Dear Editor,
Until recently, the number of positive and death cases from coronavirus disease 2019 (COVID-19) is still increasing. This pandemic disease has caused a significant impact and burden on all aspects of life, especially on the economic and health aspect. Therefore, identification of risk factors that contribute to the development of the severe disease is very important to enable risk stratification, optimize hospital resources reallocation, and guide public health recommendations and interventions. A previous study has shown that anemia was common in patients with community-acquired pneumonia (CAP) and was associated with a higher 90-day mortality rate [1]. Unfortunately, no study provides clear evidence regarding the link between anemia and COVID-19. This article aims to explore the potential association between anemia and the severity of COVID-19 infection.
A search of the literature was conducted on Google scholar using the keywords "anemia" OR “hematologic” OR "clinical characteristics" OR "comorbidities" OR "risk factors" AND "coronavirus disease 2019" OR "COVID-19", until July 21st, 2020) with language restricted to English only. The title, abstract, and full text of all articles identified that matched the search criteria were assessed, and those reporting the rate of anemia in COVID-19 patients with a clinically validated definition of "severe disease" were included in this meta-analysis.
A meta-analysis was performed using Review Manager 5.4 (Cochrane Collaboration) software. Dichotomous variables were calculated using the Mantel-Haenszel formula with random-effects models. We used the I2 statistic to assess the heterogeneity, value of < 25 %, 26–50 %, and > 50 % considered as low, moderate, and high degrees of heterogeneity, respectively. The effect estimate was reported as odds ratio (OR) along with its 95 % confidence intervals (CIs) for dichotomous variables, respectively. P-value was two-tailed, and the statistical significance set at ≤0.05.
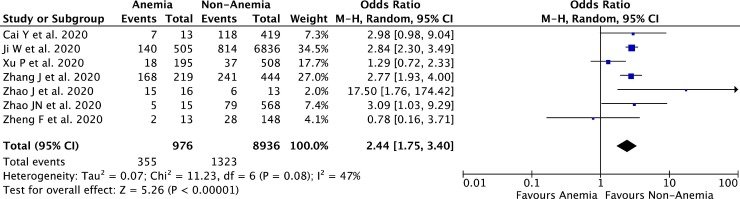
A total of 17,200 records were obtained through systematic electronic searches and other ways. After screening titles, abstracts, and full texts, 7 studies [[2], [3], [4], [5], [6], [7], [8]] with a total of 9,912 COVID-19 patients were included in the meta-analysis. The essential characteristics of the included studies and the cut-off value for anemia diagnosis are summarized in Table 1 . Most of the included studies define anemia when the hemoglobin (Hb) levels were below 13 g/L, while one included study use the cut-off value of Hb <11 g/L to define anemia. The individual and pooled ORs for anemia predicting severe COVID-19 are shown in Fig. 1 . Our pooled analysis showed a significant association of anemia with severe COVID-19, with moderate heterogeneity [OR 2.44 (95 % CI 1.75–3.40), p < 0.00001, I 2 = 47 %, random-effect modelling].
Table 1.
Characteristics of included studies.
| Study | Sample size | Design | Anemia cut-off | Severe patients |
Non-severe patients |
||
|---|---|---|---|---|---|---|---|
| n (%) | Age (years) | n (%) | Age (years) | ||||
| Cai Y et al. [2] 2020 | 432 | Retrospective cohort | Hb <13 g/L | 125 (28.9 %) | 59.6 ± 16.6 | 307 (71.1 %) | 50.1 ± 16.2 |
| Ji W et al. [3] 2020 | 7341 | Case-control | Hb <13 g/L | 954 (12.9 %) | 67 ± 15.1 | 6387 (87.1 %) | 44 ± 17.7 |
| Xu P et al. [4] 2020 | 703 | Retrospective cohort | Hb <13 g/L | 55 (7.8 %) | 60.5 ± 17.2 | 648 (92.2 %) | 44.9 ± 14.3 |
| Zhang J et al. [5] 2020 | 663 | Retrospective cohort | Hb <13 g/L | 409 (61.6 %) | 63.4 ± 17 | 254 (38.4 %) | 48.7 ± 18.5 |
| Zhao J et al. [6] 2020 | 29 | Retrospective cohort | Hb <13 g/L | 21 (72.4 %) | 60.8 ± 19.6 | 8 (27.6 %) | 36.7 ± 20.3 |
| Zhao JN et al. [7] 2020 | 583 | Retrospective cohort | Hb <13 g/L | 84 (14.4 %) | 57.2 ± 12.3 | 499 (85.6 %) | 45.3 ± 17 |
| Zheng F et al. [8] 2020 | 161 | Retrospective cohort | Hb <11 g/L | 30 (18.6 %) | 56.5 ± 14.4 | 131 (81.4 %) | 40.6 ± 14.8 |
Fig. 1.
Forest plot that demonstrates the association of anemia with severe outcome of COVID-19 infection. Events means the severe disease outcome, while non-events means the non-severe disease outcome.
Based on a contrite meta-analysis of available data, anemia seems to be associated with an enhanced risk of severe COVID-19 infection. The possible pathophysiological link between anemia and severe COVID-19 can be explained by these reasons. Patients with anemia will have low hemoglobin levels. In the circulation system, hemoglobin serves as a carrier for oxygen to target organs in the body. When the concentration of the hemoglobin in the circulation is low, the transport of oxygen to several organs in the body will be disrupted, therefore causing hypoxia that will eventually result in multiple organ dysfunction, especially respiratory organ dysfunction [9]. Multiple organ dysfunction will contribute to the development of severe outcomes in COVID-19 infection. Moreover in COVID-19 infections, the state of anemia in the patients could be worsened. First, SARS-CoV-2 can interact with hemoglobin molecules on the erythrocyte through ACE2, CD147, and CD26 receptors. This viral-hemoglobin interaction will cause the virus to attack the heme on the 1-beta chain of hemoglobin and causing hemolysis [10]. Second, SARS-CoV-2 may mimic the action of hepcidin which increases circulating and tissue ferritin (affecting liver, spleen, bone marrow, and muscles mainly), while inducing serum iron deficiency and lack of hemoglobin, by consequence. The resulting hyperferritinemia will give rise to ferroptosis, with high oxidative stress and lipoperoxidation that can precipitate the inflammatory/immune over-response (cytokine storm) and causing a severe outcome of the disease [10]. Patients with anemia should hence be advised to take extra precautions to minimize risk exposure to the virus. Physicians should be engaged in close monitoring of anemic patients with suspected COVID-19, for timely detecting signs of disease progression. Finally, the presence of anemia shall be regarded as an important factor in future risk stratification models for COVID-19.
CRediT authorship contribution statement
Timotius Ivan Hariyanto: Conceptualization, Data curation, Methodology, Investigation, Validation, Visualization, Writing - original draft, Writing - review & editing. Andree Kurniawan: Conceptualization, Validation, Resources, Writing - original draft, Writing - review & editing, Supervision.
References
- 1.Reade M.C., Weissfeld L., Angus D.C., Kellum J.A., Milbrandt E.B. The prevalence of anemia and its association with 90-day mortality in hospitalized community-acquired pneumonia. BMC Pulm Med. 2010;10:15. doi: 10.1186/1471-2466-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cai Y.Q., Zhang X.B., Zeng H.Q., Wei X.J., Zhang Z.Y., Chen L.D. Prognostic value of neutrophil-to-lymphocyte ratio, lactate dehydrogenase, D-Dimer and CT score in patients with COVID-19. Res Square. 2020 doi: 10.21203/rs.3.rs-30959/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ji W., Huh K., Kang M., Hong J., Bae G.H., Lee R. Effect of underlying comorbidities on the infection and severity of COVID-19 in Korea: a nationwide case-control study. J Korean Med Sci. 2020;35(25):e237. doi: 10.3346/jkms.2020.35.e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu P.P., Tian R.H., Luo S., Zu Z.Y., Fan B., Wang X.M. Risk factors for adverse clinical outcomes with COVID-19 in China: a multicenter, retrospective, observational study. Theranostics. 2020;10(14):6372–6383. doi: 10.7150/thno.46833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang J., Wang X., Jia X., Li J., Hu K., Chen G. Risk factors for disease severity, unimprovement, and mortality in COVID-19 patients in Wuhan, China. Clin Microbiol Infect. 2020;26(6):767–772. doi: 10.1016/j.cmi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao J., Gao H.Y., Feng Z.Y., Wu Q.J. A retrospective analysis of the clinical and epidemiological characteristics of COVID-19 patients in Henan Provincial People’s Hospital, Zhengzhou, China. Front Med (Lausanne) 2020;7:286. doi: 10.3389/fmed.2020.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao J., Zhu M., Su X., Huang M., Yang Y., Huang J. Clinical characteristics and risk factors for severe-critically ill COVID-19 adult patients in Jiangsu, China: a multiple-centered, retrospective study. Res Square. 2020 doi: 10.21203/rs.3.rs-28628/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zheng F., Tang W., Li H., Huang Y.X., Xie Y.L., Zhou Z.G. Clinical characteristics of 161 cases of corona virus disease 2019 (COVID-19) in Changsha. Eur Rev Med Pharmacol Sci. 2020;24(6):3404–3410. doi: 10.26355/eurrev_202003_20711. [DOI] [PubMed] [Google Scholar]
- 9.Hemauer S.J., Kingeter A.J., Han X., Shotwell M.S., Pandharipande P.P., Weavind L.M. Daily lowest hemoglobin and risk of organ dysfunctions in critically ill patients. Crit Care Med. 2017;45(5):e479–e484. doi: 10.1097/CCM.0000000000002288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cavezzi A., Troiani E., Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin Pract. 2020;10(2):1271. doi: 10.4081/cp.2020.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]