This case series assesses a secure teleophthalmology mobile app in military treatment facilities in Afghanistan.
Key Points
Question
Can a mobile phone application be used for teleophthalmology in a combat zone?
Findings
In this case series of 28 consults, military medics and clinicians at forward operating bases in Afghanistan placed teleophthalmology consults on their mobile phone devices and an expeditionary ophthalmologist deployed to a military hospital in Afghanistan responded. Teleophthalmology consultation prevented the need for some aeromedical evacuations and allowed patients to return to duty in 54% of consults.
Meaning
Teleophthalmology mobile phone apps in this environment may improve and extend ophthalmic care.
Abstract
Importance
The coronavirus disease 2019 pandemic has highlighted the need to expand telemedicine solutions.
Objective
To beta test a secure teleophthalmology mobile app at military treatment facilities in Afghanistan.
Design, Setting, and Participants
This prospective case series included 16 military treatment facilities at diverse roles of care including forward operating bases in Afghanistan and 1 location outside of Afghanistan. Thirty point-of-care medics and medical professionals were included from September to November 2019.
Interventions
Users placed teleophthalmology consults on their mobile phone using the mobile eye care app, and an expeditionary ophthalmologist stationed at a military hospital in Afghanistan responded. Users graded the mobile app using a rating scale from 1 to 5, with 1 being very dissatisfied and 5 being very satisfied.
Main Outcomes and Measures
Mean initial response time, agreement between the teleophthalmology diagnosis and final diagnosis, treatment and management following recommendations outlined in the Joint Trauma System clinical practice guidelines, prevention of the need for aeromedical evacuation, user satisfaction, and security and the Health Insurance Portability and Accountability Act compliance of consult.
Results
There were 28 consults placed over 6 weeks by 18 different users that were received by the expeditionary ophthalmologist. The mean (SD) patient age was 30.3 (9.8) years. Most patients were male (26 [93%]) and active duty US military (22 [78%]). The mean initial response time was 3 minutes 58 seconds (95% CI, 2 minutes 30 seconds to 5 minutes 26 seconds). There was agreement between the teleophthalmology diagnosis and final diagnosis in 24 consults (86%; 95% CI, 72%-100%). The treatment and management followed recommendations outlined in the Joint Trauma System Clinical Practice Guidelines for Eye Trauma: Initial Care in 28 consults (100%). Teleophthalmology consultation prevented the need for aeromedical evacuation in 4 consults (14%; 95% CI, 0.7%-28%). The patient returned to duty in 15 consults (54%; 95% CI, 34%-73%). Median overall satisfaction was 5 (minimum, 3; maximum, 5). All 28 consults (100%) were secure and compliant with the Health Insurance Portability and Accountability Act.
Conclusions and Relevance
While only a limited number of consults were evaluated, this study suggests that teleophthalmology mobile phone apps may improve and extend ophthalmic care in combat zones.
Introduction
Ocular trauma and disease are common at forward operating bases in Afghanistan where military personnel have limited communication, no access to ophthalmic care, and few approved and secure options for teleophthalmology. The incidence of combat ocular trauma among US and coalition forces during recent armed conflicts has been reported to be 10% to 15% of all battle injuries.1,2 Disease and nonbattle injury is also a common cause of ocular morbidity among deployed service members, with a reported rate of 3.35% per year.3
There is a need for military teleophthalmology in Afghanistan. During the current North Atlantic Treaty Organization and US missions in Afghanistan, officially named Operation Resolute Support and Operation Freedom’s Sentinel, respectively, the sole coalition ophthalmologist(s) in Afghanistan has been deployed to a single military hospital. In 2019, the expeditionary ophthalmologist at this hospital supported approximately 14 000 US active duty military personnel, 22 000 contractors, 9000 coalition military personnel, and partnered Afghan military and civilian personnel spread across great distances throughout the country.4 US military doctrine deploys and organizes health care support services with progressive capabilities referred to as the 4 roles of care.5 Role 1 provides triage, first aid, and initial resuscitation for trauma. Role 2 provides more advanced trauma management and some surgical capability. Role 3 is a military treatment facility in the theater of operations that provides comprehensive trauma management and subspecialty surgical capability, sometimes including ophthalmology. Role 4 is a military treatment facility outside the theater of operations in the US or overseas with comprehensive trauma and surgical capabilities and is the location for definitive care for US military personnel.
The solutions available for military teleophthalmology are limited, and there are none that use a mobile app. Teleophthalmology in Afghanistan is complicated by many factors, including ongoing combat operations, limited communication capabilities, restricted wireless networking, and the remote geography of the country. Currently, in ocular emergencies or time-sensitive cases, military medics and point-of-care (POC) military medical personnel at role 1 or 2 call and speak directly with physicians at role 3, which may include an ophthalmologist. Communication with an ophthalmologist may be available using a nonsecure or secure telephone, satellite telephone, or cell phone if a wireless network is available. In less time-sensitive cases, web-based teleconsultation systems developed by the Navy, called Health Experts Online Portal or Pacific Asynchronous TeleHealth, are available. Existing commercial teleophthalmology apps would need to meet required security and reliability standards before being granted the authority to operate in the military. Commercial apps that are used for text messaging, voice calls, and video teleconferencing do not have the access or audit controls to be compliant with Health Insurance Portability and Accountability Act (HIPAA) laws.6 With the growth of teleophthalmology and advancements in technology, there is an opportunity to improve the capabilities of teleophthalmology in remote deployed locations.7,8
The primary purpose of this performance improvement (PI) project was to beta test using a secure mobile app called Forward Operating Base Expert Telemedicine Resource Utilizing Mobile Application for Trauma (FOXTROT) to improve and extend ophthalmic care to any deployed location in Afghanistan. The pilot mobile eye care app used the Mobile Health Care Environment–Research system, which was developed by the US Army Medical Research and Development Command Telemedicine and Advanced Technology Research Center. The technology is engineered with security and reliability features to make it suitable for an operational environment with low or no connectivity. The Mobile Health Care Environment–Research system comprises a secure mobile app and a secure clinician portal interface. It can function on most mobile platforms with National Institute of Standards and Technology–certified encryption (FIPS 140-2) for data at rest and in transit. The mobile app functions in both synchronous and asynchronous modes, unlike other cloud-based mobile offerings, which may be dependent on connectivity to operate. To our knowledge, this was the first use of an approved mobile app for teleophthalmology in the US military in a combat zone.
Methods
Approval
This PI project occurred in support of Operation Resolute Support and Operation Freedom’s Sentinel in Afghanistan and at 1 expeditionary medical group outside of Afghanistan in the Middle East from September to November 2019. It was approved as a PI project by the United States Central Command Command Surgeon and reviewed by the US Army Medical Research and Development Command’s Office of Research Protections Institutional Review Board Office and given a determination of not research. This determination exempted the PI project from institutional review board review and waived the requirement for informed consent based on the revised Common Rule criteria.
Users of the App
Any US or coalition military or civilian personnel in the United States Central Command area of responsibility providing medical care at any role of care was eligible to participate including medics, corpsman, physician assistants, and physicians. Users downloaded the mobile eye care app on their cell phone and received an account after review and approval by the expeditionary ophthalmologist. Users were participants in the PI project once they had successfully logged into the app and placed a test consult.
Features of Mobile App
Users at the POC placed new consults in the mobile eye care app by inputting information for response time needed, demographics, history, and examination. Options for response time needed included urgent (response, <1 hour), priority (response, <4 hours), and routine (response, <24 hours) (Figure). Photographs focused by the user on the ocular adnexa, external eye and cornea, and anterior segment could be captured and encrypted within the mobile app software to maintain HIPAA compliance. Users could also include free text of relevant examination information, draw pictures of any critical findings, and check boxes for common examination findings. The mobile app directed users through the steps of inputting data and provided detailed instructions for some steps including visual acuity testing.
Figure. Military Teleophthalmology in Afghanistan Using a Mobile Phone App.
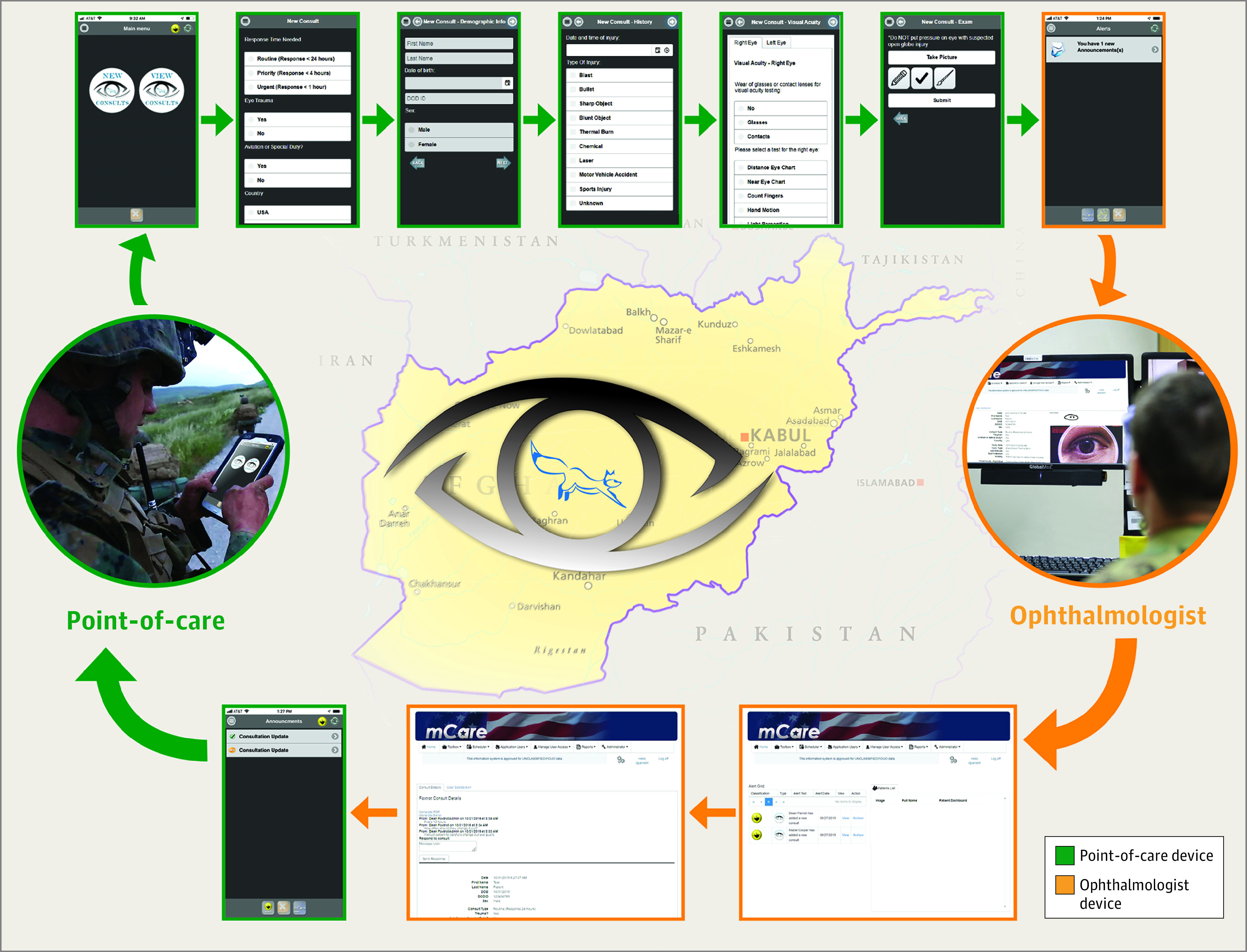
Medical professionals at the point of care placed consults using the mobile eye care application on their telephone, and an expeditionary ophthalmologist at a military hospital in Afghanistan responded by logging into a computer-based portal.
Workflow
The expeditionary ophthalmologist at role 3 was alerted to a new consult by an email notification alert on their cell phone. Teleophthalmology consults were then responded to by logging into a secure computer portal. The teleophthalmology diagnosis, treatment and management plan, need for ophthalmology evaluation, and need for aeromedical evacuation were determined at the time of consult response. Users reviewed the response from the expeditionary ophthalmologist with management recommendations by logging into the mobile app on their cell phone. Users could ask further questions, which were then responded to by the expeditionary ophthalmologist, or close the consult. Once the consult was complete, the user completed a nonvalidated satisfaction survey using a rating scale of 1 to 5, with 1 being very dissatisfied and 5 being very satisfied.
Outcomes
The main outcome measures were mean initial response time, agreement between the teleophthalmology diagnosis and final diagnosis, treatment and management following recommendations outlined in the Joint Trauma System Clinical Practice Guidelines Eye Trauma: Initial Care, prevention of the need for aeromedical evacuation, user satisfaction, and HIPAA compliance of consult.9 If ophthalmology evaluation was recommended, the final diagnosis was determined at the time of an in-person ophthalmic examination. If ophthalmology evaluation was not recommended, the final diagnosis was determined by the expeditionary ophthalmologist based on a review of all follow-up telephone calls with the POC user and/or medical record review using the Theater Medical Data Store and Joint Legacy Viewer during the 30-day period after a consult was closed. It was determined that teleophthalmology consultation prevented aeromedical evacuation if the POC user initially considered aeromedical evacuation for in-person ophthalmology evaluation but the expeditionary ophthalmologist did not recommend aeromedical evacuation and the patient was treated at their current role of care. It was determined that teleophthalmology consultation downgraded the category of aeromedical evacuation precedence if the POC user initially considered either urgent or priority aeromedical evacuation for in-person ophthalmology evaluation but the expeditionary ophthalmologist recommended routine aeromedical evacuation.
Secondary outcomes measures were response within the requested time, visual acuity tested in both eyes, downgraded category of aeromedical evacuation precedence, return to duty rate, and consult record uploaded to medical records. The patient outcome was determined after the mobile eye care app consultation and ophthalmology evaluation, if recommended, was completed. Outcome was categorized as return to duty, restricted duties, quarters, medical redeployment, redeployment in less than 1 month, admission, and surgery (eTable in the Supplement).
Statistical Analysis
For performance indicators and quality benchmarks, 95% CIs were calculated using the t distribution. Median, minimum, and maximum values were reported for the ordinal user satisfaction measures.
Results
Users and Consults
There were 30 users at 16 military treatment facilities in Afghanistan and 1 location outside of Afghanistan in the United States Central Command area of responsibility that were participants. There were 11 users (36.7%) at role 1, 6 users (20.0%) at role 2, and 13 users (43.3%) at role 3. There were an additional 12 potential users who could not participate because of limited or no connectivity and/or firewalls. There were 29 consults placed over 6 weeks by 18 different users. One consult did not synchronize owing to connectivity, so there were 28 consults that were received and responded to by the expeditionary ophthalmologist at role 3.
Patient Demographics and Consult Characteristics
The mean (SD) patient age was 30.3 (9.8) years (Table 1). Most patients were male (26 [93%]) and active duty US military (22 [78%]). The response time requested for the 28 consults received by the expeditionary ophthalmologist was routine (16 [57%]), priority (4 [14%]), and urgent (8 [29%]). The consult was for trauma in 5 cases (18%) and did not involve trauma in 23 cases (82%). The role of care where the consult was placed was role 1 (7 [24%]), role 2 (8 [28%]), and role 3 (14 [48%]).
Table 1. Demographics and Characteristics of the 28 Consults Received by the Expeditionary Ophthalmologist.
| Patient and consult characteristic | No. (%) |
|---|---|
| Age, mean (SD), y | 30.3 (9.8) |
| Sex | |
| Male | 26 (93) |
| Female | 2 (7) |
| Country | |
| US | 25 (89) |
| Coalition | 1 (4) |
| Afghanistan | 2 (7) |
| Category | |
| US military: active duty | |
| Not aviation or special duty | 13 (46) |
| Aviation | 6 (21) |
| Special duty | 3 (11) |
| US government or contractor | 3 (11) |
| Coalition military | 1 (4) |
| Afghanistan military | 1 (4) |
| Afghanistan civilian | 1 (4) |
| Response time requested | |
| Routine (response, <24 h) | 16 (57) |
| Priority (response, <4 h) | 4 (14) |
| Urgent (response, <1 h) | 8 (29) |
| Eye trauma | |
| Yes | 5 (18) |
| No | 23 (82) |
| Role of care | |
| 1 | 7 (24) |
| 2 | 8 (28) |
| 3 | 14 (48) |
Chief Complaint, Diagnosis, and Outcomes
The most common chief complaint was red eye with or without pain (10 [36%]) and trauma (5 [18%]) (Table 2). Disease and nonbattle injury (22 [79%]) was more common than battle injury (6 [21%]). The teleophthalmology diagnosis was external disease and cornea (14 [50%]), uveitis (2 [7%]), retina and vitreous (5 [18%]), neuro-ophthalmology (3 [11%]), strabismus (1 [4%]), and orbit and eyelids (3 [11%]). Ophthalmology evaluation was recommended for 17 consults (61%; 95% CI, 42%-80%). The final diagnosis was external disease and cornea (12 [43%]), uveitis (5 [18%]), retina and vitreous (4 [14%]), neuro-ophthalmology (3 [11%]), strabismus (1 [4%]), and orbit and eyelids (3 [11%]).
Table 2. Summary of Mobile Eye Care Teleophthalmology Consultations.
| Consult No. | Chief complaint | Causea | Teleophthalmology diagnosisb | Ophthalmology evaluation recommended | Aeromedical evacuationc | Final diagnosisd | Outcomee |
|---|---|---|---|---|---|---|---|
| 1 | Eye pain/discomfort | DNBI | Dry eye disease | No | No | Dry eye disease | Return to duty |
| 2 | Vision loss | DNBI | Migraine with aura | Yes | No | Migraine with aura | Return to duty |
| 3 | Red eye (with pain) | DNBI | Conjunctivitis | No | No | Conjunctivitis | Return to duty |
| 4 | Trauma | DNBI | Orbital wall fracture | Yes | Downgraded to routine | Orbital wall fracture | Restricted duties |
| 5 | Eye lesion | DNBI | Pinguecula | No | No | Pinguecula | Return to duty |
| 6 | Red eye (with pain) | DNBI | Conjunctivitis | No | Prevented | Conjunctivitis | Restricted duties |
| 7 | Trauma | BI | Corneal abrasion | No | No | Corneal abrasion | Quarters |
| 8 | Vision loss | DNBI | Migraine with aura | Yes | No | Migraine with aura | Medical redeployment |
| 9 | Eye drifting | DNBI | Intermittent exotropia | Yes | Prevented | Intermittent exotropia | Redeployment as scheduled <1 mo |
| 10 | Red eye (with pain) | DNBI | Corneal abrasion | No | Prevented | Corneal abrasion | Restricted duties |
| 11 | Eyelid pain/swelling | DNBI | Chalazion | No | No | Chalazion | Return to duty |
| 12 | Red eye (with pain) | DNBI | Corneal abrasion | No | No | Corneal abrasion | Return to duty |
| 13 | Red eye (with pain) | DNBI | Herpetic keratitis | Yes | No | Iritis | Quarters |
| 14 | Foreign body in eye | DNBI | Conjunctival foreign body | Yes | No | Conjunctival foreign body | Return to duty |
| 15 | Red eye (with pain) | DNBI | Corneal abrasion | Yes | No | Corneal abrasion | Return to duty |
| 16 | Red eye (with pain) | DNBI | Episcleritis | Yes | No | Episcleritis | Return to duty |
| 17 | Floaters | DNBI | Vitreous opacities | Yes | Downgraded to routine | Intermediate uveitis | Redeployment as scheduled <1 mo |
| 18 | Discharge and itching | DNBI | Conjunctivitis | Yes | Downgraded to routine | CSR | Return to duty |
| 19 | Trauma | BI | Eyelid contusion | No | Prevented | Eyelid contusion | Admitted |
| 20 | Optic disc drusen | DNBI | Optic disc drusen | No | No | Optic disc drusen | Return to duty |
| 21 | Trauma | BI | Eyelid laceration | Yes | Downgraded to routine | Eyelid laceration | Surgery |
| 22 | Red eye (no pain) | DNBI | Conjunctivitis | No | No | Iritis | Quarters |
| 23 | Blind spot | DNBI | CSR | Yes | No | CSR | Return to duty |
| 24 | Trauma | BI | Open globe | Yes | Urgent | Open globe | Surgery |
| 25 | Red eye (with pain) | DNBI | Iritis | Yes | No | Iritis | Quarters |
| 26 | Red eye (no pain) | DNBI | Dry eye disease | Yes | No | Dry eye disease | Return to duty |
| 27 | Laser exposure | BI | Laser exposure | Yes | No | Laser exposure | Return to duty |
| 28 | Laser exposure | BI | Laser retinal injury | Yes | No | Laser retinal injury | Return to duty |
Abbreviations: BI, battle injury; CSR, central serous chorioretinopathy; DNBI, disease and nonbattle injury; POC, point of care.
Cause of injury was categorized as BI or DNBI.
Teleophthalmology diagnosis was determined by the expeditionary ophthalmologist at the time of response to the consultation.
In-theater aeromedical evacuation for ophthalmology evaluation was required for some consults when the patient was located at another base. It was determined that teleophthalmology consultation prevented aeromedical evacuation if the POC user initially considered aeromedical evacuation for in-person ophthalmology evaluation but the expeditionary ophthalmologist did not recommend aeromedical evacuation and the patient was treated at their current role of care. It was determined that teleophthalmology consultation downgraded the category of aeromedical evacuation precedence if the POC user initially considered either urgent or priority aeromedical evacuation for in-person ophthalmology evaluation but the expeditionary ophthalmologist recommended routine aeromedical evacuation.
If ophthalmology evaluation was recommended, the final diagnosis was determined at the time of an in-person ophthalmic examination. If ophthalmology evaluation was not recommended, the final diagnosis was determined by the expeditionary ophthalmologist based on a review of all follow-up telephone calls with the POC user and/or medical record review using the Theater Medical Data Store and Joint Legacy Viewer during the 30-day period after a consult was closed.
Outcome determined after teleophthalmology mobile phone consultation and ophthalmology evaluation if recommended. Return to duty indicates no restrictions. Restricted duty indicates restrictions from performing certain duties or activities due to an illness or injury. Quarters indicates excusal from duty for a period of more than 24 hours to a maximum of 14 days due to an illness or injury that did not require hospitalization. Medical redeployment indicates redeployment to home station due to illness or injury. Redeployment in less than 1 month indicates member already scheduled to redeploy to home station so medical redeployment not recommended and the patient will follow-up as recommended when returns home. Admission indicates admission to a hospital and surgery indicates that a surgical procedure was performed.
Performance Indicators and Quality Benchmarks
The mean initial response time was 3 minutes 58 seconds (95% CI, 2 minutes 30 seconds to 5 minutes 26 seconds) (Table 3). All 28 consults (100%) were responded to within the requested time. Visual acuity was tested in both eyes in 18 consults (64%; 95% CI, 46%-83%). The treatment and management followed recommendations outlined in the Joint Trauma System Clinical Practice Guidelines Eye Trauma: Initial Care in 28 consults (100%). Teleophthalmology consultation prevented the need for aeromedical evacuation in 4 consults (14%; 95% CI, 0.7%-28%) and downgraded the category of precedence from urgent or priority to routine in 4 consults (14%; 95% CI, 0.7%-28%). The patient returned to duty in 15 consults (54%; 95% CI, 34%-73%). The consult record was uploaded in the Theater Medical Data Store medical record in 27 consults (96%; 95% CI, 89%-100%). All 28 consults (100%) were secure and HIPAA compliant. There was agreement between the teleophthalmology diagnosis and final diagnosis in 28 consults (86%; 95% CI, 72%-100%). In 3 cases where there was a disagreement, an ophthalmology evaluation was recommended because the diagnosis was uncertain based on teleophthalmology consultation alone. The user satisfaction survey was completed for 28 of 28 consults (100%). Median satisfaction was 5 (minimum, 3; maximum, 5), median satisfaction with ease of use was 5 (minimum, 3; maximum, 5), median satisfaction with the treatment and management plan was 5 (minimum, 4; maximum, 5), and median satisfaction compared with other teleophthalmology methods was 5 (minimum, 3; maximum, 5).
Table 3. Performance Indicators and Quality Benchmarks for Teleophthalmology Mobile Eye Care Consultations.
| Performance indicator or quality benchmarka | No. (%) [95% CI] |
|---|---|
| Initial response time, mean (95% CI), min:s | 3:58 (2:30-5:26) |
| Response within requested time, No. (%) | 28 (100) |
| Visual acuity tested in both eyes | 18 (64) [46-83] |
| Agreement teleophthalmology diagnosis and final diagnosisb | 24 (86) [72-99] |
| Treatment and management followed JTS CPG, No. (%)c | 28 (100) |
| Prevented need for aeromedical evacuation | 4 (14) [0.7-28] |
| Downgraded category of aeromedical evacuation precedence | 4 (14) [0.7-28] |
| Return to duty | 15 (54) [34-73] |
| Consult record uploaded to medical recordd | 27 (96) [89-100] |
| Consult secure and HIPAA compliant, No. (%) | 28 (100) |
| User satisfaction, median (range)e | |
| Overall | 5 (3-5) |
| With ease of use | 5 (3-5) |
| With the treatment and management plan | 5 (4-5) |
| Compared with other teleophthalmology methodsf | 5 (3-5) |
Abbreviations: CPG, clinical practice guidelines; HIPAA, Health Insurance Portability and Accountability Act; JTS, Joint Trauma System.
Analysis based on total of 28 new consults received by the expeditionary ophthalmologist.
There were 4 cases with disagreement between the teleophthalmology diagnosis and final diagnosis. In 3 of those cases, an ophthalmology evaluation was recommended because the diagnosis was uncertain based on teleophthalmology consultation alone.
For each consult, it was determined if treatment and management followed recommendations outlined in the JTS CPG Eye Trauma: Initial Care.
In 1 consult, the patient was not able to be located in the medical record using name, date of birth, or Department of Defense Identification Number so the mobile eye care app consultation could not be uploaded to the medical record.
Users graded their satisfaction with the mobile eye care app using a rating scale of 1 to 5, with 1 being very dissatisfied and 5 being very satisfied. The survey was completed for 28 of 28 consults.
Satisfaction with the mobile eye care app compared with previous ophthalmology consults user has placed using other methods such as telephone, email, or pager.
Discussion
Teleophthalmology has advanced for diabetic retinopathy screening and macular degeneration, but the literature is limited for its applications in trauma and emergency medicine.7,10,11,12,13 The focus of this mobile app on trauma and disease and nonbattle injury is novel, to our knowledge, in teleophthalmology. This project demonstrated that a teleophthalmology mobile app was associated with improved and extended ophthalmic care in an operational environment. Use of a mobile app was associated with agreement between the teleophthalmology diagnosis and final diagnosis in 86% (95% CI, 72%-100%) of consults. The treatment and management followed recommendations outlined in the Joint Trauma System clinical practice guidelines in all consults. User satisfaction with a nonvalidated survey was relatively high, with the median overall score of 5 (minimum, 3; maximum, 5). The positive return on investment and cost savings from prevented aeromedical evacuation has previously been reported in military telemedicine.14 The mobile eye care app prevented the need for aeromedical evacuation in 4 consults (14%; 95% CI, 0.7%-28%) and downgraded the category of precedence from urgent or priority to routine in 4 consults (14%; 95% CI, 0.7%-28%).
A mobile app has potential advantages in convenience and response time over other asynchronous telemedicine options such as email or a web-based portal. The reported average response times for military telemedicine programs using email, which have been retired because they could not transmit identifiable patient health information, were 5 hours and 41 minutes for ophthalmology and 7 hours 32 minutes for orthopaedics.15,16 The mobile eye care app immediately sent out an alert to the expeditionary ophthalmologist’s cell phone when a new consult was placed, allowing for a more timely response of 3 minutes and 58 seconds (95% CI, 2 minutes 30 seconds to 5 minutes 26 seconds).
To guide the future development of mobile apps for operational telemedicine and teleophthalmology in the military, we propose 4 development principles based on the results of the mobile eye care app beta testing: new technology should be secure, simple, reliable, and human (Table 4). This mobile eye care app was secure and HIPAA compliant in all consults. Future mobile apps should also provide data security, end-to-end encryption, and HIPAA compliance. Photographs with identifiable patient health information taken on a cell phone and stored in an unsecure location such as a photo album or cloud without additional security are not HIPAA compliant.17 This mobile eye care app allowed images to be captured and encrypted within the mobile software application directly and was HIPAA compliant.
Table 4. Proposed Development Principles and Potential Solutions for Mobile Phone Apps Engineered for Military Teleophthalmology.
| Development principle | Potential solutions |
|---|---|
| Secure |
|
| Simple |
|
| Reliable |
|
| Human |
|
Abbreviation: HIPAA, Health Insurance Portability and Accountability Act.
Operational telemedicine technology should be simple and easy to set up and use. Input of demographic information could be automated using identification card scanning. Anterior and posterior segment photographs could be automated using focusing technology integrated into a mobile device or adaptors attached to a mobile device. An integrated examination toolbox could provide users with routine or advanced examination or diagnostic testing. Artificial intelligence including image processing tools could check the accuracy of data input and provide users with diagnostic support and treatment recommendations.
Reliability of teleophthalmology devices is perceived by the authors to be important, and one of the greatest obstacles for expeditionary mobile phone application technology is connectivity and firewalls in the operational environment. In this project, there were 12 potential users who were unable to use this mobile eye care app because of limited or no connectivity and/or firewalls. Future mobile app development might consider engineering technology with firewall solutions that maintain security and are recognized by the entire US Department of Defense network spectrum. Denied, degraded, or disrupted communication environments are likely in future conflicts and therefore apps need to consider engineering to meet anti-access and area denial challenges. In some instances, especially at remote forward operating bases or ships at sea, there is no wireless connectivity or synchronous capability. Therefore, asynchronous solutions that use minimal bandwidth when it is available are needed. It is also possible that mobile apps could integrate with existing military communication systems such as nonsecure or secure telephone, satellite telephone, or tactical chat.
Beta testing for this mobile eye care app demonstrated that telemedicine is complex, and it may not always be possible to make the correct diagnosis or guide management through remote communication alone. There was agreement between the teleophthalmology diagnosis and final diagnosis in 86% (95% CI, 72%-100%) of consults but ophthalmology evaluation was required in 61% (95% CI, 42%-80%) of consults. The history and examination gathered through a teleophthalmology consult may not be as accurate, detailed, or comprehensive as that obtained from an ophthalmology evaluation. There are certain examination or diagnostic tests unavailable to POC users that can only be provided by a subspecialty evaluation. Therefore, direct follow-up with a clinician ideally should be possible with pathways to arrange referrals that are built into mobile apps.
Limitations
There are several limitations to this study. It occurred during a limited period of time in a deployed military setting on a proprietary military teleophthalmology platform with 1 expeditionary ophthalmologist responding to a limited number of consults. The results of this project may not be generalizable to how this mobile eye care app would perform in a larger population of military or civilian patients, users, and ophthalmologists. Ophthalmology evaluation was not recommended in 39% (95% CI, 20%-58%) of consults, so the final diagnosis determined from a review of all follow-up telephone calls and patient records may not be as accurate as a diagnosis from an in-person examination. The user satisfaction survey was nonvalidated, which may limit the interpretation of user satisfaction scores.
Conclusions
There may be other potential military and civilian applications for this technology and the current coronavirus disease 2019 pandemic has highlighted the need to expand telemedicine solutions. Teleophthalmology mobile phone apps can be used for virtual screening, examination, and treatment of patients during an infectious disease outbreak. Remote consultations might help patients access care while decreasing in-person visits to protect patients and health care workers. This technology might also have applications in other remote settings with limited connectivity such as cruise ships, ski resorts, wilderness trips, or international travel. It could also be used to extend ophthalmic coverage to any hospital, emergency department, urgent care clinic, outpatient medical clinic, or optometry office without an in-house ophthalmologist. The future of teleophthalmology appears to have the potential to improve and extend care in many military and civilian environments.
eTable. Patient Outcomes
References
- 1.Weichel ED, Colyer MH, Ludlow SE, Bower KS, Eiseman AS. Combat ocular trauma visual outcomes during operations Iraqi and enduring freedom. Ophthalmology. 2008;115(12):2235-2245. doi: 10.1016/j.ophtha.2008.08.033 [DOI] [PubMed] [Google Scholar]
- 2.Blanch RJ, Bindra MS, Jacks AS, Scott RAH. Ophthalmic injuries in British Armed Forces in Iraq and Afghanistan. Eye (Lond). 2011;25(2):218-223. doi: 10.1038/eye.2010.190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blanch RJ, Kerber MT, Gensheimer WG. Deployed ophthalmic workload in support of US and NATO operations in Afghanistan. BMJ Mil Health. Published online March 5, 2020. doi: 10.1136/bmjmilitary-2019-001379 [DOI] [PubMed] [Google Scholar]
- 4.U.S. Central Command. Resolute support. Accessed March 17, 2020. https://www.centcom.mil/OPERATIONS-AND-EXERCISES/RESOLUTE-SUPPORT/
- 5.Roles of medical care (United States) In: Emergency War Surgery. 5th ed Office of The Surgeon General; 2018:19-22. https://www.cs.amedd.army.mil/FileDownloadpublic.aspx?docid=6f9e0685-1290-4e92-8277-c1e7b0f2fef0 [Google Scholar]
- 6.U.S. Department of Health & Human Services. The security rule. Published September 10, 2009. Accessed June 6, 2020. https://www.hhs.gov/hipaa/for-professionals/security/index.html
- 7.Rathi S, Tsui E, Mehta N, Zahid S, Schuman JS. The current state of teleophthalmology in the United States. Ophthalmology. 2017;124(12):1729-1734. doi: 10.1016/j.ophtha.2017.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Academy of Ophthalmology. Telemedicine for ophthalmology information statement: 2018. Published February 22, 2018. Accessed November 3, 2019. https://www.aao.org/clinical-statement/telemedicine-ophthalmology-information-statement
- 9.Gensheimer WG, Mazzoli R, Reynolds M, et al. Joint Trauma System Clinical Practice Guideline (JTS CPG): eye trauma: initial care (CPG ID:03). Published August 2019. Accessed October 30, 2019. https://jts.amedd.army.mil/assets/docs/cpgs/JTS_Clinical_Practice_Guidelines_(CPGs)/Eye_Trauma_Initial_Care_28_Aug_2019_ID03.pdfhttps://jts.amedd.army.mil/assets/docs/cpgs/JTS_Clinical_Practice_Guidelines_(CPGs)/Eye_Trauma_Initial_Care_28_Aug_2019_ID03.pdf
- 10.Boucher MC, Desroches G, Garcia-Salinas R, et al. Teleophthalmology screening for diabetic retinopathy through mobile imaging units within Canada. Can J Ophthalmol. 2008;43(6):658-668. doi: 10.3129/i08-120 [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Torres Diaz A, Benkert R. Scaling up teleophthalmology for diabetic eye screening: opportunities for widespread implementation in the USA. Curr Diab Rep. 2019;19(9):74. doi: 10.1007/s11892-019-1187-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaziri K, Moshfeghi DM, Moshfeghi AA. Feasibility of telemedicine in detecting diabetic retinopathy and age-related macular degeneration. Semin Ophthalmol. 2015;30(2):81-95. doi: 10.3109/08820538.2013.825727 [DOI] [PubMed] [Google Scholar]
- 13.Sharafeldin N, Kawaguchi A, Sundaram A, et al. Review of economic evaluations of teleophthalmology as a screening strategy for chronic eye disease in adults. Br J Ophthalmol. 2018;102(11):1485-1491. doi: 10.1136/bjophthalmol-2017-311452 [DOI] [PubMed] [Google Scholar]
- 14.Lin AH, Welstead BL, Morey BL, Mahnke CB, Cole JH, Johnston MG. Return on investment analysis of health experts online at Portsmouth: a 2-year review of the navy’s newest teleconsultation system. Mil Med. 2017;182(5):e1696-e1701. doi: 10.7205/MILMED-D-16-00259 [DOI] [PubMed] [Google Scholar]
- 15.Mines MJ, Bower KS, Lappan CM, Mazzoli RA, Poropatich RK. The United States Army Ocular Teleconsultation program 2004 through 2009. Am J Ophthalmol. 2011;152(1):126-132.e2. doi: 10.1016/j.ajo.2011.01.028 [DOI] [PubMed] [Google Scholar]
- 16.Waterman BR, Laughlin MD, Belmont PJ Jr, Schoenfeld AJ, Pallis MP. Enhanced casualty care from a Global Military Orthopaedic Teleconsultation Program. Injury. 2014;45(11):1736-1740. doi: 10.1016/j.injury.2014.03.012 [DOI] [PubMed] [Google Scholar]
- 17.Reynolds RA, Stack LB, Bonfield CM. Medical photography with a mobile phone: useful techniques, and what neurosurgeons need to know about HIPAA compliance. J Neurosurg. 2019;132(1):260-264. doi: 10.3171/2018.8.JNS182075 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Patient Outcomes


