To the Editor:
As the first wave of COVID-19 came to a relative trough during May 2020 in parts of Europe and some states in the United States, for example Vermont, New York, and New Jersey, we are now beginning to observe a resurgence in acute myocardial infarction (AMI) admissions in Israel.1
We collected data from consecutive patients who presented with AMI who were hospitalized in the Intensive Coronary Care Unit of a single tertiary medical centre in Israel during a 10-week period from March 8 through May 16, 2020. Social distancing restrictions were announced in Israel on March 11, 2020. We compared the mean daily AMI hospitalization rates during this period and the corresponding periods during 2017-2019. The incidence of newly confirmed coronavirus cases in Israel was determined on the basis of the Ministry of Health records.
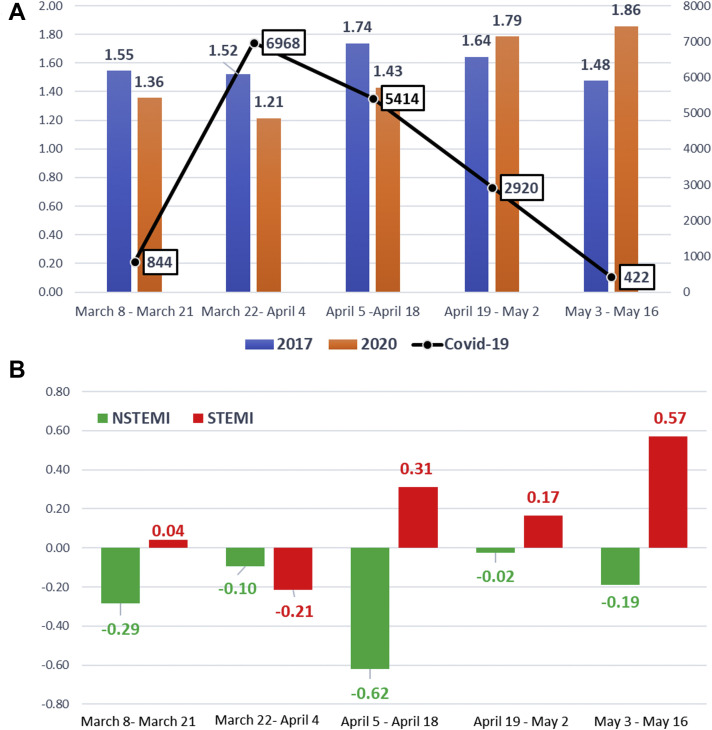
Our study comprised 440 consecutive patients, of whom 107 (24%) were hospitalized during the COVID-19 outbreak. The median age was 66 years (interquartile range, 56-75 years), 341 (78%) were male, and 241 (55%) were diagnosed with ST-elevation myocardial infarction (STEMI). In agreement with previous studies,2 , 3 we observed a 12%, 20%, and 18% reduction in the AMI daily admission rates during 3 biweekly periods at the early phase of the coronavirus outbreak (March 8-21, March 22 to April 4, and April 5-18,respectively), compared with the mean hospitalization incidence during the corresponding periods in 2017-2019. In contrast, we observed a 9% and 26% increase in AMI admissions during 2 biweekly periods at the late phase (April 19 to May 2, and May 3-16, 2020). The trend in AMI hospitalizations inversely correlated with the rise and fall in the incidence of newly diagnosed coronavirus cases during the parallel time periods (Fig. 1 A). As shown in Figure 1B, there was a substantial difference in the trends of non-STEMI (NSTEMI) and STEMI admissions. Although the observed reduction in AMI admissions during the early phase was derived mainly from a reduction in NSTEMI then STEMI patients, the rebound increase in AMI admissions during the late phase reflected by a remarkable increase in the STEMI rates (16% and 100% elevation, respectively). The rebound increase in hospitalizations during the late phase of the COVID-19 outbreak was characterized by a significantly greater proportion of men compared with the corresponding period in 2017-2019 (88% vs 70%; P = 0.01), and numerically higher compared with the early phase of the COVID-19 outbreak (88% vs 77%; P = 0.12). The proportion of older patients (> 65 years) was numerically higher compared with both previous years (67% vs 52%; P = 0.07) and the early phase of the COVID-19 pandemic (67% vs 52%; P = 0.12). We observed no difference in other baseline characteristics.
Figure 1.
Rebound effect of acute myocardial infarction admissions during fading of coronavirus outbreak. (A) Mean daily admission rate of acute myocardial infarction (STEMI and NSTEMI) during 5 subsequent biweekly periods in 2017-2019 (blue bars) and 2020 (orange bars). The Black line represents cumulative incidence of newly confirmed coronavirus cases during the same periods of time. (B) Difference in daily STEMI hospitalization rates between 2020 and the corresponding period in 2017-2019 (red bars) and NSTEMI hospitalization rates between similar time frames (green bars). NSTEMI, non-ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction.
To our knowledge, this is the first report of a worrisome increase in STEMI hospitalizations correlating with the fading of the first wave of the COVID-19 pandemic. In contrast, the trend of the reduction in NSTEMI hospitalization rates, also milder in its extent, continued during the decline in the number of COVID-19 cases. Although the explication of underlying mechanisms for these trends is beyond the scope of this report, the surge in the incidence of AMI after national disasters has been previously described.4 Regarding the different trend in NSTEMI admissions, we could hypothesize that NSTEMI patients manifest less severe symptoms than STEMI patients and might be able to tolerate them for a longer time and might opt, therefore, to remain at home even during a reduction in COVID-19 cases. We of course cannot rule out that the differences between NSTEMI and STEMI represent different biologic effects of strenuous triggers on the occurrence of NSTEMI and STEMI.
Despite the limitations of this single-centre observational study, the post-COVID-19 rebound effect should be addressed as a unique phenomenon that should be further investigated. We urge health care policy makers and critical care providers to be mindful of the potential for AMI rebound in the context of this COVID-19 pandemic and in future subsequent waves should they emerge.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.CDC. Centers for Disease Control and Prevention Trends in Number of COVID-19 Cases in the US Reported to CDC, by State/Territory. https://www.cdc.gov/COVID-data-tracker/#trends Available at: Accessed August 14, 2020.
- 2.De Filippo O., D’Ascenzo F., Angelini F., et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leor J., Poole W.K., Kloner R.A. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334:413–419. doi: 10.1056/NEJM199602153340701. [DOI] [PubMed] [Google Scholar]