Abstract
Background
There has been limited literature regarding the influence of hamstring autograft diameter on the outcome of anterior cruciate ligament (ACL) reconstruction in Asian population. This study was undertaken to investigate the failure rate after ACL reconstruction among Chinese patients treated with hamstring tendon autografts of different diameters. Our hypothesis was that an increase in hamstring tendon autograft diameter would reduce the risk of graft failure.
Methods
A retrospective review of 394 consecutive patients who underwent ACL reconstruction using quadrupled semitendinous and gracillis autografts from 2009 to 2018 at our centre was performed. Logistic regression analysis was used to determine the relationship between graft failure rate and predictor variables, including hamstring graft diameter, gender and age.
Results
Hamstring graft diameter of 8.0 mm or more was found to be associated with significant reduction of risk in graft failure rate (P = 0.001, Relative Risk 0.19). No significant association was found between graft failure rate and gender or age.
Conclusion
Hamstring graft diameter 8.0 mm or greater is associated with decreased graft failure rate and revision rate in our local Chinese population.
Keywords: Anterior cruciate ligament reconstruction, Arthroscopy, Knee, Hamstring tendon graft, Revision surgery
Introduction
Quadrupled hamstring tendon autograft has become a popular graft choice in anterior cruciate ligament (ACL) reconstruction because of its favourable biomechanical profile, the ease of harvest and positive clinical outcomes.1, 2, 3, 4 The quadrupled hamstring tendon autograft is obtained by harvesting the semitendinosus and the gracilis tendons at the pes anserinus and folding them over twice to create a four strand autograft.5 Biomechanical studies have shown that hamstring graft strength increases with increased graft diameter.6 In 2012, Magnussen et al.7 published the first clinical study comparing graft size and revision rates. It demonstrated that an increase in hamstring tendon graft size is associated with a lower revision rate. To our knowledge, despite several subsequent studies demonstrating similar findings, many of such data were derived from Caucasian patients and data from Asian patients were generally lacking in the literature. The objective of this study was to investigate the ACL reconstruction failure rate among Chinese patients treated with hamstring tendon autografts of different diameters. We hypothesized that an increase in hamstring tendon autograft diameter would reduce the risk of graft failure. In addition, we also expected the ideal graft diameter to prevent failure would be smaller than that of reported in western literature.8,9
Materials and methods
All electronic records of patients who underwent primary ACL reconstruction at our center from 2009 to 2018 were evaluated. Patients who were managed conservatively, ACL reconstructions with bone patella tendon bone grafts and multiligamentous injuries were excluded. Graft diameter, gender, pre-injury Tegner Score, age at primary surgery and whether the patient developed graft failure were documented. Graft failure was defined as symptomatic patients with positive anterior drawer and Lachmann test supported with either compatible MRI or arthroscopic findings.
All ACL reconstructions were performed by a single surgical team consisted of fellowship trained orthopaedic surgeons. Semitendinosus and gracilis tendons were harvested by standard open techniques through a longitudinal incision centered between the tibial tubercle and the posteromedial border of the tibia. All grafts were stripped of muscle and doubled to form a four strand graft. Intraoperative measurements of the fashioned quadrupled hamstring graft were performed using sizing tubes calibrated to 0.5 mm. The femoral tunnel was consistently drilled to be the same diameter as the prepared graft using transportal technique. Femoral fixation was achieved with an endobutton (ENDOBUTTON™, Smith & Nephew) in all cases, while all tibial fixations were achieved with resorbable interference screw (BIORCI, Smith & Nephew). A standard ACL postoperative rehabilitation protocol was used in all patients. The timing when patients returned to sport was individualized and was based on the assessments by orthopaedic surgeons and physiotherapist.
Statistical analysis was performed using SPSS (Version 26.0). The Mann-Whitney U test was used to compare graft size based on gender. A logistic regression model was employed to evaluate the correlation of patient age, gender, and graft size with the incidence of graft failure. P < 0.05 was defined as statistically significant.
Result
A total of 394 cases of primary anterior cruciate ligament reconstruction were included. The study population of 394 patients was 83% male (327 male and 67 female patients) and ranged in age from 13 to 55 years old (mean, 27.3 years; SD, 8.1 years). The mean pre-injury Tegner Activity Score was 6.2±0.8 (Range, 4–9). The mean graft diameter was 7.7 mm (range, 5.5–10 mm) (Table 1). There was significant difference in the mean graft size between male (7.8 mm) and female patients (7.3 mm) (P < 0.001).
Table 1.
Graft diameter by Gender.
| Graft diameter | Male patients | Female Patients | Total |
|---|---|---|---|
| 5.5 mm | 1 | 0 | 1 |
| 6 mm | 2 | 2 | 4 |
| 6.5 mm | 6 | 6 | 12 |
| 7 mm | 60 | 29 | 89 |
| 7.5 mm | 49 | 14 | 63 |
| 8 mm | 148 | 15 | 163 |
| 8.5 mm | 31 | 1 | 32 |
| 9 mm | 25 | 0 | 25 |
| 9.5 mm | 3 | 0 | 3 |
| 10 mm | 2 | 0 | 2 |
| Mean size | 7.8 | 7.3 | 7.7 |
Graft failure was noted in 20 patients (5.1%) and 14 of them underwent revision ACL reconstruction. Graft failures occurred at a mean of 23.2 months after surgery (range, 9–57 months), excluding 4 outliers in which the failure occurred more than 5 years postoperatively. No statistically significant difference was noted between the mean pre injury Tegner Activity Score of the patients with graft failure and those who didn’t (P = 0.14). The cause of ACL graft failure in our cohort was all traumatic re-rupture. None of our patients were found to have tunnel malposition from computed tomography scan or premature return to sports.
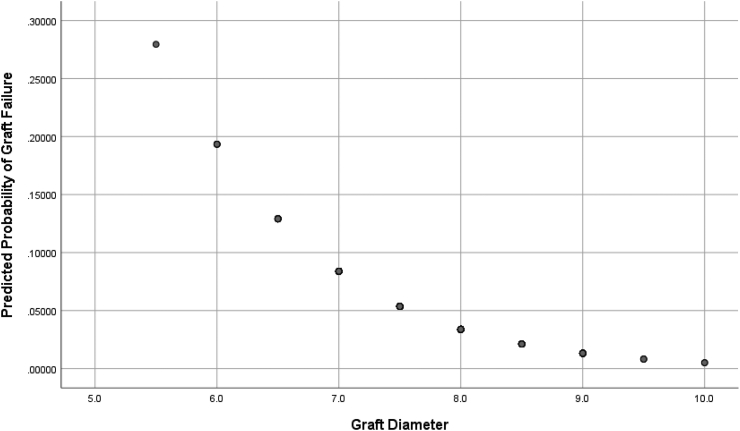
Logistic regression using forward selection with likelihood ratio test showed increased age (P = 0.10), increased graft diameter (P = 0.003) and the female subjects (P = 0.25) to be associated with reduced risk of failure. However only graft diameter was shown to be the significant factor (Fig. 1). Both the female gender and patient age were not noted to be an independent predictor of graft failure when graft diameter was taken into account.
Fig. 1.
Predicted Probability of Graft Failure by Graft diameter using Logistic Regression Analysis.
Graft failure was noted in none of the 30 patients with grafts greater than 8.5 mm in diameter, 4 out of 195 patients (2.1%) with 8.5- or 8-mm diameter grafts, and 16 of 169 patients (9.5%) with grafts 7.5 mm or less in diameter (Table 2). Graft failure was noted to occur at a significantly lower rate in grafts 8 mm or greater in diameter by Chi Square test (P = 0.001) with relative risk of 0.19.
Table 2.
Graft failure rate by Graft Diameter.
| Graft Diameter | Patient Age (Mean±SD) | No. of Patients | Graft failure | % failed |
|---|---|---|---|---|
| >9 mm | 25.4±8.4 | 5 | 0 | 0 |
| 9 mm | 26.7±6.9 | 25 | 0 | 0 |
| 8.5 mm | 25.6±6.5 | 32 | 0 | 0 |
| 8 mm | 27.6±7.8 | 163 | 4 | 2.5 |
| 7.5 mm | 27.8±9.6 | 63 | 9 | 14.3 |
| 7 mm | 26.9±7.4 | 89 | 6 | 6.7 |
| <7 mm | 28.4±12.0 | 17 | 1 | 5.9 |
| All | 27.3±8.1 | 394 | 20 | 5.2 |
Discussion
ACL reconstruction is one of the most commonly performed orthopaedic procoedures.10 Several options for graft choice are available and autologous single bundle hamstring graft is most commonly used.11 Although the results of ACL reconstruction have generally been favourable in restoring the knee stability, there is still a rate of 1.8%–10.4% of graft failure rate.12,13
In 1999, a biomechanical study conducted by Hamner et al. has shown that the strength of hamstring graft increased with increasing graft diameter.14 Later in 2012, Magnussen et al.7 found that grafts of 8 mm or less in diameter was associated with significant increase in the rate of revision ACL surgery. Mariscalco el al15 published their findings of the (MOON) cohort study and found that the revision rate was 0% if graft larger than 8.5 mm was used. In 2014 Conte el at published a systematic review showing that the relative risk of graft failure was 6.8 times greater when graft of less than 8.5 mm was used.16 The 8.5 mm cut-off was echoed by two further studies published more recently.17,18
It must be emphasized that the aforementioned studies were conducted in Europe and North America with predominant ethnic Caucasian patients. There is relatively little literature with regards to the optimal graft diameter for ACL reconstruction in Asian population. Inevitably, variability exists in the population in terms of hamstring size, and therefore the graft diameter. Recent studies have shown that a difference in the knee anthropometry may exists between Caucasians and Asians. Ho et al. published his findings on Singaporean patients showing that the median graft diameters for female and male patients were 7 mm and 8 mm respectively,19 while Xie et la revealed the median to be 7.5 mm.20 Therefore, based on the current available evidence, we did not know whether the graft diameter ‘cut-off’ of 8.5 mm could still be applied to our patients who are predominantly ethnic Chinese.
The purpose of this study was to firstly, investigate the relationship between graft failure rate and graft diameter among Chinese patients after ACL reconstruction with hamstring tendon autografts. And secondly, to see if the ‘cut-off’ point of 8.5 mm that are so commonly quoted in the European and American studies could be applied to our Chinese patients.
In our cohort of patients, we were able to demonstrate that an increase in hamstring graft diameter is associated with a reduced graft failure rate. When comparing to the European and American studies, we noted that a graft diameter of 8 mm could already reduce the risk of graft failure significantly. As in our study, Park et al.8 reported statistically significant difference in a Korean cohort when patients were classified as < 8.0 mm and ≥ 8.0 mm. The difference in results from western literature could be partly attributed by racial anthropometrical difference between the studied populations as the mean graft diameter of our cohort (Table 1) was smaller than that of reported from European and American counterparts.21
A number of studies reported that female gender to be a risk factor for graft failure.22,23 Several studies have also reported a higher graft failure rate in young and more active patients.7,24,25 However, only graft size was shown to be an independent predictor of graft failure in our logistic regression analysis. We noted in our series that 76% of female patients and 36% of male patients had graft at risk for failure based on size (<8 mm in diameter). This gender based difference in graft size may have act as a confounding variable in previous studies.
Many factors contribute to graft failure after ACL reconstruction. What we are able to describe in this study is that a smaller hamstring graft diameter is a contributor. And a graft diameter of 8 mm or larger is associated with a significant risk reduction in graft failure. The ‘cut-off’ for our Chinese patients is 8 mm. There are obviously other factors that have to be considered, including patient’s age (7,24, 25) and tunnel positioning.26, 27, 28 Therefore, larger graft size should not be the single ultimate goal of ACL reconstruction.
Different limitations can be attributed to this study. Firstly, it had a retrospective design with lack of randomization. These limitations may introduce bias into our data collection. Secondly, the review was done using the electronic record system of the Hospital Authority in Hong Kong. We might have missed those patients with post-ACL resonstruction graft failure who were not admitted to the Hospital Authority hospital system. However, we believed it is not a usual practice for patients with post-operative complications to seek help from doctors other than those who did the initial surgeries at our locality. And even if that is the case, it would be highly unlikely for the doctors performing the revision surgeries not to notify the initial operating surgeons.
It should be noted that one of the major limitation of our study is the lack of female representation within our sample population. Despite significant smaller graft size in our female subjects, a much lower graft failure rate was noted when compared to the male counterpart. This seemingly contradicting results could be due to the lack of statistical power as a result of relative small sample size of female subjects. Further large scale prospective study will be needed to assess the validity of our study.
Conclusion
Decreased hamstring autograft size is demonstrated to be a reliable predictor for graft failure and hence subsequent revision. In Chinese patients undergoing ACL reconstruction, the use of hamstring autograft 8.0 mm in diameter or more is associated with lower failure rate and revision rate. Based on the evidence presented, race could be another factor to be considered in predicting hamstring graft failure in ACL reconstruction.
Declaration of competing interest
The authors declares that there is no conflict of interest.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Lipscomb A.B., Johnston R.K., Snyder R.B., Warburton M.J., Gilbert P.P. Evaluation of hamstring muscle strength following use of semitendinosus and gracilis tendons to reconstruct the anterior cruciate ligament. Am J Sports Med. 1982;10:340–342. doi: 10.1177/036354658201000603. [DOI] [PubMed] [Google Scholar]
- 2.Otero A.L., Hutcheson L. A comparison of the doubled semitendinosus/gracilis and central third of the patellar tendon autografts in arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 1993;9:143–148. doi: 10.1016/s0749-8063(05)80363-9. [DOI] [PubMed] [Google Scholar]
- 3.Mott H.W. Semitendinosus anatomic reconstruction for cruciate ligament insufficiency. Clin Orthop. 1983;172:90–92. [PubMed] [Google Scholar]
- 4.Marder R.A., Rasking J.R., Carroll M. Prospective evaluation of arthroscopically assisted anterior cruciate ligament reconstruction, patellar tendon vs semitendinosus and gracilus tendons. Am J Sports Med. 1991;19(5):478–484. doi: 10.1177/036354659101900510. [DOI] [PubMed] [Google Scholar]
- 5.Pagnani M.J., Warner J.J., O’Brien S.J., Warren R.F. Anatomic considerations in harvesting the semitendinosus and gracilis tendons and a technique of harvest. Am J Sports Med. 1993;21:565–571. doi: 10.1177/036354659302100414. [DOI] [PubMed] [Google Scholar]
- 6.Hamner D.L., Brown C.H., Jr., Steiner M.E., Hecker A.T., Hayes W.C. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81:549–557. doi: 10.2106/00004623-199904000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Magnussen R.A., Lawrence J.T., West R.L., Toth A.P., Taylor D.C., Garrett W.E. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012 Apr;28(4):526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 8.Park S.Y., Oh H., Park S., Lee J.H., Lee S.H., Yoon K.H. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1111–1118. doi: 10.1007/s00167-012-2085-4. [DOI] [PubMed] [Google Scholar]
- 9.Chiang E.R., Ma H.L., Wang S.T., Hung S.C., Liu C.L., Chen T.H. Hamstring graft sizes differ between Chinese and Caucasians. Knee Surg Sports Traumatol Arthrosc. 2012 May;20(5):916–921. doi: 10.1007/s00167-011-1653-3. [DOI] [PubMed] [Google Scholar]
- 10.Mall N.A., Chalmers P.N., Moric M. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42:2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 11.Lee Y.H.D., Kuroda R., Chan K.M. Anterior cruciate ligament reconstruction: a 2015 global perspective of the magellan society. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2(4):122–128. doi: 10.1016/j.asmart.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wright R.W., Magnussen R.A., Dunn W.R., Spindler K.P. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93:1159–1165. doi: 10.2106/JBJS.J.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright R.W., Dunn W.R., Amendola A. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 14.Hamner D.L., Brown C.H., Jr., Steiner M.E., Hecker A.T., Hayes W.C. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81:549–557. doi: 10.2106/00004623-199904000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Mariscalco M.W., Flanigan D.C., Mitchell J. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013;29:1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conte E.J., Hyatt A.E., Gatt C.J., Jr., Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30(7):882–890. doi: 10.1016/j.arthro.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 17.Schlumberger M., schuster P., schulz M. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1535–1541. doi: 10.1007/s00167-015-3699-0. [DOI] [PubMed] [Google Scholar]
- 18.Snaebjörnsson T., Hamrin-Senorski E., Svantesson E. Graft diameter and graft type as predictors of anterior cruciate ligament revision: a cohort study including 18,425 patients from the Swedish and Norwegian national knee ligament registries. J Bone Joint Surg Am. 2019 Oct 16;101(20):1812–1820. doi: 10.2106/JBJS.18.01467. [DOI] [PubMed] [Google Scholar]
- 19.Ho S.W., Tan T.J., Lee K.T. Role of anthropometric data in the prediction of 4-stranded hamstring graft size in anterior cruciate ligament reconstruction. Acta Orthop Belg. 2016;82(1):72–77. [PubMed] [Google Scholar]
- 20.Xie G., Huangfu X., Zhao J. Prediction of the graft size of 4-stranded semitendinosus tendon and 4-stranded gracilis tendon for anterior cruciate ligament reconstruction: a Chinese Han patient study. Am J Sports Med. 2012;40(5):1161–1166. doi: 10.1177/0363546511435627. [DOI] [PubMed] [Google Scholar]
- 21.Tuman J.M., Diduch D.R., Rubino L.J., Baumfeld J.A., Nguyen H.S., Hart J.M. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35:1945–1949. doi: 10.1177/0363546507304667. [DOI] [PubMed] [Google Scholar]
- 22.Kim S.G., Kurosawa H., Sakuraba K. Analysis of the risk factors regarding anterior cruciate ligament reconstruction using multiple-looped semitendinosus tendon. Knee. 2005;12(5):366–369. doi: 10.1016/j.knee.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Noojin F.K., Barrett G.R., Hartzog C.W., Nash C.R. Clinical comparison of intraarticular anterior cruciate ligament reconstruction using autogenous semitendinosus and gracilis tendons in men versus women. Am J Sports Med. 2000;28(6):783–789. doi: 10.1177/03635465000280060301. [DOI] [PubMed] [Google Scholar]
- 24.Kamien P.M., Hydrick J.M., replogle W.H., Go L.T., Barrett G.R. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41:1808–1812. doi: 10.1177/0363546513493896. [DOI] [PubMed] [Google Scholar]
- 25.Marchand J.B., Ruiz N., Coupry A., Bowen M., Robert H. Do graft diameter or patient age influence the results of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2016;24:2998–3004. doi: 10.1007/s00167-015-3608-6. [DOI] [PubMed] [Google Scholar]
- 26.Simmons R., Howell S.M., Hull M.L. Effect of the angle of the femoral and tibial tunnels in the coronal plane and incremental excision of the posterior cruciate ligament on tension of an anterior cruciate ligament graft: an in vitro study. J Bone Joint Surg Am. 2003;85(6):1018–1029. doi: 10.2106/00004623-200306000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Rahr-Wagner L., Thillemann T.M., Pedersen A.B., Lind M.C. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy. 2013;29(1):98–105. doi: 10.1016/j.arthro.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 28.Zavras T.D., Race A., Amis A.A. The effect of femoral attachment location on anterior cruciate ligament reconstruction: graft tension patterns and restoration of normal anterior-posterior laxity patterns. Knee Surg Sports Traumatol Arthrosc. 2005;13(2):92–100. doi: 10.1007/s00167-004-0541-5. [DOI] [PubMed] [Google Scholar]