Abstract
A 78 year-old female presented with dropped head syndrome (DHS). Three months before her initial visit to our hospital, the patient noticed a pronounced flexion of her head and neck with subsequent deterioration of symptoms, which included neck pain, difficulty with forward gaze, and gait disturbance. Cervical radiographs demonstrated scoliotic and kyphotic changes, and her symptom deteriorated over time, especially in the standing position. Duloxetine was administered for her low back pain because nonsteroidal anti-inflammatory drugs deemed ineffective. The patient demonstrated marked improvements in both radiographic and clinical appearances after 4 months. Her neck pain decreased from 8 to 2 out of 10 in the Numeric Rating Scale, and her symptoms such as difficulty with forward gaze and gait disturbance had also resolved. Duloxetine is a serotonin noradrenaline reuptake inhibitor that is usually used for chronic musculoskeletal pain, neuropathic pain, or depression. In this report, we present another potential application of duloxetine in the treatment of DHS. The following possibilities were considered for the improved outcomes: (1) pain relief may have helped the patient feel comfortable enough to move her neck, and (2) we suppose that serotonin and noradrenaline reuptake may contribute to the improvement of DHS, because there might be a potential disequilibrium of neurotransmitters such as serotonin, dopamine and noradrenaline in DHS patients. Although further investigation is needed to clarify the mechanism, duloxetine should be considered as one of the optional treatments for DHS.
Keywords: Neuroscience, Pharmaceutical science, Aging, Musculoskeletal system, Neurology, Clinical research, Dropped head syndrome, Duloxetine, Serotonin noradrenaline reuptake inhibitor
Neuroscience; Pharmaceutical science; Aging; Musculoskeletal system; Neurology; Clinical research; Dropped head syndrome; Duloxetine; Serotonin noradrenaline reuptake inhibitor.
1. Introduction
Dropped head syndrome (DHS) is a rare condition that most commonly occurs in the seventh decade of life [1]. A growing number of patients with DHS must be managed by clinicians due to an aging population. Symptoms of DHS are neck pain, gait disturbance due to impaired forward gaze and, in some cases, the development of dysphagia. The etiologies of DHS include neuromuscular or autoimmune diseases; however, the majority of patients only present with cervical muscle weakness without any causative disease, and this condition is defined as isolated neck extensor myopathy (INEM) [2]. Because the pathomechanism of INEM is still unknown, there has been no specific treatment or medication for INEM.
Duloxetine, which is a serotonin noradrenaline reuptake inhibitor (SNRI), is usually used for chronic musculoskeletal pain, neuropathic pain, or depression [3, 4]. In this report, we present another potential application of duloxetine in the treatment of DHS. A patient with DHS markedly improved both clinical and radiographic outcomes following duloxetine use.
2. Case report
A 78 year-old female presented with DHS. Three months before her initial visit to our hospital, the patient noticed a pronounced flexion of her head and neck with subsequent deterioration of symptoms. Although the patient had a history of hypertension and dementia, there was no change in her daily medication. She complained of neck pain, difficulty with forward gaze, and gait disturbance; however, she did not have dysphagia. The patient denied any neurological deficit such as motor weakness or loss of sensation in her bilateral upper and lower extremities. No neuromuscular or autoimmune diseases were noted.
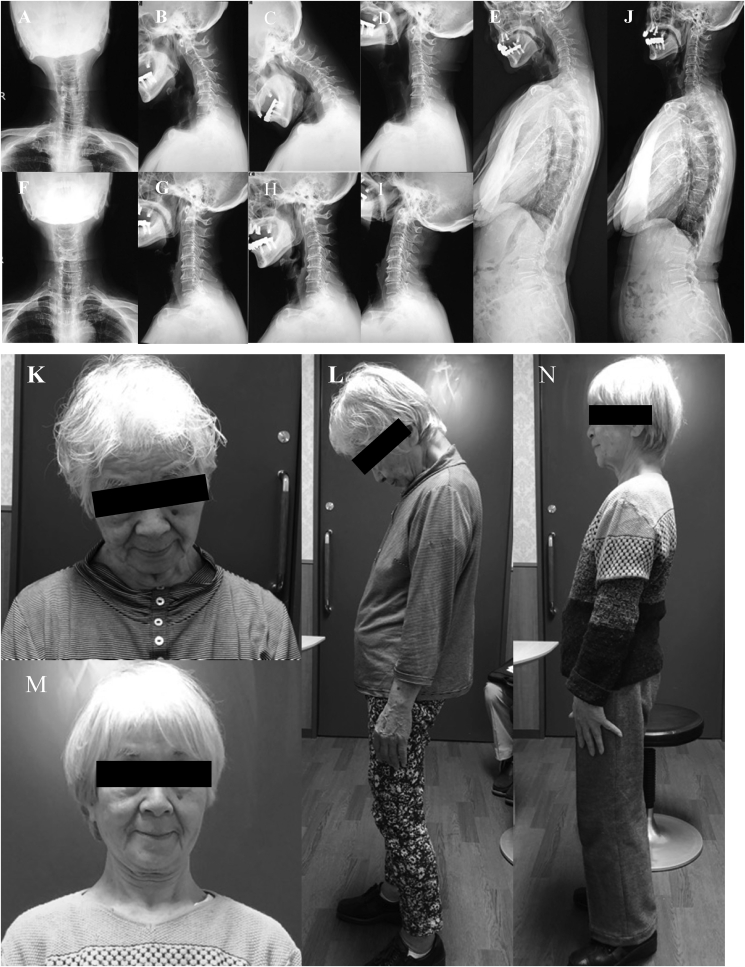
Her cervical radiographs demonstrated scoliotic and kyphotic changes in her cervical spine (Figure 1A–E). Her symptoms deteriorated over time, especially in the standing position (Figure 1K,L). Duloxetine was initially administered at 20 mg per day, because she also complained of low back pain and stated that nonsteroidal anti-inflammatory drugs did not alleviate her symptoms at all. She experienced some improvement in neck pain and head drop following duloxetine use. Therefore, the duloxetine dose was increased from 20 to 40 mg per day at 2 months after her initial visit. There was marked improvement in both radiographic (Figure 1F–J) and clinical (Figure 1M,N) appearances after 4 months. Her neck pain decreased from 8 to 2 out of 10 in the Numeric Rating Scale, and her symptoms such as difficulty with forward gaze and gait disturbance had also resolved. The patient did not experience any side effects, such as nausea, dizziness, somnolence, or constipation. And, her serum electrolyte levels were within normal range during follow-up.
Figure 1.
Initial radiographs. (A) A-P view, (B) lateral view on neutral, (C) lateral view on flexion, (D) lateral view on extension, (E) lateral view on standing radiograph. Radiographs at 6-month follow-up; (F) A-P view (G) lateral view on neutral (H) lateral view on flexion (I) lateral view on extension, (J) lateral view on standing radiograph. Initial appearance; (K) front view, (L) lateral view. Appearance at 6-month follow-up; (M) front view, (N) lateral view.
This case report follows the CARE case report guidelines 2013.
2.1. IRB approval/Research Ethics Committee
A single case report is exempt from ethical approval in our institution. Written informed consent was obtained from the patient for publication of this report and the accompanying images.
3. Discussion
The management of DHS has always been challenging for clinicians, since the pathomechanism of INEM remains unclear with no standardized treatment. The daily life of a patient may become restricted as a result of impaired forward gaze, gait disturbance, and neck pain with or without dysphagia. Flexion deformity of the head and neck can be corrected passively; however, patients are unable to keep their head upright when sitting or standing due to weakness of the cervical paraspinal muscles. Bracing and steroid injections have been described as a first-line treatment in INEM [5, 6]. However, these treatments sometimes fail, and no specific medication has been identified for the treatment of INEM. The etiologies of DHS in the literature include neurological diseases such as Parkinson's disease and autoimmune diseases such as polymyositis [7]. These conditions can be treated by medication according to their own disease. However, the majority of patients are diagnosed with INEM without any neuromuscular disease or inflammatory myopathy [1].
Duloxetine is an SNRI that inhibits the reuptake of serotonin and noradrenaline, which are neurotransmitters in the descending pain inhibitory pathways. Although the exact mechanism is unknown, duloxetine may increase synaptic cleft levels of neurotransmitters in spinal and supraspinal pathways, resulting in the activation of descending pain inhibitory pathways with an analgesic effect [8]. Therefore, duloxetine is usually applied to chronic musculoskeletal or neuropathic pain [3].
Duloxetine is also known as an antidepressant for depressive symptoms [4]. Furthermore, Morgante and Fasano reported a 58-year-old patient with primary progressive freezing of gait, and the patient showed a remarkable response to duloxetine [9]. They suggested that the effect of duloxetine on freezing of gait was not related to antidepressant action, because switching to s-citalopram caused a severe recurrence of freezing of gait without any worsening of mood. Previous reports suggested that the effect of duloxetine on gait disorders might result from enhancement of both noradrenergic and serotoninergic transmission [9, 10].
In this report, the patient with DHS showed marked improvements in both radiographic and clinical outcomes following duloxetine use, and we also experienced 4 other cases that were treated successfully by duloxetine. The following possibilities were considered for the improved outcomes: (1) pain relief may have helped the patient feel comfortable enough to move her neck with increased range of neck motion, and (2) serotonin and noradrenaline reuptake may have been induced by duloxetine. We suppose that serotonin and noradrenaline reuptake may contribute to the improvement of DHS, because there might be a potential disequilibrium of neurotransmitters such as serotonin, dopamine and noradrenaline in DHS patients. Side effects of duloxetine were reported in the literatures, such as somnolence, constipation, nausea, dizziness, and dry mouth [11]. Falls, hyponatremia, and discontinuation syndrome were also reported [12, 13]. These side effects and adverse events should be carefully monitored especially in the elderly patients.
To date, there is no specific medication for the treatment of DHS. Although further investigation is needed in animal studies or larger case series to clarify the mechanism, duloxetine should be considered as one of the optional treatments for DHS.
Declarations
Author Contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
None.
References
- 1.Drain J.P., Virk S.S., Jain N., Yu E. Dropped head syndrome: a systematic review. Clin. Spine. Surg. 2019;32(10):423–429. doi: 10.1097/BSD.0000000000000811. [DOI] [PubMed] [Google Scholar]
- 2.Katz J.S., Wolfe G.I., Burns D.K., Bryan W.W., Fleckenstein J.L., Barohn R.J. Isolated neck extensor myopathy: a common cause of dropped head syndrome. Neurology. 1996;46:917–921. doi: 10.1212/wnl.46.4.917. [DOI] [PubMed] [Google Scholar]
- 3.Pergolizzi J.V., Jr., Raffa R.B., Taylor R., Jr., Rodriguez G., Nalamachu S., Langley P. A review of duloxetine 60 mg once-daily dosing for the management of diabetic peripheral neuropathic pain, fibromyalgia, and chronic musculoskeletal pain due to chronic osteoarthritis pain and low back pain. Pain Pract. 2013;13:239–252. doi: 10.1111/j.1533-2500.2012.00578.x. [DOI] [PubMed] [Google Scholar]
- 4.Richard I.H., McDermott M.P., Kurlan R. A randomized, double-blind, placebo-controlled trial of antidepressants in Parkinson disease. Neurology. 2012;78:1229–1236. doi: 10.1212/WNL.0b013e3182516244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gourie-Devi eM., Nalini A., Sandhya S. Early or late appearance of “dropped head syndrome” in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry. 2003;74:683–686. doi: 10.1136/jnnp.74.5.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finsterer J., Frank M., Krexner E. Steroid-responsive dropped-head syndrome due to polymyositis. Joint Bone Spine. 2010;77:485–486. doi: 10.1016/j.jbspin.2010.02.028. [DOI] [PubMed] [Google Scholar]
- 7.Sharan A.D., Kaye D., Charles Malveaux W.M., Riew K.D. Dropped head syndrome: etiology and management. J. Am. Acad. Orthop. Surg. 2012;20:766–774. doi: 10.5435/JAAOS-20-12-766. [DOI] [PubMed] [Google Scholar]
- 8.Jones C.K., Peters S.C., Shannon H.E. Efficacy of duloxetine, a potent and balanced serotonergic and noradrenergic reuptake inhibitor, in inflammatory and acute pain models in rodents. J. Pharmacol. Exp. Therapeut. 2005;312:726–732. doi: 10.1124/jpet.104.075960. [DOI] [PubMed] [Google Scholar]
- 9.Morgante F., Fasano A. Improvement with duloxetine in primary progressive freezing gait. Neurology. 2010;75:2130–2132. doi: 10.1212/WNL.0b013e318200d7a3. [DOI] [PubMed] [Google Scholar]
- 10.Devos D., Defebvre L., Bordet R. Dopaminergic and nondopaminergic pharmacological hypotheses for gait disorders in Parkinson’s disease. Fundam. Clin. Pharmacol. 2010;24:407–421. doi: 10.1111/j.1472-8206.2009.00798.x. [DOI] [PubMed] [Google Scholar]
- 11.Konno S., Oda N., Ochiai T., Alev L. Randomized, double-blind, placebo-controlled phase III trial of duloxetine monotherapy in Japanese patients with chronic low back pain. Spine. 2016;41(22):1709–1717. doi: 10.1097/BRS.0000000000001707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takayama A., Nagamine T., Matsumoto Y., Nakamura M. Duloxetine and angiotensin ii receptor blocker combination potentially induce severe hyponatremia in an elderly woman. Intern. Med. 2019;58(12):1791–1794. doi: 10.2169/internalmedicine.2059-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagamine T. Responsibility of the doctor who prescribes serotonin and noradrenaline reuptake inhibitors for patients with chronic musculoskeletal pain. Psychiatr. Clin. Neurosci. 2018;72(1):45–46. doi: 10.1111/pcn.12612. [DOI] [PubMed] [Google Scholar]