Abstract
Background
Due to uncertainties encompassing the transmission dynamics of COVID-19, mathematical models informing the trajectory of disease are being proposed throughout the world. Current pandemic is also characterized by surge in hospitalizations which has overwhelmed even the most resilient health systems. Therefore, it is imperative to assess health system preparedness in tandem with need projections for comprehensive outlook.
Objective
We attempted this study to forecast the need for hospital resources for one year period and correspondingly assessed capacity and tipping points of Indian health system to absorb surges in need due to COVID-19.
Methods
We employed age-structured deterministic SEIR model and modified it to allow for testing and isolation capacity to forecast the need under varying scenarios. Projections for documented cases were made for varying degree of containment and mitigation strategies. Correspondingly, data on health resources was collated from various government records. Further, we computed daily turnover of each of these resources which was then adjusted for proportion of cases requiring mild, severe and critical care to arrive at maximum number of COVID-19 cases manageable by health care system of India.
Findings
Our results revealed pervasive deficits in the capacity of public health system to absorb surge in need during peak of epidemic. Also, model suggests that continuing strict lockdown measures in India after mid-May 2020 would have been ineffective in suppressing total infections significantly. Augmenting testing to 1,500,000 tests per day during projected peak (mid-September) under social-distancing measures and current test to positive rate of 9.7% would lead to more documented cases (60, 000, 000 to 90, 000, 000) culminating to surge in demand for hospital resources. A minimum allocation of 13x, 70x and 37x times more beds for mild cases, ICU beds and mechanical ventilators respectively would be required to commensurate with need under that scenario. However, if testing capacity is limited to 9,000,000 tests per day (current situation as of 19th August 2020) under continued social-distancing measures, documented cases would plummet significantly, still requiring 5x, 31x and 16x times the current allocated resources (beds for mild cases, ICU beds and mechanical ventilators respectively) to meet unmet need for COVID-19 treatment in India.
Keywords: Capacity-need gap, Numerical model, COVID-19, Policy, India
1. Introduction
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by a novel strain of coronavirus (SARS-CoV-2) which was first informed as the cluster of viral pneumonia cases of unknown etiology detected in Wuhan City, Hubei Province, China. Coronaviruses are enveloped, positive single-stranded large RNA virus that infect humans, but also a wide range of animals (Velavan & Meyer, 2020). Amongst humans, they have known to cause myriad of illness with varying degree of severity ranging from relatively benign common cold to more severe forms like SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome). However, illness onset among rapidly increasing number of people and mounting evidence human-to-human transmission suggests that SARS-CoV-2 is more contagious than its predecessors (Weekly, 2020).
Following the outbreak of COVID-19, the WHO Emergency Committee declared it a global health emergency on January 30, 2020 and a pandemic on March 11, 2020. Within a short span of time, a localized outbreak evolved into pandemic with three defining characteristics: a) Speed and Scale-the disease has spread quickly to all corners of the world, and its capacity for explosive spread has overwhelmed even the most resilient health systems b) Severity- Overall, 20% cases are severe or critical, with a crude clinical case fatality rate currently of over 3%, increasing in older age groups and in those with certain underlying conditions c) Societal and economic disruption-shocks to health and social care systems and measures taken to control transmission having deep socio-economic consequences (D-19 strategy update, 2020). Currently, approximately 22, 910, 959 confirmed cases of COVID-19 has been reported including an estimated 797,914 deaths in 210 countries and territories as on August 21, 2020.
Around seven months have elapsed since the first case of COVID-19 was reported in India on January 30, 2020. Since then, number of cases have surged to 2,925,337 with 55,174 deaths as on August 21, 2020. As part of the pandemic preparedness, in the absence of vaccines or antivirals, India adapted gamut of non-pharmaceutical interventions such as lockdown, quarantining and tracing and testing concomitantly to alter the trajectory of pandemic. These interventions encompassed two types of strategies a) Suppression, which aims to reverse epidemic growth, by minimizing the effective reproduction number (average number of secondary cases each case generates), R, to below 1 and thus, reduce case numbers to low levels and maintaining that indefinitely b) Mitigation, which aims to slow the spread of epidemic with the rationale of preventing significant overload on health system and gradually allowing the population to develop herd immunity (Ferguson et al., 2020).
WHO enforced a binding instrument of International Health Regulation (IHR) in 2007 to prevent, detect and respond to public health emergencies. The IHR monitoring and evaluation framework includes State Party Annual Reporting Tool (SPAR) which underscores 13 capacity indicators to gauge the preparedness of nations to mitigate the effect of public health emergencies, including the emergence of novel pathogen (WHO, 2018). In 2018, although India’s SPAR composite score (0.75) was above the international average (0.61), albeit, the scores for indicators pertaining to health service provisioning and laboratory capacity were incongruous as India had only half the average readiness in these indicators as compared to international scores. Therefore, it is imperative to unravel the suppply side readiness especially, with regards to infrastructural capacity of India to handle the surge of hospitalization cases.
Need for hospitalization services for COVID-19 can be estimated by analyzing the interface between transmission curve, age-structure, contact patterns and morbidity status of population. Disease progression is characterized by myriad of uncertainties and the trajectory of an epidemic is defined by some key factors and parameters. Specifically, for a novel infection whose disease dynamics are still unclear, mathematical models are thus, pertinent to understand the mechanics of transmission. Deterministic compartmental models such as Susceptible- Exposed-Infectious and Recovered (SEIR) are widely used to provide insight into disease progression and can be chosen over complex models due to minimum number of assumptions. Yet, there is a caveat in using the baseline SEIR model as it does not incorporate the testing capacity in the model which punctuates the dynamics in two ways. Firstly, in basic model, the undetected yet infectious individuals are not accounted in determining probability of infection and potential transmissibility and secondly, there’s reduced transmissibility from confirmed positive cases which no longer transmit the disease once they are tested and isolated. Modelling exercises allowing for testing and isolation capacity and undetected cases are rather scarce. Further, COVID-19 has differential impact on different age groups and additionally, heterogeneities in contact networks have a major effect in determining whether pathogen can become epidemic or persist at endemic levels. Consequently, mathematical models of disease transmission incorporating age and social contact structures are more congruous to the reality.
Therefore, in this study we have attempted the short and long term prediction of transmission of COVID-19 using age-structured compartment based model allowing heterogeneities in contact networks and simulating for varying assumptions and scenarios around containment and mitigation strategies. Drawing from international experience and literature on COVID-19, we determined the proportion of high-risk population with underlying conditions in India who are more vulnerable to progress into severe condition upon infection that can guide triage and targeted intervention decisions. Further, we assessed the capacity and tipping points of Indian health system to absorb surges in the number of people that will need hospitalization and critical care because of COVID-19 based on varying scenarios.
2. Objectives
The objectives of the study can be elucidated as follows: a) Estimate the projected need for hospital resources under various mitigation strategies of reduced social mixing and varying levels of testing capacity in India. b) Analyze the hospital surge capacity of the Indian Health System to absorb the surge in need under different scenarios.
3. METHODS
3.1. Need estimation
3.1.1. Model
The spread of any virus is incumbent upon the infectivity of pathogen and the pool of susceptible population. We formulated the transmission dynamics model for the outbreak of COVID-19 in a heterogeneously mixing population. Compartmental disease models divide population into groups (or compartments) based on each individual’s infection status and track the corresponding population sizes through time. Modified SEIR model in which the population was divided according to infection status into Susceptible(S), Exposed (E), Latency, Infected (I), Quarantined and Removed(R) was employed in the study. Susceptible individuals become infected at a given rate when they interact/contact with an infectious person and enter the exposed state. These exposed pool transition to infectious state after a latency period and later either recover or die. However, it is crucial to consider host age structure to enable realistic modelling for disease prevention policy. Also, the spread of an infectious disease is sensitive to the contact patterns in the population as person-to-person transmission is largely driven by who interacts with whom. The age-specific mixing patterns of individuals in age group i alter their likelihood of being exposed to the virus given the extent of infections in the group. The assumption of homogenously mixing population can lead to an overestimation of the final epidemic size and magnitude of interventions needed to stop an epidemic (Valle et al., 2020). Contrarily, including contact patterns that vary across age and locations (e.g. home, work, and schools) as predictors in transmission dynamic model improves the model’s realism. Thus, we investigated the impact that different mixing assumptions have on the spread of COVID-19 in an age structured SEIR model with infectivity in both latent and infectious period described by a system of ordinary differential equations.
3.1.2. Model map
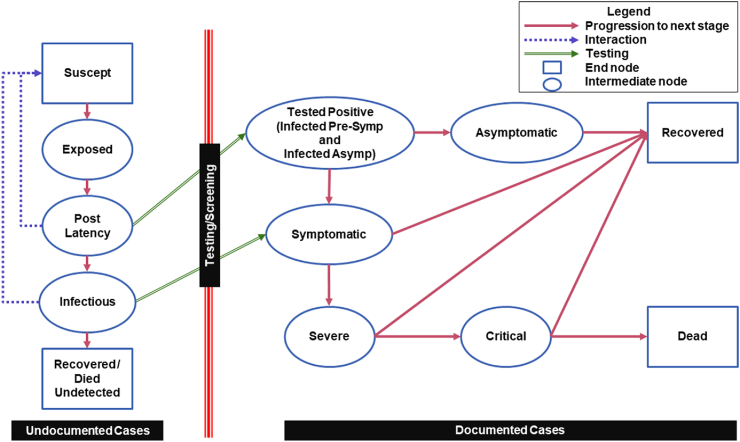
Our model incorporates two sections as illustrated in Fig. 1 where left part represents the classic SEIR model with additional post latency node accounting for infections in the terminal stage of incubation period. The transmission dynamics is further branched out into asymptomatic, symptomatic, severe and critical on the right-hand side constrained by the testing coverage. Following equations represents the dynamics of the model.
| (1) |
where β′ is the probability of infection upon contact with infectious people, N is the total number of considered age groups, Cij is the number of age wise interaction between infectious and susceptible population.
| (2) |
| (3) |
| (4) |
| (5) |
where Si, Ei, Li, Ii and Rui are the susceptible, exposed, post latency, infectious and undocumented recovered group of people of age group i. Rate constant k1 = is defined by time from exposure to onset of infectiousness (latent period), k2′ and k3′ are rate for testing, k2 is defined by part of incubation time after latent period and k3 is rate at which undocumented infectious people recover or die.
| (6) |
| (7) |
Fig. 1.
Model map.
Documented cases in the model are determined and constrained by the testing. Positive cases can be Pre-symptomatic, Symptomatic and Asymptomatic. Pre-symptomatic and Symptomatic may progress to severe and critical state before either recovery or death. Whereas true asymptomatic positives recover without exhibiting any symptoms over the course of illness.
| (8) |
| (9) |
| (10) |
| (11) |
| (12) |
| (13) |
| (14) |
where Tpi is tested positive, Asi is asymptomatic, Ssi is symptomatic, Svi is severe, Cri is critical, Di is dead and Rdi is documented recovered for age group i. Rates of progression are given as follows
| (15) |
| (16) |
| (17) |
| (18) |
| (19) |
| (20) |
| (21) |
| (22) |
To account for the mitigation factor such as social distancing, the contact matrix is divided into household contacts, workplace contacts, school contacts and other contacts using the following form
| (23) |
where tw, ts and to can range from 0 to 1 allowing various degree of interactions of contacts delineating the impact of same on progression of the epidemic.
3.1.3. Model parameters and data
Main parameters of the model are surmised in Table 1 which were extracted/estimated from various sources. Population age distribution for India was obtained from website of Population Pyramid (Population Pyramid: India, 2020) and Social Contact Matrices were adapted from state-of-the-art compilation by Prem et al. in which matrices were projected by Bayesian hierarchical model for 152 countries using contact surveys and demographic data (Prem et al., 2017). Time parameters were extracted from a systematic review which synthesized parameters using meta-analysis of 43 studies on COVID-19 (Khalili et al., 2020). Further, age-distributed data from U.S. was used to estimate the epidemiological parameters in the study. As reported in Table 2, age wise fractions of transition from one state to another and case fatality ratio (CFR) was calculated from the report published by U.S. Center for Disease Control (Chow et al., 2019), as CFR in India is analogous to that of USA when CDC carried out the study. Also, we collated the data on confirmed positive cases, hospitalizations, recovery and deaths from publicly available time series data of USA published by U.S. CDC to estimate the probability of infection β’. Remaining model parameters such as latency rate, testing rate and rate of recovery/death were estimated using crowdsourced Indian data (COVID-19 India Tracker) from March 10, 2020 till August 19, 2020 while incorporating mitigation strategies of lockdown starting from March 24 to May 3 and current social distancing guidelines based on the zones which is issued by Indian government starting from May 3, 2020 till date. Three scenarios of mitigation measures were modeled – (a) Full lockdown (assuming closure of schools, workplace and community spaces and doubling of contacts in households) (b) Social distancing measures or moderate lockdown (assuming closure of schools, staggered opening of workplace and community spaces with half strength and social distancing of vulnerable population including aged above 70 years and people with at-least one underlying high risk chronic condition with 75% compliance) and (c) No lockdown (assuming 100% contacts in schools, workplace, community spaces and households). The model is augmented to incorporate the testing coverage and Test to positive (TTP) ratio of average 8.35% till date in India.
Table 1.
Parameters used in the model equations.
| Name | Parameter | Value | Reference |
|---|---|---|---|
| Incubation time | t_i | 5.83 ± 0.515 | Meta-analysis (Khalili et al., 2020) |
| Symptomatic to Recover time | t_s_r | 11.76 ± 2.61 | Meta-analysis (Khalili et al., 2020)) |
| Symptomatic to Severe time | t_s_sv | 4.82 ± 0.683 | Meta-analysis (Khalili et al., 2020) |
| Severe to Recover time | t_sv_r | 17.76 ± 2.61 | Meta-analysis (Khalili et al., 2020) |
| Sever to Critical time | t_sv_c | 5.66 ± 0.765 | Meta-analysis (Khalili et al., 2020) |
| Critical to Recover time | t_c_r | 17.76 ± 2.61 | Meta-analysis (Khalili et al., 2020) |
| Critical to Dead time | t_c_r | 5.45 ± 1.49 | Meta-analysis (Khalili et al., 2020) |
| Testing time | t_test | 1 | Estimated from crowdsourced Indian data (https://www.covid19india.org/) |
| Latency time | t_latency | 1.5 | Estimated from crowdsourced Indian data (https://www.covid19india.org/) |
| Rate of recovery/death | k3 | 0.1 | Estimated from crowdsourced Indian data (https://www.covid19india.org/) |
| Test to positive ratio | – | 9.7% | Estimated from crowdsourced Indian data (https://www.covid19india.org/) |
| Probability of infection | 0.074 | Estimated from India’s data on reported cases (from March 10 to August 19, 2020) | |
| Positive to pre-symptomatic/symptomatic ratio | – | 98% | ECDC (Eurosurveillance, 2020) |
Table 2.
Age wise fractions in symptomatic, severe, critical, dead and recovered. Source- U.S. Center for Disease Control.
| Age Groups (N = 5) | Fraction | Value |
|---|---|---|
| 0–14 | Fraction symptomatic to recover | 97.95% |
| 0–14 | Fraction Severe | 2.05% |
| 0–14 | Fraction Critical | 0% |
| 0–14 | CFR | 0% |
| 15–49 | Fraction symptomatic to recover | 76.99% |
| 15–49 | Fraction Severe | 18.67% |
| 15–49 | Fraction Critical | 4.08% |
| 15–49 | CFR | 0.26% |
| 50–69 | Fraction symptomatic to recover | 60.89% |
| 50–69 | Fraction Severe | 27.77% |
| 50–69 | Fraction Critical | 9.26% |
| 50–69 | CFR | 2.09% |
| 70–80 | Fraction symptomatic to recover | 40.01% |
| 70–80 | Fraction Severe | 38.95% |
| 70–80 | Fraction Critical | 15.93% |
| 70–80 | CFR | 5.02% |
| 80 + | Fraction symptomatic to recover | 18.84% |
| 80 + | Fraction Severe | 48.19% |
| 80 + | Fraction Critical | 18.96% |
| 80 + | CFR | 14.02% |
3.1.4. Model assumptions
The underlying set of assumptions characterizing the transmission dynamics are elucidated as follows-
-
i)
India was assumed to be a closed system with constant population size of 1.3 billion (S + E + L + I + R = 1.3 billion) throughout the course of epidemic.
-
ii)
Different inflows and outflows and imbalance by demographics, migration etc. is not considered.
-
iii)
Seasonal effects, weather conditions like temperature and humidity and mutations not included in the model.
-
iv)
Heterogeneous mixing in the contact networks is assumed and interactions at four spheres are considered: home, work, school and other locations.
-
v)
Infectivity from latency period is considered, a latent individual can transmit the disease to the susceptible, i.e., individual has force of infection in both latent and infectious period.
-
vi)
Asymptomatic transmission from truly asymptomatic cases is accounted in the model.
-
vii)
Positively diagnosed cases are documented and isolated from rest of the susceptible pool, thus, less likely to spread the infection.
-
viii)
The recovered individuals develop the immunity and do not revert back to the susceptible pool.
3.2. Proportion of high-risk individuals
Multi country evidence suggests that there are certain underlying conditions most associated with severe and critical cases of COVID-19. In conjunction with elderly, younger and working population group with chronic health conditions are also vulnerable and can be classified as high risk for developing complications. U.S. Center for Disease Control and Prevention in its Morbidity and Mortality Weekly report (COVID & Rep, 2020) divulged that, 71% hospitalized non-ICU cases and 78% ICU cases had one or more precondition. Similarly, early evidence from Italy (Onder et al., 2020) affirmed that in a sample of 355 deaths in Italy, 99.2% patients had some pre-condition(s). Overall, among dead, 25.1% had single disease, 25.6% had 2 diseases and 48.5% had 3 or more underlying diseases in Italy. Therefore, analyzing the prevalence of high-risk underlying condition associated with COVID-19 is germane to understand the progression of cases from mild to severe/critical stage and identify the vulnerable population to design more effective interventions. Hence, we used the information on burden of chronic diseases from a study conducted by London School of Hygiene and Tropical Medicine (Clark et al., 2020) in which number of individuals at increased risk of severe COVID-19 disease were estimated for 188 countries. The study identified following underlying conditions characterizing high-risk groups and special populations requiring urgent care (a) HIV/AIDS (b) Tuberculosis (c) Cancers with direct immunosuppression (d) Cancers with possible immunosuppression (e) Cardiovascular diseases (f) Chronic respiratory diseases (g) Cirrhosis and other chronic liver diseases (h) Diabetes mellitus (i) Chronic kidney diseases (j) Chronic neurological disorders (h) Sickle cell disorders. Therefore, we used the information on prevalence of these underlying conditions in India (Table 3) by culling out information from above-mentioned study to estimate proportion of population with at-least one underlying condition.
Table 3.
Fraction of India’s population with 1+ and 2+ underlying conditions.
| Age Group | % people with 1+ condition | % people with 2+ condition |
|---|---|---|
| 0–14 | 6.5 | 0.4 |
| 15–49 | 19.0 | 2.4 |
| 50–69 | 49 | 14.0 |
| 70–80 | 69.9 | 29.8 |
| 80 + | 79.9 | 49.3 |
Source:Clark et al., 2020
3.3. Estimating health system surge capacity
Data on Indian health infrastructure was coalesced from different sources. Information on beds in public hospitals (PHC + CHC + DH) and Medical College Hospitals was extracted from National Health Profile, 2019 (Central Bureau of Health Intelligence, 2019). However, there was missing information in this data source for some states and colleges, which was then scrapped individually from websites of the colleges. Beds under AYUSH, Defense, Railways and ESI Corporation are also incorporated in the analysis as India is likely to rope in beds from these institutions during surge in need. The data for bed availability in these institutions was taken from National Health Profile, 2018 (Central Bureau of Health Intelligence, 2018). Further, due to absence of veritable data available on private sector, approximations using utilization rates for hospitalizations in private hospitals from recently released National Sample Survey Organization 75th round (Ministry of statstics and programme implementationG of I) was used and crude estimations were made based on proportion of inpatients treated in private hospitals. Further, there is major lacunae in credible data availability for ICU beds and ventilators required for critical care. Henceforth, another assumption was made that only 5% of total beds are ICU beds and 50% ICU beds are equipped with ventilators in India.
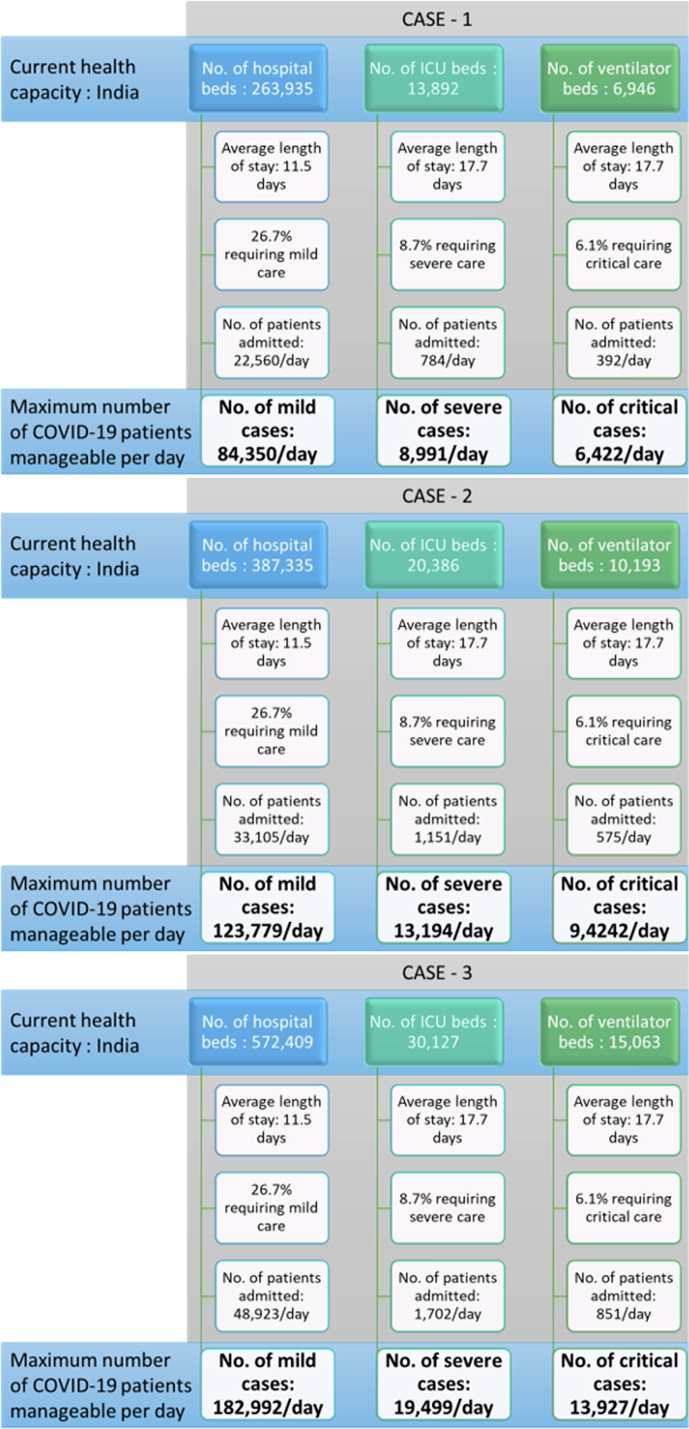
Health system’s capacity to accommodate the increasing number of COVID-19 patients was computed using an open access tool developed by Giannakeas et al. (2020) (Giannakeas et al., 2020). This tool enables the modelling of steady state patient flow dynamics that can guide the tipping point of health care system in terms of the availability of hospital beds, ICU beds and mechanical ventilators. Entire dynamics of capacity readiness is explained in Fig. 4. The left-hand panel in the figure is representative of the current health capacity with total number of hospital beds, ICU beds and ventilators. Average length of stay determining the daily turnover rates for mild, severe and critical cases were set as 11.76 days, 17.76 days and 17.76 days respectively (parameter values from model). Using population-weighted age-stratified probabilities, number of cases requiring hospital beds, ICU beds and ventilators was estimated. Further, the daily turnover of each of these resources was measured by dividing the number of available resources with average length of stay for that resource. Thereafter, the daily turnover rates were divided by the proportion of cases requiring mild, severe and critical care to arrive at the maximum number of COVID cases manageable by health care system of India. Three distinct cases based on the allocation of resources were made to discern the surge capacity for each of these cases. In all three cases, we assumed that public health facilities dedicate fixed 20% of their hospital beds, ICU beds and ventilators for COVID-19 patients since existing bed occupancy rate of public hospitals in India is high around 94% (Sanyal, 1995) and excess capacity is not available. However, for private sector hospitals, varied assumptions pertaining to allocation was made. Under case 1, the provision of private infrastructure was assumed to be 5%. Whereas, the allocation of hospital beds, ICU beds and ventilators in private hospitals was 15% under case 2 and further expanded to 30% under case-3.
Fig. 4.
Maximum daily number of incident COVID-19 cases manageable by healthcare system.
4. Results
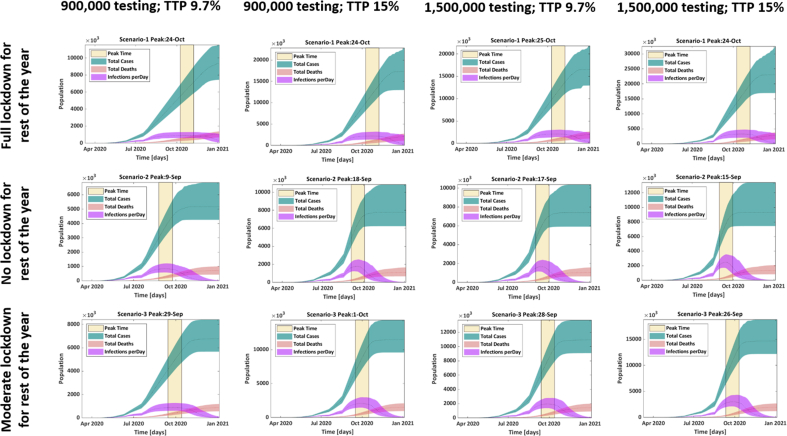
Main findings of the study are presented in this section. Fig. 1 encapsulates various transmission curves under the scenario of ramping up of testing coverage (number of individuals tested daily) and increased TTP from 9.7% to 15% if the pandemic leads to more widespread community transmission. The impact of other non -pharmaceutical interventions like social distancing and lockdown is also explicated in the figure. While the lockdown was effective in slowing down the infection rate and shifting the peak to later months of the year 2020, it perpetuated heavy socio-economic costs in India. Therefore, it is pertinent to compare how continuing with moderate lockdown/social-distancing measures or lifting the restrictions completely would impact the number and spread of total COVID-19 cases in India.
4.1. Projected need for hospital resources
The detailed representation of our modelling results is exhibited in Fig. 2. Our modelling exercise revealed that with the current testing rate of 900,000 individuals tested daily in India as of August 19, 2020 and 9.7% TTP ratio, the estimated total documented COVID-19 infections in India would range from (5,000,000 to 9,000,000 in an year) across the scenarios of no lockdown, full lockdown and moderate lockdown guidelines. Lifting the restrictions completely for rest of the year, would hasten the surge in need to mid-September as compared to late-October if the full lockdown continues for rest of year. Although, continuing with restrictions would push the maximum surge to late-September, however, total number of infections will not plummet by this intervention.
Fig. 2.
Scenarios of full lockdown, no lockdown and social distancing measures/moderate lockdown compared with varying testing rates for India for rest of the year.
Average (from March 10, 2020 to August 19, 2020) TTP ratio in India is around 8.35%, however current TTP ratio in India (as on August 19, 2020) is 9.7%. Thus, we estimated the number of total infections and peak time dynamically to account for surge in need with 900,000 tests per day (as being conducted currently) and at the further augmented capacity of 1,500,000 tests per day at 9.7% TTP as well as at 15% TTP accounting for the current situation (as on August 19, 2020) as well as worst case scenario.
Assuming limited community spread with TTP of 9.7% and augmenting the testing to 1,500,000, in the absence of lockdown, our model estimated the peak to be around mid- September with total documented cases ranging from 5,500,000 to 6,500,000 during peak time. However, continuing restrictions (with 50% contacts in workplaces and public places, and no schools), estimated number of documented cases would be around 8,000,000 at the peak time of ending-September. With this increased testing of 1,500,000 individuals per day, surge in need would be highest (~12, 000, 000) if stringent lockdown measures would have been imposed for rest of the year starting from May 17, 2020 which marked the ending of strict lockdowns in India. This higher surge in need is because complete lockdown will delay the overall community spread and more people will be diagnosed and tested positive during peak time.
Under the worst case scenario of community spread in India with TTP of 15% and current testing capacity of 9,000,000 per day, peak will be witnessed around mid-September 2020 to late-October 2020. Total documented infections under current moderate lockdown scenario will range from 7,000,000 to 10, 000, 000 around early-October. However, the total documented infections will increase with higher testing rate of 1,500,000 individuals per day ranging from 10, 000, 000 to 12, 000, 000 cases around peak time by late –September. In a no lockdown situation during worst case scenario with TTP 15%, number of cases would have peaked around 10 days ahead with similar number of infected cases in moderate lockdown.
4.2. Estimated surge capacity of indian healthcare system
Our analysis indicated paucity of resources in India to handle surge in need during the peak time for both mild infections and severe cases. The capacity of Indian healthcare system to absorb increases in caseload is constrained by availability of beds and ventilators. India has a total (public + private) bed capacity of 2,363,296 which can be allocated for COVID-19 infections according to existing bed occupancy rate and government guidelines. The availability of health care infrastructure which is collected from multiple sources is presented in Table 4. According to Case-1 where only 5% allocation is made by private sector and 20% resources are dedicated in public infrastructure, actual availability of hospital beds, ICU beds and ventilators is 202,261, 13,892 and 6946 respectively. The estimated inflow/outflow of mild, severe and critical cases per day are 22,560, 784 and 392 respectively. Under this scenario, India has the capacity to accommodate only 84,350 mild cases, 8991 severe and 6422 critical new COVID cases every day. However, leveraging upon expansive private health care system, India can bolster the capacity. The tipping point for beds and ventilators increases significantly when 15% (case-2) and 30% (case-3) private health care resources were assumed to earmarked to accommodate COVID-19 patients. For example, under case-2, we found that the surge capacity of health system for mild, severe and critical care is distinctly higher than case 1 as can be seen in Fig. 3 and Fig. 4. Moreover, when the allocation of private infrastructure increases by 30%, the capacity to manage new COVID cases doubles.
Table 4.
Number of hospital beds, ICUs and ventilators available in India.
| OVERALL | AVAILABILITY FOR COVID |
SOURCE | |||
|---|---|---|---|---|---|
| CASE 1 | CASE 2 | CASE 3 | |||
| TOTAL HOSPITAL BEDS | |||||
| Government Hospitals | 739,024 | 147,805 | 147,805 | 147,805 | National Health Profile, 2019 |
| Medical Colleges | 202,233 | 40,447 | 40,447 | 40,447 | National Health Profile, 2019 and scrapping missing data from college websites. |
| ESI Hospitals | 19,765 | 3,953 | 3,953 | 3,953 | National Health Profile, 2018 |
| Railways | 13,748 | 2,750 | 2,750 | 2,750 | National Health Profile, 2018 |
| Defense | 34,520 | 6,904 | 6,904 | 6,904 | National Health Profile, 2018 |
| AYUSH | 55,242 | 11,048 | 11,048 | 11,048 | National Health Profile, 2018 |
| Public Beds | 1,064,532 | 212,906 | 212,906 | 212,906 | |
| Private beds | 1,298,764 | 64,938 | 194,815 | 389,629 | Approximation from NSSO 75th round data |
| Total beds (Public + Private) | 2,363,296 | 277,845 | 407,721 | 602,536 | |
| RESOURCES AVAILABLE FOR SEVERE AND CRITICAL CASES | |||||
| ICU beds (Public) | 53,226 | 10,645 | 10,645 | 10,645 | |
| ICU beds (Private) | 64,938 | 3247 | 9741 | 19,481 | |
| ICU beds (Public + Private) | 118,164 | 13,892 | 20,386 | 30,127 | |
| Ventilators (Public) | 26,613 | 5323 | 5323 | 5323 | |
| Ventilators (Private) | 32,469 | 1623 | 4870 | 9741 | |
| Ventilators (Public + Private) | 59,082 | 6946 | 10,193 | 15,063 | |
| RESOURCES AVAILABLE FOR MILD CASES | |||||
| Public Beds | 1,011,306 | 202,261 | 202,261 | 202,261 | |
| Private Beds | 1,233,826 | 61,691 | 185,074 | 370,148 | |
| Total Beds | 2,245,132 | 263,953 | 387,335 | 572,409 | |
Assumption: Case1- 20% public beds and 5% private beds are dedicated for COVID patients. Case 2–20% public beds and 15% private beds are dedicated for COVID patients. Case 3–20% public beds and 30% private beds are dedicated for COVID patients.
ICU Beds and Ventilators: Case1- 20% ICU beds & Ventilators in public hospitals and 5% in private hospitals. Case 2- 20% ICU beds & Ventilators in public hospitals and 15% ICU beds in private hospitals are dedicated for COVID patients. Case 3- 20% ICU beds & Ventilators in public hospitals and 30% ICU beds & Ventilators in private hospitals are dedicated for COVID treatment.4.3Capacity-need gap under various scenarios.
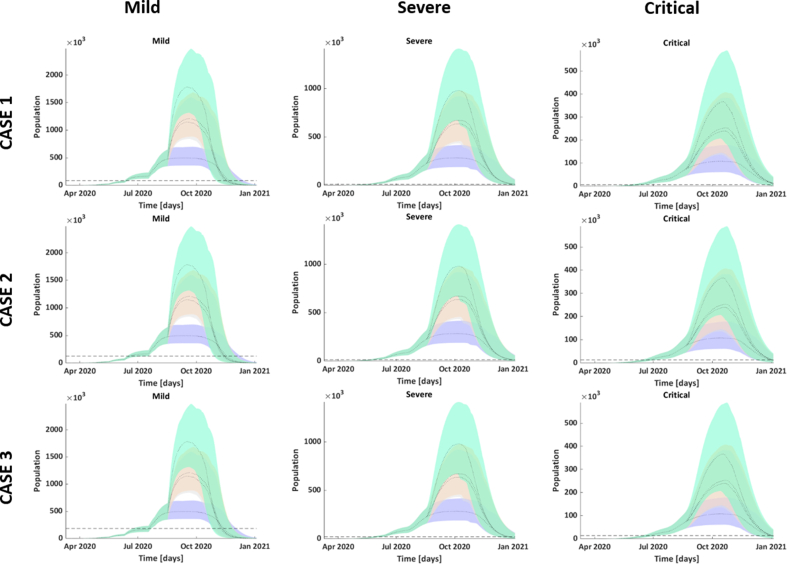
Fig. 3.
Assessing need for varying level of severity under Moderate Lockdown. Blue: 900,000 tests with 9.5% ttp; Peach: 900,000 tests with 15% ttp; Grey: 1,500,000 tests with 9.5% ttp; Cyan: 1,500,000 tests with 15% ttp.
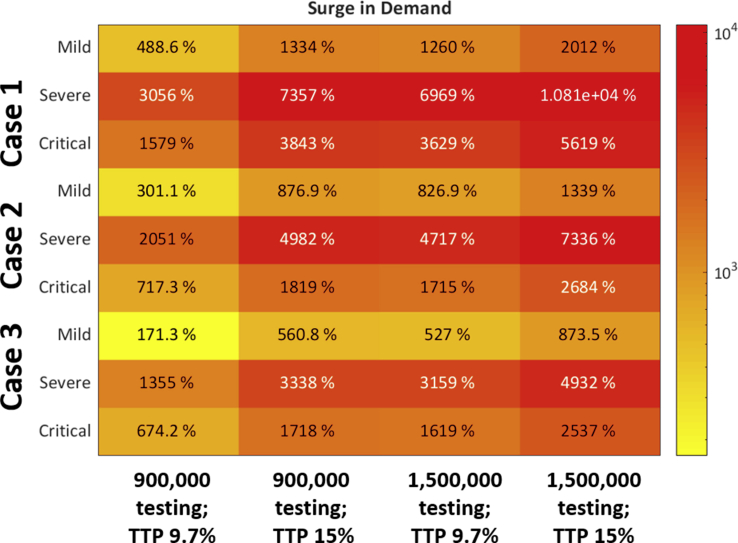
We computed the surge capacity, which is determined by trajectory of cases and infrastructure dedicated to COVID-19 patients by accessing the time period around which Indian hospitals will face serious crisis in terms of availability of beds and ventilators. The capacity-need gap during peak time if the social distancing measures and restrictions is continued for rest of the year for mild, severe and critical cases is presented in the form of heat map (Fig. 5). Coloured boxes suggest the extent of health infrastructure that must be upgraded to meet the real need during peak time. As mentioned earlier, surge capacity is likely to vary across different testing scenarios. For example, when the current social distancing measures are considered with current testing coverage of 900,000 per day and current TTP of 9.7%, our capacity and need side projections indicate that the Indian health care system is facing a huge deficit in terms of the availability of health care infrastructure, especially for severe and critical case.
Fig. 5.
Percent beds available (green) and needed (non-green) from maximum capacity during peak time if moderate lockdown continues with multiple increased testing scenarios.
Refer Table 4 for cases definitions.
Assuming the community spread and scaling up of testing to 1,500,000 tests per day with TTP of 15%, if resources are allocated as per Fig. 4, Case-1; India will have to increase the availability of ICU beds and availability of ventilators by 57 times (5619%) before peak time around late-September. However, under current scenario where TTP is 9.7%, if we increase testing to 1,500,000 cases per day, we will have to ramp up the availability of ICU beds by 6969% and ventilators by 3629% before peak time around ending-September. However, augmenting the resource allocation as per Fig. 4, Case-3; where 20% of capacity in public facilities and 30% in private facilities is apportioned for COVID-19, and testing coverage is 900,000 per day with TTP of 9.7%, the estimated need for severe and critical cases can only be met if capacity of ICU beds and ventilators is increased further by 1355% and 674% before ending-September. If community spread is assumed with TTP of 15%, at current testing rate of 900,000, number of ICU beds must be increased by 3338%, and capacity of ventilators has to be increased by 1718% before starting-October in addition to resources dedicated for COVID-19 as per case 3. Currently, on the other hand, resources are not allocated even according to Case 1 in India culminating into massive bed shortage. Therefore, necessary steps must be made to by adding new public resources and including private-sector hospitals in the treatment of COVID-19 patients in order to be prepared for the widespread community transmission and increase in detected cases due to aggressive testing. Time to surge in capacity or tipping point will occur much earlier than the peak. Hence, this analysis delineates an urgent need of procuring the ventilators and upgrading the capacity in this month and a half time window.
5. Discussion
Our study calibrated the model to preliminary data arising from outbreak in India in order to project the need for hospital resources under three transmission curve scenarios: No lockdown, Moderate lockdown and Full lockdown across varying testing coverage. We also evaluated the extent to which the full lockdown and moderate lockdown delays the peak of outbreak, thereby, prolonging the window of time to augment the health-system capacity in order to accommodate the surge in need during peak period. Our analysis of Indian healthcare system’s preparedness to absorb surges for infected cases exhibited pervasive deficits. There was a substantial variation in tipping points of surge capacity across the assumptions on resource allocation in private sector to accommodate COVID-19 patients.
One of the important finding of our analysis is that extending lockdown after May 17, 2020 which marked the ending of strict lockdowns in India would have been ineffective, as lockdown is only likely to push the surge in need for hospital resources by a month without suppressing the total number of cases significantly. India was amongst the countries to implement lockdown early with highest stringency in the world which is also indicated by the stringency index of lockdown (100% for India) prepared by University of Oxford (Hale et al., 2020).
Due to the high costs of lockdowns, there is a policy conundrum if the countries should quarantine everyone at a large social cost or test everyone and apply quarantine in a more directed fashion. The increase in documented cases with augmented testing in our study suggests that there should be thrust on public health intervention of testing, tracing and isolating in conjunction with surveillance and real time data. More targeted sequestering of infected case (both symptomatic and asymptomatic) aided with increased random testing, along-with the social distancing measures for containment zones with higher incidence of cases and isolating vulnerable with underlying conditions and aged population is recommended.
Our analysis underscored the absence of surge capacity for severe and critical cases under all the transmission and testing scenario. The shortage of beds for even mild and asymptomatic cases can be corroborated with the reports as early as May 2020 from Indian cities of Chennai (The New Indian Express. R, 2020) and Mumbai (Business Today. Coronavir, 2020) where government hospitals are running out of beds due to explosion of cases. Many countries are resorting to home isolation of mild and asymptomatic cases, a measure which Union Health Ministry of Indian government has also announced. However, we recommend ramping up institutional capacity to isolate infected cases under institutional care as India’s congested housing conditions are not conducive to quarantining at home. The National Sample Survey Office data (Ministry of statstics and programme implementation, 2020) reveals that for 60% Indians, per capita space available is less than a single room leading to unprecedented challenges for effective home isolation.
Our model did not consider the potential staff shortages in transmission dynamics and capacity readiness due to uncertainty around their predictions and unavailability of quality data. Age-distributed data on severe, critical and recovered cases is rather sparse in India, therefore, we adapted/estimated some parameters from detailed data released by other countries. Modelling is rather a necessary input to guide policy decisions, however, a more comprehensive approach incorporating stakeholder’s analysis, case studies and triangulating information across multitude of sources should be adapted for nuanced decision making. The study can be further extended to map the geographical accessibility of facilities providing COVID-19 care, specifically spatial accessibility for critical care needs to be explored. Also, rapid health facility assessments for COVID-19 preparedness unravelling mean availability of tracer items for emergency response should be conducted for targeted interventions at hospital level. Finally, study can be extended at more granular level to inform capacity-need gap so that resources can be mobilized in commensuration with need at more local level, thereby enabling local government systems to combat COVID-19 in India.
Data availability
Data used in this study has been reported in the form of tables in this manuscript.
Statement of ethical approval
Ethical approval not required as human subjects are not involved in this study.
Funding
The study is not funded by any agency/organization.
Declaration of competing interest
None declared.
Handling editor: Dr. J Wu
Footnotes
Peer review under responsibility of KeAi Communications Co., Ltd.
References
- Business Today. Coronavirus: Mumbai hospitals face bed, medical personnel shortage as cases rise. https://www.businesstoday.in/current/economy-politics/coronavirus-mumbai-hospitals-face-bed-medical-personnel-shortage-as-cases-rise/story/403016.html [Internet]. [cited 2020 May 14]. Available from:
- Center for Disease Control and Prevention U.S. https://www.cdc.gov No Title [Internet]. Available from:
- Central Bureau of Health Intelligence Directorate general of health services M of H and FW. National health profile. 2018. [Internet]. 13th Issue. 2018. Available from: http://www.cbhidghs.nic.in/Ebook/National Health Profile-2018 (e-Book)/files/assets/common/downloads/files/NHP 2018.pdf.
- Central Bureau of Health Intelligence Directorate general of health services M of H and FW. National health profile. 2019. http://www.cbhidghs.nic.in/showfile.php?lid=1147 [Internet]. 2019. Available from:
- Chow N., Fleming-Dutra K., Gierke R., Hall A., Hughes M. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 — United States. https://stacks.cdc.gov/view/cdc/87230 February 12–March 28, 2020 [Internet]. 2020 [cited 2020 May 14]. Available from: [DOI] [PMC free article] [PubMed]
- Clark A, Jit M, Warren-Gash C, Guthrie B, Wang HH, Mercer SW, et al How many are at increased risk of severe COVID-19 disease? Rapid global, regional and national estimates for 2020. medrxiv.org [Internet]. [cited 2020 May 7]; Available from: https://doi.org/10.1101/2020.04.18.20064774.
- Covid-19 India Tracker https://api.covid19india.org/ [Internet]. Available from:
- COVID-19 strategy update (as of 14 April 2020)–Mise à jour de la stratégie COVID-19. https://www.who.int/docs/default- (au 14 avril 2020) [Internet]. apps.who.int. [cited 2020 May 13]. Available from:
- Covid C., Rep RT-MMMW . 2020. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, february 12–march 16, 2020.https://www.cdc [Internet]. ecie.com.ar. 2020 [cited 2020 May 13]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eurosurveillance E.E.T.- undefined. Updated rapid risk assessment from ECDC on the novel coronavirus disease 2019 (COVID-19) pandemic: increased transmission in the EU/EEA and the UK. ncbi.nlm.nih.gov. 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7078827/ [Internet]. [cited 2020 May 12]; Available from:
- Ferguson N., Laydon D., Gilani G.N., Imai N. 2020. Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand.https://spiral.imperial.ac.uk/handle/10044/1/77482 [cited 2020 Apr 23]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannakeas V., Bhatia D., of I M.W.-A. 2020. Estimating the maximum capacity of COVID-19 cases manageable per day given a health care system’s constrained resources.https://annals.org/aim/fullarticle/2764818 undefined. annals.org [Internet]. [cited 2020 May 10]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T, Angrist N, Kira B, Petherick A, Phillips T, Webster S. Variation in government responses to COVID-19 [Internet]. bsg.ox.ac.uk. 2020 [cited 2020 May 11]. Available from: www.bsg.ox.ac.uk/covidtrackerme.
- Khalili M, Karamouzian M, Nasiri N, Javadi S, Sharifi H. Epidemiological characteristics of COVID-19; A systemic review and meta-analysis 1. medrxiv.org [Internet]. [cited 2020 Apr 28]; Available from: https://doi.org/10.1101/2020.04.01.20050138.
- Ministry of statstics and programme implementation. Drinking water, sanitation, Hygiene and housing condition in India, NSS 76th Round [Internet]. 2020. Available from:http://www.mospi.gov.in/sites/default/files/publication_reports/Report_584_final_0.pdf.
- Ministry of statstics and programme implementation G of I. Social consumption:health, NSS 75th Round.
- The New Indian Express. Running out of beds, Chennai hospitals shifting COVID-19 patients to quarantine centres [Internet]. [cited 2020 May 14]. Available from: https://www.newindianexpress.com/cities/chennai/2020/may/04/running-out-of-beds-chennai-hospitals-shifting-covid-19-patients-to-quarantine-centres-2139062.html.
- Onder G., Rezza G., Jama S.B.- 2020. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy.https://jamanetwork.com/journals/jama/article-abstract/2763667 undefined. jamanetwork.com [Internet]. [cited 2020 Apr 30]; Available from: [DOI] [PubMed] [Google Scholar]
- Population Pyramid: India https://www.populationpyramid.net/india/2020/ [Internet]. Available from:
- Prem K., Cook A.R., Jit M. Projecting social contact matrices in 152 countries using contact surveys and demographic data. PLoS Computational Biology. 2017 Sep 1;13(9) doi: 10.1371/journal.pcbi.1005697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanyal SK. UTILIZATION PATTERN AND FINANCING OF PUBLIC HOSPITALS: A REPORT ˆ [Internet]. nipfp.org.in. 1995 [cited 2020 May 10]. Available from:.
- Valle SY D., Hyman JM, Chitnis N. Mathematical models of mixing patterns between age groups for predicting the spread of infectious diseases. pdfs.semanticscholar.org [Internet]. [cited 2020 Apr 25]; Available from: https://pdfs.semanticscholar.org/ed6e/e5e494e6183a00fbbd9106d313c2c3ce89cf.pdf.
- Velavan TP, Meyer CG. The COVID-19 epidemic. blogs.e-me.edu.gr [Internet]. 2020 [cited 2020 Apr 22]; Available from: 10.1101/2020. [DOI]
- Weekly V.S.-C.C. 2020. https://cdn.onb.it/2020/03/COVID-19.pdf.pdf undefined. Method Study Design [Internet]. cdn.onb.it. [cited 2020 May 13]. Available from:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used in this study has been reported in the form of tables in this manuscript.