Summary
Ensuring burn patients get appropriate care without pursuing futile treatment has always constituted a challenging balance for burn surgeons. Patients with no prospect of cure who eventually die should potentially experience more comfortable and peaceful end-of-life (EoL) care. Recognizing that death for some patients is inevitable and can only be postponed but not avoided would open the way to a more humane comfort care for such patients. Though comfort EoL services are still not universal in burns intensive care units (ICU) and disparities still exist in access, and use of palliative care appears underutilized, its integration in the burns ICU has increased over the past decade with undeniable benefits. Palliative care consultations should be considered in select burn patients for whom survival is highly unlikely.
Keywords: severe burns, end-of-life, palliative, comfort care, withdrawal of life support, futile care
Abstract
Assurer des soins adaptés sans obstination déraisonnable a toujours représenté un équilibre subtil pour les brûlologues. Les patients à qui il ne peut être proposé de traitement curatif mourront et nous devons leur assurer une fin de vie confortable et apaisée. Ainsi, reconnaître que certains patients mourront inéluctablement, un traitement agressif ne faisant que reculer l’échéance, doit nous amener à leur prescrire des soins de confort. La culture des SP semble insuffisamment développée et leur prescription aléatoire au sein des CTB, alors que leur développement dans les décennies passées a indubitablement représenté un progrès. Des consultations de SP au profit des patients au-delà de toute ressource thérapeutique devraient être développées.
Introduction
Complex modern burn care has not been without great consequences to health care systems worldwide. Care of severe burn patients who decades ago would have died, in addition to patients for whom resuscitation and aggressive management is futile, has a profound impact on resource utilization.1,2,3 Severely burned patients usually receive acute resuscitation including intubation on the scene prior to transfer to a specialized burn center. Upon arrival, mechanical ventilation is initiated and many interventions performed, including escharotomy, fasciotomy, central venous catheterizations and tracheostomy, mostly to no avail. In the event that patients do survive this initial acute phase, they typically succumb within 48-96 hrs, or later following septic and multi-organ failure after a more or less prolonged hospitalization.3,4 Heroic life-saving interventions are not without negative effects. Integrity of the patient’s body is often violated as a result of aggressive interventions with no real benefit, in addition to wasted resources related to use of materials, bed occupancy, and distribution of workforce.4 Prediction of poor outcome and recognizing the point of futility remains, however, a challenge, but should remain a priority as quality end-of-life (EoL) care is arguably as important as life-sustaining care, if not more so.5
Some non-survivors may be obvious from the outset. In others, however, a decision of futility needs to be made during the course of treatment.5 Whenever extent of injury makes survival highly unlikely, or when the patient’s condition deteriorates during resuscitation, or when it becomes apparent that despite best efforts the patient will fail to respond to treatment, early withdrawal of life support (WLS) care has been advocated.5,6,7,8 The burn team has a most difficult task of anticipating whether active and aggressive treatment is likely to result in acceptable outcomes for their patients;9 nevertheless ensuring burn patients get appropriate care without pursuing futile treatment is a challenging balance to attain.7 Though care in burn intensive care units (ICUs) focuses mainly on the aggressiveness of burn treatment, the role of palliative end-of-life (EoL) care should not be overlooked; unfortunately this role remains unclear. Patients with no prospect of cure who eventually die should potentially experience more comfortable and peaceful EoL.6,10,11 Goals of burn care are nowadays gradually shifting from saving lives to making sure that those who survive their injuries are able to return to a good quality of productive life.1,10,12 It must be mentioned though that quality of life after burns is greatly determined by the resources a society is willing to set aside for rehabilitation of burn survivors.13
With highly unlikely survival following a severe burn injury, challenging and complex discussions regarding comfort care, EoL and/or WLS become a must. The decision is based on a combination of objective and subjective criteria, including extent and depth of burn injury, pre-existing medical comorbidities, clinician knowledge and previous experiences, potential future quality of life, and likelihood to return to independent living.1 This is difficult for patients, their families and providers, nevertheless early transition to comfort care may be both appropriate and humane.1,6
Though determinants of burn mortality have been well documented and despite the fact that a number of predictive models to determine survival have been described, EoL care in burn patients is still not well appreciated. Unfortunately, clear objective predictors for EoL decisions to reduce reliance on clinical intuition and help in decision-making are still not universally approved.1 Mortality prediction remains no more than a probable risk of death estimate.9
The goal of this paper is to review available recent literature about this critical issue, and try to determine the major obstacles that are still preventing the elaboration and wide acceptance of objective guidelines for EoL comfort care and WLS for severely burned patients.
Materials and methods
A PubMed search of title and abstract keywords “comfort care and burns”, “palliative care and burns”, and “end-of-life care and burns” was conducted for related publications in the English literature, limiting the search to the last 10 years until the present.
Results
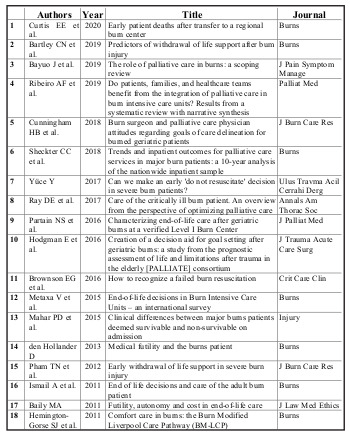
Despite numerous publications related to EoL palliative care, only 18 publications directly related to burn injuries could be retrieved within the time frame of the search (Table I). Interesting to note that not a single non-English publication about this topic could be identified. Medline search was not useful in identifying further publications.
Table I. List of retrieved publications.
Discussion
The concept of palliative care has evolved over the years as an active and global approach aiming to improve quality of life of patients and their families with problems related to life-threatening conditions. 11 The concept of comfort care in burns is not new. Back in 1987 Wachtel et al.14 proposed comfort care as “an alternative treatment program for seriously burned patients”, emphasizing that a decision to engage in comfort care does not mean no care. It should be viewed as a change in goals; rather than prolonging life, it is directed to enhance the quality of remaining life of patients dying in hospital settings by managing the multidimensional nature of suffering and providing a holistic approach to care for patients and their families.5,11
Much of the research into EoL care has been carried out on patients dying from end stage metastatic or chronic disease; this has led to an improved understanding of factors important in terminal care and what constitutes a “good death”.5 The core elements of palliative care are symptom control, communication, psychosocial, emotional and spiritual support to both patients and their families, without neglecting the staff caring for these patients as well.7,11
Though palliative care quality measures are proposed abundantly in the general critical care literature focused primarily on chronic terminal illnesses, research in EoL care for burn patients with non-survivable injuries is still sparse.2,6 However, general principles developed can be of great benefit to patients with more pressing acute injuries such as severe burns with high likelihood of death.15
Efforts have been made to develop precise predictive models of burn mortality.16 Determinants of burn mortality associated with increased likelihood for comfort care and WLS have been well documented in the literature; they include age, burn size, and presence of inhalation injury as well as associated comorbidities.1 The revised-Baux (r-Baux) score, perhaps the most frequently utilized burn severity scoring system, is a valuable tool to estimate burn mortality based on age, % Total Body Surface Area (% TBSA) and presence of inhalation injury - Age + % TBSA (Total Body Surface Area) + 17 (if inhalation injury present).3 For patients with very high scores and high mortality, provision of comfort measures would be most likely.3 Burn patients with r-Baux scores above 130 have an 88% mortality rate and scores of 150 signify certain death. Survival rates with different r-Baux scores in relation to age have been reported from 1974 to 2009, nevertheless r-Baux scores greater than 130 in >65 year olds are uniformly fatal.3,17,18 Though this score is highly valuable in determining futility of care, prognostic uncertainty still exists and it should be assessed and interpreted with care.3,10 For example, a 50% partial thickness burn injury in an 85-year-old (without inhalation injury) may be survivable, whereas an equivalent size of full thickness burns with the same r-Baux score of 135 may be non-survivable.3 Moreover, the strength of this scoring system in determining EoL care is variable with different age groups. A Do-Not-Attempt-Resuscitation (DNAR) order or WLS treatment for a young patient or patients < 65 years old is most commonly due to %TBSA and burn depth, whereas patients’ co-morbidities are generally the principal trigger in the >65-year-old group.1,6,13 Contrary to comorbid conditions, inhalation injury by itself is not predictive of palliative care services.15 Female gender in general is significantly associated with an increased odd of WLS,1 probably because women are more likely to have less aggressive treatment preferences or have surrogates that are more likely to make end of life decisions.19 As general understanding of burn pathophysiology and resuscitation has evolved, newer scoring models have been developed, incorporating additional independent variables particularly to establish accurate predictive models and probabilistic predictors for the elderly burn population.16 Evaluation of the relationship between biochemical markers and mortality has been recently recommended to strengthen the existing burn prognostication models. 10 However, all models are more useful for research than for bedside decision-making.7 Although prognostication outcome may suggest that an injury is un-survivable, the point a burn patient gets to the EoL phase from a clinical perspective may be difficult to ascertain.10 Difficulties in accurately predicting survival are mostly attributed to the complex nature of burn physiology and high incidence of sepsis and multi-organ failure in severely burned patients.13 Determining patients that will benefit most from aggressive resuscitation and management and those for whom this type of management is futile remains a major challenge.1 Moreover, little information is available about those patients that die as an active decision to withdraw treatment, or secondary to comfort measures alone when active and aggressive management is deemed to likely be futile or contrary to the patient’s best interests.9 It must be noted also that available predictive scoring models to date have been developed in high standard wellresourced health care facilities; their determined cut off points certainly do not apply to less resourced facilities.
Currently, the likelihood of return to independent living is an important factor, and recovery to an acceptable quality of life is often more important than simple survival. It is being increasingly valued in goals of care (GoC) and palliative care decisions.6,7
Meaningful recovery, however, is defined differently by each individual and is difficult to measure.7
Moreover, the concept of an “acceptable outcome” is a subjective determination that can only truly be made in hindsight by the patient himself.9
Palliative end-of-life (EoL) burn care
Palliative EoL care and comfort care, though distinct, are used synonymously in burns literature.10 Physical, psychosocial, and spiritual comfort support of patients suffering a life threatening injury and their families is the current standard of care required to improve quality of life, reduce anxiety and depression, and reduce hospital costs.7,10 With the knowledge that an injury is non-survivable, futility decision in burns management ensures the initiation of EoL support by delivering only palliative comfort care and/or WLS, or facilitates change in GoC from active treatment to issuing of DNAR orders to avoid futile inappropriate resuscitation and maintain patients’ dignity.10,13 Understanding the predictors of EoL comfort care and WLS supported by objective clinical data are indispensable to burn surgeons, caregivers and family members alike to be able to make informed and ethical futility decisions.11 Involvement of palliative care specialists and application of their concepts in the burns ICU has been increasing over the last decades, thus improving symptom control and the dying process of severely burned patients as well as improving communication between care providers and patients’ families.11 The greatest benefit of palliative care services may be realized in those patients with modified Baux scores of between 120-150, given this group is unlikely to survive and could be aided by avoiding unnecessary intervention.7 Several care pathways have been described as practical guides to meet EoL needs and support the dying burn patient in achieving a “good death”; they encompass pain management, distressing symptoms management, and deal with existential issues, respect and dignity; in addition these pathways improve availability of relatives with patients.10 Comfort care pathways guided and supported by a team approach also decrease likelihood of surgical interventions; they facilitate discontinuation of treatment modalities deemed unnecessary, and enhance the decision-making process between health care providers, burn patients and families.10 Pham et al.6 have described three key components for stepwise WLS protocol; these are preparation, provision of adequate analgesia and sedation, followed by weaning and terminal discontinuation from the ventilator. The preparation phase begins with EoL decision making followed by discontinuing all treatment that does not provide comfort, including monitors, invasive devices, enteral nutrition, and active fluid resuscitation. The next step ensures adequate analgesia and sedation, preferably by continuous infusion of opioids and benzodiazepines. The terminal final phase consists of weaning and liberating the dying patient from the ventilator by either extubation or T-piece. The Liverpool care pathway (BM-LCP) has also been developed for EoL management.5
With clearly defined treatment goals, such structured guidelines make the burn team more at ease with the concept of impending death and more confident treating dying patients.5 However, these care pathways do not make clear how the notion of “good death” is to be measured; moreover, how family members experience the applied pathway remains also unclear. In addition, robust evidence of outcomes for burn patients and their families requiring EoL care is also lacking.10 Some institutions have implemented such standardized protocols but each institution looks at its own survival rates to determine what is the futility cut off or threshold they would want to subscribe to.1,3
End-of-life (EoL) discussions and goals of care (GoC) decision-making
The decision of comfort care involves many factors that vary between institutions, patients and their families, as well as providers.1,9,20,21 Ultimately any health care decision must respect in principle patient autonomy, one of the cornerstones of patient-doctor relationship, and must be in accordance with patient wishes.1,6 Moreover, communicating with patients and families has long been identified as an important physician competency.7
Unlike chronic diseases, a severe burn is a sudden unexpected life-changing event and burn victims and their families have little time to adjust;22 EoL discussions with immediacy of death on the order of days to weeks are different than for long-term palliation of terminally ill patients with a predicted death horizon on the order of months to years.15 Very often patients are not able to make autonomous decisions; major burn injuries incapacitate patients because of shock, mechanical ventilation or sedation rendering them unable to express their autonomy.6 They also create complex situations where expeditious important life-changing decisions need to be made under time pressure and high stress navigating between unexpected medical emergencies.11,23 Essential decisions thus need to be discussed with a family member, usually the spouse, in most instances the wife, or with a designated surrogate.1,6 Usually family members are also unable to make informed decisions, particularly in the early stages of the injury. In such situations the burn physician has to take the lead and decide in the patient’s best interest.21 Historically, family meetings for futility and EoL discussions have been led by burn surgeons given their expertise in thermal injury and their sense of responsibility to their patients. Such discussions are often inspired by injury severity alone and are guided by the surgeons’ inherent drive to save patients’ lives. Despite established guidelines, surgeons generally feel less comfortable holding GoC conversations and usually fail to make timely ethically-challenging decisions.23,24 Burn surgeons are no exception.
Surgeons often rely upon the patient’s family attitude and response before consulting a palliative care specialist. They believe that consulting a nonsurgically trained palliative care specialist should be reserved for patients with no remaining treatment options for fear that the patient or his family would misinterpret the consultation as abandonment of care or hope and a sign of giving up.23,24 On the contrary, increasing involvement and integration of palliative care physicians in the ICU in recent years has made a major and meaningful shift in defining GoC and has resulted in better communication, decisionmaking process, symptom control, patient comfort, and family care. It has resulted also in fewer feelings of hopelessness, and a better overall experience for the patient, their family, and possibly the treating team.11,24 The concept of a multidisciplinary team approach to the physical, emotional, and spiritual needs of patient, family, and also of staff, and coordinated conversations with the families, would ideally help mitigate fears and aid in a fuller understanding of palliative care by the patients and their family.7,23,24 The benefits of early goal setting with multidisciplinary family discussions and the palliative care specialist cannot be more evident than with geriatric burn victims that frequently undergo prolonged and debilitating ICU admissions, multiple invasive procedures, with resultant reductions in their independence and quality of life.17,24,25 Timing of end-of-life (EoL) care decision Clinicians are used to actively treating their patients, moving forward with their care and preserving life wherever possible; however, in doing so, opportunity for good palliation may be missed.13 Timing of discussions and decision-making are very important to facilitate the family’s understanding of the critical nature of the situation and to allow earlier cessation of aggressive measures when indicated.23,25 It is recommended that EoL care discussions/decisions with the family should be initiated early in the course of treatment.10 This helps to set expectations early for all stakeholders in the event a patient’s condition deteriorates.23 The approach of trying to “see how the patient will do” can delay comfort care initiation and may have significant ramifications such as emotional distress and poor outcomes for the burn patient, family and burn care staff.10 For patients with high risk of mortality or disability for whom withholding treatment has not been made initially on admission, a structured family meeting is recommended within 72 hrs.23
EoL care for burn patients can be initiated as soon as active resuscitation and life support treatment are withheld within 24-72 hrs of admission (early deaths) or withdrawn at a later stage of the management after a clear period of active treatment (late deaths).1,6,9,10 Either way, death occurs soon after.13 Early transition to comfort care, symptom palliation, and WLS is a process specific to burns triggered by the severity of the injury and %TBSA.1,6 Reaching a futility decision for patients who experience late deaths is particularly challenging; it usually involves maintaining a balance between diagnosis, therapeutics and ethics.10 The clinical course of adult burn patients who die after prolonged intensive treatment is distressing for all involved and is associated as expected with higher daily costs, extended length of stay and increased total cost of care. This fact highlights the need for experienced clinicians to be realistic about the burden of care while considering the best interests of the patient at all stages of treatment. 1,9 Considering that geriatric survivors of thermal injury frequently undergo prolonged and debilitating ICU admissions, and multiple invasive procedures with reduction in their independence and quality of life, this particular group benefits from early goal-setting conversations that align their treatment plan with their values, goals and preferences.24 For children, however, the approach may be drastically different; decision of EoL care is generally made late, just hours before death.1,26,27 Ethical considerations of futility of care decision Defining futility, a recent newcomer in medical ethics, is a difficult endeavour; defining futility for the severely burned patient is probably one of the most difficult decisions a burns team can make.6,21 It may be argued by some that futility decision relies on clinical judgment and epidemiological skills; others insist that futility should be based on sound knowledge of prognosis of the disease condition at hand.21 The principle of futility that curbs patient autonomy cannot work without listening to and negotiating with the patient and his or her family.21 However the futility debate cannot be confined to the narrow context of the individual patient-doctor relation. It is “part of the larger power struggle over the values that should prevail in determining what options will be available”.13,27 With severely burned patients, expeditious life-sustaining decisions with serious ethical implications and uncertain mortality and morbidity must be made, such as emergent surgical procedures, blood transfusions, prolonged ventilation, feeding tubes, and the use of cardiopulmonary resuscitation.23 Ultimately the responsibility to make such decisions lies with the treating clinician.9 Deciding whether a treatment is considered futile or not, and whether passive withholding or active withdrawing of life-sustaining therapy should be contemplated or not, or a DNAR order in such patients must be made, can be extremely challenging. 13,21 Once a treatment is considered futile, regardless of patient autonomy, patient and family wishes become irrelevant.21
Circumstances in which treatment may be considered futile in a burns unit vary.6,13 EoL decisions are not purely subjective; certainly they are based on objective criteria of burn severity and probabilities of survival, but in many instances they are dictated by assumptions physicians are not especially qualified to make, such as poor outcome and quality of life that are still controversial.22 Prognosis is often assessed on the basis of percentage burned area; it is no secret that accuracy of determination of %TBSA is notoriously poor. Moreover, prognostic burn scores often validated for specialized high standard burn centers certainly do not apply to the population a given practitioner may be serving.13 Advances in burn care occur rapidly; the fact that a score considered non-salvageable only 10 years ago may deny potentially salvageable patients a chance now, must not be overlooked either.13 There is also a serious issue regarding the wide variety amongst burn care providers about what is considered an acceptable quality of life.13 Reasons for denying lifesustaining treatment may also be influenced by individual experiences, personal beliefs and religious convictions.22 Cultural differences and legal imperatives such as the absolute obligation to provide active treatment whether it is considered futile or not should not be taken lightly.9,13 The legal aspects of providing end of life care are complex and multifaceted.5 At present in some countries like Turkey, it is not possible to give DNR orders for patients with severe burns that are incompatible with survival due to legal interdiction.4 Moreover, opinions and feelings of the patient and their next of kin may influence the decision making process, particularly where futility of treatment is uncertain.13 Given the different clinicians involved with different levels of experience and knowledge, it is also difficult to clearly discern which factors have been truly taken into account and the exact means by which such futility of care decisions may have been made.9
Though no value can be put on human life, socio-economical implications are not negligible. In principle every salvageable life is to be saved but there is a limit to the amount of effort and resources that a society is able and willing to make, particularly in settings with low resources. Issues related to the value placed upon human life in society at large, in addition to the total amount of the Gross National Product a society is willing and/or able to spend on health care and national and international policies that influence healthcare priorities, pose serious ethical challenges.13
Conclusion
Palliative care guidelines and protocols in other specialties such as geriatric care and oncology are well developed; long-term palliation pathways are not however transferable to the unique needs of the burn patient and can be difficult to implement logistically. 13 Recognizing that death for some patients is inevitable and can only be postponed but not avoided would open the way to a more humane EoL care for such patients.21 End of life care of severely burned patients is as important as it is in other settings. 5 Palliative care in the burn ICU for patients with no prospect of curative treatment favours comfort rather than aggressive management.18 Upon conversion from curative to palliative care, new goals for the patient’s therapy emerge in order to achieve comfortable and dignified death.13 Though comfort EoL services are still not universal and disparities still exist in access, in addition to the fact that these services seem to be underutilized in the care of severely burned patients, their integration in the burns ICU has increased over the past decade with undeniable benefits. Palliative care consultations should be considered in select burn patients for whom survival is highly unlikely.15
References
- 1.Bartley CN, Atwell K, Cairns B, Charles A. Predictors of withdrawal of life support after bum injury. Burns. 2019;45:322–327. doi: 10.1016/j.burns.2018.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanchez JL, Pereperez SB, Bastida JL, Martinez MM. Cost-utility analysis applied to the treatment of burn patients in a specialized center. Arch Surg. 2007;142:50–57. doi: 10.1001/archsurg.142.1.50. [DOI] [PubMed] [Google Scholar]
- 3.Curtis EE, Yenikomshian HA, Carrougher GJ, Gibran NS, Mandell SP. Early patient deaths after transfer to a regional burn center. Burns. 2020;46:97–103. doi: 10.1016/j.burns.2019.02.022. [DOI] [PubMed] [Google Scholar]
- 4.Yüce Y, Acar HA, Erkal KH, Tuncay E. Can we make an early ‘do not resuscitate’ decision in severe burn patients? Ulus Travma Acil Cerrahi Derg. 2017;23:139–143. doi: 10.5505/tjtes.2016.71508. [DOI] [PubMed] [Google Scholar]
- 5.Hemington-Gorse SJ, Clover AJ, Macdonald C, Harriott J. Comfort care in burns: the Burn Modified Liverpool Care Pathway (BM-LCP). Burns. 2011;37:981–985. doi: 10.1016/j.burns.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 6.Pham TN, Otto A, Youg S, Kramer CB. Early withdrawal of life support in severe burn injury. J Burn Care Res. 2012;33:130–135. doi: 10.1097/BCR.0b013e31823e598d. [DOI] [PubMed] [Google Scholar]
- 7.Ray DE, Karlekar MB, Crouse DL, Campbell M. Care of the critically ill burn patient. An overview from the perspective of optimizing palliative care. Annals Am Thorac Soc. 2017;14:1094–1102. doi: 10.1513/AnnalsATS.201607-577PS. [DOI] [PubMed] [Google Scholar]
- 8.Brownson EG, Pham TN, Chung KK. How to recognize a failed burn resuscitation. Crit Care Clin. 2016;32:567–575. doi: 10.1016/j.ccc.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Mahar PD, Wasiak J, Cleland H, Paul E. Clinical differences between major burns patients deemed survivable and nonsurvivableon admission. Injury. 2015;46:870–873. doi: 10.1016/j.injury.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Bayuo J, Bristowe K, Harding R, Agyei FB. The role of palliative care in burns: a scoping review. J Pain Symptom Manage. 2019;Nov 13. pii:S0885-3924(19)30653-0. doi: 10.1016/j.jpainsymman.2019.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Ribeiro AF, Martins Pereira S, Gomes B, Nunes R. Do patients, families, and healthcare teams benefit from the integration of palliative care in burn intensive care units? Results from a systematic review with narrative synthesis. Palliat Med. 2019;33:1241–1254. doi: 10.1177/0269216319862160. [DOI] [PubMed] [Google Scholar]
- 12.Prendergast TJ, Claessens MT, Luce JM. A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med. 198;158:1163–1167. doi: 10.1164/ajrccm.158.4.9801108. [DOI] [PubMed] [Google Scholar]
- 13.Ismail A, Long J, Moiemen N, Wilson Y. End of life decisions and care of the adult burn patient. Burns. 2011;37:288–293. doi: 10.1016/j.burns.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 14.Wachtel TL, Frank HA, Nielsen JA. Comfort care: an alternative treatment programme for seriously burned patients. Burns. 1987;13:1–6. doi: 10.1016/0305-4179(87)90247-6. [DOI] [PubMed] [Google Scholar]
- 15.Sheckter CC, Hung KS, Rochlin D, Maan Z. Trends and inpatient outcomes for palliative care services in major burn patients: a 10-year analysis of the nationwide inpatient sample. Burns. 2018;44:1903–1909. doi: 10.1016/j.burns.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Davis JS, Prescott AT, Varas RP, Quintana OD. A new algorithm to allow early prediction of mortality in elderly burn patients. Burns. 2012;38:1114–1118. doi: 10.1016/j.burns.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 17.Hodgman E, Joseph B, Mohler J, Wolfe SE. Creation of a decision aid for goal setting after geriatric burns: a study from the prognostic assessment of life and limitations after trauma in the elderly [PALLIATE] consortium. J Trauma Acute Care Surg. 2016;81:168–172. doi: 10.1097/TA.0000000000000998. [DOI] [PubMed] [Google Scholar]
- 18.Fratianne RB, Brandt CP. Determining when care for burns is futile. J Burn Care Rehabil. 1997;18:262–267. doi: 10.1097/00004630-199705000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Quill CM, Ratcliffe SJ, Harhay MO, Halpem SD. Variation in decisions to forgo life-sustaining therapies in US ICUs. Chest. 2014;146:573–582. doi: 10.1378/chest.13-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–366. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 21.den Hollander D. Medical futility and the burns patient. Burns. 2013;39:851–855. doi: 10.1016/j.burns.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 22.Metaxa V, Lavrentieva A. End-of-life decisions in Burn Intensive Care Units - An International Survey. Burns. 2015;41:53–57. doi: 10.1016/j.burns.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 23.Bhangu JK, Young BT, Posillico S, Ladhani HA. Goalsof care discussions for the imminently dying trauma patient. J Surg Res. 2020;246:269–273. doi: 10.1016/j.jss.2019.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cunningham HB, Scielzo SA, Nakonezny PA, Bruns BR. Burn surgeon and palliative care physician attitudes regarding goals of care delineation for burned geriatric patients. J Burn Care Res. 2018;39:1000–1005. doi: 10.1093/jbcr/iry027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Partain NS, Subramanian M, Hodgman EI, Isbell CL. Characterizing end of life care after geriatric burns at a verified level I burn center. J Palliat Med. 2016;19:1275–1280. doi: 10.1089/jpm.2016.0152. [DOI] [PubMed] [Google Scholar]
- 26.O’Mara MS, Chapayk D, Greenhalgh DG, Palmieri TL. End of life in the pediatric burn patient. J Burn Care Res. 2006;27:803–808. doi: 10.1097/01.BCR.0000245436.06218.95. [DOI] [PubMed] [Google Scholar]
- 27.Baily MA. Futility, autonomy and cost in end-of-life care. J Law Med Ethics. 2011;39:172–182. doi: 10.1111/j.1748-720X.2011.00586.x. [DOI] [PubMed] [Google Scholar]


