Dear Editor
The pandemic due the Coronavirus Disease 2019 (COVID-19) have led to a significant compromise of the healthcare workers (HCW), including those in training attending COVID-19 patients [1,2], especially in developing countries such as Colombia. As previously stated [1] COVID-19 may also present in them with a broad and changing spectrum of clinical disease, including cardiovascular conditions, as is the case of the pericarditis.
The patient, a 25-year-old male, with no past medical history, first-year internal medicine resident attending patients in the emergency department in a reference public tertiary hospital in Bucaramanga, Santander, Northeast Colombia, wearing all personal protective equipment (PPE) and complying the protection policies and procedures implemented in his hospital during the early COVID-19 pandemic.
On July 19, 2020, the physician presented with myalgias, arthralgias and diarrhoea (watery stools, with no blood or mucus, from five to six episodes per day). However, with no fever or respiratory symptoms, he self-medicated with paracetamol and probiotics. On July 21, he additionally presented with fever (38.6 °C) and nausea. The same day reported his clinical condition to the hospital and started home isolation, a nasopharyngeal swab for SARS-CoV-2 test (Logix Smart, IVD/CE/FDA) was done at home. His initial symptoms persisted, the body temperature varied between 38 and 38.6 °C, oxygen saturation >95%, and the myalgias and arthralgias intensified in the following days. On July 25, his RT-PCR test confirmed the viral RNA of SARS-CoV-2.
On the 8th day of home isolation, he reported an intense pleuritic centrothoracic chest pain that improved sitting forward and worsened with supine position and dyspnea at rest (mMRC scale 3) with persistent symptoms. Hence, he presented to the emergency department. On arrival, he was tachycardic and tachypneic with a blood pressure of 153/88 mmHg. Initial oxygen saturation was 97% on room air. The cardiopulmonary examination demonstrated distant heart sounds and decreased breath sounds at the lung bases bilaterally. Firstly, enoxaparin 40 mg subcutaneously and intravenous 6 mg of dexamethasone was administered (off-label).
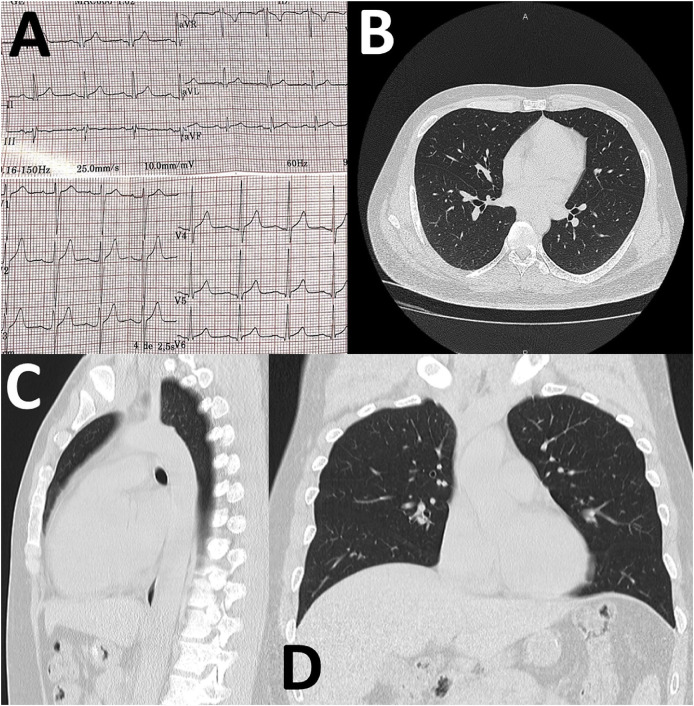
A 12-lead electrocardiogram (EKG) revealed sinus rhythm at 91 bpm with a nonspecific intraventricular conduction delay in DIII and V2 (Fig. 1 ). Laboratory tests showed WBC 6.39 × 103/μL (58% neutrophils; 40% lymphocytes), ferritin 58 ng/ml [normal range, 30−400], LDH 159 IU/L [normal range, 135−250], D-dimer 75 ng/mL [normal range, 0–500], CRP 12 mg/dL [normal range, 0–5], troponin T < 1.5 ng/L [normal range, 0–2], ultrasensitive assay of thyroid-stimulating hormone 0.42 IU/ml [normal range, 0.25–5] and mild metabolic acidemia (pH 7.31, HCO3 20 mmol/L) and serum lactate of 3 mmol/L. The liver and kidney function were within normal values. Testing for human immunodeficiency virus (HIV) antibodies, VDRL and acid-fast bacilli smear and culture were negative.
Fig. 1.
EKG (A) and CT-scan of the thorax (B–D) of the COVID-19 patient showing signs of pericarditis.
Computed tomography of the chest (Fig. 1) showed no alterations in the lung parenchyma. However, a slight pericardial effusion, therefore transthoracic echocardiography was performed confirming the finding of pericardial effusion of approximately 150 mL without signs of early right ventricular diastolic collapse, a normal left ventricular ejection fraction (65%) and LV end-diastolic diameter (47 mm).
With these findings, the diagnosis of acute pericarditis was made, meeting 2 of 4 criteria: pericarditic chest pain and new pericardial effusion. At that moment, treatment was started with colchicine 0.5 mg OD, ibuprofen 800 mg three times daily. During his hospital course, the patient presented severe chest pain that was difficult to relieve, requiring high doses of morphine, with the subsequent change to oxycodone with clinical improvement. After that, lactate levels were normalized, electrocardiograms and serial troponin tests were performed without changes. He was discharged home in stable condition with colchicine 0.5 mg two times daily, ibuprofen 800 mg three times daily and acetaminophen plus codeine with plans for a gradual taper following complete resolution of symptoms.
Colombia is currently on the top ten of countries with the highest cumulative cases of COVID-19, with 590,520 cases (August 28, 2020). Despite the use of PPE by the HCW, including those on training, as the case described, SARS-CoV-2 infection risk is evident, and transmission may occur.
Our case also presented with, a still considered novel, clinical manifestation of COVID-19. Although cardiovascular conditions have been reported widely in COVID-19 so far [3,4], there is a lack of cases presenting with pericarditis, especially without other significant complications.
Multiple viruses can lead to the development of pericarditis [5]. In the case of COVID-19, this consequence requires more detailed studies to understand their pathophysiology, but especially their clinical course and implications. As the pandemic increases, early detection and suspicion of cases, based on broader clinical findings, would be useful, to aid diagnosis, in addition to the confirmation by the rRT-PCR [1,6]. Pericarditis is not frequent in the context of common cold and flu, then, an increase in this finding, in the COVID-19 context, make this case relevant.
Credit author statement
Yeimer Ortiz-Martínez: Conceptualization; Writing - original draft; Writing - review & editing. Luis Daniel Cabeza-Ruiz: Writing - review & editing. Sergio Humberto Vásquez-Lozano: Writing - review & editing. Wilmer E. Villamil-Gómez: Writing - review & editing. Alfonso J. Rodriguez-Morales: Conceptualization; Writing - original draft; Writing - review & editing.
Declaration of competing interest
We declare that we have no competing interests. YOM is the physician case reported in this article.
References
- 1.Ollarves-Carrero M.F., Rodriguez-Morales A.G., Bonilla-Aldana D.K., Rodriguez-Morales A.J. Anosmia in a healthcare worker with COVID-19 in Madrid, Spain. Trav Med Infect Dis. 2020;35:101666. doi: 10.1016/j.tmaid.2020.101666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sommerstein R., Fux C.A., Vuichard-Gysin D., Abbas M., Marschall J., Balmelli C. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. Antimicrob Resist Infect Contr. 2020;9:100. doi: 10.1186/s13756-020-00763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aghagoli G., Gallo Marin B., Soliman L.B., Sellke F.W. Cardiac involvement in COVID-19 patients: risk factors, predictors, and complications: a review. J Card Surg. 2020;35:1302–1305. doi: 10.1111/jocs.14538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutierrez-Ocampo E., Villamizar-Pena R., Holguin-Rivera Y., Escalera-Antezana J.P. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Trav Med Infect Dis. 2020;34:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marschall A., Concepcion Suarez R., Dejuan Bitria C., Fernandez Pascual M.C. Acute pericarditis secondary to COVID-19. Emerge. 2020;32:221–222. [PubMed] [Google Scholar]
- 6.Dhama K., Khan S., Tiwari R., Sircar S., Bhat S., Malik Y.S. Coronavirus disease 2019-COVID-19. Clin Microbiol Rev. 2020:33. doi: 10.1128/CMR.00028-20. [DOI] [PMC free article] [PubMed] [Google Scholar]