Abstract
In December 2019, the first data emerged from Wuhan, China, of a serious acute respiratory disease caused by a new coronavirus, SARS-CoV-2 (COVID-19). In a short time, the health emergency became a global pandemic. To date, there are about 18.8 million infected people and about 700,000 deaths. There are currently no effective vaccines, and treatments are mostly experimental. The symptoms associated with COVID-19 are different, ranging from mild upper respiratory tract symptoms to severe acute respiratory distress syndrome (SARS). Data from previous coronavirus outbreaks such as SARS-CoV (2003 outbreak) and emerging epidemiological data from the current global COVID-19 pandemic suggest that there could be substantial tissue fibrotic consequences following SARS-CoV-2 infection, responsible for severe and in some cases fatal lung lesions. Some data show that even patients cured of viral infection have lung fibrotic tissue residues responsible for incorrect respiratory function even after healing. The role of antifibrotic drug therapy in patients with ongoing SARS-CoV-2 infection or in patients cured of residual pulmonary fibrosis is still to be defined and unclear; the scientific rationale for initiating, continuing, or discontinuing therapy is poorly defined. In this article, we describe the advantages of antifibrotic therapy in patients with ongoing SARS-CoV-2 viral infection to prevent the worsening and aggravation of the clinical situation, and the advantages it could have in the role of preventing pulmonary fibrosis after SARS-CoV-2 infection, and in accelerating the complete healing process.
Keywords: Fibrotic, Pulmonary, Covid-19, Infection, Pirfenidone
SARS-CoV-2 Clinical Aspects
The new coronavirus SARS-CoV-2 (COVID-19) is responsible for the current global pandemic, representing a health challenge with few precedents in human history.
At the time of writing this manuscript, COVID-19 infected 6.42 million people and caused about 700,000 deaths [1]. SARS-CoV-2 infection can have a completely asymptomatic or mildly symptomatic course, but in some cases, it can also cause systemic hyperinflammation, pulmonary fibrosis and scarring with lung collapse, multi-organ dysfunction, and patient death [2]. To date, no effective or antiviral vaccines against SARS-CoV-2 are available, treatments are mostly experimental, so it is very important to know the advantages of current therapeutic solutions to decrease the aggressiveness of the viral infection, avoiding serious complications and consequent patient death. The most serious phases of viral infection are characterized by a sudden and excessive release of pro-inflammatory mediators, which leads to lung damage with extensive fibrosis and rapid onset of respiratory distress syndrome [3]. Studies have shown that bilateral interstitial pneumonia caused by COVID-19, so called because it attacks the tissue covering the lung alveoli, is associated with the presence of fibrotic tissue caused by excess collagen (fibrosis) in the lung crevice with associated hyperinflammation present. In this direction, the use of a pharmacological approach to reduce or prevent fibrotic status, with antifibrotic agents such as pirfenidone, used with demonstrated clinical efficacy in idiopathic pulmonary fibrosis [4] can be a valuable aid in the prevention of serious or fatal complications from COVID-19 in patients with ongoing infection, or in those already healed with residual fibrotic lung lesions [5].
SARS-CoV-2 and Lung Fibrosis
Pulmonary fibrosis is a pathological consequence of interstitial pulmonary diseases and is characterized by the persistence of fibroblasts and excessive deposition of collagen and extracellular matrix, as well as the destruction of normal pulmonary architecture [6]. The progression of pulmonary fibrosis leads to a loss of pulmonary function with damage to the correct exchange of oxygen capillary alveoli [7]. Causes of pulmonary inflammation include age, smoking, and viral infections [8]. Among the pathological mechanisms are altered oxidative stress and excessive production of reactive oxygen species (ROS); altered TGF-b, FGF, and PDGF contribute to the development of fibrosis [9]. A hyperactive inflammatory state such as that present in the most severe stages of COVID-19 infection, caused by the cytokine storm, is probably the main cause of pulmonary fibrosis responsible for severe and in some cases fatal lung lesions. Evidence shows that the most severe cases of COVID-19 have an extensive presence of pulmonary fibrotic tissue, and data show that serum levels of the above-mentioned cytokines and growth factors causing pulmonary fibrosis are strongly increased in patients with COVID-19 [10]. Mediators such as TGF-β, VEGF, Il-6, and TNF-α vascular dysfunctions can lead to the progression of fibrosis [11, 12].
The pathophysiological similarity between IPF and COVID-19 viral infection suggests a similar pathogenetic mechanism of pulmonary fibrosis in these two diseases; therefore, it is hypothesized that drugs useful for the treatment of IPF could also be useful for patients with COVID-19.
Pharmacological Approach with Antifibrotic Therapy
The reason for the use of antifibrotic therapy in COVID-19 patients is primarily based on the following objectives: to avoid serious complications and fatal lung injury in patients with ongoing infection, to accelerate the healing process in healed patients with residual reversible fibrotic lesions [13]. As described above, unregulated immune/inflammatory mechanisms as a result of a cytokine storm promote pulmonary fibrosis [14].
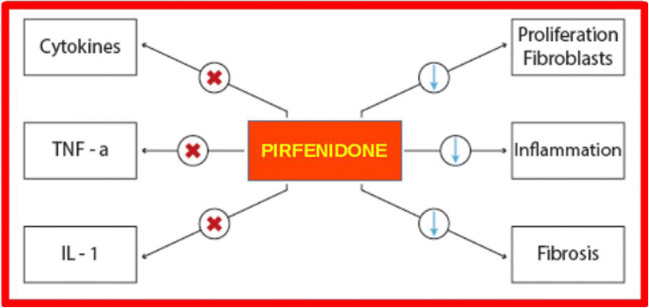
To date, there are antifibrotic drugs such as pirfenidone and nintedanib used with proven efficacy in the treatment of IPF. Specifically, pirfenidone is attributed to pleiotropic actions [15] (Fig. 1).
Fig. 1.
Antifibrotic therapy, pleiotropic effects of Pirfenidone
In fact, existing data indicate that pirfenidone has both antifibrotic and anti-inflammatory properties and is able to mitigate the proliferation of fibroblasts and the production of proteins and cytokines associated with fibrosis; it also mitigates the accumulation of extracellular matrix in response to cytokine growth factors such as TGF-β and PDGF [16, 17]. Data suggest that pirfenidone has more anti-inflammatory and antioxidant effects than its exceptional antifibrotic capacity. Indeed, the data show that with early use, its strong anti-SOD activity and inhibition of the effects mediated by IL-1 and IL-4, an important therapeutic scenario for the prevention of interstitial pulmonary fibrosis caused by COVID-19, can be opened. To date, the therapeutic efficacy of antifibrotic therapy in pulmonary fibrosis induced by SARS-CoV-2 is still being investigated in clinical trials. Nevertheless, evidence has already demonstrated the efficacy of antifibrotics in diseases with profibrotic pathways activated by immune/inflammatory dysregulation, which may have similarities with those caused by SARS-CoV-2 infection [18]. A key aspect to consider is the timing of the onset of antifibrotic action. In some severe cases of SARS-CoV-2, the evolution towards a severe pulmonary fibrotic lung state can be very rapid which can lead to antifibrotic therapy not acting in time; probably in these cases, a therapeutic regimen combined with immunomodulants (IL-1 or IL-6 inhibitors) and antifibrotics could lead to an important and more effective pharmacological synergism. Synergistic therapy could more quickly counteract the anti-inflammatory and antifibrotic pathways and mitigate their consequences.
Although many patients who develop SARS-CoV-2 respiratory distress syndrome survive the acute phase of the disease, data have shown that some of them die from progressive pulmonary fibrosis [19]. However, some studies indicate that pulmonary fibrosis is more prevalent in patients who have a longer duration of viral infection, suggesting that antifibrotic therapy should be administered early to be more effective clinically.
It should also be added that a percentage of patients cured of COVID-19 show radiological and physiological abnormalities consistent with fibrotic lung disease; even in this type of patients, a medium-long-term antifibrotic therapy may be necessary to accelerate the complete healing process [20].
Monotherapy or Combination Therapy
While pirfenidone in the acute phase of the disease can be used in combination with anti-inflammatory drugs to limit the damage produced by the cytokine storm and avoid the death of the patient, in the chronic phase, when the patient is saved and cured of the infection, pirfenidone can be used to eliminate residual complications, such as fibrotic tissue in the lungs. This can be done in monotherapy or together with other medications if there are multiple post-infection complications [21].
Several reports suggest, however, that there are differences between IPF and COVID-19-induced pulmonary fibrosis, diversity in the rapid evolution of the fibrotic and inflammatory state, and a highly developed procoagulant effect in SARS-CoV-2 viral infection [22, 23]. All these considerations suggest that other treatments should be implemented in synergy with antifibrotic therapy. The use of steroids or inhibitors IL-1/IL-6 is important to reduce inflammatory status. The use of spironolactone may be of significant importance in fibrosis prevention [24], the use of anticoagulants may reduce the risk of thrombosis, and the administration of antivirals is important to reduce the viral load. In addition, agents acting RAS could be efficacy by increasing of ACE-2 with a key role protective in the lungs.
Conclusions
The global COVID-19 pandemic seems to be continuing, and the lack of effective and antiviral vaccines directed against SARS-CoV-2 forces scientists to seek new treatment options from existing therapeutic solutions. In this article, we have described the pathophysiological similarities of SARS-CoV-2 virus infection with IPF.
One of the causes of severe lung injury is pulmonary fibrosis. While waiting for antivirals directed against SARS-CoV-2, a valid therapeutic solution to avoid the most serious complications in patients with ongoing infection or aimed at accelerating healing processes in patients after COVID-19 infection can be represented by antifibrotic therapy, in therapeutic regimens combined with other drugs. Ongoing clinical studies will provide us with the necessary evidence.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Topical Collection on COVID-19
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization HO (2020) Coronavirus disease 2019 (COVID-19) situation report Available from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2.Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Viro. 2020. [DOI] [PMC free article] [PubMed]
- 3.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single centered, retrospective, observational study. Lancet Respir Med. 2020;8:457–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung MP, Park MS, et al. Safety and efficacy of pirfenidone in advanced idiopathic pulmonary fibrosis: a nationwide postmarketing surveillance study in Korean patients. Adv Ther. 2020;15. [DOI] [PMC free article] [PubMed]
- 5.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for Covid-19 Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sime PJ, O’Reilly KM. Fibrosis of the lung and other tissues: new concepts in pathogenesis and treatment. Clin Immunol (Orlandofla) 2001;99:308–319. doi: 10.1006/clim.2001.5008. [DOI] [PubMed] [Google Scholar]
- 7.Razzaque MS, Taguchi T. Pulmonaryfibrosis: Cellularandmolecularevents. Pathol Int. 2003;53:133–145. doi: 10.1046/j.1440-1827.2003.01446.x. [DOI] [PubMed] [Google Scholar]
- 8.Naik PK, Moore BB. Viral infection and aging as cofactors for the development of pulmonary fibrosis. Expert Rev Respir Med. 2010;4:759–771. doi: 10.1586/ers.10.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gonzalez-Gonzalez FJ, Chandel NS, Jain M, Budinger GRS. Reactive oxygen species as signaling molecules in the development of lung fibrosis. Transl Res J Lab Clin Med. 2017;190:61–68. doi: 10.1016/j.trsl.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nile SH, Nile A, Qiu J, Li L, Jia X, Kai G. COVID-19: Pathogenesis, cytokine storm and therapeutic potential of interferons. Cytokine Growth Factor Rev. 2020;53:66–70. 10.1016/j.cytogfr.2020.05.002. [DOI] [PMC free article] [PubMed]
- 11.Pittet J-F, Griffiths MJD, Geiser T, Kaminski N, Dalton SL, Huang X, Brown LAS, Gotwals PJ, Koteliansky VE, Matthay MA, et al. TGF-β isacriticalmediatorofacutelunginjury. J Clin Investig. 2001;107:1537–1544. doi: 10.1172/JCI11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamada N, Kuwano K, Yamada M, Hagimoto N, Hiasa K, Egashira K, Nakashima N, Maeyama T, Yoshimi M, Nakanishi Y. Anti-vascular endothelial growth factor gene therapy attenuates lung injury and fibrosis in mice. J Immunol. 2005;175:1224. doi: 10.4049/jimmunol.175.2.1224. [DOI] [PubMed] [Google Scholar]
- 13.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Wang BJ, Yang JC, et al. [Advances in the research of mechanism of pulmonary fibrosis induced by corona virus disease 2019 and the corresponding therapeutic measures. [DOI] [PubMed]
- 15.Seifirad S. Pirfenidone: a novel hypothetical treatment for COVID-19. Med Hypotheses. 2020;144:110005. doi: 10.1016/j.mehy.2020.110005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferrara F, Granata G, Pelliccia C, La Porta R, Vitiello A. The added value of pirfenidone to fight inflammation and fibrotic state induced by SARS-CoV-2 : anti-inflammatory and anti-fibrotic therapy could solve the lung complications of the infection? [published online ahead of print, 2020 Jun 27]. Eur J Clin Pharmacol. 2020:1–4. 10.1007/s00228-020-02947-4. [DOI] [PMC free article] [PubMed]
- 17.Lancaster LH, de Andrade JA, Zibrak JD, Padilla ML, Albera C, Nathan SD, Wijsenbeek MS, Stauffer JL, Kirchgaessler KU, Costabel U. Pirfenidone safety and adverse event management in idiopathic pulmonary fibrosis. Eur Respir Rev. 2017;26(146):170057. doi: 10.1183/16000617.0057-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maher TM, Corte TJ, Fischer A, et al. Pirfenidone in patients with unclassifiable progressive fibrosing interstitial lung disease: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir Med. 2019;8:147–157. doi: 10.1016/S2213-2600(19)30341-8. [DOI] [PubMed] [Google Scholar]
- 19.Meduri GU, Headley S, Kohler G, Stentz F, Tolley E, Umberger R, Leeper K. Persistent elevation of inflammatory cytokines predicts a poor outcome in ARDS. Plasma IL-1β and IL-6 levels are consistent and efficient predictors of outcome over time. Chest. 1995;107:1062–1073. doi: 10.1378/chest.107.4.1062. [DOI] [PubMed] [Google Scholar]
- 20.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J’, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vitiello A, Ferrara F, Pelliccia C, Granata G, La Porta R. Cytokine storm and colchicine potential role in fighting SARS-CoV-2 pneumonia. Italian Journal of Medicine. 2020;14(2):88–94. doi: 10.4081/itjm.2020.1284. [DOI] [Google Scholar]
- 22.Ranucci M, Ballotta A, Di Dedda U, Bayshnikova E, Dei Poli M, Resta M, Falco M, Albano G, Menicanti L. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020;18:1747–1751. doi: 10.1111/jth.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barut F, Ozacmak VH, Turan I, Sayan-Ozacmak H, Aktunc E. Reduction of acute lung injury by administration of spironolactone after intestinal ischemia and reperfusion in rats. Clin Investig Med Med. 2016;39:E15–E24. doi: 10.25011/cim.v39i1.26326. [DOI] [PubMed] [Google Scholar]
- 24.Vitiello A, Ferrara F. Correlation between renin-angiotensin system and severe acute respiratory syndrome coronavirus 2 infection: what do we know? [published online ahead of print, 2020 Jul 14] Eur J Pharmacol. 2020;883:173373. doi: 10.1016/j.ejphar.2020.173373. [DOI] [PMC free article] [PubMed] [Google Scholar]