted from March to April 2017 at FHRH in Ethiopia. This referral hospital is specifically located in Bahir Dar city, the capital of Amhara Regional State in the Northwest part of Ethiopia. It is a public hospital that provides health services for many of the people in that area of the country. It provides and promotes preventive, curative, and rehabilitative services to the community. In the outpatient and chronic follow up departments approximately 220 adult individuals with DM are seen weekly [18].
2.2. Study participants
All individuals with diabetes over 15 years old who visited the outpatient chronic department for follow up for at least one year were included in the study. However, those who were critically ill and unable to give a response during interview were not included.
2.3. Sample size determination and sampling procedure
The required sample size of the study was determined using a single population proportion formula:
The prevalence of dietary non-adherence among participating individuals with diabetes (P) was taken as 51.4% [14] and with the assumptions of a 95% confidence level and 5% margin of error. Based on this assumption and adding a 10% non-response rate, the final sample size was 404.
A systematic random sampling technique was employed to select the study participants from the total individuals with DM who had follow up during the data collection period (as recorded in the hospital's registration book). To find the sampling interval; K = N/n formula was used; where N is the total number of individuals with diabetes who had an appointment during the data collection period (880) and n is the calculated final sample size (404). Based on this, every second participant was interviewed until the required sample size was fulfilled. The first participant was selected randomly for interview by a lottery method.
2.4. Data collection procedures and quality control
Four trained (diploma) nurses through face-to-face interviews and medical chart review methods using an Amharic version of a structured questionnaire collected the data. The questionnaire contains socio-demographic, social support, clinical and nutrition recommendation related factors: measurements of wealth index were developed from the 2011 Ethiopian Demographic and Health Survey [19].
To determine the dietary non-adherence of individuals with DM, we used a modified form of the eight items Morisky medication adherence scale (MMAS-8) which was modified by Worku et al. [14]. This scale has 11 components and was computed by taking the mean value to classify the respondents' poor dietary practice as “dietary non-adherence” and good practice as “dietary adherence”.
Social support was measured using the Oslo-3 Social Support Scale (OSS-3) with three questions. The response categories were assessed independently for each of the three questions, and a sum score was created by summarizing the raw scores. The sum score scale ranging from 3 to 14 was then divided into “poor support” 3–8, “moderate support” 9–11, and “good support”12–14 [20].
To make the questionnaire easily understood by both the data collectors and respondents, the English version questionnaire was translated into Amharic (their mother tongue). Then it was translated back into English to check the consistency. The questionnaire was pre-tested among 20 individuals with DM at Debre-Tabor hospital. Based on the pre-test minor modifications were made to the questionnaire, such as editing or replacement of words that were not easily understood by the respondents. The principal investigator and two supervisors were responsible for monitoring the data collection process.
2.5. Data analysis
The collected quantitative data were coded and entered into the computer using Epi data version 3.1 was then exported into the Windows® Statistical Package for Social Science (SPSS) version 20 for analysis. The household wealth index was determined from asset data using principal component analysis (PCA). First, variables were coded between 0 and 1, and then the variables were entered and analyzed using PCA. Variables that had commonality values greater than 0.5 were used to produce factor scores. The resultant scores were computed to produce a common factor score, that was categorized into three groups (tertile) as (poor, middle, and rich). The frequencies, percentage, mean and standard deviation were presented using tables and graphs. Logistic regression was applied to determine the association between dependent and explanatory variables. Both bivariate and multivariable analysis were applied to determine factors affecting dietary non-adherence. Those independent variables at the p-value of 0.2 in the bivariate analysis were retained for the multivariable analysis. The degree of association was interpreted by using adjusted odds ratios with 95% confidence intervals and a p-value less than 0.05 was considered statistically significant.
2.6. Ethical approval and consent to participants
Ethical clearance was obtained from the University of Gondar Institute of Public Health review board committee. Permission and supportive letters were obtained from the respective hospital chief executive officer before data collection. Participation was voluntarily and information was collected anonymously after obtaining written informed consent from each respondent by assuring confidentiality throughout the data collection period.
3. Results
3.1. Socio-demographic characteristics of respondents
A total of 385 individuals with diabetes participated in this study with a response rate of 95.3%. Around seventy-five percent of the participants had type 2 DM. With regard to gender, 56.4% were male. The mean (±SD) age was 42.5 years (±15. 13). More than half of the participants (62.6%) were married and 29.1% were unable to read and write (Table1).
Table 1.
Socio-demographic characteristics of individuals with diabetes who were on treatment follow-up at FHRH, Bahirdar city, Northwest Ethiopia, 2017 (n = 385).
| Variables | Frequency | Percentage |
|---|---|---|
| Sex | ||
| Female | 168 | 43.6 |
| Male | 217 | 56.4 |
| Age in years | ||
| 15-30 | 108 | 28.1 |
| 30-60 | 232 | 60.3 |
| Above 60 | 45 | 11.7 |
| Marital status | ||
| Single | 102 | 26.5 |
| Married | 241 | 62.6 |
| Divorced | 26 | 6.8 |
| Widowed | 16 | 4.2 |
| Educational status | ||
| Unable to read and write | 112 | 29.1 |
| Able to read and write only | 73 | 19.0 |
| Grade 1-8 | 69 | 17.9 |
| Grade 9-12 | 50 | 13.0 |
| Diploma and above | 81 | 21.0 |
| Wealth status | ||
| Poor | 128 | 33.2 |
| Middle | 136 | 35.3 |
| Rich | 121 | 31.4 |
| Occupational status | ||
| Farmer | 81 | 21.0 |
| Civil servants | 136 | 35.3 |
| Merchant | 50 | 13.0 |
| Housewife | 65 | 16.9 |
| Day labourer | 53 | 13.8 |
3.2. Magnitude of dietary non-adherence among individuals with DM
The overall proportion of dietary non-adherence among diabetes patients who were on treatment follow up at FHRH during the study period was 46.8% [95% CI: (41.1, 52.0)]. The proportion of dietary non-adherence among type 2 DM and type 1 DM was almost the same 46.7% and 46.9, respectively. Dietary non-adherence was significantly decreased with an increase in the duration of diabetes. For instance, dietary non-adherence among DM individuals with less than 5 years duration was 52.6%, but non-adherence in individuals who lived with DM for more than 10 years was 22.0%. The proportion of dietary non-adherence was slightly higher in females (49.4%) than males (44.7%). Dietary non-adherence decreased with age increase (54.6% in 15–30 age, 45.7% in 31–60 age, and 33.3% in above 60 age groups). Of the total participants, 50.6% failed to include fruit in their meal plans (Table 2).
Table 2.
Magnitude of dietary practice of individuals with diabetes who were on treatment follow-up at FHRH, Bahir Dar city, Northwest Ethiopia, 2017 (n = 385).
| Variable | Frequency | Percent |
|---|---|---|
| Do you forget to plan the meals you eat ahead? | ||
| Yes | 148 | 38.4 |
| No | 237 | 61.6 |
| Have you missed dietary planning within the last 24 h | ||
| Yes | 186 | 48.3 |
| No | 199 | 51.7 |
| Over the past two weeks, were there any days when you did not adhere to your dietary plan properly? | ||
| Yes | 161 | 41.8 |
| No | 224 | 58.2 |
| Do you sometimes forget to comply with your dietary plan because of your day-to-day life activities? | ||
| Yes | 153 | 39.7 |
| No | 232 | 60.3 |
| When you feel like your DM is under control, do you sometimes stop complying with your dietary plan? | ||
| Yes | 111 | 28.8 |
| No | 274 | 71.2 |
| Are you encouraged to follow your dietary plan? | ||
| Yes | 231 | 60.0 |
| No | 154 | 40.0 |
| Did you feel of dietary deprivation? | ||
| Yes | 308 | 80.0 |
| No | 77 | 20.0 |
| Do you rigidly adhere to your dietary plan to control DM? | ||
| Yes | 199 | 51.7 |
| No | 186 | 48.3 |
| Do you feel to include fruits in your daily foodstuff? | ||
| Yes | 195 | 50.6 |
| No | 190 | 49.4 |
| Do you fail to include vegetables in your food daily? | ||
| Yes | 169 | 43.9 |
| No | 216 | 56.1 |
| Do you forget to reduce butter and fat intake in your food? | ||
| Yes | 152 | 39.5 |
| No | 233 | 60.5 |
3.3. Psychosocial, health, and information factors of dietary non-adherence among participants
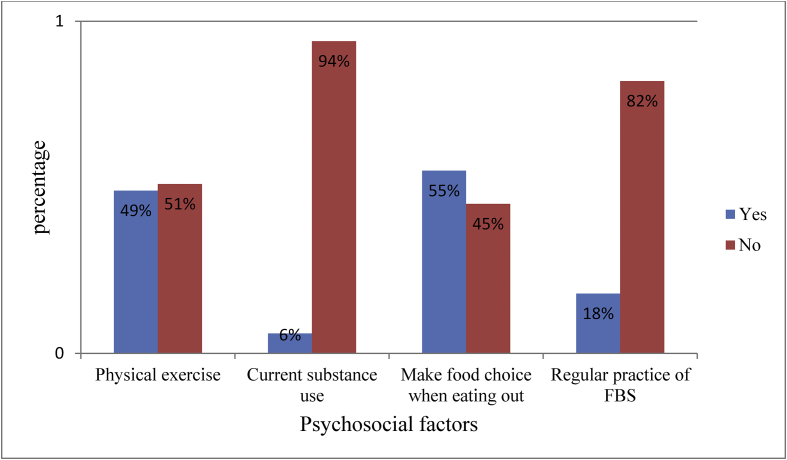
Of the 385 participants, 79.5% had no chronic co-morbidity that affected their dietary practices. Around 70% of participants had received nutritional education in the hospital, 32.7% received printed educational material on nutrition; 56.1% had poor social support, and 50.9% did not take regular physical exercises. In addition, 94% did not use any stimulant substance (khat or/and alcohol etc.), 81.8% did not have regular fast blood sugar (FBS) checks, and 55.3% made a choice when eating out (Table 3, Figure 1).
Table 3.
Psychosocial, health and information related characteristics of individuals with diabetes who were on treatment follow-up at FHRH, Bahir Dar city Northwest, Ethiopia 2017 (n = 385).
| Variables | Frequency | Percent |
|---|---|---|
| Duration of DM in years | ||
| <5 | 209 | 54.3 |
| 5-10 | 117 | 30.4 |
| >10 | 59 | 15.3 |
| Chronic diseases other than DM | ||
| Yes | 79 | 20.5 |
| No | 306 | 79.5 |
| Received nutritional education | ||
| Yes | 270 | 70.1 |
| No | 115 | 29.9 |
| Received printed nutritional education material | ||
| Yes | 126 | 32.7 |
| No | 259 | 67.3 |
| Received nutritional audio-visual nutrition education | ||
| Yes | 149 | 38.7 |
| No | 236 | 61.3 |
| Social support | ||
| Strong social support | 59 | 15.3 |
| Moderate social support | 110 | 28.6 |
| Poor social support | 216 | 56.1 |
Figure 1.
Psychosocial factors of dietary non-adherence among individuals with diabetes who are on treatment follow-up at FHRH, Bahir Dar city, Northwest Ethiopia, 2017.
3.4. Factors associated with dietary non-adherence among participants
The overall proportion of dietary non-adherence among participants was 46.8% (95% CI: 41.1–52.0). Dietary non-adherence was statistically significant with residency, duration of DM, nutritional education, making food choices when eating out, and social support. Individuals with diabetes who lived in rural areas were 3.75 times more likely to have dietary non-adherence than who lived in urban areas (AOR = 3.75; 95% CI: 2.12–6.63). Participants who had lived with diabetes for less than 5 years were 2.81 times more likely to have dietary non-adherence than those who had lived with diabetes for more than 10 years (AOR = 2.81; 95% CI: 1.22–6.50). Those who had not received nutritional education at the hospital were 5.88 times more likely to have dietary non-adherence than those who had received nutritional education (AOR = 5.88; 95% CI: 3.30–10.48). Participants who did not make good choice on food during eating out were 3.49 times more likely to have dietary non-adherence than their counterparts (AOR = 3.49; 95% CI: 2.09–5.81). Participants who had poor social support were 3.84 times more likely to have dietary non-adherence than those who had strong social support (AOR = 3.84; 95% CI: 1.74–8.46) (Table 4).
Table 4.
Bivariate and multivariable analysis of factors associated with dietary non-adherence of individuals with diabetes who are on treatment follow up at FHRH, Bahir Dar city, Northwest Ethiopia 2017.
| Variables | Dietary practice |
COR (95%CI) | AOR (95%CI) | |
|---|---|---|---|---|
| Poor | Good | |||
| Residence | ||||
| Urban | 103 | 172 | 1 | 1 |
| Rural | 77 | 33 | 3.90 (2.42–6.27) | 3.75 (2.12–6.63)∗∗ |
| Age in years | ||||
| 15-30 | 59 | 49 | 2.41 (1.17–4.98) | 1.28 (0.44–3.68) |
| 31-60 | 106 | 126 | 1.68 (0.86–3.30) | 1.48 (0.59–3.72) |
| >60 | 15 | 30 | 1 | 1 |
| Educational status | ||||
| Unable to read and write | 70 | 42 | 3.33 (1.83–6.07) | 1.81 (0.61–5.34) |
| Able to read and write | 37 | 36 | 2.06 (1.07–3.94) | 1.21 (0.43–3.39) |
| Grade 1-8 | 26 | 43 | 1.21 (0.62–2.37) | 1.28 (0.46–3.61) |
| Grade 9-12 | 20 | 30 | 1.33 (0.64–2.77) | 1.26 (0.49–3.18) |
| Diploma and above | 27 | 54 | 1 | 1 |
| Occupation | ||||
| Farmer | 57 | 24 | 1.82 (0.88–3.75) | 1.68 (0.54–5.17) |
| Civil servants | 45 | 91 | 0.38 (0.19–0.75) | 0.86 (0.32–2.32) |
| Merchant | 17 | 33 | 0.39 (0.18–0.88) | 0.87 (0.29–2.59) |
| Housewife | 31 | 34 | 0.70 (0.34–1.45) | 0.51 (0.18–1.45) |
| Day labourer | 30 | 23 | 1 | 1 |
| Wealth status | ||||
| Poor | 71 | 57 | 1.66 (0.85–3.27) | 0.84 (0.35–2.03) |
| Middle | 52 | 84 | 0.98 (0.51–1.90) | 0.73 (0.32–1.69) |
| Rich | 39 | 82 | 1 | 1 |
| Type of DM | ||||
| Type 1 | 67 | 62 | 1 | 1 |
| Type 2 | 113 | 143 | 0.73 (0.48–1.12) | 1.30 (0.70–2.43) |
| Duration of DM in years | ||||
| <5 | 110 | 99 | 3.93 (2.01–7.71) | 2.81 (1.21–6.50)∗ |
| 5-10 | 57 | 60 | 3.36 (1.65–6.87) | 2.79 (1.15–6.73)∗ |
| >10 | 13 | 46 | 1 | 1 |
| Received nutritional education | ||||
| No | 89 | 26 | 6.73 (4.07–11.15) | 5.88 (3.30–10.48)∗∗ |
| Yes | 91 | 179 | 1 | 1 |
| Performing physical exercise | ||||
| No | 118 | 78 | 3.10 (2.04–4.70) | 1.12 (0.64–1.96) |
| Yes | 62 | 127 | 1 | 1 |
| Make choice when eating out | ||||
| No | 113 | 59 | 4.17 (2.72–6.40) | 3.49 (2.09–5.83)∗∗ |
| Yes | 67 | 146 | 1 | 1 |
| Social support | ||||
| Strong social support | 13 | 46 | 1 | 1 |
| Moderate social support | 40 | 70 | 2.02 (0.98–4.19) | 2.09 (0.90–4.86) |
| Poor social support | 1 27 | 89 | 5.05 (2.58–9.89) | 3.84 (1.74–8.46)∗∗ |
Abbreviations: COR: Crude Odds Ratio; AOR: Adjusted Odds Ratio; CI: Confidence Interval; DM = diabetes Miletus.
Note: ∗ = p-value<0.05, ∗∗ = p-value < 0.01.
4. Discussion
We assessed the dietary non-adherence and associated factors among diabetes patients who were on treatment follow up at Felege Hiwot Referral Hospital outpatient department. The study findings would contribute in part to improving dietary adherence by the participants, it will identify opportunities and constraints to the health professionals and policy makers who are addressing dietary non-adherence barriers proactively, and in designing effective dietary practice guidelines to policymakers.
In this study, the overall proportion of dietary non-adherence was 46.8% (95% CI: 41.8–51.9). This is in line with similar studies conducted in Addis Ababa, Ethiopia [14], and in other countries such as United Arab Emirates [21], India [22], and Saudi Arabia [23]. On the contrary, the findings differ from studies conducted in Egypt, Ghana, and Botswana [13, 16, 24]. This discrepancy might be due to social, economic, and cultural characteristic differences, and participants' understanding and perceptions about the role of diet [10, 25].
Individuals who evinced non-adherence to the recommended diet is influenced by many factors emanated from individuals, small groups, communities, organizations, and policies [7]. In this study, non-adherence to the recommended diet was significantly associated with nutritional education, the making of good choices when eating out, duration of DM, social support, and participants' residency factors.
We found that nutrition education given at the hospital was strongly associated with dietary adherence. This was in agreement with studies conducted in Addis Ababa (Ethiopia) [14], China [8], India [22], Botswana [13], and South Africa [26]. This is because individuals with diabetes would did not receive information (recommendations) on healthier diets and the importance of nutrition in the management of their diabetes, they would not be aware of the need follow the dietary guidelines given to them. They would only eat what is available in their home and/or because of fear of increased blood glucose, they may abstain from eating [8, 27].
Not making good food choices when eating out was identified as a second factor linked to poor dietary practice. This variable was also associated with poor dietary practice among individuals with diabetes in studies conducted in Addis Ababa (Ethiopia) and Botswana [13, 14]. Individuals with diabetes may not always get the foods they are recommended to consume when they eat out of their homes. The recommend foodstuff may not be available or affordable when they eat out in places or at events such as restaurants, social gatherings, and the homes of extended families and friends [28].
In our study, the level of social support was strongly associated with consequent level of the dietary non-adherence of shown by participants, which was consistent with similar studies carried out in Niger and Bahrain [9, 29]. This might be due to depression if they do not receive support from their family or wider social group, their depression may cause neglect of their dietary meal plan. Individuals with diabetes might develop behaviors like stress, isolation, frustration, anger, and guilt when they do not get support from close social networks. These behavioral might make them not care about the diet they consume [28, 30, 31]. However, positive feedback from supportive people can encourage one's self-motivation to do something [32].
The duration of diabetes was identified as a third factor contributing to dietary non-adherence among individuals with diabetes involved in this study. Individuals with diabetes that lived shorter time with the disease were more likely to not adhere to their diet. This is similar to a study conducted in northwest Iran [33]. This is in part because that they may be challenged to understand the disease condition, negative emotion, time pressure, and competing priorities to adhere to the recommended foodstuff and begin consuming what they easily get and their preference to adhere to the recommended foodstuffs may be impossible [28].
A further factor was that participants who lived in rural areas were more likely to non-adhere to the recommended diet than those who lived in urban areas. However, previous studies reported that residency was not significantly associated with the dietary non-adherence of individuals with diabetes [9, 14]. This could be explained by the reason that those who lived in rural areas might not be getting enough information, unlike urban participants who have more access to information. Most individuals who lived in rural areas and participated in this study were unable to read and write so, they could not use the information on the printed materials. In addition, participants who came from rural areas had a minimal perception of the linkage between their health and their diet.
Although we utilized our best efforts to find good quality data, these findings have some limitations. The first was a social desirability bias, which could lead to inaccurate findings. Also since we employed a cross-sectional study design method, the direction of causal relationships between variables cannot always be determined.
5. Conclusion and recommendation
Our study revealed that nearly half of the participants involved in this study did not follow their recommended dietary plan. Nutrition education, duration of DM, social support, making good choices when eating out, and residency were significantly associated with the status of dietary adherence. The findings indicate the need to focus on integrated intervention on nutritional education, social bonding, and meal planning when eating out. Therefore, we recommend the inclusion of a brief intervention strategy for nutritional education provision and the establishment of a nutrition-counseling unit for individuals with diabetes at the hospital. We also recommend conducting further population-based research to explore factors associated with poor dietary practice for better management of DM. Conducting a study using longitudinal study design, estimation of portion size of individuals' diet and repeated 24-hour recall is also necessary.
Declarations
Author contribution statement
M. Bayih and T. Woldegiorgis: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
M. Birhanu and T. Shibabaw: Analyzed and interpreted the data; Wrote the paper.
S. Tadesse and H. Woldie: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We would like to offer our in-depth gratitude to the data collectors, participants, and hospital workers, especially those who work in diabetes follow up outpatient departments for their support. We also acknowledge University of Gondar for financial support to collect the data. Our great thanks goes to Bernard Stewart and Christopher Stewart for thier support by editing the language through the manuscript.
References
- 1.International Diabetes Federation . ninth ed. 2019. IDF Diabetes Atlas. [Google Scholar]
- 2.Sicree R., Shaw J., Zimmet P., Heart B. 2010. The Global burden. Diabetes and Impaired Glucose Tolerance Baker IDI Heart and Diabetes Institute. [Google Scholar]
- 3.Roglic G., editor. Global Report on Diabetes. World Health Organization; 2016. [Google Scholar]
- 4.IDF, editor. The International Diabetes Federation Consensus Worldwide Definition of the Metabolic Syndrome. The International Diabetes Federation; 2006. [Google Scholar]
- 5.Bantle J.P., Wylie-Rosett J., Albright A.L., Apovian C.M., Clark N.G., Franz M.J. 2008. Nutrition Recommendations and Interventions for Diabetes: a Position Statement of the American Diabetes Association. [DOI] [PubMed] [Google Scholar]
- 6.American Diabetes Association Standards of medical care in diabetes—2016: summary of revisions. Diabetes Care. 2016 Jan 1;39(Supplement 1):S4–5. doi: 10.2337/dc16-S003. [DOI] [PubMed] [Google Scholar]
- 7.Ebrahim Z., De Villiers A., Ahmed T. Factors influencing adherence to dietary guidelines: a qualitative study on the experiences of patients with type 2 diabetes attending a clinic in Cape Town. J. Endocrinol. Metabol. Diabetes S. Afr. 2014;19(2):76–84. [Google Scholar]
- 8.Wang H., Song Z., Ba Y., Zhu L., Wen Y. Nutritional and eating education improves knowledge and practice of patients with type 2 diabetes concerning dietary intake and blood glucose control in an outlying city of China. Publ. Health Nutr. 2014;17(10):2351–2358. doi: 10.1017/S1368980013002735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shamsi N., Shehab Z., AlNahash Z., AlMuhanadi S., Al-Nasir F. Factors influencing dietary practice among type 2 diabetics. Bahrain Med. Bull. 2013;158(749):1–6. [Google Scholar]
- 10.Parajuli J., Saleh F., Thapa N., Ali L. Factors associated with nonadherence to diet and physical activity among Nepalese type 2 diabetes patients; a cross sectional study. BMC Res. Notes. 2014;7(1):758. doi: 10.1186/1756-0500-7-758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tiew K.F., Chan Y.M., Lye M.S., Loke S.C. Factors associated with dietary diversity score among individuals with type 2 diabetes mellitus. J. Health Popul. Nutr. 2014;32(4):665. [PMC free article] [PubMed] [Google Scholar]
- 12.Nthangeni G., Steyn N.P., Alberts M., Steyn K., Levitt N.S., Laubscher R. Dietary intake and barriers to dietary compliance in black type 2 diabetic patients attending primary health-care services. Publ. Health Nutr. 2002;5(2):329–338. doi: 10.1079/PHN2002256. [DOI] [PubMed] [Google Scholar]
- 13.Ganiyu A.B., Mabuza L.H., Malete N.H., Govender I., Ogunbanjo G.A. Non-adherence to diet and exercise recommendations amongst patients with type 2 diabetes mellitus attending Extension II Clinic in Botswana. Afr. J. Prim. Health Care Fam. Med. 2013;5(1) [Google Scholar]
- 14.Worku A., Abebe S.M., Wassie M.M. Dietary practice and associated factors among type 2 diabetic patients: a cross sectional hospital based study, Addis Ababa, Ethiopia. SpringerPlus. 2015;4(1):15. doi: 10.1186/s40064-015-0785-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Isara A., Omonigho L., Olaoye D. Non-medical management practices for type 2 diabetes in a teaching hospital in southern Nigeria. Afr. J. Diabetes Med. 2014;22(2) [Google Scholar]
- 16.Mahfouz E.M., Awadalla H.I. Compliance to diabetes self-management in rural El-Mina, Egypt. Cent. Eur. J. Publ. Health. 2011;19(1):35. doi: 10.21101/cejph.a3573. [DOI] [PubMed] [Google Scholar]
- 17.Hailu E., Mariam W.H., Belachew T., Birhanu Z. Self-care practice and glycaemic control amongst adults with diabetes at the Jimma University Specialized Hospital in south-west Ethiopia: a cross-sectional study. Afr. J. Prim. Health Care Fam. Med. 2012;4(1) [Google Scholar]
- 18.Felege- Hiwot Referal Hospital . 2017. Six Month Performance Report. [Google Scholar]
- 19.Icf CS . 2012. Ethiopian demographic health survey 2011. Addis Ababa and calverton: central statistical agency (Ethiopia) and ICF International; pp. 17–27. [Google Scholar]
- 20.Dalgard O.S., Dowrick C., Lehtinen V., Vazquez-Barquero J.L., Casey P., Wilkinson G. Negative life events, social support and gender difference in depression. Soc. Psychiatr. Psychiatr. Epidemiol. 2006;41(6):444–451. doi: 10.1007/s00127-006-0051-5. [DOI] [PubMed] [Google Scholar]
- 21.Al-Kaabi J., Al-Maskari F., Saadi H., Afandi B., Parkar H., Nagelkerke N. Assessment of dietary practice among diabetic patients in the United Arab Emirates. The review of diabetic studies. Reg. Dev. Stud. 2008;5(2):110. doi: 10.1900/RDS.2008.5.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chacko M., Begum K. Dietary practices among type 2 diabetic patients-A cross-sectional study from a major city in India. Int. J. Health Sci. Res. 2016;6(4):370–377. [Google Scholar]
- 23.Mohamed B.A., Almajwal A.M., Saeed A.A., Bani I.A. Dietary practices among patients with type 2 diabetes in Riyadh, Saudi Arabia. J. Food Agric. Environ. 2013;11(2):110–114. [Google Scholar]
- 24.Nti C.A., Arthur D., Opare-Obisaw C. Relationship between dietary practices, physical activity and body mass indices of type 2 diabetics attending a clinic in Accra, Ghana. J. Publ. Health Epidemiol. 2016;8(4):60–66. [Google Scholar]
- 25.Alsairafi Z.K., Taylor K.M.G., Smith F.J., Alattar A.T. Patients’ management of type 2 diabetes in Middle Eastern countries: review of studies. Patient Prefer. Adherence. 2016;10:1051. doi: 10.2147/PPA.S104335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ralineba T., Netshikweta M.L., Shilubane N.H. Knowledge and practices associated with diabetes among patients with chronic diabetes mellitus in rural areas of Vhembe District, Limpopo Province, South Africa. J. Hum. Ecol. 2015 Jul 1;51(1-2):193–201. [Google Scholar]
- 27.Glanz K. Nutrition education for risk factor reduction and patient education: a review. Prev. Med. 1985;14(6):721–752. doi: 10.1016/0091-7435(85)90069-6. [DOI] [PubMed] [Google Scholar]
- 28.Schlundt D.G., Rea M.R., Kline S.S., Pichert J.W. Situational obstacles to dietary adherence for adults with diabetes. J. Am. Diet Assoc. 1994;94(8):874–879. doi: 10.1016/0002-8223(94)92367-1. [DOI] [PubMed] [Google Scholar]
- 29.Uchenna O., Ijeoma E., Pauline E., Sylvester O. Contributory factors to diabetes dietary regimen non adherence in adults with diabetes. World Acad. Sci. Eng. Technol. 2010;4(9):644–651. [Google Scholar]
- 30.Brownell K.D., Cohen L.R. Adherence to dietary regimens 2: components of effective interventions. Behav. Med. 1995;20(4):155–164. doi: 10.1080/08964289.1995.9933732. [DOI] [PubMed] [Google Scholar]
- 31.Glasgow R.E., Toobert D.J. Social environment and regimen adherence among type II diabetic patients. Diabetes Care. 1988;11(5):377–386. doi: 10.2337/diacare.11.5.377. [DOI] [PubMed] [Google Scholar]
- 32.Sherman A.M., Bowen D.J., Vitolins M., Perri M.G., Rosal M.C., Sevick M.A. Dietary adherence: characteristics and interventions. Contr. Clin. Trials. 2000;21(5):S206–S211. doi: 10.1016/s0197-2456(00)00080-5. [DOI] [PubMed] [Google Scholar]
- 33.Yekta Z., Pourali R., Aghassi M.R., Ashragh N., Ravanyar L., Rahim P.M.Y. 2011. Assessment of Self-Care Practice and its Associated Factors Among Diabetic Patients in Urban Area of Urmia, Northwest of Iran. [PubMed] [Google Scholar]