Abstract
Background
Sexual minority men who use drugs have high sexual HIV transmission risk. Sexual interactions may also increase COVID-19 risk.This study compared marijuana use, other illegal drugs use (i.e. cocaine/crack, methamphetamine, MDMA/ecstasy, GHB, and ketamine) and sexual behavior with casual partners among sexual minority cismen active on social networking and dating applications before and during the COVID-19 epidemic.
Methods
This cohort-control study compared 455 adult respondents (surveyed May 6th to 17th, 2020) and a matched sample selected from 65,707 respondents surveyed pre-COVID. Participants were recruited on social networking and dating applications and completed surveys online.
Results
The proportion reporting marijuana use declined significantly in the COVID cohort (34.5 % versus 45.7 % pre-COVID,p < .001) as did their illegal drug use (11.0 % versus 22.9 % pre-COVID, p < .001). While the number of casual partners per month was stable, the proportion reporting condomless anal sex with casual partners declined significantly during COVID (26.4 % versus 71.6 % pre-COVID, p < .001). The effect of illegal drug use (excluding marijuana) on number of casual partners per month (aRR = 1.45 pre-COVID versus 2.84, p < .01) and odds of condomless anal sex (aOR = 2.00 pre-COVID versus 5.22, p = .04) were significantly greater in the COVID cohort.
Conclusions
While the proportion of participants reporting drug use and condomless anal sex with casual partners declined in the COVID cohort, the association between drug use and sexual behavior was magnified. Sexual minority men who use drugs are significantly more likely to engage in sexual behaviors that place them at risk for HIV and COVID-19 transmission.
Keywords: SARS-CoV-2, Marijuana, Sexual risk taking, HIV, Gay and bisexual males
1. Introduction
Since December 2019, the Coronavirus Disease 2019 (COVID-19)—otherwise known as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—pandemic has affected billions of lives across the globe (World Health Organization, 2020). The United States alone has accounted for over 5.4 million infections and more than 170,000 deaths as of August 2020 (Coronavirus Resource Center, 2020). In the absence of biomedical treatment and prevention options, non-pharmaceutical interventions, such as social distancing, remain the sole efforts to reduce transmission rates (Centers for Disease Control and Prevention, 2020; Koirala et al., 2020).
According to the Centers for Disease Control and Prevention, social distancing comprises a set of behavioral practices that aim to reduce close proximity between persons (i.e., maintaining 6 feet of distance from others, limiting social activity, and face covering) (Centers for Disease Control and Prevention, 2020b). Limited research on social distancing and COVID-19 (Koo et al., 2020) has shown that such behavioral practices are effective in mitigating risk of infection and preventing the overburdening of local healthcare systems when properly implemented (Haqqi et al., 2020).
Sexual minority men – including gay, bisexual and other men who have sex with men – accounted for 69 % of new HIV diagnoses in the United States in 2018 (Centers for Disease Control and Prevention, 2020a). Condomless anal sex (CAS) in the absence of pre-exposure prophylaxis (PrEP) to prevent HIV infection is the most common mode of transmission (Centers for Disease Control and Prevention, 2019). Sexual interactions present a risk for COVID-19 transmission even when HIV prevention strategies are used.
Exacerbating their HIV risk, sexual minority men use substances—including marijuana and other illegal drugs—at higher rates than heterosexual men (Medley et al., 2016; Schuler et al., 2019). A substantial body of literature illustrates a consistent link between the use of illegal drugs (e.g., cocaine, methamphetamine, ketamine, gamma hydroxybutyrate – GHB, mephedrone, or Methylenedioxymethamphetamine – MDMA/ecstasy) and an increased risk of engaging in sexual HIV transmission risk (Kurka et al., 2015; Petersson et al., 2016). Studies utilizing both aggregate and event-level data indicate that sexual minority men who use illegal drugs (excluding marijuana in most studies) are more likely to engage in CAS with casual partners (Card et al., 2017; Daskalopoulou et al., 2014; Rendina et al., 2015).
While many studies aggregate these substances into a single indicator, there is substantial evidence that individual illegal drugs have specific associations with sexual behavior. Research has consistently found associations between CAS and stimulant use among sexual minority men, in particular that of methamphetamine and cocaine (Daskalopoulou et al., 2014; Johnson et al., 2017; Melendez-Torres et al., 2016b; Semple et al., 2017). Although findings are less robust, CAS has also been linked to the use of sedatives, such as ketamine and GHB (He et al., 2018; Melendez-Torres et al., 2016a; Ottaway et al., 2016). Limited research has also found a higher propensity for CAS among sexual minority men who report the singular use of MDMA prior to or during a sexual encounter (Barrón-Limón et al., 2012). Furthermore, while studies have suggested that polydrug use (excluding marijuana) in sexual contexts is prevalent among sexual minority men, the concurrent use of multiple drugs specified above has been associated with an increased likelihood of CAS (Evers et al., 2019; Pakianathan et al., 2018).
A breadth of existing research on drug use has shown that the use of marijuana is associated with sexual risk broadly (Andrade et al., 2013; Metrik et al., 2016; Zhang and Wu, 2017). Among sexual minority men in particular, marijuana is consistently indicated among the substances most commonly used in conjunction with sex (e.g., Mor et al., 2019; Morgan et al., 2016). Some studies on sexual minority men have found that the use of marijuana in the context of sex is also associated with an increased risk for CAS with casual partners (e.g., Mitchell et al., 2016; Passaro et al., 2019). As marijuana use with sex is likewise associated with CAS with main partners, those who are partnered and non-monogamous are also at increased risk of HIV infection between main partners (Mitchell et al., 2016).
In spite of speculation that the pandemic may result in increased substance use for society at large, preliminary findings from the European Monitoring Centre for Drugs and Drug Addiction have indicated a decrease in use during the pandemic’s first three months (Mota, 2020; European Monitoring Centre for Drugs and Drug Addiction, 2020). In fact, widespread lockdown orders across Europe from March to May 2020 saw disruptions to the production and distribution of illegal drugs and a subsequent decline in individual use (European Monitoring Centre for Drugs and Drug Addiction, Europol, 2020). However, more robust data on differences in substance use pre and post-pandemic—for sexual minority men notwithstanding—is still very limited (Mota, 2020).
Recent retrospective data suggests sexual minority men have fewer sex partners during the COVID-19 pandemic while condom use during sex or drug use have remained stable (Sanchez et al., 2020). Understanding the prevalence of drug use and sexual behavior among sexual minority men during the COVID-19 pandemic has critical prevention implications. Non-compliance with social distancing guidelines and pandemic-related barriers to HIV testing (Santos et al., 2020) may contribute to an increase in concurrent COVID-19 and HIV diagnoses.
This study compared the prevalence of drug use and sexual behaviors among sexual minority men pre-COVID-19 and during the epidemic using a cohort-control design. We hypothesized sexual minority men would report fewer casual sex partners while the proportion reporting condomless sex with casual partners and drug use would remain unchanged. In addition, we hypothesized drug use would be associated with engagement in sexual behaviors that may transmit COVID-19 and HIV.
2. Methods
2.1. Participants
Participants included in these analyses were aged 18 or older. All indicated cismale gender. Those participants in relationships indicated that their partner was cismale as well. Due to the nature of casual sex partner data collection, respondents included in the COVID cohort who reported vaginal sex were excluded. All participants completed consent and responded in English.
2.2. Procedures
Cohorts were recruited between May 6 and May 17, 2020 (COVID) and between November, 2017 and November, 2019 (pre-COVID). In both cohorts, recruitment occurred through geosocial networking apps for gay, bi, trans, and queer people seeking sexual partners. The COVID cohort responded to an advertisement that included an image of one or more adolescent or adult males. The study name “PRIDE Endures” and one of several study tag lines (e.g., “Sex in the time of social distancing” or “COVID-19 and the LGBTQ + community”). Pre-COVID cohort electronic advertisements contained similar images. Study tag lines varied over the two years of data collection, but were typically crafted to appeal to sexual and gender minority people broadly or sexual minority men specifically (e.g., “UNITE to end the epidemic,” “In a gay relationship?” or “Click here to find out if you are eligible for one of our paid research studies.”).
Respondents who clicked on the ad were directed to consent information. Those consenting completed online surveys administered through Qualtrics. Participants in the pre-COVID cohort completed a brief screening survey, completion time approximately 10 min, intended to establish eligibility for a number of ongoing studies. Their participation was not compensated. Participants in the COVID cohort completed a survey that comprised a broader range of measures. Completion time was approximately 30 min. At the end of the survey, participants had the option to provide an email contract and be entered into a random drawing for one of 20 Amazon.com gift certificates worth $50 each. All procedures for collection of data from both cohorts were approved by the Institutional Review Board of Hunter College, City University of New York.
2.3. Measures
2.3.1. Demographics
Participants provided their birthdate, which was used to calculate age, as well as their zip code of residence. Zip code was utilized to determine geographical region of residence in the U.S.A. Race (Asian or Asian American, Black or African American, American Indian or Alaska Native, White, Native Hawaiian or Pacific Islander, and Other) and ethnicity (Hispanic or Latino versus not Hispanic or Latino) were assessed independently and consolidated into a single variable indicating identification as White, Black, Latino, or Other. Participants also responded to items indicating biological sex (male, female, or other); gender identity (male, female, transmale, transfemale, non-binary/gender-queer/agender/gender non-conforming, or other); sexual identity (gay, lesbian, bisexual, heterosexual, queer, other); relationship status (single/not single; what best describes your relationship status); PrEP uptake (yes versus no), and HIV status (positive, negative or unknown).
2.3.2. Drug use
In the pre-COVID survey, participants indicated the number of days in the past 3 months (90 days) that they used marijuana, cocaine, crack, crystal methamphetamine, GHB, and Ketamine. To achieve consistency with COVID-cohort responses, data were aggregated into four dichotomous variables indicating whether or not a participant used marijuana, cocaine or crack, methamphetamine, and MDMA, GHB, or Ketamine. In the COVID-cohort, participants indicated whether or not they used marijuana, cocaine or crack, methamphetamine, and MDMA, GHB, or Ketamine in the past 90 days. In regression analyses, responses to variables measuring the use of cocaine or crack, methamphetamine, and MDMA, GHB or Ketamine were aggregated into a single variable indicate the use of any of these illegal drugs in the past 90 days.
2.3.3. Number of casual male sex partners
After providing information about relationship status, including the identification of their main partner, pre-COVID respondents reported the number of male sex partners excluding their main partner in the past 6-months. This number was transformed to a 30-day rate for comparability with responses from the COVID cohort. In the COVID cohort, participants were similarly asked to indicate their relationship status and identify their main partner. After this, respondents reported the number of sex partners in the past 30-days, regardless of gender, excluding their main partner. Participants who reported any vaginal sex with a casual partner were excluded from analyses.
2.3.4. Condomless anal sex (CAS) with casual male partners
Pre-COVID respondents who reported having any casual male sex partners subsequently reported the number of times they had condomless sex with any casual partner who had the same, different or unknown HIV status in the last 6 months. For comparability with the COVID-cohort, responses were aggregated into a single variable indicating the occurrence of any CAS with a casual male partner. COVID-cohort respondents who reported at least one casual sex partner subsequently indicated the number of partners with whom they had anal sex. Those indicating anal sex were asked to indicate their use of condoms with casual anal sex partners (“We always used condoms”; “We had sex without a condom at least once” or “We never use condoms.”). Responses were recoded into a single variable indicating the occurrence of any CAS with a casual partner.
2.4. Statistical analysis
Survey responses were inspected for duplicates based upon convergent information from IP addresses, contact information, and demographic responses. Responses were also screened for patterned or improbable responses. The matched sample was selected based upon a set of characteristics with well-established associations with HIV infection risk including age, race and ethnicity, relationship status, and geographic location in the U.S.A. (e.g., Centers for Disease Control and Prevention, 2020; Sullivan et al., 2009). In addition, matching procedures accounted for sexual orientation or identity (Everett, 2013), HIV status, and PrEP uptake (e.g., Gafos et al., 2019; Parsons et al., 2017), common correlates of sexual behavior.
Samples were matched using the MatchIt package (3.0.2) in R (4.0.2) on propensity scores calculated via regression trees with parameters tuned to optimize accuracy in cohort prediction (Stuart, 2010). Regression models calculated in Mplus (v8.2) examined associations between drug use and sexual behaviors in a multivariable context. The number of casual partners and CAS with casual partners were analyzed as negative binomial and logistic distributions respectively. These models included demographic covariates in addition to the main effects of marijuana and other illegal drugs, cohort, and cohort by drug use interaction terms. Offset terms were included to control for differences in reporting period between cohorts; the COVID-cohort assessed a 30-day span, while the pre-COVID cohort assessed a 6-month span. Weights were therefore set to 1 for all COVID-cohort respondents and 6 for all pre-COVID respondents in these models.
3. Results
A total of 1001 participants began the COVID survey and 455 (45.5 %) sexual minority men met eligibility criteria for these analyses and provided complete responses to the -COVID survey. The pre-COVID cohort was drawn from a pool of 65,707 sexual minority men. Table 1 contains demographic data for both cohorts. Consistent with the success of propensity score matching procedures, cohorts did not differ significantly with respect to any demographic variables. The average age across cohorts was 40.53 (SD = 13.41). In both samples, approximately 48.2 % of respondents indicated a majority White racial and ethnic identity (the remaining identified as 28.7 % Black; 13.8 % Latino; and 9.2 % Other). Most identified as gay (77.0 %) or bisexual (18.1 %) and indicated that their relationship status was single (77.3 %). The majority of the sample was HIV negative (55.5 % not on PrEP and 20.2 % on PrEP) while the remaining (24.3 %) indicated an HIV positive sero-status. The sample was geographically diverse with respect to location of residence in the U.S.A. Most respondents indicated they lived in the South (38.4 %), with 23.7 % residing in the Northeast, 18.2 % in the Midwest, and 19.1 % in the West (Table 1).
Table 1.
Demographic characteristics.
| Cohort |
χ2 (DF) | P value | |||
|---|---|---|---|---|---|
| Total (n = 910) | Pre-COVID (n = 455) | COVID (n = 455) | |||
| n (%) | n (%) | n (%) | |||
| Race/Ethnicity | |||||
| Black | 261 (28.7) | 130 (28.6) | 131 (28.8) | 0.01 (1) | 0.94 |
| Latino | 126 (13.8) | 63 (13.8) | 63 (13.8) | 0.00 (1) | 1.00 |
| White | 439 (48.2) | 220 (48.4) | 219 (48.1) | 0.00 (1) | 0.95 |
| Other | 84 (9.2) | 42 (9.2) | 42 (9.2) | 0.00 (1) | 1.00 |
| Region | |||||
| Northeast | 216 (23.7) | 108 (23.7) | 108 (23.7) | 0.00 (1) | 1.00 |
| Midwest | 166 (18.2) | 83 (18.2) | 83 (18.2) | 0.00 (1) | 1.00 |
| South | 349 (38.4) | 177 (38.9) | 172 (37.8) | 0.12 (1) | 0.73 |
| West | 174 (19.1) | 87 (19.1) | 87 (19.1) | 0.00 (1) | 1.00 |
| Sexual Orientation | |||||
| Gay | 701 (77.0) | 353 (77.6) | 348 (76.5) | 0.16 (1) | 0.69 |
| Bisexual | 165 (18.1) | 80 (17.6) | 85 (18.7) | 0.19 (1) | 0.67 |
| Other | 44 (4.8) | 22 (4.8) | 22 (4.8) | 0.00 (1) | 1.00 |
| PrEP, HIV | |||||
| Positive | 221 (24.3) | 108 (23.7) | 113 (24.8) | 0.15 (1) | 0.70 |
| Negative, no PrEP Rx | 505 (55.5) | 255 (56.0) | 250 (54.9) | 0.11 (1) | 0.74 |
| Negative, PrEP Rx | 184 (20.2) | 92 (20.2) | 92 (20.2) | 0.00 (1) | 1.00 |
| Relationship status | |||||
| Single | 703 (77.3) | 351 (77.1) | 352 (77.4) | 0.01 (1) | 0.98 |
| Partnered | 207 (22.7) | 104 (22.9) | 103 (22.6) | 0.01 (1) | 0.98 |
| Drug Use | |||||
| Marijuana | 365 (40.1) | 208 (45.7) | 157 (34.5) | 11.90 (1) | <0.01 |
| Other illegal Drugs | 154 (16.9) | 104 (22.9) | 50 (11.0) | 22.79 (1) | <0.001 |
| Meth | 87 (9.6) | 54 (11.9) | 33 (7.3) | 5.61(1) | 0.02 |
| MDMA, GHB, K | 78 (8.6) | 61 (13.4) | 17 (3.7) | 27.15(1) | < 0.001 |
| Cocaine, Crack | 67 (7.4) | 48 (10.5) | 19 (4.2) | 13.55 (1) | < 0.001 |
| CAS with casual partners | 446 (49.0) | 326 (71.6) | 120 (26.4) | 186.61 (1) | < 0.001 |
| M (SD) | M (SD) | M (SD) | Test Statistic | ||
| Age | 40.53 (13.41) | 40.08 (13.40) | 40.97 (13.42) | t(908) = -0.99 | 0.32 |
| Casual sex partners, per month | 1.56 (3.14) | 1.59 (3.07) | 1.53 (3.22) | Waldχ2(1) = 0.25 | 0.62 |
The proportion of participants reporting marijuana use declined significantly from 45.7 % pre-COVID to 34.5 % during COVID). Similarly, the proportion of respondents reporting other illegal drug use declined significantly from 22.9 % pre-COVID to 11.0 % during COVID. Significant declines were observed uniformly across subtypes of illegal drugs (cocaine//crack, methamphetamine, and MDMA, GHB or Ketamine). Similarly, The unweighted probability of reporting CAS with a casual partner declined significantly from 71.6 % pre-COVID to 26.4 % during COVID; however, the weighted number of casual sex partners did not differ significantly (Mpre-COVID = 1.59, SD = 3.07 versus Mduring COVID = 1.53, SD = 3.22).
3.1. Associations between drug use and casual male sex partners per month
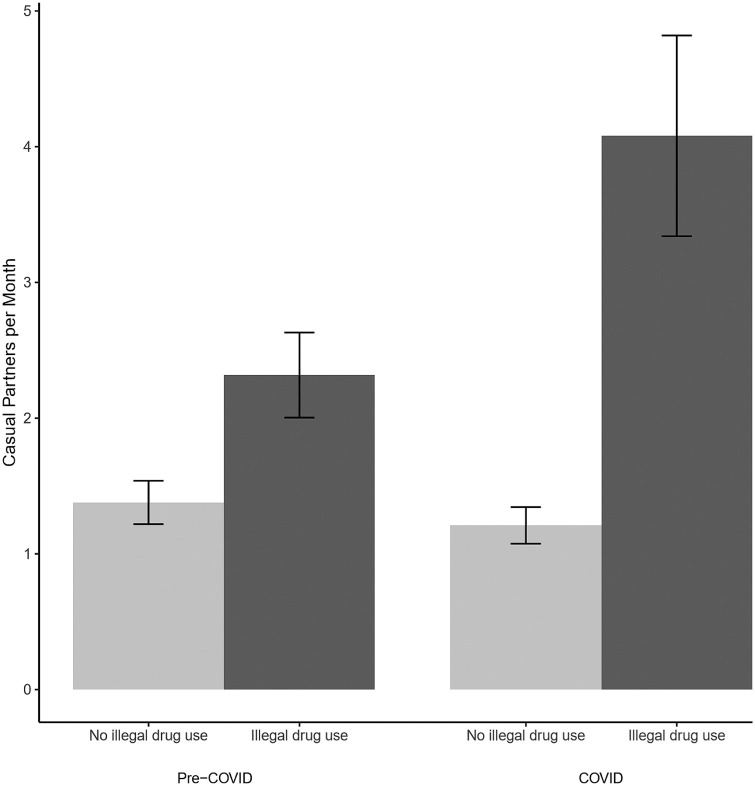
Results of regression models (Table 2 ) indicated that, pre-COVID, the use of marijuana and other illegal drugs were both associated with reporting significantly more casual partners per month (aRR = 1.34, p = .03 and aRR = 1.45, p = .02 respectively). The effect of other illegal drug use increased significantly in the COVID cohort; meanwhile, the effect of marijuana did not differ significantly between cohorts. As a result, in the COVID-cohort, both marijuana and other illegal drug use remained significantly associated with number of casual partners (aRR = 1.58, p = .02 and aRR = 2.84, p < .01 respectively). Fig. 1 displays the mean number of casual partners per month reported by respondents who indicated the use of illegal drugs (excluding marijuana) compared to those who did not for participants in both cohorts.
Table 2.
Associations of demographic and substance use correlates with risky sexual behavior during COVID-19 time-period versus pre-COVID reports (n = 910).
| Casual partners per month |
Condomless anal sex with casual partners |
|||||
|---|---|---|---|---|---|---|
| Adjusted Rate Ratio |
95 % Confidence Interval |
p | Adjusted Odds Ratio |
95 % Confidence Interval |
p | |
| Age | 1.01 | (0.998, 1.017) | 0.14 | 1.00 | (0.98, 1.01) | 0.76 |
| Race/Ethnicity (ref = White) | ||||||
| Black | 0.85 | (0.66, 1.09) | 0.20 | 0.97 | (0.63, 1.50) | 0.90 |
| Latino | 1.00 | (0.71, 1.40) | 0.99 | 0.75 | (0.45, 1.24) | 0.26 |
| Other | 1.23 | (0.70, 2.14) | 0.47 | 1.00 | (0.57, 1.74) | 0.99 |
| Region (ref = Northeast) | ||||||
| Midwest | 1.07 | (0.75, 1.51) | 0.72 | 0.73 | (0.45, 1.19) | 0.21 |
| South | 1.03 | (0.80, 1.33) | 0.83 | 1.03 | (0.68, 1.56) | 0.90 |
| West | 1.18 | (0.83, 1.66) | 0.36 | 1.24 | (0.78, 1.96) | 0.36 |
| Sexual Orient (ref = Gay) | ||||||
| Bisexual | 0.81 | (0.64, 1.03) | 0.09 | 0.79 | (0.51, 1.24) | 0.31 |
| Other Orient | 0.63 | (0.39, 1.01) | 0.06 | 0.91 | (0.46, 1.81) | 0.79 |
| PrEP, HIV (ref = Neg/Unk, no PrEP Rx) | ||||||
| HIV positive | 1.33 | (1.01, 1.74) | 0.04 | 2.18 | (1.42, 3.33) | 0.00 |
| Current PrEP | 1.60 | (1.21, 2.10) | 0.00 | 2.08 | (1.40, 3.11) | 0.00 |
| Drug Use | ||||||
| Marijuana | 1.34 | (1.03, 1.72) | 0.03 | 1.88 | (1.19, 2.97) | 0.01 |
| Other illegal drugs | 1.45 | (1.07, 1.98) | 0.02 | 2.00 | (1.07, 3.72) | 0.03 |
| Relationship Status (ref = Partnered) | ||||||
| Single | 1.30 | (1.01, 1.68) | 0.04 | 1.58 | (1.06, 2.36) | 0.03 |
| Cohort | 0.02 | (0.018, 0.034) | 0.00 | 0.02 | (0.012, 0.029) | 0.00 |
| Interactions | ||||||
| Cohort*Marijuana | 1.18 | (0.76, 1.83) | 0.45 | 1.03 | (0.54, 1.98) | 0.93 |
| Cohort*Other illegal drugs | 1.96 | (1.19, 3.21) | <0.01 | 2.61 | (1.05, 6.49) | 0.04 |
Fig. 1.
Observed number of casual male partners per month across cohorts: Associations with illegal drug use (excluding marijuanna).
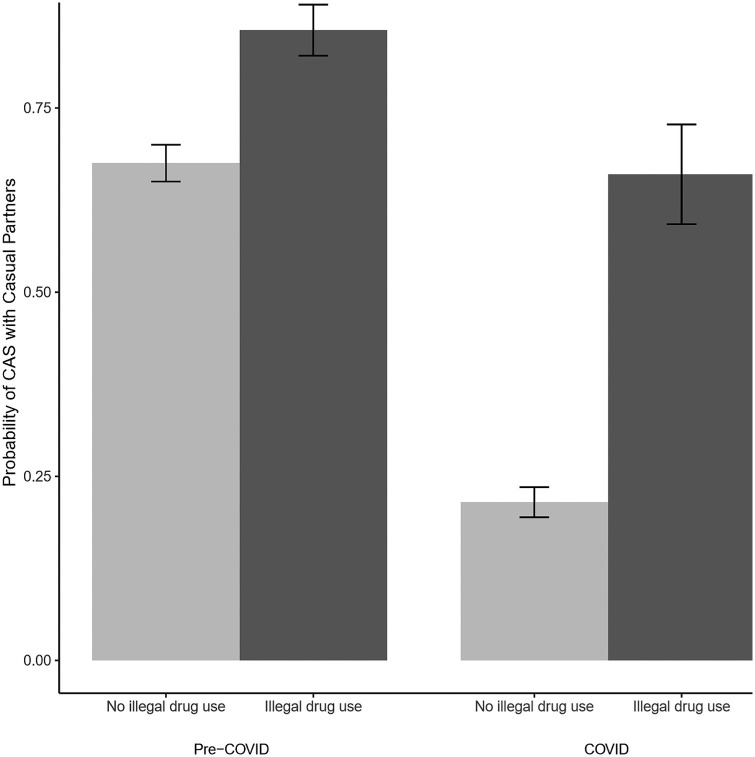
3.2. Associations between drug use and CAS with casual male partners
Results of regression models (Table 2) indicated that, pre-COVID, the use of marijuana and other illegal drugs were both associated with significantly greater odds of engaging in CAS with a casual partner (aOR = 1.88, p = .01 and aOR = 2.00, p = .03 respectively). The effect of other illegal drug use increased significantly in the COVID cohort; meanwhile, the effect of marijuana did not differ significantly between cohorts. As a result, in the COVID cohort, both marijuana and other illegal drug use remained significantly associated with the odds of CAS with casual partners (aOR = 1.58, p = .03 and aOR = 5.22, p < .01 respectively). Fig. 2 displays the probability of CAS with casual partners reported by respondents who indicated the use of illegal drugs (excluding marijuana) compared to those who did not for participants in both cohorts.
Fig. 2.
Observed probability of condomless anal sex with casual partners across cohorts: Associations with illegal drug use (excluding marijuanna).
4. Discussion
While the proportion of participants reporting marijuana and other illegal drug use as well as CAS with casual partners declined during COVID, the association between other illegal drug use and sexual risk behavior was amplified. These results suggest that though rates of drug use overall may have fallen, those sexual minority men who use drugs continue to face elevated risks of HIV transmission. To the extent that sexual interactions with casual partners also constitute a breach in social distancing practices, these sexual minority men who use drugs are at particularly high risk of engaging in sexual behaviors that place them at risk for COVID-19 infection as well. Notably, while interaction terms were non-significant, marijuana use alone was also associated with an increase in casual sex partners per month and greater odds of CAS with casual partners in both cohorts. While the magnitude of the effect was smaller than that observed for other illegal drug use, particularly in the COVID-cohort, there is at least some indication of increased risk among those sexual minority men who use marijuana.
While these findings partially align with existing data indicating declining engagement in sexual behavior with casual partners among sexual minority men (Sanchez et al., 2020); they also indicate that this general assertion requires substantial contextualization. Broadly, these results indicate that declines were restricted primarily to the occurrence of CAS with casual partners while the overall number of casual partners per month was stable across cohorts. Furthermore, the number of casual male sex partners per month actually increased among men who used illegal drugs (excluding marijuana) despite stability in the overall sample.
To date, few data are available on trends in drug use since the onset of the COVID-19 pandemic. While limited research on substance use in Europe has found a decrease in use within the first three months of the pandemic, no research has identified any such trend in substance use in the U.S.A within this same timeframe (European Monitoring Centre for Drugs and Drug Addiction, Europol, 2020). The findings from the current study indicate that both marijuana and other illegal drug use have declined significantly among sexual minority men in the U.S.A. active in online social networking and dating spaces. One plausible explanation for these findings is that COVID-19 has made it more challenging to access drugs or more financially difficult to afford their costs. Mota (2020) cogently points to the risks that the stress of the pandemic and the demands of quarantine and social distancing might exacerbate problems associated with substance use. While these findings provide no indication that substance use is expanding among sexual minority men – they do suggest that those sexual minority men who are using drugs during the COVID-19 pandemic face exacerbated sexual health risks consistent with Mota’s (2020) general premise.
Sanchez et al. (2020) suggested that while sexual minority men followed early social distancing directives, long-term compliance may prove challenging. Those sexual minority men who use drugs may be among the most likely to deviate from distancing guidance through sexual interactions. It has been suggested that HIV prevention interventions may inform COVID-19 prevention efforts (Eaton and Kalichman, 2020). Interventions tailored for sexual minority men addressing drug use and HIV prevention exist (e.g., Parsons et al., 2014; Starks et al., 2019a, b). Potentially relevant interventions have also been developed addressing drug use and HIV medication adherence for HIV positive sexual minority men (e.g., Kahler et al., 2018; Mimiaga et al., 2018; Naar et al., in press; Reback and Shoptaw, 2014). These findings point to the potentially urgent need to adapt and implement such interventions to also address COVID-19 risk.
The COVID-19 pandemic has evolved dramatically during the course of only a few months (Coronavirus Resource Center, 2020). From May 6 to May 17, when data were collected from the COVID-cohort, the primary epicenters of infection in the U.S.A. were states in the Northeast (New York, New Jersey and Connecticut) as well as the West (Washington) (Coronavirus Resource Center, 2020a). Trends from June through August, 2020 indicate the pandemic stabilized in the Northeast, while rates of new infections spiked in a number of Southern (Texas, Georgia, and Florida) and Western (California, and Arizona) states at various times (Coronavirus Resource Center, 2020a). Ongoing surveillance will be required to track the evolution of drug use and sexual behavior over time as the epidemic continues to unfold.
Generalizability is limited by recruitment from dating and social networking applications. It is plausible that fewer sexual minority men overall are utilizing these kinds of applications during COVID-19 pandemic and those who continue to use them represent a unique subset of sexual minority men. There is also some methodological variability in survey length and compensation for participation that may have led to different levels of respondent motivation and attrition between the two cohorts. This threat to internal validity is addressed, at least in part, by the use of a matched cohort also recruited in the same venues as the COVID-cohort respondents. While these findings may not generalize to the larger population of sexual minority men, they do point to substantial health risks – for both COVID-19 and HIV transmission – faced by those sexual minority men who use drugs and continue to occupy these online spaces. Trends in drug use and sexual behavior among sexual minority men may not generalize across gender and sexual orientation groups. Two additional caveats limiting causal inferences must be acknowledged. First, while our matching procedures were successful, the use a cohort control design precludes an examination of within-person variability in outcome behaviors over time. Second, regression analyses testing associations between drug use and sexual behavior were cross-sectional. While they provide information about the co-occurrence of these behaviors, they do not constitute evidence of casual associations between them.
This paper presents the most rigorous assessment to date of the impact the COVID-19 pandemic has had on the drug use and sexual behavior of sexual minority men in the U.S.A. Sexual minority men who use drugs faced high rates of HIV infection prior to COVID-19. While rates of use have declined; those sexual minority men who use drugs during COVID are in urgent need of both HIV and COVID-19 prevention.
Author contribution
Tyrel Starks planned the study which produced the data and was primarily responsible for formulating the research question and designing the analytic plan.
Scott Jones executed the analytic plan and contributed substantially to Methods and Results sections.
Daniel Sauermilch and Matthiew Benedict contributed to the literature review and discussion.
Trinae Adebayo provided extensive support for data collection and management.
Demetria Cain collaborated in study design and provided feedback on the overall manuscript.
Kit Simpson consulted on the analytic plan, reviewed preliminary Tables and Results, and provided feedback on the overall manuscript.
All authors have read and approved of the submission.
Role of funding sources
This project was funded by grants from the National Institutes of Health. The funder was not directly involved in the design or execution of the study.
Contributors
Tyrel J. Starks, S. Scott Jones, Daniel Sauermilch, Matthew Benedict, Demetria Cain, Trinae Adebayo, Kit Simpson.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
Data collection for the pre-COVID cohort was supported by grants from the National Institute of Allergy and Infectious Diseases, National Institute on Mental Health, Eunice Kennedy Shriver National Institute on Child Health and Human Development, and National Institute on Drug Abuse (UG3AI133674, PI: Rendina; R01MH114735, PI: Rendina; R01DA041262, PI: Starks; R34DA043422, PI: Starks; R01DA045613, PI: Starks; U19HD089875, PI: Naar).
References
- Andrade L.F., Carroll K.M., Petry N.M. Marijuana use is associated with risky sexual behaviors in treatment-seeking polysubstance abusers. Am. J. Drug Alcohol Abuse. 2013;39(4):266–271. doi: 10.3109/00952990.2013.803112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrón-Limón S., Semple S.J., Strathdee S.A., Lozada R., Vargas-Ojeda A., Patterson T.L. Correlates of unprotected anal sex among men who have sex with men in Tijuana, Mexico. BMC Public Health. 2012;12(1):433. doi: 10.1186/1471-2458-12-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card K.G., Lachowsky N.J., Cui Z., Shurgold S., Armstrong H.L., Rich A.J., Forrest J.I., Gislason M., Moore D.M., Roth E.A., Hogg R.S. An event-level analysis of the interpersonal factors associated with condomless anal sex among gay, bisexual, and other men who have sex with men (MSM) with online-met partners. AIDS Educ. Prev. 2017;29(2):154–174. doi: 10.1521/aeap.2017.29.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2019. HIV Transmission.https://www.cdc.gov/hiv/basics/transmission.html [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Diagnoses of HIV Infection in the United States and Dependent Areas, 2018: Diagnoses.https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol31/content/diagnoses.html#age [Google Scholar]
- Centers for Disease Control and Prevention . 2020. HIV in the United States and Dependent Areas.https://www.cdc.gov/hiv/statistics/overview/ataglance.html [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Social Distancing.https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html [Google Scholar]
- Coronavirus Resource Center . 2020. Coronavirus COVID‐19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University.https://coronavirus.jhu.edu/map.html [Google Scholar]
- Coronavirus Resource Center . 2020. New Cases of COVID-19 in US States by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University.https://coronavirus.jhu.edu/data/new-cases-50-states [Google Scholar]
- Daskalopoulou M., Rodger A., Phillips A.N., Sherr L., Speakman A., Collins S., Elford J., Johnson M.A., Gilson R., Fisher M., Wilkins E., Anderson J., McDonnell J., Edwards S., Perry N., O’Connell R., Lascar M., Jones M., Johnson A.M., Hart G., Miners A., Geretti A.-M., Burman W.J., Lampe F.C. Recreational drug use, polydrug use, and sexual behaviour in HIV-diagnosed men who have sex with men in the UK: results from the cross-sectional ASTRA study. Lancet HIV. 2014;1(1):e22–e31. doi: 10.1016/S2352-3018(14)70001-3. [DOI] [PubMed] [Google Scholar]
- Eaton L.A., Kalichman S.C. Social and behavioral health responses to COVID-19: lessons learned from four decades of an HIV pandemic. J. Behav. Med. 2020;43:341–345. doi: 10.1007/s10865-020-00157-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction . 2020. EMCDDA Trendspotter Briefing: Impact of COVID-19 on Patterns of Drug Use and Drug-related Harms in Europe.https://www.emcdda.europa.eu/system/files/publications/13130/EMCDDA-Trendspotter-Covid-19-Wave-2_1.pdf [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction, Europol . 2020. EU Drug Markets— Impact of COVID-19.https://www.emcdda.europa.eu/system/files/publications/13097/EU-Drug-Markets_Covid19-impact_final.pdf Retrieved from Luxembourg: [Google Scholar]
- Everett B.G. Sexual orientation disparities in sexually transmitted infections: examining the intersection between sexual identity and sexual behavior. Arch. Sex. Behav. 2013;42(2):225–236. doi: 10.1007/s10508-012-9902-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evers Y.J., Van Liere G., Hoebe C., Dukers-Muijrers N. Chemsex among men who have sex with men living outside major cities and associations with sexually transmitted infections: a cross-sectional study in the Netherlands. PLoS One. 2019;14(5) doi: 10.1371/journal.pone.0216732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gafos M., Horne R., Nutland W., Bell G., Rae C., Wayal S., Rayment M., Clarke A., Schembri G., Gilson R., McOwan A., Sullivan A., Fox J., Apea V., Dewsnap C., Dolling D., White E., Brodnicki E., Wood G., Dunn D., McCormack S. The context of sexual risk behaviour among men who have sex with men seeking PrEP, and the impact of PrEP on sexual behaviour. AIDS Behav. 2019;23(7):1708–1720. doi: 10.1007/s10461-018-2300-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haqqi, A., Awan, U.A., Ali, M., Saqib, M.A.N., Ahmed, H., Afzal, M.S., 2020 June. COVID-19 and dengue virus coepidemics in Pakistan: A dangerous combination for an overburdened healthcare system. J. Med. Virol. 10.1002/jmv.26144. [DOI] [PMC free article] [PubMed]
- He L., Pan X., Wang N., Yang J., Jiang J., Luo Y., Zhang X., Li X. New types of drug use and risks of drug use among men who have sex with men: a cross-sectional study in Hangzhou, China. BMC Infect. Dis. 2018;18(1) doi: 10.1186/s12879-018-3091-z. 182–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.W., Herrmann E.S., Sweeney M.M., LeComte R.S., Johnson P.S. Cocaine administration dose-dependently increases sexual desire and decreases condom use likelihood: the role of delay and probability discounting in connecting cocaine with HIV. Psychopharmacology (Berl) 2017;234(4):599–612. doi: 10.1007/s00213-016-4493-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler C.W., Pantalone D.W., Mastroleo N.R., Liu T., Bove G., Ramratnam B., Monti P.M., Mayer K.H. Motivational interviewing with personalized feedback to reduce alcohol use in HIV-infected men who have sex with men: a randomized controlled trial. J. Consult. Clin. Psychol. 2018;86(8):645–656. doi: 10.1037/ccp0000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koirala A., Joo Y.J., Khatami A., Chiu C., Britton P.N. Vaccines for COVID-19: the current state of play. Paediatr. Respir. Rev. 2020;35:43–49. doi: 10.1016/j.prrv.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo J.R., Cook A.R., Park M., Sun Y., Sun H., Lim J.T., Tam C., Dickens B.L. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infect. Dis. 2020;20(6):678–688. doi: 10.1016/S1473-3099(20)30162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurka T., Soni S., Richardson D. O10 Msm report high use of club drugs which is associated with high risk sexual behaviour. Sex. Transm. Infect. 2015;91(Suppl 1):A4. [Google Scholar]
- Medley G., Lipari R.N., Bose J., Cribb D.S., Kroutil L.A., McHenry G. Sexual orientation and estimates of adult substance use and mental health: results from the 2015 National Survey on Drug Use and Health. NSDUH Data Rev. 2016 https://www.samhsa.gov/data/sites/default/files/NSDUH-SexualOrientation-2015/NSDUH-SexualOrientation-2015/NSDUH-SexualOrientation-2015.htm [Google Scholar]
- Melendez-Torres G.J., Hickson F., Reid D., Weatherburn P., Bonell C. Findings from within-subjects comparisons of drug use and sexual risk behaviour in men who have sex with men in England. Int. J. STD AIDS. 2016;28(3):250–258. doi: 10.1177/0956462416642125. [DOI] [PubMed] [Google Scholar]
- Melendez-Torres G.J., Hickson F., Reid D., Weatherburn P., Bonell C. Nested event-level case–control study of drug use and sexual outcomes in multipartner encounters reported by men who have sex with men. AIDS Behav. 2016;20(3):646–654. doi: 10.1007/s10461-015-1127-6. [DOI] [PubMed] [Google Scholar]
- Metrik J., Caswell A.J., Magill M., Monti P.M., Kahler C.W. Sexual risk behavior and heavy drinking among weekly marijuana users. J. Stud. Alcohol Drugs. 2016;77(1):104–112. doi: 10.15288/jsad.2016.77.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga M.J., Pantalone D.W., Biello K.B., Glynn T.R., Santostefano C.M., Olson J., Pardee J.D., Hughto J.M.W., Valles G., Carrico A.W., Mayer K.H., Safren S.A. A randomized controlled efficacy trial of behavioral activation for concurrent stimulant use and sexual risk for HIV acquisition among MSM: project IMPACT study protocol. BMC Public Health. 2018;18(1):914–925. doi: 10.1186/s12889-018-5856-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell J.W., Pan Y., Feaster D. Actor-partner effects of male couples substance use with sex and engagement in condomless anal sex. AIDS Behav. 2016;20(12):2904–2913. doi: 10.1007/s10461-016-1355-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor Z., Turner D., Livnat Y., Levy I. Recreational drug and excessive alcohol use among HIV-infected men who have sex with men in Central Israel. BMC Public Health. 2019;19(1):1360. doi: 10.1186/s12889-019-7747-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan E., Skaathun B., Michaels S., Young L., Khanna A., Friedman S.R., Davis B., Pitrak D., Schneider J. Marijuana use as a sex-drug is associated with HIV risk among black MSM and their network. AIDS Behav. 2016;20(3):600–607. doi: 10.1007/s10461-015-1195-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mota P. Avoiding a new epidemic during a pandemic: the importance of assessing the risk of substance use disorders in the COVID-19 era. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113142. 113142–113142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naar S., Robles G., Macdonell K.E., Dinaj-Koci V., Simpson K.N., Lam P., Parsons J.T., MSizemore K.M., Starks T.J. Comparative effectiveness of community-based vs clinic-based Healthy Choices Motivational Intervention to improve health behaviors among youth living with HIV: A randomized clinical trial. JAMA Netw. Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.14650. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottaway Z., Finnerty F., Amlani A., Pinto-Sander N., Szanyi J., Richardson D. Men who have sex with men diagnosed with a sexually transmitted infection are significantly more likely to engage in sexualised drug use. Int. J. STD AIDS. 2016;28(1):91–93. doi: 10.1177/0956462416666753. [DOI] [PubMed] [Google Scholar]
- Pakianathan M., Whittaker W., Lee M.J., Avery J., Green S., Nathan B., Hegazi A. Chemsex and new HIV diagnosis in gay, bisexual and other men who have sex with men attending sexual health clinics. HIV Med. 2018;19(7):485–490. doi: 10.1111/hiv.12629. [DOI] [PubMed] [Google Scholar]
- Parsons J.T., Lelutiu-Weinberger C., Botsko M., Golub S.A. A randomized controlled trial utilizing motivational interviewing to reduce HIV risk and drug use in young gay and bisexual men. J. Consult. Clin. Psychol. 2014;82(1):9–18. doi: 10.1037/a0035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons J.T., Millar B.M., Moody R.L., Starks T.J., Rendina H.J., Grov C. Syndemic conditions and HIV transmission risk behavior among HIV-negative gay and bisexual men in a US national sample. Health Psychol. 2017;36(7):695–703. doi: 10.1037/hea0000509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passaro R.C., Castañeda-Huaripata A., Gonzales-Saavedra W., Chavez-Gomez S., Segura E.R., Lake J.E., Cabello R., Clark J.L. Contextualizing condoms: a cross-sectional study mapping intersections of locations of sexual contact, partner type, and substance use as contexts for sexual risk behavior among MSM in Peru. BMC Infect. Dis. 2019;19(1):958. doi: 10.1186/s12879-019-4517-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersson F.J.M., Tikkanen R., Schmidt A.J. Party and play in the closet? Exploring club drug use among swedish men who have sex with men. Subst. Use Misuse. 2016;51(9):1093–1103. doi: 10.3109/10826084.2016.1160117. [DOI] [PubMed] [Google Scholar]
- Reback C.J., Shoptaw S. Development of an evidence-based, gay-specific cognitive behavioral therapy intervention for methamphetamine-abusing gay and bisexual men. Addict. Behav. 2014;39(8):1286–1291. doi: 10.1016/j.addbeh.2011.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina H.J., Moody R.L., Ventuneac A., Grov C., Parsons J.T. Aggregate and event-level associations between substance use and sexual behavior among gay and bisexual men: comparing retrospective and prospective data. Drug Alcohol Depend. 2015;154:199–207. doi: 10.1016/j.drugalcdep.2015.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez T.H., Zlotorzynska M., Rai M., Baral S.D. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav. 2020;24(7):2024–2032. doi: 10.1007/s10461-020-02894-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos G.-M., Ackerman B., Rao A., Wallach S., Ayala G., Lamontage E., Garner A., Holloway I.W., Arreola S., Silenzio V., Strömdahl S., Yu L., Strong C., Adamson T., Yakusik A., Doan T.T., Huang P., Cerasuolo D., Bishop A., Noori T., Pharris A., Aung M., Dara M., Chung S.Y., Hanley M., Baral S., Beyrer C., Howell S. Economic, mental health, HIV prevention and HIV treatment impacts of COVID-19 and the COVID-19 response on a global sample of cisgender gay men and other men who have sex with men. AIDS Behav. 2020:1–11. doi: 10.1007/s10461-020-02969-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler M.S., Stein B.D., Collins R.L. Differences in substance use disparities across age groups in a national cross-sectional survey of lesbian, gay, and bisexual adults. LGBT Health. 2019;6(2):68–76. doi: 10.1089/lgbt.2018.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple S.J., Pitpitan E.V., Goodman-Meza D., Strathdee S.A., Chavarin C.V., Rangel G., Torres K., Patterson T.L. Correlates of condomless anal sex among men who have sex with men (MSM) in Tijuana, Mexico: the role of public sex venues. PLoS One. 2017;12(10) doi: 10.1371/journal.pone.0186814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks T.J., Dellucci T.V., Gupta S., Robles G., Stephenson R., Sullivan P., Parsons J.T. A pilot randomized trial of intervention components addressing drug use in Couples HIV testing and Counseling (CHTC) with male couples. AIDS Behav. 2019:1–14. doi: 10.1007/s10461-019-02455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks T.J., Robles G., Pawson M., Jimenez R.H., Gandhi M., Parsons J.T., Millar B.M. Motivational Interviewing to reduce drug use and HIV incidence among young men who have sex with men in relationships and are high priority for pre-exposure prophylaxis (Project PARTNER): randomized controlled trial protocol. JMIR Res. Protoc. 2019;8(7) doi: 10.2196/13015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart E.A. Matching methods for causal inference: a review and a look forward. Stat. Sci. 2010;25:1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan P.S., Salazar L., Buchbinder S., Sanchez T.H. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease (COVID-19) Situation Report – 172. [Google Scholar]
- Zhang X., Wu L.-T. Marijuana use and sex with multiple partners among lesbian, gay and bisexual youth: results from a national sample. BMC Public Health. 2017;17(1) doi: 10.1186/s12889-016-3905-0. 19–19. [DOI] [PMC free article] [PubMed] [Google Scholar]