Highlights
-
•
This article provides insights into the evolution and implications of the Norwegian policy response to the COVID-19 crisis.
-
•
Three different agendas motivated the Norwegian policy response: limiting disease spread, mitigating economic effecs and engaging with the social consequences.
-
•
The oil and gas industry and the Sovereign Wealth Fund insulate Norway from the full economic consequences of the pandemic and policy response.
-
•
The social implications of the policy response and the pandemic, particularly on young people are a key consideration for the emergence from the crisis.
Keywords: Norway, COVID-19, Policy, Social impact
Abstract
Objectives
To describe the impact and policy response to the COVID-19 Pandemic on Norway and the implications this has for future policy development and Norwegian society.
Methods
Documentary analysis of publicly available statistics, government documents and media sources.
Results
Three different agendas motivated Norwegian policy: stemming the spread of the virus domestically, mitigating the impact on the economy and addressing the social costs of the policy response.
Conclusions
The oil and gas industry and the Sovereign Wealth Fund have permitted Norway to manage the costs of the pandemic. But may also lead to a shift in government priorities in health, social and economic policy.
Introduction
This article describes the response to the COVID-19 epidemic in Norway. The Norwegian context provides a number of distinctive elements that make it an interesting case for considering government thinking, the policy response and the engagement of the public in a global crisis. Norway has a special relationship with the other Nordic countries (Denmark, Finland, Iceland and Sweden) including significant policy transfer and favourable treatment on a range of issues. While operating a Bevridgean publicly funded national health system, the dispersed population of Norway creates particular challenges in terms of travel, provision and access. In common with the other Nordic countries, the Norwegian population exercises significant trust in the state which operates within a consensual form of policy making. Finally, the oil and gas sector is extremely important to the Norwegian economy constituting in 2018 18% of GDP and 62% of exports. As the seventh largest exporter of crude oil internationally, the collapse of the oil price inevitably has implications for government policy responses to the COVID-19 crisis.
Initially we describe the characteristics of Norway and its population before considering the organisation and utilisation of health services. We go on to detail the policy responses to the COVID-19 crisis before reflecting on the implications and distinctive aspects of the Norwegian policy response. In particular, we consider the justification for the evolution of the government response and the way that the social implications of lockdown shaped the policy discourse.
Norway and the Norwegian health system
Norway is a prosperous country with a population of 5.3 million and a GDP per capita of €43,900. It is a high tax economy with the top personal income tax rate of 47.8% and corporate tax rate of 22% and an overall tax burden of 38.2% of domestic income. Life expectancy at birth is the third highest in the EU at 82.7 [1] with a small education gap, although women live an average of 3.3 years longer than men. The over-65-year old's make up 17% of the population with a median age of 39.5 and an elderly dependency rate of 26.9 [1]. Most of the population is concentrated in the south of the country and 83% live in urban areas but there are significant dispersed populations as the overall population density in 2016 was 14.3 people per square kilometre of land area [2].
Norway has a healthy population with limited health disparities, but ischemic heart disease is the single largest cause of death. One in seven adults is obese, there are low levels of smoking (10% of adults) but other forms of tobacco use have risen over the last 20 years [1]. In part, due to high taxation, alcohol consumption for adults and adolescents is low at just under seven litres per person per year.
Like other Nordic countries and the United Kingdom, Spain, Italy and New Zealand, Norway has a public financed national healthcare system (a Bevridgean system) providing universal coverage for all residents financed through general taxation (74%), the national insurance scheme (11%) and private expenditure (15%) while private health insurance is marginal covering less than 5% of elective services [1]. Co-payment is capped but relates primarily to dental care and outpatient pharmaceuticals. In 2017, Norway spent 10.4% of GDP on health or €4,545 per capita [1].
A decentralised system, the government owns the four regional health authorities that manage hospital services and employ staff. The municipalities manage primary care, long-term care and social services and general practitioners are self-employed but integrated into the public system via contracts. The for-profit hospital sector is tiny providing less than 0.2% of hospital stays and 7% of daytime stays [1].
Prior to the Pandemic there were 2.9 physicians (2018 WB), 3.9 hospital beds (2013 WB) and 18.2 nurses and midwives (2018 WB) per 1,000 population. In 2010, Norway had approximately 300 ICU beds [3].
COVID-19 trends in Norway
The National Institute of Public Health started testing for COVID-19 on 23 January, registered the first incidence on 26 February and the first death caused by COVID-19 on 12 March 2020. The Norwegian National Institute of Public Health (NIPH) has overseen all data collection and measurements since COVID-19 was first listed as a notifiable disease in Norway on 31 January. By the 13 August NIPH has published 11 reports updating Covid-19 data. Municipalities are responsible for detecting, reporting and surveiling the spread of infectious diseases therefore, the Municipality Director of Public Health has local oversight over COVID-19 testing which is performed by a nasopharynx and throat test or by a blood test, and analysed using PCR-technology [4]. Initially testing took place in hospitals, but later special testing sites were established in municipalities, but all the samples were analysed in hospital laboratories and the results submitted electronically directly to the Norwegian Surveillance System for Communicable Diseases (MSIS) Laboratory database. There is little evidence of delays in access to tests or results.
The first nationally televised press conference was held by the government on 10 March 2020 and continued daily until 8 April. Thereafter, press conferences were held three times a week and from 15 June were only held when needed but at least once a week. The Prime-Minister, Health Minister and Head of the NIPH were all present initially, while later the panel included the Minister of Education and Integration and the Minister of Justice and Public Security. Links to streamed press conferences, written information and reports are available through government web sites with daily updates. While data is available at regional and county level, municipalities have been active in adopting a range of communications strategies in order to reach their citizens using daily press conferences, local newspapers, radio and twitter.
Plotting the course of COVID-19 in Norway
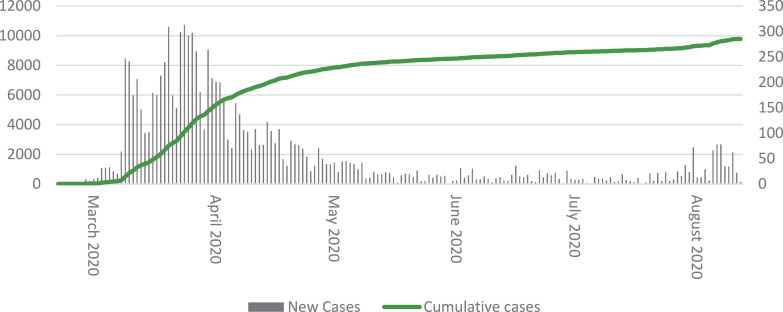
The NIPH monitors the evolution of COVID-19 and has published daily reports since 12 March on their website. As of 13 August, a total 518,893 (see Fig. 1 ) people have been tested [5].
Fig. 1.
Number of reported COVID-19 cases by date as of 13 August 2020.
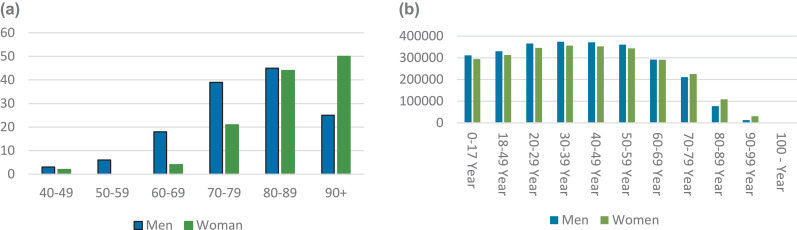
As of 13 August, 257 COVID-19 related deaths had been reported or 5.4 per 100,000 population [6]. The average age of death is 82 years. The peak of deaths associated with COVID-19 was the week of 6 April and includes those who died of and with COVID-19. In total, more men have died than women but due to the interaction between age and gender there have been more female than male deaths among 90+ (see Fig. 2 ) [6].
Fig. 2.
a: Deaths by age and gender compared to total Norwegian population by age and gender Fig. 2b.
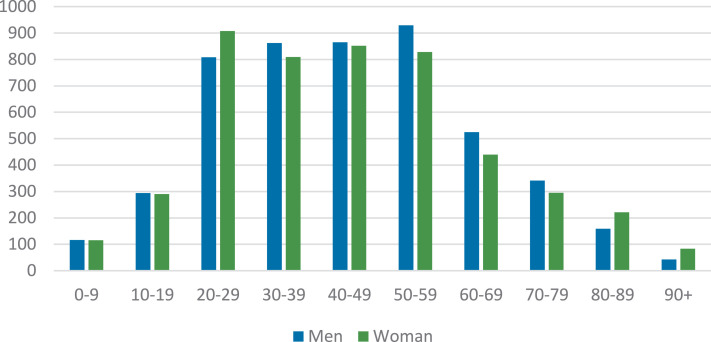
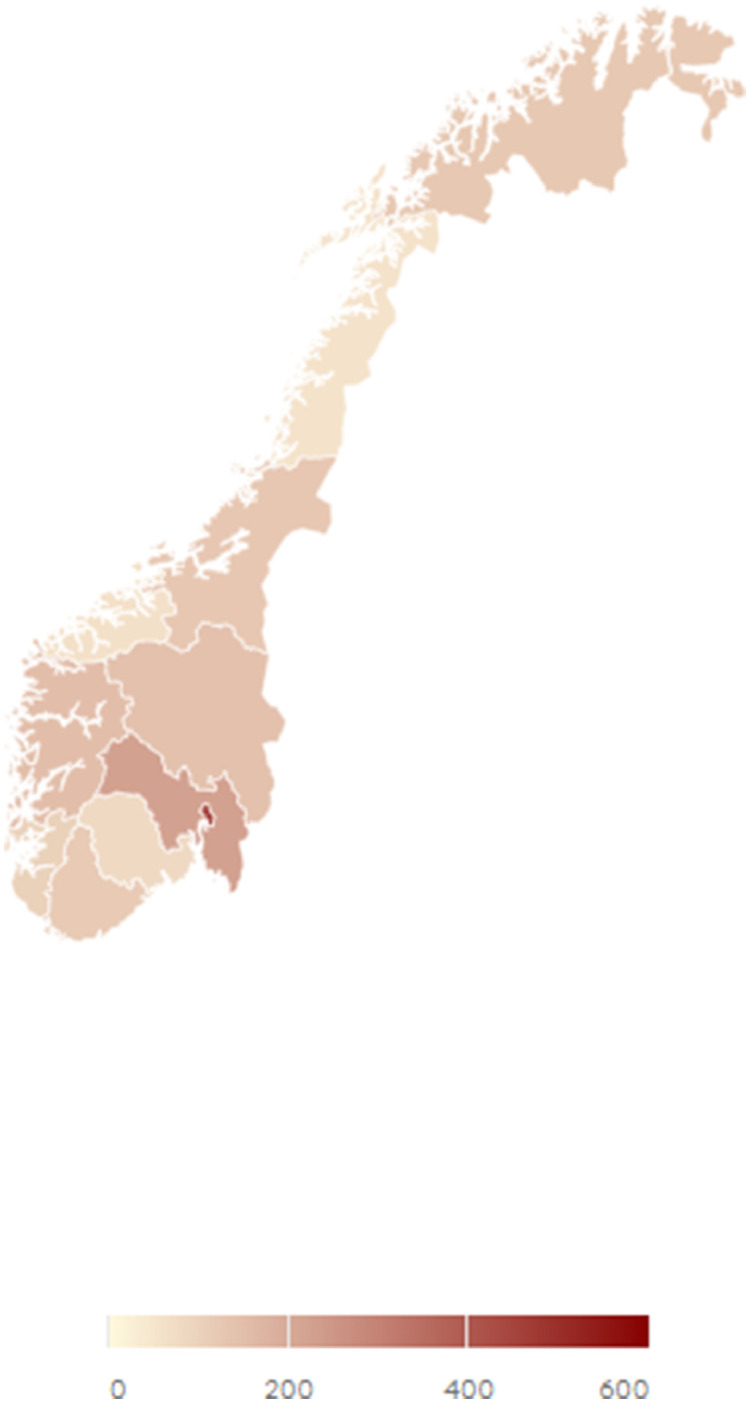
By 13 of August 9783 cases of COVID-19 had been reported and a total of 1233 patients admitted to hospital in Norway, 180 cases per 100,000 [6]. This figure grew from 8383 total cases by 29 April but exhibits little obvious gender pattern (See Fig. 3 ). With an average age of 59 the 230 patients admitted to ICU up to 13 August (4.3 per 100,000 population) (See Fig. 4 ), were 75% male and 63% had at least one risk factor such as age, obesity (BMI >30), gender, comorbidity, ethnicity and low socioeconomic status [6]. There is no available data on length of hospital stay. According to the NIPH modelling published on 12 August the scenario based on an R=1.1 suggests a peak of Covid-19 patients in hospitals and patients in hospital needing ventilator treatment in April-May 2021; the current R value is 1 [7]. The first reported cases in Norway were among those who had travelled abroad while the first case without direct contact was reported on 9 March [6]. On 28 February two medical doctors were infected but there are no published statistics on the number of health care professionals with COVID-19. Oslo (the capital and largest city in Norway) has the highest level of infection (24,2 per 100,000 population), double the national average (10,4 per 100,000 population) [8] (see Fig. 5 ). Far higher rates of infection have been recorded among those not born in Norway. Between 13 July and 2 August 43% of all Covid-19 cases were associated with the immigrant population [6].
Fig. 3.
Number of confirmed COVID-19 cases by age and gender as of 13 August 2020.
Fig. 4.
New patients admitted to ICU by date as of 13 August 2020.
Fig. 5.
Confirmed COVID-19 cases country heatmap as of 13 August 2020.
Norwegian policy road map
On 12 March the Norwegian Government presented new policies intended to limit and delay the COVID-19 outbreak [9]. Regulations ranged from advice on avoiding infection through restrictions to travel and group meetings and enforced closure of restaurants, coffee shops and pubs if social distancing between customers was not maintained (See Table 1 ) [10]. Violations were punishable by fines or imprisonment for up to six months, but there have been very few cases of the authorities issuing fines.
Table 1.
Norwegian government COVID-19 policies (issued 12 March 2020).
| Government recommendations | |
|---|---|
| Hand hygiene and cough etiquette | Wash hands frequently and thoroughly Avoid shaking hands and hugging people you do not live with. Cough or sneeze into a paper tissue or the crook of your elbow. |
| Work from home | Home working should be used if possible |
| Public transport | Use of public transport should be avoided |
| Domestic travel | Limit leisure travel in Norway |
| Health institutions | No visits to members of vulnerable groups |
| Mandated by law with potential sanctions | |
| Stay at Home | People with respiratory tract infection symptoms must stay at home until at least 1 day after they feel completely well. |
| Home Quarantine | People who travelled abroad must quarantine in their home for 14 days from the day they returned to the country. Backdated to 27.02.2020. Exception for travel from Finland and Sweden. People who have been in close contact with someone with a confirmed case of COVID-19 must home quarantine for 14 days. Those in quarantine must remain at home and not attend school or work. They can go outside, carry out necessary shopping maintaining social distancing of at least 1 metre but not use public transport. People who live in the same household are not quarantined. |
| Home isolation | People with confirmed COVID-19 must be isolated at home or in a healthcare institution else. The isolation lasts until 3 days after you have recovered and at least 8 days after you became ill. They can go outside in private garden or balcony and should try to maintain social distance from others in their household; people in the same household are in quarantine. |
| Closure | Educational institutions (from Kindergarten to Higher Education) Exception: Open to children of key workers up to 10, and children with special needs Restaurants, bars, pubs and clubs. Exception: If they can serve food to customers maintaining social distancing of 1 metre. Fitness centres, swimming pools and waterparks. Hairdressers, tattoo and piercing parlours, massage studios, spas and beauty parlours. |
| Cancelled/postponed | All organised sports activities, competitions and cultural events. |
| International travel ban | Applies to healthcare professionals with patient contact. |
Another set of policies related to the economic impact of the COVID-19 pandemic and the consequences of the movement restrictions: a work furlough scheme and loan guarantees for businesses. On 13 March, the government announced a 20-day furlough scheme to be implemented on 20 March. Usually when an employee is made redundant, the employer is responsible for paying the first 15 days; for the employee, following a three-day stop in pay they can receive unemployment benefits from the state. The new furlough scheme reduced the period the employer was responsible to pay to two days, followed by an 18-day period where the state provided the payment; beyond the 20-day period an individual could apply for unemployment benefits. The notification period to the employee was cut from 14 to two days to support businesses that were shut down overnight. A further flexibility for employers was that employees could be furloughed part-time (up to 50%) and therefore could continue to be in contact with and contributing to their workplace. The intention was to support companies to rotate staff on furlough within a business to try to limit unemployment.
The Norwegian government response also relies heavily on loan guarantees to the private sector. Government loan guarantees for small and medium enterprises were announced on 15 March, presented to Parliament on the 20th and implemented on the 27th. This scheme was extended to all private firms including those with more than 250 employees on 2 April. On the 19th of March 6 billion NOK loan guarantees for the aviation industry were agreed including specific protection for particular domestic routes and abolition of the air-passenger tax from 1 January-31 October while airport taxes paid by the carriers were cancelled from 1 January-31 June.
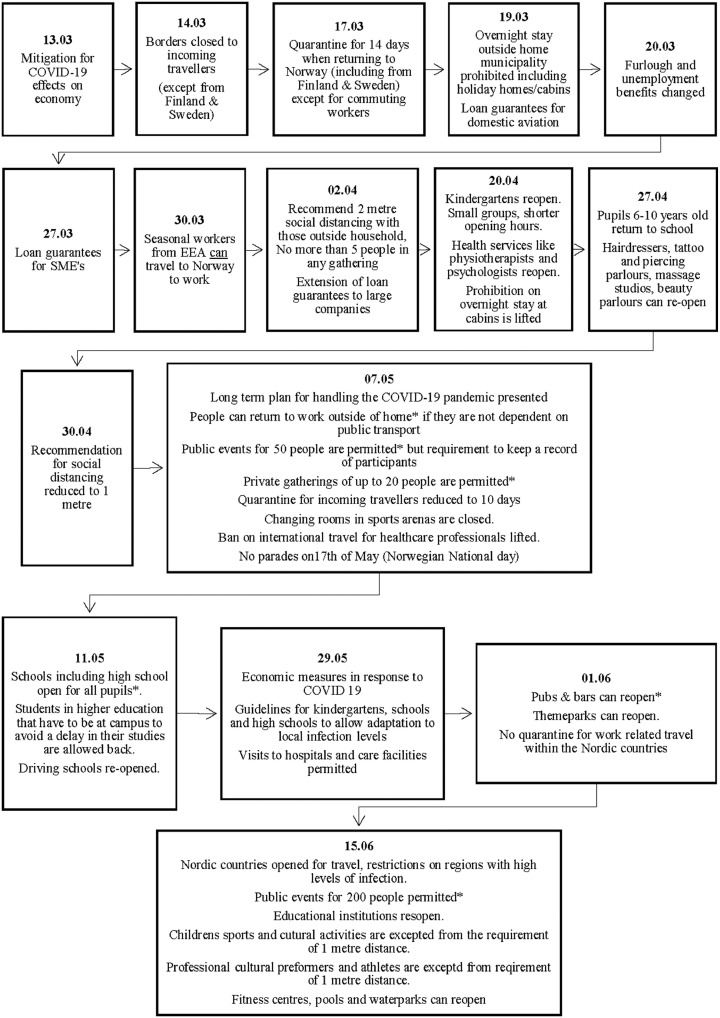
On 29 May the Government initiated a new policy phase, where movement control measures were scaled back, and economic measures were revised to increase economic activity and help the unemployed return to work. The new measures were; 1) a temporary subsidy scheme for companies to take back temporarily laid off workers, 2) measures to underpin activity in the construction sector, 3) a green transition package, 4) government purchase of air and train routes from private providers, 5) a compensation scheme for statutory maintenance expenses in seasonal businesses with severe income loss, 6) increased education funding and 7) measures to strengthen integration. Fig. 6 provides a diagram of the evolution of the full range of Norwegian COVID-19 policies.
Fig. 6.
The evolution of Norwegian COVID-19 policies.
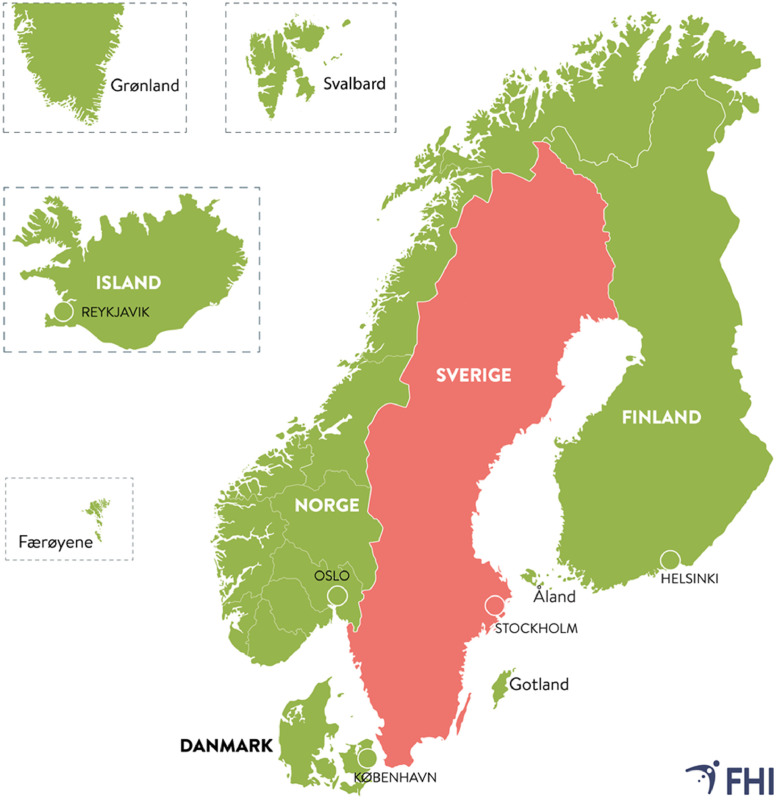
In the press conference on 7 May the government presented a plan to gradually open the national borders for travel, emphasising that it would be the development of the pandemic that would regulate which countries would be permitted access for travel. The first step was to be opening travel between the Nordic countries on 15 June. On 12 June a new system to communicate travel permitted without quarantine restrictions was launched. Travel access was based on a set of criteria and regions assessed as safe would be published every other week in the form of a map [11]. The first assessment resulted in opening borders to all the Nordic countries except Sweden. Initially travel to the island of Gotland, part of Sweden, without quarantine was permitted although on 15 June all of Sweden was excluded from quarantine free travel (see Fig. 7 ).
Fig. 7.
Regions opened for travel without requiring a quarantine period.
In a press conference on 10 July The Ministry of Foreign Affairs presented new regulations on travel permitting quarantine-free travel from 15 July for all countries within the Schengen area/EEA except for Portugal, Bosnia-Herzegovina, Croatia, Hungary, Bulgaria and Romania. Applying the same set of criteria as for the Nordic region, the government will continue, every other week, to assess any changes in the list of countries that can be visited without quarantine restrictions.
Initially the nationally provided information on COVID-19 was primarily about symptoms, the spread of the disease and prevention strategies. On 12 March, the government launched multiple strategies to contain the virus by closing national borders, schools and nurseries, prohibiting cultural and sports events and establishing national quarantine regulations. These responses were enshrined in a time-limited Corona Law on 18 March that extended the authority of the Prime Minister to act during the crisis.
From 14 March, there was a shift in the content and nature of the information disseminated focusing more on government responses to the economic consequences of the pandemic and quarantine regulations such as the work furlough scheme or the loss of seasonal agricultural workers. Increasingly, the social consequences of the situation have become the focus of government communication and the political discourse underpinning the policy response; loneliness, isolation, insecurity and the impact on young people and the delays in processing welfare claims and especially those associated with unemployment and the furlough scheme.
Alongside the evolution of policy there were also changes in COVID-19 testing criteria (See Table 2 ) [12]. Due to the low levels of COVID-19 virus in Norway large-scale population testing was never recommended by the NIPH. Until 25 May, people who were asymptomatic were not tested as a negative result might not indicate that an individual is in the incubation period, and therefore might give a false sense of security. Testing with nasopharyngeal or oropharyngeal swabs requires trained personnel and close contact between the person being tested and health personnel, this is resource intensive and risks further spreading the disease. Therefore, from 15 June the Norwegian Health Directorate together with Oslo municipality piloted a test using self-collected saliva samples. This non-invasive test requires minimal equipment and no close contact between test subject and the health personnel [13]. Municipalities were informed on 9 August that from 12 August testing should be available to any person with suspected infection without requiring a physician referral. Some municipalities provide drop-in services for testing, while others require a booked appointment.
Table 2.
COVID-19 testing criteria and prioritization by date of implementation.
| Date implemented | Priority | Testing where there is suspect COVID-19 |
|---|---|---|
| 8 February | 1 | Patients in need of hospital admission |
| 2 | Patients/residents of nursing homes or healthcare facilities | |
| 3 | Patient-facing healthcare professionals | |
| 4 | At risk population: 65+, serious or poorly managed long-term conditions | |
| 5 | Individuals quarantined due to close contact with a confirmed case of COVID-19 or after international travel | |
| 20 April | 6 | Employee, child or pupil in a re-opened childcare centre, school or after-school programme |
| 24 April | Post-mortem tests where there is suspicion of COVID-19 | |
| 7 May | 7 | Others with suspected COVID-19 disease Those on priority 6-7 tested after home monitoring of symptoms for 2 days |
| 25 May | 8 | Nursing home residents who are asymptomatic |
| 10 June | All those with suspected COVID-19 should be tested. |
Norwegian health care system response
Norway has 250 ICU beds, and 500 beds that can be upgraded to critical care [14]. Current modelling suggests that the peak of the epidemic will occur between May and October potentially requiring 600-1200 ICU beds [14]. Hospitals were given authority to cancel planned activity and reallocate beds to increase the number of ICU beds, this has led to a significant increase in waiting lists. There has been very little attention to the response to COVID-19 from primary care. There has been little public or government discussion, apart from restrictions on home visits and no reallocation of work or staff.
Providing critical care requires specially trained health care professionals, especially nurses. Many hospitals created digital education on infection control and for health care professionals who were not in daily practice in order to reallocate nurses from other wards to ICU [15]. Nursing students in their final year of an undergraduate degree were permitted to apply for temporary authorization to work in hospitals to increase the size of the health workforce; this was parallel to the existing opportunity available to final year medical students [16].
Effective infection control requires personal protection equipment such as facemasks, gloves and face shields. Many hospitals and health care facilities had very little infection control equipment at the beginning of March, orders and distribution of such equipment was then centralised to prioritize institutions with the greatest need [17]. Municipal health care facilities (primarily residential elderly care) and home care services, and general practitioners had to submit their orders though a national contact point along with hospitals [18]. Private initiatives to assist in producing facemasks and shields were encouraged to increase the available supply of PPE for use in health care facilities.
Even though the government prioritized the transport of food, supplies and pharmaceuticals, many people living with long-term conditions feared for their own health. Because of limited supplies and to combat hoarding the availability of seven pharmaceuticals was restricted: oxazepam (Xanax), insulin, metformin, Azitromcin (antiboticum), prednisolon, plaquentil and Paracetamol [19].
Norway is part of an international collaboration for the development of vaccines (The Coalition of Epidemic preparedness innovations) that started work developing a vaccine against COVID-19 in January. Norway has donated NOK36 million to develop the vaccines [20].
Health technology response
Norway's technology response was primarily focussed and track and trace. In part this is due to the existing highly developed electronic records system in Norway and the technology that underpins the centralised health information system. The “Smittestopp” app was released on 16 April. The app collects anonymised data about movement patterns as well as notifies users if they have been in close contact with a person that later is confirmed as infected with COVID-19. This requires that those who are infected also download and register with the app. By 19 March more than 1.5 million people had downloaded the app [21]. An expert committee assessed the technology and concluded that it requires further development as it stored too much personal information [22]. On 12 June the Norwegian Data Protection Authority warned the government that continuing to collect data that was not being analysed due to the extremely low numbers of infections contravened the law. In response, on 15 June, the NIPH announced that all data collection was being stopped, data already collected would be deleted and advising members of the public to deactivate the app.
The key role of municipalities in detecting, reporting and surveiling the spread of the pandemic prompted digital solution to making the relevant data available to inform policy at both national and regional levels. The NIPH collaborated with The Norwegian Association of Local and Regional Authorities (KS) and selected the District Health Information Software 2 (DHIS2). A mobile phone application that permits offline data capture DHIS2 is an open source, web-based health management information system platform, that makes it possible to generate analyses from data in real time [23]. Previously the software was used by low and middle income countries to track infection disease but in collaboration with the WHO a group led by the University of Oslo developed a module specifically for the COVID-19 pandemic [24]. All municipalities were given access to the Norwegian version through a national web page on 5 June.
Economic and financial fluctuation
Norway, like so many other countries has faced the challenge of the loss of revenues due to the dramatic decline of the economy as well as the cost of delivering increased levels of health services and schemes to support employers and employees. However, Norway has also faced a significant decline in the oil price that creates a direct challenge to the national budget from petroleum and tax revenues and an indirect challenge related to the contraction of a significant industrial sector. Table 3 summarizes the estimated costs of the policies put in place to support the economy [25]. Overall, it is estimated that tax revenues will decline by NOK59.4bn while the government budget balance is expected to weaken by NOK245.4bn.
Table 3.
Estimated costs of economic stimulus measures (NOK billions) (as of 8 June 2020).
| Mitigate income loss for businesses including compensation for large losses | 74.1 |
| Aviation sector loss provision and guarantee scheme | 14.1 |
| Government guaranteed loans to businesses through the banking system | 10.0 |
| Counteract loss of income for individuals | 27.3 |
| Strengthening critical infrastructure sectors | 23.3 |
| Other compensation schemes | 7.2 |
| Other measures | 6.1 |
| Increased spending on unemployment benefits | 23.9 |
| Total | 186.0 |
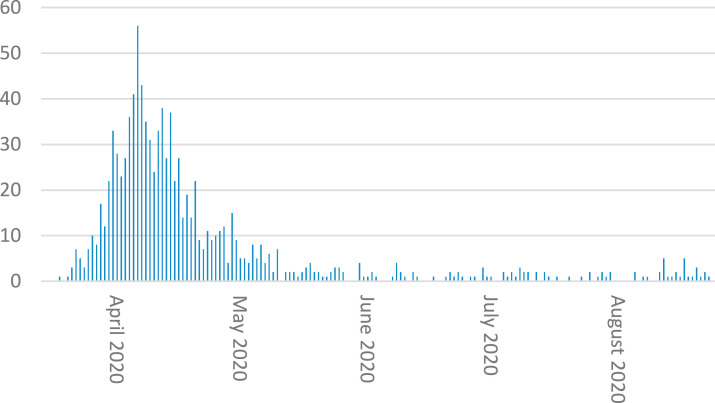
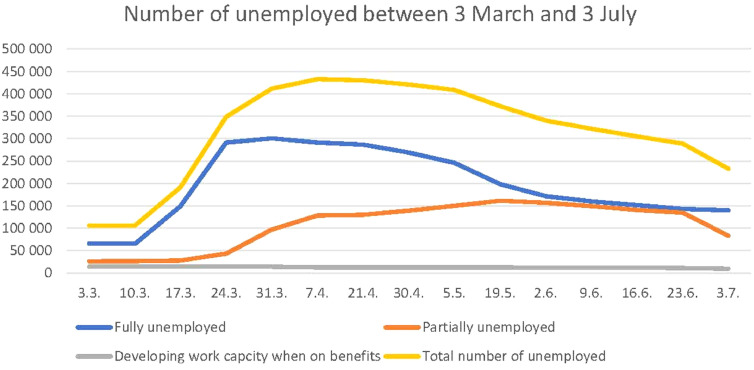
In part, these costs are due to the significant increase in levels of unemployment which has doubled since the outbreak of COVID-19 and as of 3 July 232,734 individuals were fully unemployed [26]. This is apparent in Fig. 8 as following the expansion of the furlough scheme on 24 March the number of fully unemployed declined while those in partial unemployment (including those on the furlough scheme) increased. Despite these interventions the number of fully unemployed remains more than double the number at the beginning of March 2020 and the seasonally adjusted unemployment rate (average from April-June) is 4.6%.
Fig. 8.
Number of unemployed by type of unemployment 3 March - 5 May.
In response to the significant costs incurred by policies and the drop in oil revenues on 12 May the Government proposed a revised state budget for 2020. The new budget entails the use of NOK382bn (€34.6bn) from the Sovereign Wealth fund rather than the planned NOK3.9bn inflow to the fund. The revised budget includes the structural oil-corrected budget deficit, or the amount of petroleum revenue included in the budget has increased to NOK419.6bn from the NOK243.6bn announced in the October budget [27]. The revised budget was considered by parliament on 19 June.
There has also been a significant impact on the Norwegian economic and financial context due to the COVID-19 pandemic (see Fig. 9 ). The Norwegian stock market, OSEAX fell by more than 34% but has rallied in line with other international financial markets but remains 10% below the level at the beginning of 2020. Norwegian currency markets have also been affected, the rate against the US$ dropped by 26% to a historic low on 22 March and remains 3% below the start of the year. Against the Euro the pattern is similar with the Norwegian Krona weakening over the course of the pandemic reaching a low point on 22 March before rallying but remaining almost 7% below the first of January level. In response the Norwegian central bank, Norges Bank, is “Continuously considering whether there is a need to intervene in the market by purchasing Norwegian Kroner” [28]. This has been followed by the central bank cutting interest rates to a record low of zero and forecast that they would remain there until at least 2023. The 0.25% cut was part of a 1.5% cut over the period since March [29].
Fig. 9.
Financial market reaction to major policy events in Norway (in percentage change from 1 January 2020).
The oil and gas industry is central to the Norwegian economy and the oil price crash continues to have a significant impact. Norway produces 2% of the world's oil supply but on 29 April the Oil and Energy Minister, Tina Bru, announced that Norway would cut oil production by 13% in June; the first cut in production for 18 years. Norway's state-owned operator Equinor announced capital expenditure and exploration cuts as part of its £3 billion COVID-19 action plan, the suspension of a share buyback program, and set up a department with the aim of preserving production and the jobs it supports in the North Sea [30].
Conclusions and policy implications
Norway acted quickly to stem the spread of the virus domestically, and limit infection from abroad while increasing health service capacity. The policy emphasis quickly shifted to concerns about economic impacts, the need to buttress both employers and employees and support specific industries such as domestic air travel. Most recently, concerns about the social cost of the implementation of the lock down procedures and the need to mitigate the consequences has shaped policies relating to the easing of lock down procedures. This attention to the social aspects, and the ability to fund these, we believe, is a key differentiator of the Norwegian response. As the Norwegian Prime Minister, Erna Solberg, reflected, “The government has chosen to prioritise children, then working life, and finally other activities.” [31].
Services for vulnerable children and youth were considerably reduced during the first stage of fighting the pandemic. Most of the low threshold services for children and young people where closed due to social distancing and many of the social care workers in these services were reallocated to other parts of the health system. In addition, the rate of referrals to child welfare services declined dramatically, and collaboration across services was reported as more problematic [32]. Despite the decline in provision and formal demand a large-scale epidemiological investigation assessing the prevalence of depression and anxiety associated with COVID-19 mitigation strategies found a two to threefold increase in depressive and anxiety symptoms in individuals experiencing the restrictions [33]. A study of quality of life between 9 and 29 March showed that people were more concerned after the COVID-19 outbreak regulations were implemented. The groups expressing the greatest increase in level of concern were single people under the age of 45 and immigrants, followed by parents with children under the age of 17 [34]. This has implications for future health policies.
Older people and those with compromised immune systems or with long-term conditions have also been particularly affected by the regulations. For the families of many of these, being unable to visit, or finding that those they loved died alone has been a significant source of anxiety and further grief. To address this issue and relieve social stress, the government announced on 27 May that visits by family members to residential facilities and to attend births would be permitted.
The significant outbreak of COVID-19 cases among the immigrant population especially in Oslo was, at least in part related to the communication strategy that had been adopted. The response, the provision of information in a range of minority languages and engagement with community information as part of an engagement strategy generated significant success. This has forced a reflection by health authorities on the need to consider indirect processes of discrimination such as defining an immigrant community as ‘problematic’. As a consequence, health authorities now recognise the importance of engaging with such communities in a different way.
Despite these areas of concern, the Norwegian policy response to COVID-19 is considered a success nationally and internationally. While there is a low level of community infection relying on herd immunity has never been an aspect of the Norwegian strategy. As the Prime Minister explained on 7 May “up until now, the strategy has been to stop the spread of the virus. We are now transitioning to a control strategy. We have had the same aim all along, to ensure that the health services have the capacity to assist everyone that needs it, both patients in need of health care due to COVID-19 and patients that need health care due to other reasons and diseases.” It is unclear whether this policy will need to change in response to current modelling suggesting a second wave peaking in May 2021 [7].
Norway is a rich country, and the strength of the oil and gas industry over the last 20 years, generating the Sovereign Wealth fund, has provided a buffer to the economic consequences of the crisis. Indeed, the need to draw on these reserves may also reshape the government's orientation to the country's economic dependence on this industrial sector.
The 27 of February, the CEO of the Norwegian central bank, Yngve Slyngstad, argues that Norway needed to shift from “an oil-dependent nation to an oil fund nation” [35]. This echoed statements by Norge Bank governor, Oystein Olsen who in his annual speech stated, “If this transition to a less oil-dependent economy could happen gradually, I'm very optimistic. If you have a more abrupt changes in conditions or policies…that…would make the transition more challenging” [36]. Perhaps COVID-19 provides the impetus for this transition, a transition and a context that all, policymakers, business leaders and the population, feel is challenging. There will inevitably be shifts in health policy, to ensure greater sensitivity and responsiveness to immigrant populations, support for vulnerable young people and greater attention to the mental health consequences of isolation. But as telling will be the fallout both from the economic consequences, the impact on employment particularly amongst young people and the challenge to Swedish policy leadership across the Nordic countries. The Swedish response to COVID-19 has exposed a fracture in Nordic solidarity apparent in the continued closure of borders; a fracture that is likely to echo in other aspects of policy.
Author Statements
Funding
None.
Declaration of Competing Interest
None declared.
Ethical approval
Not required.
References
- 1.OECD/European observatory of health system and policies . OECD publishing; Paris: 2019. Norway country health profile 2019: state of health in the EU. [Google Scholar]
- 2.The world bank group. Population density. [Internet] 2020 [Cited 2020 14/06]. Available from:https://data.worldbank.org/indicator/EN.POP.DNST?end=2016&locations=IS-NO-DK-SE-FO&start=1996&view=chart.
- 3.Flaatten H., og Soreide E. Intensivmedisin i Norge. [Intensive medicine in Norway] Tidsskr Nor Laegeforen. 2010;130(2):166‐168. doi: 10.4045/tidsskr.08.0054. [DOI] [PubMed] [Google Scholar]
- 4.Legeforeningen. Informasjon til fastleger om koronavirus- Sars-CoV-2 [Information to GP about Sars-CoV-2] [Internet] Oslo; Legeforeningen, 2020 [cited 2020 14/06] Available from: https://www.legeforeningen.no/foreningsledd/fagmed/norsk-forening-for-allmennmedisin/nyheter2/informasjon-til-fastleger-om-koronavirus-sars-cov-2/.
- 5.Norwegian Institute of Public Health . Norwegian institute of public health; Oslo: 2020. News report. [Internet]https://www.fhi.no/nyheter/2020/farre-pasienter-legges-inn-i-intensivavdelingene [cited 2020 14/06]. Available from: [Google Scholar]
- 6.Norwegian institute of public health . Norwegian institute of public health; Oslo: 2020. Weekly report. [Internet]https://www.fhi.no/publ/2020/koronavirus-ukerapporter/ [cited 2020 14/06]. Available from: [Google Scholar]
- 7.Norwegian institute of public health . Norwegian institute of public health; Oslo: 2020. National corona report. [Internet]https://www.fhi.no/sv/smittsomme-sykdommer/corona/koronavirus-modellering/ [cited 2020 14/08] Available from: [Google Scholar]
- 8.Norwegian institute of public health . Norwegian institute of public health; Oslo: 2020. Report on risk and response. [Internet]https://www.fhi.no/contentassets/c9e459cd7cc24991810a0d28d7803bd0/notat-om-risiko-og-respons-2020-05-05.pdf) [cited 2020 14/06]. Available from: [Google Scholar]
- 9.Norwegian Government. Timeline: news from Norwegian ministries about the coronavirus disease COVID-19. [Internet] Oslo; Norwegian government, 2020 [cited 2020 14/06]. Available from: https://www.regjeringen.no/en/topics/koronavirus-covid-19/timeline-for-news-from-norwegian-ministries-about-the-coronavirus-disease-covid-19/id2692402/.
- 10.Office of the Prime Minister & Ministry of Health and Care Services. Omfattende tiltak for å bekjempe koronaviruset. [Comprehensive measures to fight the coronavirus] [Press release] 2020 March 12 [cited 2020 14/06] Available from: https://www.regjeringen.no/no/aktuelt/nye-tiltak/id2693327/.
- 11.Norwegian institute of public health. Advice for infection control related to travel and vacation. [Internet] Oslo; Norwegian institute of public health, 2020 [cited 2020 14/06]. Available from: https://www.fhi.no/nettpub/coronavirus/fakta/reiserad-knyttet-til-nytt-koronavirus-coronavirus/.
- 12.Norwegian institute of public health. Aktuelt fra MSIS under COVID-19-epidemien. [Relevant information from the notification system for infectious diseases under the COVID-19-pandemic] [Internet] Oslo; Norwegian Institute of public health, 2020 [cited 2020 14/06]. Available from:https://www.fhi.no/publ/2020/COVID-19-msis/.
- 13.Norwegian institute of public health. COVID19 Epidemic Saliva sample for testing SARS-CoV-2 infection – a rapid review. [Internet] Oslo; Norwegian institute of public health, 2020 [cited 2020 14/06]. ISBN (digital): 978-82-8406-093-4.
- 14.Norwegian health directorate, Intensivkapasitet i Norge. [The capacity of ICU in Norway] [Internet] Oslo; Norwegian health directorate, 2020 [cited 2020 14/06]. Available from: https://www.helsedirektoratet.no/nyheter/intensivkapasitet-i-i-norge.
- 15.Helse nord. [Internet]. Regional handlingsplan [Regional plan of action] Bodo; 2020 April [cited 2020 14/06]. Available from: https://helse-nord.no/Documents/Korona2020/Regional%20handlingsplan%20for%20koronapandemi%20med%20vedlegg/Regional%20handlingsplan%20for%20koronapandemi.pdf).
- 16.Norwegian Health Directorate. Vedtak om forskrift om lisens til helsefaglige studenter [Resolution on regulations regarding the license for health and medical students] [Internet] Oslo; Norwegian health directorate, 2020 [cited 2020 14/06]. Available from: https://www.helsedirektoratet.no/tema/beredskap-og-krisehandtering/koronavirus/anbefalinger-og-beslutninger/Informasjon%20til%20utdanningsinstitusjonene%20om%20lisens%20til%20helsefaglige%20studenter.pdf/_/attachment/inline/b92367c9-0300-4856-9423-dfadc8df2edb:0dc1540a7be90699172aa16d9a504b47662a51ef/Informasjon%20til%20utdanningsinstitusjonene%20om%20lisens%20til%2Aso0helsefaglige%20studenter.pdf.
- 17.Helse SorOst [Internet]. Smittevernutstyr [Personal Protective equipment], Oslo; 2020 April [cited 2020 14/06]. Available from: https://www.helse-sorost.no/nyheter/smittevernutstyr.
- 18.Norwegian health directorate. Anbefalinger og beslutninger. [Advice and decisions] [Internet] Oslo; Norwegian health directorate, 2020 [cited 2020 14/06]. Available from: https://www.helsedirektoratet.no/tema/beredskap-og-krisehandtering/koronavirus/anbefalinger-og-beslutninger.
- 19.Norwegian medicines agency. Parallelleksport, meldeplikt og rasjonering i forbindelse med COVID-19. [Parallel export, notification and rationing for Covid-19] [Internet] Oslo; Norwegian medicines agency, 2020 [cited 2020 14/06]. Available from: https://legemiddelverket.no/import-og-salg/import-og-grossistvirksomhet/parallelleksport-meldeplikt-og-rasjonering-i-forbindelse-med-COVID-19.
- 20.Norsk Rikskrinkastning. Det siste vi trenger nå er at enkelt land stikker av med vaksine mot korona. [The last thing we need now is for some countries to get rid of the corona vaccine] [Internet] 2020 [cited 2020 14/06]. Available from: https://www.nrk.no/norge/_-det-siste-vi-trenger-na-er-at-enkeltland-stikker-av-med-vaksine-mot-korona-1.14954228.
- 21.Norwegian institute of public health. Antall nedlastinger og antall brukere av Smittestopp. [The number of downloads and the number of users of Infection Stop] [Internet] Oslo; Norwegian institute of public health, 2020 [cited 2020 14/06]. Available from: https://www.fhi.no/sv/smittsomme-sykdommer/corona/nokkeltall-fra-smittestopp/.
- 22.Lilleng J., Lykkebø O.R., Borud B. Norwegian government; Oslo: May 2020. Endelig rapport for kildekodegjennomgang av løsning for digital smitesporing av koronavirus. [Final report for source code review of digital coronavirus infection detection approach]https://www.regjeringen.no/contentassets/88ec3360adae44a1a9635fd6c1a58fca/200520_rapport_ekspertgruppa_smittestopp.pdf [cited 2020 14/06]. Available from: [Google Scholar]
- 23.District Health information software 2 (DHIS2). COVID19 surveillance package released. [Internet] District health information software 2, 2020 [cited 2020 14/06]. Available from: https://www.dhis2.org/.
- 24.Norwegian institute of public health. Nytt digitalt verktøy skal gjøre smittesporingen enklere for kommunene. [A new digital tool to make tracking infection easier for the municipalities]. [Internet] Oslo; Norwegian institute of public health, 2020 [cited 2020 14/06]. Available from: https://www.fhi.no/nyheter/2020/nytt-digitalt-verktoy-skal-gjore-smittejakten-enklere-for-kommunene/.
- 25.Ministry of finance. Economic measures in Norway in response to covid-19. [Internet] Oslo; Ministry of finance, 2020 [cited 2020 14/06]. Available from: https://www.regjeringen.no/en/topics/the-economy/economic-policy/economic-measures-in-norway-in-response-to-covid-19/id2703484/.
- 26.NAV. Weekly information [Internet] Oslo; NAV, 2020 [cited 2020 14/06]. Available from: https://www.nav.no/no/nav-og-samfunn/statistikk/flere-statistikkomrader/relatert-informasjon/ukentlig-statistikk-over-arbeidsledige.
- 27.Ministry of finance. Prop.67 S Endringer i statsbudsjettet 2020 [Proposal to Parliament Changes in the budget 2020]. [Internet] Oslo; Ministry of finance, 2020 [cited 2020 14/06]. Available from: https://www.regjeringen.no/no/dokumenter/prop.-67-s-20192020/id2695373/.
- 28.Miles, R. Norway cuts rates to zero as economy faces twin shocks. London: The financial times. [Internet] 2020 [cited 2020 14/06]. Available from: https://www.ft.com/content/da37b5a3-ff17-4151-95fc-e1176d4e60c8.
- 29.Miles, R. Norway considers action to break ‘extraordinary’ Krone slide. London: The financial times. [Internet] 2020 [cited 2020 14/06]. Available from: https://www.ft.com/content/e2ef5144-69c9-11ea-800d-da70cff6e4d3.
- 30.Sheppard, D. Norway to cut oil production by 13%. London: The financial times. [Internet] 2020 [cited 2020 14/06]. Available from: https://www.ft.com/content/363b603e-8234-4a6b-9167-90371b7c4285.
- 31.Milne, R. Denmark and Norway announce further loosening of lockdown. London: The financial times. [Internet] 2020 [cited 2020 14/06]. Available from: https://www.ft.com/content/af754259-381d-45fd-9ae9-584d414f78d4.
- 32.The Norwegian directorate for children youth and family affairs. Utsatte barn og unges tjenestetilbud under COVID19 pandemien [Services for vulnerable children and youth during the COVID-19 Pandemic]. [Internet] Oslo; The Norwegian directorate for children youth and family affairs, 2020 [cited 2020 14/06]. Available from: https://www.regjeringen.no/contentassets/3f92f45f0b384e0da0b2d89a9f55b7b6/2020-04-20-statusrapport-nr-1-fra-koordineringsgruppe-til-bfd-revidert.pdf.
- 33.Ebrahimi, O. V., Hoffart, A., & Johnson, S. U.The mental health impact of non-pharmacological interventions aimed at impeding viral transmission during the COVID-19 pandemic in a general adult population and the factors associated with adherence to these mitigation strategies. 2020. Preprint. [cited 2020 14/06]. Available from: 10.31234/osf.io/kjzsp. [DOI]
- 34.Støren, K. S.Mer bekymring og mindre glede etter korona-tiltakene. [More concern and less joy following the corona interventions] 2020. Oslo; Statistics Norway. [cited 2020 14/06]. Available from: https://www.ssb.no/sosiale-forhold-og-kriminalitet/artikler-og-publikasjoner/mer-bekymring-og-mindre-glede-etter-korona-tiltakene.
- 35.Milne, R.SWF head says Norway now ‘an oil fund nation’. London: The financial times. [Internet] 2020 [cited 2020 14/06]. Available from: https://www.ft.com/content/64b553cc-593f-11ea-a528-dd0f971febbc.
- 36.Milne, R. Norway bank chief warns on politicizing wealth fund. London: The financial times. [Internet] 2020 [cited 2020 14/06]. Available from https://www.ft.com/content/311760de-4e66-11ea-95a0-43d18ec715f5.