Abstract
Background
Left ventricular assist device (LVAD) patients are vulnerable to over-utilization of resources.
Methods and results
We explored the pattern of emergency department (ED) presentations of LVAD patients and their costs compared with non-LVAD heart failure patients. ED visits between 7/2008 and 7/2017 were reviewed to identify 145 LVAD patients, and 435 patients with known heart failure were selected using propensity score matching for age and sex. ED evaluation metrics, hospitalization cost, and length of stay (LOS) were analyzed. Although the most common ED presentations and their frequency differed between groups, few were LVAD specific. LVAD patients were more likely to have taken personal vehicles or be flown to the ED. They had similar times to triage, rooming, and physician evaluation compared with non-LVAD patients. However, LVAD patients were noted to have a shorter time from physician assessment to disposition (109.8 min vs. 177.0 min, p < 0.001) and, overall, LVAD patients had shorter ED LOS (6.33 vs. 9.82 hrs, p = 0.0001). For patients admitted, no significant difference was found between groups in hospital LOS (6.67 vs 6.58 days, p = 0.928) or total cost ($28,766 vs $21,524, p = 0.087).
Conclusion
Shorter disposition times without increases in LOS or costs may identify a created healthcare disparity among LVAD patients.
Keywords: Left ventricular assist device, Heart failure, Healthcare utilization, Cost, Hospitalization
1. Introduction
Patients with end-stage heart failure (HF) are increasingly implanted with left ventricular assist devices (LVADs) as a bridge patients to transplantation (BTT) or as long-term therapy for those who are not candidates for transplantation (destination therapy, DT). This has resulted in a tremendous reduction in mortality advantage, with 1-year survival now >80% regardless of device type [1]. Despite advancements in survival, these devices are commonly associated with complications including bleeding, infection, stroke, and device malfunction. As the median life expectancy after LVAD implantation continues to increase, with 55% survival at 48 months on device support in the most recent registry analysis, the hazard of LVAD-specific complications will continue to be burdensome [2]. Therefore, how these patients interface with the medical system, and in particular their need for urgent and emergent care, is an issue of increasing importance.
Emergency department (ED) utilization by LVAD patients has emerged as a unique aspect of emergency medicine. The presence of an LVAD may lead to a form of framing bias wherein providers fixate on the LVAD to the neglect of non-LVAD related chief complaints. Therefore, the presence of an LVAD potentially represents a created healthcare disparity that may affect provider attention, alter established practice patterns, and result in misuse of healthcare resources. In this study, we review the pattern of ED presentations of LVAD patients, metrics of their ED evaluation, and the respective cost of hospitalizations compared with those of non-LVAD HF patients.
2. Methods
2.1. Overview
This is a retrospective, observational study of clinical data in the electronic medical records of HF patients presenting to our institution’s academic ED.
2.2. Study design
The study population included adults aged ≥18 years with an ED encounter between July 2008 and July 2017. Utilizing ICD9 and ICD 10 codes, our institution’s Integrated Data Repository (IDR) identified HF patients (ICD9 428 and ICD10 I50) as well as those with an LVAD (ICD9 V43.21 and Z95.811). Using a propensity score logistic regression model for age and sex, every LVAD patient was matched to 3 non-LVAD patients as randomly selected by the computer from a pool of HF patients (mismatch tolerance 0). ED triage metrics and total hospitalization cost were collected and analyzed. Repeated ED visits by the same patient were treated as separate cases. Direct hospital–to–hospital transfers were not included, unless it was an ED–ED transfer.
2.3. Human subjects protection
This study was approved by our Institutional Review Board, which waived the requirement of informed consent as the analysis included only de-identified data.
2.4. Settings and population
The ED houses 70 beds with an annual volume over 110,000 patient visits. Our institution serves as a regional LVAD implant center with an average annual implant volume of 35 LVADs, with a hotline available for LVAD patients to contact an on-call certified LVAD provider at any time. All LVAD patients, by protocol, are seen in clinic within 72 h of implant discharge, at 1 week, 4 weeks, and if stable, at 3-month intervals thereafter. At the time of analysis, our LVAD program was managing 90 ambulatory out-patient LVADs. The hospital is a level 1 trauma and critical care center, serving as a regional quaternary receiving center for transplant, trauma, burn, and complex critically ill patients.
2.5. Data collection
Baseline demographics including age at encounter, sex, race, and ethnicity were retrieved from electronic medical records of included patients. ED encounter variables such as chief complaint, diagnosis, and disposition were obtained. ED evaluation metrics included time-to-room, time-to-MD, and total ED LOS. Additionally, for admitted patients, hospital LOS, hospital disposition, and total cost of hospitalization were extracted. Data regarding past medical history, previous number of ED encounters and hospitalizations, current medications, and ED interventions during this encounter (including results of labs and imaging) were abstracted by a team of four physicians. After initial data extraction, two individuals, a fellow and research associate, examined abstracted records for inaccuracies.
2.6. Outcomes of interest
ED measures of health utilization metrics were grouped into three categories. The first category described the pattern of clinical presentation including mode of transfer, and chief complaint. The second examined timeliness of ED evaluation, which included time from arrival to room, physician assessment, ED disposition orders, and total ED LOS. The third category compared groups by rates of admissions from the ED, in-patient length of stay (LOS) and total cost of the hospital encounter.
2.7. Statistical analysis
All clinical data were extracted from the REDCap (Research Electronic Data Capture, University of Florida, Gainesville, FL) to Stata (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC). Descriptive statistics (means, frequencies, and percentages) and inferential tests (the independent t test, Chi-square test, and Fisher exact test) were used to examine the relationships between the outcome variable and the covariates. All p-values were from two-sided tests, and results were deemed statistically significant at P < 0.05.
3. Results
One-hundred forty-five LVAD patient visits were discovered, and using a dataset of 9461 HF patient visits without the presence of an LVAD, a propensity score using logistic regression model for age and sex was conducted for each patient. Each visit was matched in a ratio of 1:3 to ED encounters for non-LVAD HF patients (HF group), providing a total cohort of 580. Population demographics are presented in Table 1. Mean duration of LVAD support was 2 years. Ninety one percent had a HeartMate II device, with all others being supported with a HeartWare HVAD, with 66% of patients being destination therapy. The vast majority of both groups presented to the ED from home, however the route of transportation differed significantly with more LVAD patients being transported via air (5.48% vs 1.38%, p < 0.001). Additionally, while the distribution of chief complaints differed between groups, the predominance of presentations to the ED in the LVAD group was not readily attributable to their device. LVAD patients were noted, however, to have a higher incidence of bleeding or altered mentation bringing them to the ED, to which their device may have contributed (Table 1). Of note, no patients in the LVAD group required any surgical interventions as a result of their ED presentation.
Table 1.
Patient characteristics.
| Characteristics | Heart failure, (n = 435) | LVAD (n = 145) | Total (n = 580) | p-value |
|---|---|---|---|---|
| Age in years, mean (SD) | 57.29 (14.27) | 57.53 (14.16) | 57.35 (14.23) | 0.858 |
| Race, n (%) | ||||
| White | 260 (59.8) | 104 (71.23) | 364 (62.76) | 0.014 |
| African American | 148 (34.10) | 28 (19.18) | 176 (30.34) | 0.010 |
| Other | 26 (5.99) | 14 (9.59) | 40 (6.90) | 0.562 |
| Sex, n (%) | 0.914 | |||
| Women | 88 (20.28) | 29 (19.86) | 117 (20.17) | 0.99 |
| Men | 346 (79.72) | 117 (80.14) | 463 (79.83) | 0.99 |
| Prior Location (before coming to ED) | ||||
| Home | 309 (72.03) | 102 (70.34) | 411 (71.60) | 0.759 |
| Skilled nursing facility | 28 (6.53) | 3 (2.07) | 31 (5.40) | 0.053 |
| Long-term acute care facility | 5 (1.17) | 1 (0.69) | 6 (1.05) | 0.063 |
| Public place | 33 (7.69) | 9 (6.21) | 42 (7.32) | 0.562 |
| Unknown | 15 (3.50) | 0 | 15 (2.61) | 0.016 |
| ED-ED transfer | 39 (9.09) | 30 (20.69) | 69 (12.02) | <0.001 |
| Route to ED | ||||
| Ambulance | 238 (54.84) | 53 (36.3) | 291 (50.17) | <0.001 |
| Personal vehicle | 160 (36.87) | 71 (48.63) | 231 (39.83) | 0.012 |
| Air | 6 (1.38) | 8 (5.48) | 14 (2.14) | 0.005 |
| Others | 30 (6.91) | 14 (9.59) | 44 (7.59) | 0.291 |
| Chief complaint | ||||
| Altered mentation, fatigue, malaise, headache/ dizziness, falls | 65 (14.98) | 35 (23.97) | 100 (17.24) | 0.013 |
| Musculoskeletal pain, trauma | 37 (8.53) | 7 (4.79) | 44 (7.59) | 0.141 |
| Abnormal vitals/labs | 19 (4.38) | 9 (6.16) | 28 (4.83) | 0.317 |
| LVAD alarm | 0 | 8 (5.48) | 8 (1.38) | <0.001 |
| Fever | 12 (2.76) | 8 (5.48) | 20 (3.45) | 0.101 |
| Bleeding | 6 (1.38) | 17 (11.64) | 23 (3.97) | <0.001 |
| Dyspnea, cough, or wheezing | 109 (25.12) | 18 (12.33) | 127 (21.9) | 0.001 |
| Chest pain / discomfort | 67 (15.44) | 17 (11.64) | 84 (14.48) | 0.260 |
| Abdominal pain, vomit | 54 (12.44) | 16 (10.96) | 70 (12.07) | 0.634 |
| Stroke | 10 (2.3) | 3 (2.05) | 13 (2.234) | 0.86 |
| Others | 51 (11.75) | 7 (4.79) | 58 (10.0) | 0.009 |
ED = emergency department, LVAD = left ventricular assist device.
p-values for categorical variables are calculated using Chi-square or Fisher’s exact test.
The results of the primary outcome analysis examining the timeliness of ED evaluation are shown in Table 2. Time from arrival at the ED to triage did not significantly differ between groups. There was a trend toward more expedient rooming and physician assessment in the LVAD group (p = NS). However, after being assessed by an ED physician, the LVAD group had a significantly shorter time to disposition (admission or discharge, 109.8 min vs 177.0 min, p < 0.001). Overall, LVAD patients had significantly shorter ED lengths of stay than propensity matched HF patients (6.33 hrs vs 9.82 hrs, p = 0.0001). For those patients admitted to the hospital, there was no difference in hospital LOS, and while there was a trend toward higher cost in the LVAD group, this difference was not statistically significant (Table 2).
Table 2.
Emergency Department (ED) and hospitalization metrics.
| Characteristics | Heart failure, n (%) | LVAD, n (%) | Total, n (%) | p-value |
|---|---|---|---|---|
| Total Time to Triage (minutes) | 21.20 (210.13) | 29.30 (238.79) | 23.26 (217.59) | 0.6994 |
| Total Time to Room (minutes) | 73.4 (238.22) | 42.99 (242.68) | 65.69 (239.51) | 0.1853 |
| Total Time to physician (minutes) | 97.27 (239.90) | 51.77 (243.36) | 85.95 (241.36) | 0.0506 |
| Total Time from physician to disposition (minutes) | 177.0 (142.77) | 109.82 (109.65) | 160.41 (138.33) | <0.001 |
| ED Decisions | 0.08 | |||
| Admit | 344 (79.81) | 126 (87.50) | 470 (81.70) | 0.061 |
| Discharge | 76 (17.63) | 18 (12.5) | 94 (16.35) | 0.142 |
| Left against medical advice | 10 (2.32) | 0 | 10 (1.74) | 0.064 |
| Other | 1 (0.23) | 0 | 1 (0.17) | 0.99 |
| ED length of stay (h), mean (SD) | 9.82 (10.24) | 6.33 (6.16) | 8.94 (9.50) | 0.0001 |
| Hospital length of stay, mean (SD) | 6.58 (10.94) | 6.67 (8.04) | 6.61 (10.28) | 0.928 |
| Hospitalization charges in USD (median) | 21524.25 | 28766.95 | 23304.1 | 0.087 |
LVAD = left ventricular assist device.
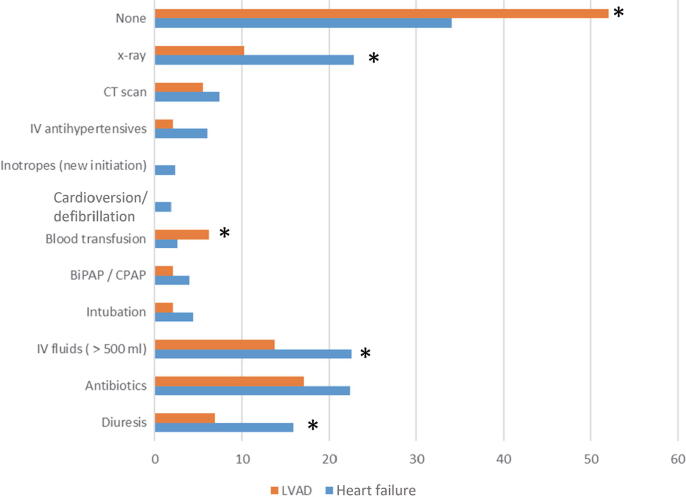
The nature of ED evaluations and specific resource utilization is shown in Fig. 1. While LVAD patients were more likely to be given a blood transfusion in the ED, overall, the LVAD group was more likely to have no interventions or testing ordered in the ED (p < 0.001).
Fig. 1.
Emergency department resource utilization. *indicates p < 0.05. BiPAP = bilevel positive airway pressure, CPAP = continuous positive airway pressure, CT = computed tomography, IV = intravenous, LVAD = left ventricular assist device.
4. Discussion
In this study, LVAD patients presented to the ED for a variety of reasons, largely unrelated to the LVAD device itself. In our cohort, only 5.48% of LVAD patients presented to the ED with a device complication or LVAD alarm. Broadening this definition to include bleeding and stroke, known complications of continuous-flow LVADs, still accounts for fewer than 1 in 5 LVAD ED presentations. This pattern is similar to that described previously in the literature, and is likely a manifestation of 24-hour care provided by the LVAD team and coordinators at our center and many others, which can facilitate expedited direct admission to LVAD trained units for suspected device-related complications and malfunctions [3], [4], [5]. The overall admission rate from the ED in our study is similar to those of prior evaluations, suggesting that the overwhelming majority of LVAD presentations to the ED result in admission [5], [6].
Of more interest, LVAD patients who presented to the ED had significantly shorter times from physician assessment to disposition, and an overall shorter ED LOS. When reviewed with the finding that those patients who were ultimately admitted had no significant difference in their hospital LOS or charges, the shorter times in the ED suggest that LVAD patients may be prioritized over non-LVAD patients, despite having similar degrees of illness. While shorter times to admission could be explained by the early involvement of the LVAD team upon patient presentation to the ED, the observation that rates of admission to the hospital did not differ between LVAD and non LVAD patients argues against this. The shorter time from ED physician assessment to disposition noted in LVAD patients, taking into account that almost 90% of them were admitted, may simply highlight a lower threshold to admit LVAD patients irrespective of their presenting complaint or ED workup. This threshold may be related to a higher perceived complexity of patients with LVADs by virtue of the device itself which may dissuade emergency care providers from discharging patients even when a clear indication for admission has not been established. This concept is supported by the observation that fewer interventions and tests were ordered for LVAD patients as compared to matched HF patients, regardless of presentation.
LVAD patients utilized air transport at a significantly higher rate than non-LVAD patients. ED-to-ED air transport is a costly healthcare resource generally utilized to minimize delay in critical situations that need immediate life-saving measures that cannot be provided at the sending facility. The higher rate of air transport utilization in the LVAD group was noted despite propensity score matching, with no difference in LOS or hospital charges to suggest a higher level of acuity in the LVAD group compared with the non-LVAD group. We speculate that an overall sense of unfamiliarity with LVADs in community EDs may lead to inappropriate utilization of resources, including inappropriate use of air transport. While this overutilization of resources may be understandable it suggests a need for LVAD patients to have a more direct and cost-effective pathway to the appropriate healthcare setting (i.e., direct admission to LVAD trained units, or units trained with LVAD credentialed providers). Guidelines for the emergent treatment and prehospital care of LVAD patients that are hemodynamically unstable are available for reference, along with more-detailed reviews of emergency LVAD care targeted to ED physicians [7], [8], [9]. Given the growing number of patients with LVADs, these resources are likely invaluable for emergency providers who do not care for LVAD patients on a daily basis. The recently published joint consensus statement from the Heart Failure Society of America, Society of Academic Emergency Medicine, and International Society of Heart and Lung Transplantation also provides an excellent overview for the management of a myriad of LVAD related complications, in both the pre-hospital and ED settings [10]. Of note, these publications do not provide specific guidance as to the triage and optimal management of LVAD patients presenting with non-LVAD related chief complaints, which appear to represent the majority of emergency department visits. Our analysis did not adjudicate the appropriateness or admission or treatment for presenting LVAD patients, but they do suggest a bias toward admission regardless of acuity. Further exploration of the reasons for this bias maybe warranted to avoid misutilization of resources.
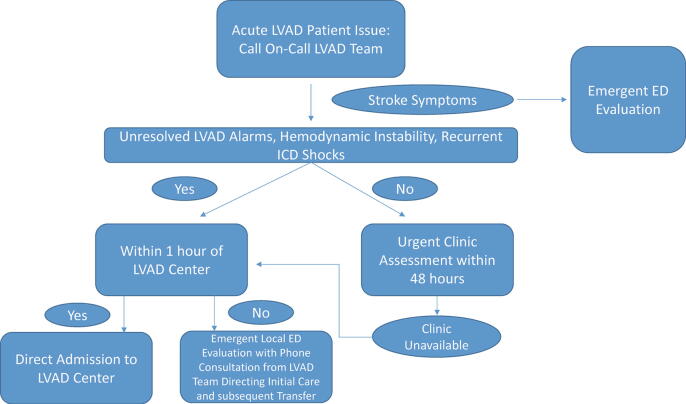
In addition to continued efforts to improve LVAD awareness and competency across healthcare providers, we suggest a care algorithm that emphasizes use of LVAD clinic assessments for less-urgent issues to avoid unnecessary and possibly inefficient, healthcare utilization in the ED (Fig. 2). Such an algorithm would favor routing potential LVAD device related complications for direct admission to an LVAD implant center, reserving ED care for only select cases where high acuity and complex multidisciplinary care is required, with management and potential transfer from remote EDs addressed in a collaborative fashion under the direction of the LVAD team. Adherence to such an algorithm, however, will depend on the willingness and knowledge of LVAD patients to call the available hotline for triage prior to presentation. Therefore, future investigations should examine how many of the LVAD patients presenting to the ED were able to contact the LVAD team beforehand. It may also be useful to examine the relationships between LVAD patient characteristics (e.g. socioeconomic status, caregiver presence, and distance from LVAD center) and ED utilization rates, to determine ways in which education or remote management may be structured to best meet patient’s individual needs. Additionally, increased utilization of digital health and telemedicine tools, such as HIPAA compliant smartphone applications which allow real time two-way communication, may assist in patient triage and the development of these robust algorithms. These platforms could also allow for better remote consultation and collaborations with outlying EDs. As such tools evolve in their capacities and capabilities, they may play an important role in reducing avoidable ED visits and aid in cost control.
Fig. 2.
Proposed LVAD care algorithm. ED = emergency department, ICD = implantable cardioverter-defibrillator, LVAD = left ventricular assist device.
The focus on out-patient care optimization, ED utilization, and by extension hospital admissions is paramount if LVAD therapy is to become more cost effective. While estimates of the true incremental cost-effectiveness ration (ICER) and quality-adjusted life-years (QALY) vary due to the heterogeneous nature of LVAD patients, readmission rates and out-patient expenses are a key driver of cost. One recent analysis demonstrates that were outpatient costs to be decreased by 50% and readmission rates reduced by 1 per-patient year, the impact was dramatic resulting in greater than 50% improvement in ICER per QALY gained [11]. This provides additional incentive for LVAD care teams to avoid hospital admissions, while also developing more robust and efficient out-patient protocols and algorithms. While the aforementioned analysis does establish a benchmark for monthly outpatient costs for LVAD care at less than $3000, slightly less than pre-LVAD costs, a detailed cost analysis which takes into account reimbursement and the staffing models needed to maintain 24-hour LVAD care has yet to be completed. Furthermore, the variability of outpatient algorithms likely affect ED utilization, hospitalizations, and costs and similarly have not been studied. In addition to the suggested algorithms, such investigations are needed to optimally guide patient care while improving cost effectiveness of LVAD therapy.
4.1. Limitations
This is a single-center retrospective study, and we were only able to capture ED utilization of LVAD patients that visited our ED. Additionally, while our LVAD team often direct admits patients or arranges urgent clinic visits for less ill patients, it is unknown to what extent individuals in our cohort were directed to come to the ED due to logistical challenges with either admissions or clinic visits. Furthermore, we are unable to precisely determine the time-point when the LVAD team was notified of ED presentation and variance therein may have affected our results.
4.2. Conclusion
LVAD patients most commonly present to the ED with complaints not directly related to their device. The presence of an LVAD results in a significant reduction in time from physician assessment to disposition and an overall shorter ED LOS. Despite this, there is no difference in hospital LOS and charges for LVAD patients presenting to the ED compared with those with HF and no LVAD. This may represent a created healthcare disparity. Developing more robust care pathways wherein the true role of ED care for LVAD patients is precisely defined may be helpful to improve ED and healthcare resource utilization.
Financial support
We acknowledge the University of Florida Integrated Data Repository (IDR) and the UF Health Office of the Chief Data Officer for providing the analytic data set for this project. Additionally, the Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under University of Florida Clinical and Translational Science Awards UL1 TR000064 and UL1TR001427.
The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CRediT authorship contribution statement
Mohammad Al-Ani: Conceptualization, Data curation, Writing - original draft, Writing - review & editing. Sarah S. Gul: Writing - review & editing. Abhishek Khatri: Writing - review & editing. Muhammad Abdul Baker Chowdhury: Writing - review & editing. Matthew Drabin: Writing - review & editing. Travis Murphy: Writing - review & editing. Brandon Allen: Methodology, Funding acquisition, Writing - review & editing. Juan M. Aranda: Writing - review & editing. Juan Vilaro: Writing - review & editing. Eric I. Jeng: Writing - review & editing. George J. Arnaoutakis: Writing - review & editing. Alex M. Parker: Writing - review & editing. Lauren E. Meece: Writing - review & editing. Mustafa M. Ahmed: Funding acquisition, Conceptualization, Investigation, Methodology, Project administration, Writing - review & editing.
Declaration of Competing Interest
The authors report no relationships that could be construed as a conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2020.100617.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Goldstein D.J., Meyns B., Xie R. Third annual report from the ISHLT Mechanically Assisted Circulatory Support Registry: a comparison of centrifugal and axial continuous-flow left ventricular assist devices. J. Heart Lung Transplant. 2019;38:352–363. doi: 10.1016/j.healun.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Kirklin J.K., Xie R., Cowger J. Second annual report from the ISHLT Mechanically Assisted Circulatory Support Registry. J. Heart Lung Transplant. 2018;37:685–691. doi: 10.1016/j.healun.2018.01.1294. [DOI] [PubMed] [Google Scholar]
- 3.Dunlay S.M., Haas L.R., Herrin J. Use of post-acute care services and readmissions after left ventricular assist device implantation in privately insured patients. J. Card. Fail. 2015;21:816–823. doi: 10.1016/j.cardfail.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McKillip R.P., Gopalsami A., Montoya M. Analysis of patients with ventricular assist devices presenting to an urban emergency department. West. J. Emerg. Med. 2018;19:907–911. doi: 10.5811/westjem.2018.8.38851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tainter C.R., Braun O.O., Teran F. Emergency department visits among patients with left ventricular assist devices. Intern. Emerg. Med. 2018;13:907–913. doi: 10.1007/s11739-017-1776-8. [DOI] [PubMed] [Google Scholar]
- 6.Goebel M., Tainter C., Kahn C. An urban 9-1-1 system's experience with left ventricular assist device patients. Prehosp. Emerg. Care. 2019;23:560–565. doi: 10.1080/10903127.2018.1532475. [DOI] [PubMed] [Google Scholar]
- 7.Bowles C.T., Hards R., Wrightson N. Algorithms to guide ambulance clinicians in the management of emergencies in patients with implanted rotary left ventricular assist devices. Emerg. Med. J. 2017;34:842–850. doi: 10.1136/emermed-2016-206172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brady W., Weigand S., Bergin J. Ventricular assist device in the emergency department: evaluation and management considerations. Am. J. Emerg. Med. 2018;36:1295–1299. doi: 10.1016/j.ajem.2018.04.047. [DOI] [PubMed] [Google Scholar]
- 9.Long B., Robertson J., Koyfman A., Brady W. Left ventricular assist devices and their complications: a review for emergency clinicians. Am. J. Emerg. Med. 2019;37:1562–1570. doi: 10.1016/j.ajem.2019.04.050. [DOI] [PubMed] [Google Scholar]
- 10.Givertz M.M., DeFilippis E.M., Colvin M. HFSA/SAEM/ISHLT clinical expert consensus document on the emergency management of patients with ventricular assist devices. J. Heart Lung Transplant. 2019;38:677–698. doi: 10.1016/j.healun.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Shreibati J.B., Goldhaber-Fiebert J.D., Banerjee D. Cost-effectiveness of left ventricular assist devices in ambulatory patients with advanced heart failure. JACC Heart Failure. 2017;5:110–119. doi: 10.1016/j.jchf.2016.09.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.