Abstract
Purpose
The aims of this study were to evaluate the reliability of three classifications of severity of dislocation in late-detected developmental dysplasia of the hip (DDH), especially to assess whether they are predictive of long-term outcomes.
Methods
Two groups of patients were analyzed. Group 1 (57 patients, 69 hips) underwent closed reduction between 1958 and 1962. Mean age at reduction was 20.3 months (4 to 65). Group 2 (50 patients, 54 hips) treated between 1996 and 2005, was used for analysis of the association between severity of dislocation and treatment (open or closed reduction). The primary radiographs were graded according to the Tönnis classification, the classification of the International Hip Dysplasia Institute and a new method based on the position of the most lateral point of the proximal femoral metaphysis (lateral metaphysis height classification, LMH). The outcome at a mean age of 51.2 years (55 to 60) was graded according to the occurrence of osteoarthritis (OA) and total hip arthroplasty (THA).
Results
There were significant associations between the classifications, and the intra- and interobserver agreements were high. More severe grades of DDH were significantly associated with age ≥ 18 months and with open reduction. None of the classifications were significantly associated with long-term OA. The LMH method was significantly associated with the need for THA, whereas the other classifications were not.
Conclusion
All the classifications were reliable in grading severity of DDH. The LMH method seems preferable in clinical practice because the main landmarks were easy to define and because it had long-term prognostic value.
Level of Evidence
III
Keywords: late-detected developmental dysplasia of the hip, severity of dislocation, radiographic classifications, prognostic value, long-term outcome
Introduction
The severity of dislocation in late-detected developmental dysplasia of the hip (DDH) varies from acetabular dysplasia alone to complete dislocation. Different classifications have been proposed to characterize the severity of displacement. Tönnis1 used the position of the ossific nucleus in relation to acetabular landmarks. Others used the position of the proximal femoral metaphysis related to the acetabulum.2,3 Because the Tönnis method cannot be used when the ossific nucleus of the femoral head has not appeared, a new classification was introduced by members of the International Hip Dysplasia Institute (IHDI) and was called the IHDI method.4 The authors found excellent inter-rater reliability and recommended the method for general use in classifying the severity of DDH. They also planned further studies aiming at evaluating the method for clinical decision-making and prognostication. The IHDI classification has been found to be significantly related to the type of primary treatment.5,6 One study reported that the Tönnis classification was of predictive value for treatment results,7 whereas another study reported no relation between Tönnis grading and radiographic results,8 but the follow-up time in both studies was limited (a mean of 4.1 years and 6.8 years, respectively). We have found no studies of the ability of radiographic classifications to predict long-term outcome.
This study evaluated three classifications of severity of late-detected DDH: the Tönnis classification, the IHDI classification and an additional method which we have named the lateral metaphysis height (LMH) classification. The main purpose was to evaluate the prognostic value of these classifications with approximately 50 years follow-up. Other aims were to evaluate the association of the classifications with patient age and to find the predictive ability with regard to type of primary treatment (open or closed reduction) and residual hip dysplasia/subluxation.
Patients and methods
Two groups of patients were studied. The patients in Group 1 were identified through a search of the diagnosis card index for patients who had been treated with preliminary traction and closed reduction for late-detected DDH during the period between 1958 and 1962. A total of 68 patients (83 hips) were identified but 11 patients (14 hips) were excluded because the primary radiographs were missing. The first available radiographs in these 11 patients had been taken with abducted hips during the first part of the traction period, which we thought would make the radiographic classifications uncertain. Thus, 57 patients (48 female)/69 hips, were included in the study. Their mean age at hip reduction was 20.3 months (4 to 65).
Since all the patients in Group 1 had been treated with closed reduction, another group (Group 2) was included for analysis of the association between severity grading and treatment (open or closed reduction). A total of 53 patients were treated for late-detected DDH in our hospital during the period between 1996 and 2005. Three patients were omitted, two because of no available primary radiographs and one because the first available radiograph had been taken in traction. Thus, Group 2 included 50 patients (48 female)/54 dislocated hips. Their mean age at reduction was 16.3 months (3 to 50). In all, 32 patients (34 hips) had undergone closed reduction and 18 patients (20 hips) had had open reduction. In four of the latter patients (five hips) with age above 3.0 years, open reduction was combined with Dega type pelvic osteotomy and/or proximal femoral osteotomy.
Radiographic evaluation
The primary anteroposterior radiographs were graded according to the Tönnis classification,1 the IHDI method4 and the LMH method.
Tönnis classification
This method is based on the relative position of the ossific nucleus of the femoral head (Fig. 1).1 In Tönnis grade I hips, the ossific nucleus is medial to a vertical line through the superior acetabular rim (Perkins’ line, P-line). In grade II hips the ossific nucleus is lateral to the P-line and below the superolateral margin of the acetabulum (SMA-line). In grade III hips the ossific nucleus is level with the SMA-line. In grade IV hips the ossific nucleus is located above the SMA-line.
Fig. 1.

The Tönnis classification is divided into four grades (I to IV) based on the position of the ossification centre of the femoral head according to Perkins’ line (P-line) and the superolateral margin of the acetabulum (SMA)-line (horizontal line through the SMA). The figure shows a hip with grade III dislocation.
IHDI classification
This method is based on the relative position of the proximal femoral metaphysis.4 The main landmark is the H-point (Fig. 2), which is defined as the midpoint of the superior margin of the ossified metaphysis. The H-point is described in relation to three lines: the P-line, the line through the top of the triradiate cartilages bilaterally (Hilgenreiner’s line, H-line) and the diagonal line (D-line), which is drawn 45° from the junction of the H-line and P-line. In grade I, the H-point is at or medial to P-line. In grade II the H-point is lateral to P-line and at or medial to the D-line. In grade III the H-point is lateral to D-line and at or inferior to H-line. In grade IV the H-point is superior to H-line.
Fig. 2.

The International Hip Dysplasia Institute classification is divided into four grades (I to IV) based on the position of the midpoint of the proximal femoral metaphysis (H-point), in relation to Perkins’ line (P-line), Hilgenreiner’s (H-line) and diagonal line. The figure shows a hip with grade III dislocation.
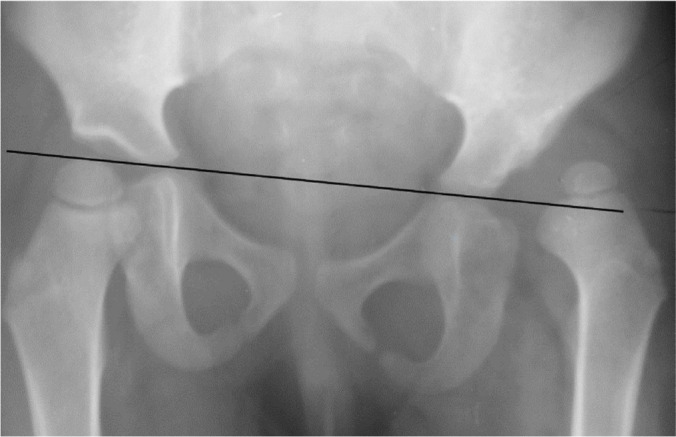
LMH classification
This method is a modification of the measurements described by Terjesen et al3 and is based on the position of the proximal femoral metaphysis in relation to P-line and H-line. Since distances and percentages were used in the original study,3 we made a simple grading system (LMH classification) for the present study (Fig. 3). In LMH grade I, one half or more of the proximal femoral metaphysis is medial to the P-line (as in the IHDI classification). In grade II more than half of the proximal femoral metaphysis is lateral to the P-line and the most lateral point of the metaphysis (which usually is the same as the most proximal point of the metaphysis) is inferior to H-line. In grade III the most lateral point of the metaphysis is at or superior to H-line.
Fig. 3.

The lateral metaphysis height classification is divided into three grades. Grades II and III are defined according to the position of the lateral margin of the metaphysis in relation to Hilgenreiner’s line (H-line). The figure shows a hip with grade III dislocation (P-line, Perkins’ line).
Evaluation of the classifications
The primary radiographs in Group 1 were used for evaluation of inter- and intraobserver agreements of the three classifications and for the associations between the classifications. Interobserver agreement was performed between the two authors (TT and JH) who independently assessed the initial radiograph for all the patients. Intraobserver agreement was performed by one of the authors (TT) who assessed the radiographs two times with a four-week interval. Group 1 was also used for assessing the ability of the classifications to predict residual hip dysplasia during childhood and adolescence and to predict the long-term outcome. Long-term follow-up included whether or not the hip had developed osteoarthritis (OA) and whether or not the hip had undergone total replacement at approximately 50 years follow-up. OA was defined according to Jacobsen and Sonne-Holm,9 using the minimum joint space width of the upper weight-bearing part of the joint. OA is present when the minimum joint space is < 2 mm.
The hips in Group 2 were used for evaluation of the ability of the classifications to predict the types of primary treatment: closed or open reduction. The LMH classification was performed prospectively by the first author (TT) using the primary radiographs in all the 54 hips before treatment was initiated. IHDI classification, which was done retrospectively, was available in 22 hips because the primary radiographs of the other patients were no longer available when this study was performed. The same applied to the Tönnis classification, which was available in only 17 hips (five hips could not be classified because they lacked an ossification centre of the femoral head).
Statistical analysis
SPSS (version 25) was used for the statistics (IBM, Armonk, New York). Categorical data were analyzed with the Pearson chi-squared test and with Kappa statistics. Continuous variables were analyzed using the t-test for independent samples and one-way analysis of variance with Sheffe’s post hoc test. Differences were considered significant when the p-value was < 0.05.
Results
The inter- and intraobserver agreements of the classifications were good, with interobserver kappa values from 0.75 (Tönnis method) to 0.80 (LMH method) and 0.81 (IHDI method) and intraobserver kappa values from 0.69 (Tönnis method) to 0.85 (IHDI method) and 0.88 (LMH method). In hips with interobserver disagreement, the final classification was made by the two authors, assessing the radiographs together. The final distribution of the 69 hips in Group 1 according to the IHDI method was grade I in one hip, grade II in 21 hips, grade III in 28 and grade IV in 19 hips, whereas the distribution according to the LMH classification was grade I in one hip, grade II in 34 hips and grade III in 34 hips (Table 1). Six hips (9%) could not be classified with the Tönnis method because the ossification centre of the femoral head had not appeared. The median age at reduction of these six hips was seven months. The distribution of the remaining 63 hips was grade I in one hip, grade II in 45 hips, grade III in 16 hips and grade IV in one hip. There was a good association between the three classifications (p < 0.001; Table 1). Only one of the hips with a moderate degree of dislocation (grade II) according to the IHDI and LMH classifications had severe dislocation (grade III) in the Tönnis classification.
Table 1.
Association between the three radiographic classifications of severity of dislocation in Group 1 (number of hips)
| Classification | IHDI grade | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | Total | ||||||
| Tönnis grade | ||||||||||
| I | 1 | 0 | 0 | 0 | 1 | |||||
| II | 0 | 18 | 23 | 4 | 45 | |||||
| III | 0 | 1 | 2 | 13 | 16 | |||||
| IV | 0 | 0 | 0 | 1 | 1 | |||||
| Total | 1 | 19 | 25 | 18 | 63* | |||||
| Tönnis grade | ||||||||||
| LMH grade | I | II | III | IV | Total | |||||
| I | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 |
| II | 0 | 21 | 13 | 0 | 34 | 0 | 29 | 1 | 0 | 30 |
| III | 0 | 0 | 15 | 19 | 34 | 0 | 16 | 15 | 1 | 32 |
| Total | 1 | 21 | 28 | 19 | 69 | 1 | 45 | 16 | 1 | 63* |
the Tönnis classification could not be used in six hips because the ossification centre of the femoral head had not appeared
IHDI, International Hip Dysplasia Institute; LMH, lateral metaphysis height classification
In Group 1, the mean age at reduction in IHDI grades II, III and IV were 18.9 months, 18.3 months, and 24.4 months, respectively (p = 0.173). According to the LMH classification, the mean age was significantly lower in grade II compared with grade III (16.9 months versus 23.4 months; p = 0.013). The association between dislocation severity and age at reduction (< 18 months versus ≥ 18 months) is shown in Table 2. Age ≥ 18 months was significantly associated with more severe dislocation in all the classifications.
Table 2.
Association between radiographic classifications and age (< 18 months versus ≥ 18 months) in Group 1, given as number of hips
| Age at reduction | |||
|---|---|---|---|
| Radiographic grading | < 18 mths | ≥ 18 mths | p-value* |
| IHDI | |||
| I | 0 | 1 | 0.003 |
| II | 12 | 9 | - |
| III | 14 | 14 | - |
| IV | 1 | 18 | - |
| LMH | |||
| I | 0 | 1 | 0.004 |
| II | 20 | 14 | - |
| III | 7 | 27 | - |
| Tönnis | |||
| I | 0 | 1 | 0.022 |
| II | 21 | 24 | - |
| III | 1 | 15 | - |
| IV | 0 | 1 | - |
IHDI, International Hip Dysplasia Institute classification; LMH, lateral metaphysis height classification
Pearson’s chi-square test.
Patient Group 2 was used to test the ability of the classifications to predict the type of primary treatment (Table 3). All the classifications had significant associations with the type of treatment (closed or open reduction). Using the LMH classification, which was available in all the 54 hips, there was a marked difference between grade II dislocations with only four open reductions in 32 hips and grade III dislocations with 16 open reductions in 22 hips.
Table 3.
Association between radiographic classifications and primary treatment in Group 2 (closed or open reduction), given as number of hips
| Primary treatment | |||
|---|---|---|---|
| Radiographic grading | Closed reduction | Open reduction | p-value* |
| IHDI | |||
| II | 4 | 0 | 0.004 |
| III | 8 | 4 | - |
| IV | 0 | 6 | - |
| LMH | |||
| II | 28 | 4 | < 0.001 |
| III | 6 | 16 | - |
| Tönnis | |||
| II | 10 | 2 | 0.034 |
| III | 1 | 2 | - |
| IV | 0 | 2 | - |
IHDI, International Hip Dysplasia Institute classification; LMH, lateral metaphysis height classification
Pearson’s chi-square test.
Group 1 was used to analyze the relationship between the radiographic classifications and residual hip dysplasia, defined as additional surgery to correct hip dysplasia/subluxation during childhood and adolescence or centre-edge angle < 20° at skeletal maturity.10 The LMH classification was significantly associated with residual dysplasia/subluxation (p = 0.034), whereas the IHDI classification showed the same trend, but the association was not statistically significant (Table 4).
Table 4.
Association between radiographic classifications and residual hip dysplasia/subluxation during childhood in Group 1, given as number of hips
| Residual hip dysplasia | |||
|---|---|---|---|
| Radiographic grading | No | Yes | p-value* |
| IHDI | |||
| I | 1 | 0 | 0.135 |
| II | 16 | 5 | - |
| III | 16 | 12 | - |
| IV | 8 | 11 | - |
| LMH | |||
| I | 1 | 0 | 0.034 |
| II | 25 | 9 | - |
| III | 15 | 19 | - |
| Tönnis | |||
| I | 1 | 0 | 0.325 |
| II | 29 | 16 | - |
| III | 7 | 9 | - |
| IV | 1 | 0 | - |
IHDI, International Hip Dysplasia Institute classification; LMH, lateral metaphysis height
Pearson’s chi-square test.
The long-term outcome of the hips in Group 1 (Figs 4 and 5), at a mean patient age of 51.2 years (44 to 57), was graded according to the occurrence of OA and total hip arthroplasty (THA). Information about THA was provided from the Norwegian Arthroplasty Registry. OA had developed in 30 of the 69 hips (43%) and 24 hips (35%) had undergone THA. None of the radiographic classifications were significantly associated with the occurrence of OA (Table 5). The LMH method was significantly associated with THA (p = 0.030) whereas the other two methods were not.
Fig. 4.
a) Initial radiograph showing dislocation of the left hip in a girl 18 months of age. The Hilgenreiner’s line, Perkins’ line, diagonal line and line through the superolateral margin of the acetabulum are indicated, and so are the H-point (midpoint) and the most lateral point of the proximal femoral metaphysis. The severity of dislocation is grade II according to the Tönnis and the lateral metaphysis height classifications and grade III according to the International Hip Dysplasia Institute classification; b) radiograph of the same patient at an age of 51 years, showing good outcome without osteoarthritis.
Fig. 5.
a) Radiograph showing dislocation of the left hip in a girl 28 months of age. The Hilgenreiner’s line and the superolateral margin of the acetabulum line are indicated. The severity was classified as grade III according to the Tönnis and lateral metaphysis height classifications and grade IV according to the International Hip Dysplasia Institute method; b) radiograph of the same patient showing poor long-term outcome. Total hip arthroplasty was performed at a patient age of 34 years.
Table 5.
Association between long-term outcome at a mean age of 50 years in Group 1, given as the number of hips according to osteoarthritis and total hip arthroplasty (THA)
| Osteoarthritis | THA | |||||
|---|---|---|---|---|---|---|
| Radiographic grading | No | Yes | p-value* | No | Yes | p-value* |
| IHDI | ||||||
| I | 1 | 0 | 0.827 | 1 | 0 | 0.503 |
| II | 12 | 9 | - | 16 | 5 | - |
| III | 16 | 12 | - | 17 | 11 | - |
| IV | 10 | 9 | - | 11 | 8 | - |
| LMH | ||||||
| I | 1 | 0 | 0.231 | 1 | 0 | 0.030 |
| II | 22 | 12 | 27 | 7 | - | |
| III | 16 | 18 | 17 | 17 | - | |
| Tönnis | ||||||
| I | 1 | 0 | 0.459 | 1 | 0 | 0.643 |
| II | 26 | 19 | 30 | 15 | - | |
| III | 7 | 9 | 9 | 7 | - | |
| IV | 1 | 0 | 1 | 0 | - |
IHDI, International Hip Dysplasia Institute classification; LMH, lateral metaphysis height classification; Tönnis, the Tönnis classification
Pearson’s chi-square test.
Discussion
Classifications of the severity of late-detected DDH are desirable for several reasons. First, a classification is useful to monitor changes of severity over time. The frequency of the most severe dislocation grade according to the LMH classification was 49% in Group 1 and 41% in Group 2 and thus had changed little over the 40-year period. Secondly, a classification is required for comparison of severity of dislocation in different studies.
An appropriate classification system should satisfy certain requirements. It should not be too complicated, and the landmarks should be clearly and easily identified. Further, good intra- and interobserver agreement is necessary. The classifications that were examined in this study met some of these demands. There were good intra- and interobserver agreements in all the classifications, supporting previous studies of the Tönnis and IHDI classifications.4,5,11,12 There were also statistically significant associations between the three classifications.
Classifications should be clinically relevant in the sense that they should be useful for decision-making regarding types of primary treatment (open and closed reduction) and for prognostication of long-term outcome. Both the Tönnis and the IHDI classifications have been reported to have predictive ability regarding type of primary treatment.5,6,11,13,14 The present results confirmed the ability of these two classifications to predict open or closed reduction, and the same predictive ability was found using the LMH method. Open reduction was performed in all the six IHDI grade IV hips and in 73% of the LMH grade III hips, indicating that open reduction is usually the treatment of choice in the most severely displaced hips.
We have found no data on the association between the IHDI grades and patient age at hip reduction in previous studies.4,11 Not unexpectedly, this study found that the severity of dislocation in all the classifications increased with patient age ≥ 18 months compared with the severity in younger children. This relationship supports the importance of early detection of DDH, when treatment is easier and the results are better.
The association between severity of dislocation, assessed by the Tönnis and IHDI classifications, and the need of late pelvic osteotomy to correct residual hip dysplasia/subluxation was studied in hips with at least four years of follow-up by Ramo et al.5 Both classifications had the ability to predict late pelvic osteotomies. In the present study, only the LMH method had a significant ability to predict residual dysplasia. More severe dislocation grade predicted increased risk of residual dysplasia/subluxation. A similar trend, although not statistically significant, occurred with the other two methods, indicating a type-2 statistical error.
According to Narayanan et al,4 a future goal of the IHDI was to establish the ability of their classification for the purpose of prognostication. This ability was evaluated for all the three classifications in the present study. The prognostic ability was limited, since there was no statistically significant association between the classifications and long-term OA. This could be due to other variables with influence on treatment outcome: age of the patient, type of reduction, and later additional surgery such as pelvic and femoral osteotomies. However, the LMH method had a significant ability to predict the necessity of THA, which had been inserted in 20% of hips with grade I/II dislocation and half the hips with the most severe grade of dislocation.
Although good intra- and interobserver agreement, a problem with all the classifications is the correct identification of the anatomical landmarks. Narayanan et al4 pointed out that the greatest variability could occur in identifying the SMA. In a severely dislocated hip, the bony SMA is often resorbed, and there is no sharp distinction between the acetabular roof and the lateral ilium proximal to the hip joint (Fig. 6). In such hips it is difficult and probably unreliable to use the Tönnis classification, because the distinction between grades II, III and IV is entirely dependent on a correct location of the SMA. The P-line is also dependent on the location of the SMA, which may lead to unreliable distinction between grades II and III of the IHDI classification. Surprisingly enough, this problem was not addressed in previous studies.4,11 The LMH method does not have this problem because the SMA is not used as a landmark for grading severity of dislocation. Since Hilgenreiner’s line is usually easy to identify, the distinction between grades II and III in the LMH classification and grades III and grade IV in the IHDI classification is quite reliable. All the three methods use Perkins’ line to distinguish between grade I and grade II. This is usually no big problem since SMA is easier to identify in normal hips and hips with slight dislocation.
Fig. 6.
Radiograph showing dislocation of the left hip in a girl 32 months of age. Hilgenreiner’s line is indicated. Perkins’ line and superolateral margin of the acetabulum line are difficult to define because of bone absorption of the lateral acetabular rim. The severity was classified as International Hip Dysplasia Institute grade IV, lateral metaphysis height grade III and Tönnis grade III.
There are some limitations of the present study. First, there were few hips with Tönnis grade IV dislocation, which made the study less relevant for hips with the most severe grade of dislocation. Secondly, the long-term outcome was analyzed after one type of treatment only (closed reduction) and might, therefore, not be valid for hips treated with open reduction. The strength of the study was that all the patients were available for the long-term follow-up.
What are the clinical implications of this study? All the classifications had adequate interobserver agreement, were significantly associated with patient age and were predictive for the choice of open or closed reduction. The Tönnis method has an obvious weakness, since it is not possible to use in hips without an ossification centre of the femoral head. Moreover, this classification and the IHDI method are based on the location of the lateral acetabular rim, which could be difficult to identify in severe grades of dislocation, and they had limited ability to predict long-term outcome. The LMH method seems to be the most appropriate classification because the main landmarks are more easily defined and the method had better prognostic ability. Therefore, this classification of grading severity in late-detected DDH is recommended for routine clinical use.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: This study was approved by our institutional review board. Formal consent is not required for this type of work (anonymized radiographs).
ICMJE Conflict of interest statement
None declared.
Acknowledgements
The authors would like to thank the photographer Øystein Horgmo for help with the illustrations.
Author Contributions
TT: Planned and executed the study, Wrote the manuscript.
JH: Executed the study, Revised the manuscript.
References
- 1. Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Telger TC, trans. New York: Springer Verlag, 1987:82-83. [Google Scholar]
- 2. Boniforti FG, Fujii G, Angliss RD, Benson MKD. The reliability of measurements of pelvic radiographs in infants. J Bone Joint Surg [Br] 1997;79-B:570-575. [DOI] [PubMed] [Google Scholar]
- 3. Terjesen T, Rundén TØ, Tangerud A. Ultrasonography and radiography of the hip in infants. Acta Orthop Scand 1989;60:651-660. [DOI] [PubMed] [Google Scholar]
- 4. Narayanan U, Mulpuri K, Sankar WN, et al. Reliability of a new radiographic classification for developmental dysplasia of the hip. J Pediatr Orthop 2015;35:478-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ramo BA, De La Rocha A, Sucato DJ, Jo C-H. A new radiographic classification system for developmental hip dysplasia is reliable and predictive of successful closed reduction and late pelvic osteotomy. J Pediatr Orthop 2018;38:16-21. [DOI] [PubMed] [Google Scholar]
- 6. Talathi NS, Trionfo A, Patel NM, et al. Should I plan to open? Predicting the need for open reduction in the treatment of developmental dysplasia of the hip. J Pediatr Orthop 2020;40:e329-e334. [DOI] [PubMed] [Google Scholar]
- 7. Rosen A, Gamble JG, Vallier H, et al. Analysis of radiographic measurements as prognostic indicators of treatment success in patients with developmental dysplasia of the hip. J Pediatr Orthop B 1999;8:118-121. [PubMed] [Google Scholar]
- 8. Heesakkers NAM, MMEH Witbreuk, Besselaar PP, Van Der Sluijs JA. Retrospective radiographic evaluation of treatment results of developmental dysplasia of the hip in walking-age children. J Pediatr Orthop B 2013;22:427-431. [DOI] [PubMed] [Google Scholar]
- 9. Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology (Oxford) 2005;44:211-218. [DOI] [PubMed] [Google Scholar]
- 10. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand 1939;83(suppl 58):7-135. [Google Scholar]
- 11. Miao M, Cai H, Hu L, Wang Z. Retrospective observational study comparing the international hip dysplasia institute classification with the Tönnis classification of developmental dysplasia of the hip. Medicine (Baltimore) 2017;96:e5902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ismiarto YD, Agradi P, Helmi ZN. Comparison of interobserver reliability between junior and senior resident in assessment of developmental dysplasia of the hip severity using Tönnis and International Hip Dysplasia Institute radiological classification. Malays Orthop J 2019;13:60-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bolland BJ, Wahed A, Al-Hallao S, Culliford DJ, Clarke NMP. Late reduction in congenital dislocation of the hip and the need for secondary surgery: radiologic predictors and confounding variables. J Pediatr Orthop 2010;30:676-682. [DOI] [PubMed] [Google Scholar]
- 14. Alassaf N. Prediction of the requirement of open reduction for developmental dysplasia of the hip. J Int Med Res 2018;46:54-61. [DOI] [PMC free article] [PubMed] [Google Scholar]




