Abstract
The separation of the vitreous from the optic nerve head and the macula plays a primary role in the spontaneous resolution of optic disc pit (ODP) maculopathy. Optical coherence tomography (OCT) helps in the non-invasive monitoring of this condition, when treated conservatively. The aim of this report was to describe a pediatric case of spontaneously resolved ODP maculopathy, managed conservatively and monitored by means of spectral domain (SD)-OCT. A 14-year-old girl presented with severe visual loss in the right eye (RE). Fundus examination demonstrated a temporal ODP with altered foveal reflex. The SD-OCT B-scans revealed severe intraretinal schisis-like changes, broad vitreal adhesion in the optic nerve head area, posterior hyaloid thickening, and vitreal entrapment in the premacular space. The patient was managed conservatively. Spontaneous resolution of ODP maculopathy took place over 3 months, with vision improved up to 1.0 (Snellen charts). The macular schisis progressively resolved after posterior vitreous detachment. In conclusion, in our report, a complete restoration of the foveal anatomy was achieved without any surgical intervention. This OCT-based report confirms the role of the vitreomacular abnormalities in the pathogenesis of the disease.
Keywords: optic disc pit maculopathy, optical coherence tomography, posterior vitreous detachment
Introduction
First described in 1882, optic disc pit (ODP) is a rare congenital malformation of the optic disc, secondary to a failure in the closure of the superior edge of the embryonic fissure during embryogenesis.1,2 ODP usually remains asymptomatic unless associated with ODP maculopathy, which presents as macular edema, macular schisis, or serous detachment.3,4 Although the exact pathogenesis of ODP maculopathy is not known, different theories about the source of fluid responsible of the above-mentioned macular changes have been proposed, according to which it may be secondary to vitreous penetration in the subretinal space, or to a direct connection between the subarachnoidal and the subretinal or intraretinal space.5,6 Regardless the most likely explanation, vitreous traction appears to be an important factor in the pathogenesis of ODP maculopathy.7,8
We describe a pediatric case of spontaneously resolved ODP maculopathy, in which the role of vitreous traction is emphasized and documented by means of spectral domain–optical coherence tomography (SD-OCT). No identifiable health information was included in this case report.
Case
A 14-year-old girl presented to our department with a 2-week history of severe visual loss in her right eye (RE). Her medical history, as well as her family history, was negative for any macular disorders. Moreover, she did not have any ocular history of previous surgeries and/or treatments. On examination, her best-corrected visual acuity (BCVA) measured with Snellen chart was 0.1 in the RE and 1.0 in the left eye. Intraocular pressure was 14 mmHg in both eyes. The anterior segment examination was unremarkable, while fundus examination demonstrated a temporal ODP (approximate measure of 750 µm) with an altered foveal reflex in the RE. The visual field measured on automated perimetry showed an enlarged blind spot and a central arcuate scotoma in the RE. The SD-OCT B-scans of the macular region revealed a reduced foveal thickness; intraretinal schisis-like changes between the outer nuclear layer and the outer plexiform layer; a broad vitreal adhesion in the optic nerve head area; a diffuse parafoveal vitreomacular traction due to a posterior hyaloid thickening, with significant neuroretinal distortion; and vitreal entrapment in the premacular space (Figure 1(a)). Subfoveal focal interruption of the inner segment–outer segment (IS-OS) band and a defect of the lamina cribrosa at the site of the ODP were also discernible on the tomographic scan. Considering the age of the patient, we decided to observe the clinical course of the disease. Over the next 3 months, the vision of the RE dramatically improved until a BCVA of 1.0, and the macular schisis progressively resolved and spontaneous posterior vitreous detachment from the optic nerve head was noted (Figure 1(b)). The macular anatomy, including the IS-OS band, was perfectly restored (Figure 1(c)). The patient did not undergo ocular interventions during the follow-up period.
Figure 1.
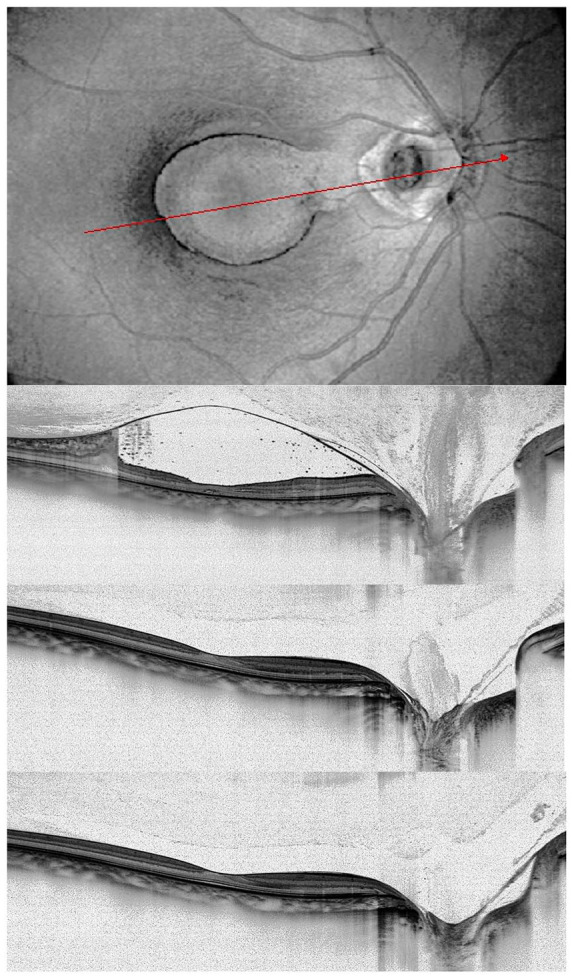
Progressive optical coherence tomography (OCT) of a case of optic disc pit maculopathy, with spontaneous resolution after posterior vitreous detachment.
(a) En-face reconstruction of the posterior pole, showing a round-shaped defect nasally to the optic disc, corresponding to the optic disc pit. The horizontal OCT passing through the fovea (red arrow) showed a reduced foveal thickness, schisis-like changes, a broad vitreal adhesion in the optic nerve head area, a posterior hyaloid thickening, vitreal entrapment in the premacular space, and a focal subfoveal defect in the photoreceptor layer. (b) The horizontal OCT in the same position showed resolution of the vitreomacular traction and the weakening of the vitreal adhesion on the optic nerve head. (c), [d] The OCT scans at the last follow-up visit showed a completely released vitreal adhesion on the optic nerve head and a full restoration in the photoreceptor band subfoveally.
Discussion
Many interventions have been considered for the treatment of ODP maculopathy, with no consensus regarding the approach which maximizes the surgical success and minimizes the side effects and the potential complications. Laser photocoagulation,9 vitrectomy with internal limiting membrane peeling,10,11 macular buckling,12 gas,13 or silicone tamponade14 have all been demonstrated to be beneficial in restoring macular anatomy and function, with long-lasting results. As well, cases of spontaneous resolution of ODP maculopathy have been described in the literature.
Regardless of the surgical technique adopted, recent evidences have shown that a separation of the vitreous from the optic nerve head and the macula plays a primary role in the resolution of the disease.15 Our report clearly depicts the vitreal changes in the peripapillary and in the macular region, from broad adhesion to complete posterior detachment, reinforcing this theory. Indeed, albeit rare, other similar examples of spontaneous resolution of ODP maculopathy have been described in the literature, all featuring a relief of the vitreomacular traction forces in the macular region.16–19 Novelty of this report is the progressive OCT-based documentation of this process.
Of note, we assisted to the complete restoration of the foveal anatomy, with no consequences on the outermost retinal layers and on the final visual acuity.
In conclusion, this report confirms the possibility of spontaneous resolution of the ODP maculopathy in pediatric patients, giving deeper insights on the role of the vitreomacular abnormalities in the pathogenesis of the disease. A wait-and-watch approach may be a valuable option in pediatric patients.
Footnotes
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethics statement: Approval by an ethical committee was not required since this was a retrospective observational case presentation. Written informed consent was obtained from patient’s parents for future retrospective use and publication of her data.
ORCID iD: Giuseppe Querques  https://orcid.org/0000-0002-3292-9581
https://orcid.org/0000-0002-3292-9581
Contributor Information
Massimo Lorusso, Department of Ophthalmology, Ente Ecclesiastico Ospedale Generale Regionale ‘F, Miulli’, Bari, Italy.
Roberta Zito, Department of Ophthalmology, Ente Ecclesiastico Ospedale Generale Regionale ‘F, Miulli’, Bari, Italy.
Luisa Micelli Ferrari, Department of Ophthalmology, Ente Ecclesiastico Ospedale Generale Regionale ‘F, Miulli’, Bari, Italy.
Eleni Nikolopoulou, Department of Ophthalmology, Ente Ecclesiastico Ospedale Generale Regionale ‘F, Miulli’, Bari, Italy.
Maria Vittoria Cicinelli, Department of Ophthalmology, University Vita-Salute, IRCCS Ospedale San Raffaele, Milan, Italy.
Enrico Borrelli, Department of Ophthalmology, University Vita-Salute, IRCCS Ospedale San Raffaele, Milan, Italy.
Giuseppe Querques, Department of Ophthalmology, University Vita-Salute, IRCCS Ospedale San Raffaele, Via Olgettina 60, 20132 Milan, Italy.
Tommaso Micelli Ferrari, Department of Ophthalmology, Ente Ecclesiastico Ospedale Generale Regionale ‘F, Miulli’, Bari, Italy.
References
- 1. Georgalas I, Ladas I, Georgopoulos G, et al. Optic disc pit: a review. Graefes Arch Clin Exp Ophthalmol 2011; 249: 1113–1122. [DOI] [PubMed] [Google Scholar]
- 2. Shah SD, Yee KK, Fortun JA, et al. Optic disc pit maculopathy: a review and update on imaging and treatment. Int Ophthalmol Clin 2014; 54: 61–78. [DOI] [PubMed] [Google Scholar]
- 3. Regenbogen L, Stein R, Lazar M. Macular and juxtapapillar serous retinal detachment associated with pit of optic disc. Ophthalmologica 1964; 148: 247–251. [DOI] [PubMed] [Google Scholar]
- 4. Theodossiadis GP, Koutsandrea C, Theodossiadis PG. Optic nerve pit with serous macular detachment resulting in rhegmatogenous retinal detachment. Br J Ophthalmol 1993; 77: 385–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moisseiev E, Moisseiev J, Loewenstein A. Optic disc pit maculopathy: when and how to treat? A review of the pathogenesis and treatment options. Int J Retina Vitreous 2015; 1: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gowdar JP, Rajesh B, Giridhar A, et al. An insight into the pathogenesis of optic disc pit-associated maculopathy with enhanced depth imaging. JAMA Ophthalmol 2015; 133: 466–469. [DOI] [PubMed] [Google Scholar]
- 7. Theodossiadis PG, Grigoropoulos VG, Emfietzoglou J, et al. Vitreous findings in optic disc pit maculopathy based on optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 2007; 245: 1311–1318. [DOI] [PubMed] [Google Scholar]
- 8. Joko T, Kusaka S. Tangential vitreous traction observed in optic disc pit maculopathy without apparent serous detachment. Ophthalmic Surg Lasers 1998; 29: 677–679. [PubMed] [Google Scholar]
- 9. Nebbioso M, Dapoto L, Lenarduzzi F, et al. Preliminary study on combined pharmacological and laser treatment in optic pit serous maculopathy after literature review. Panminerva Med 2012; 54: 59–66. [PubMed] [Google Scholar]
- 10. Dai S, Polkinghorne P. Peeling the internal limiting membrane in serous macular detachment associated with congenital optic disc pit. Clin Exp Ophthalmol 2003; 31: 272–275. [DOI] [PubMed] [Google Scholar]
- 11. Cevher S, Sahinoglu-Keskek N, Unal F, et al. Serous macular detachment secondary to optic pit: surgical treatment and long time results. Case Rep Ophthalmol Med 2016; 2016: 4567840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Theodossiadis GP, Chatziralli IP, Theodossiadis PG. Macular buckling in optic disc pit maculopathy in association with the origin of macular elevation: 13-year mean postoperative results. Eur J Ophthalmol 2015; 25: 241–248. [DOI] [PubMed] [Google Scholar]
- 13. Teke MY, Citirik M. 23 gauge vitrectomy, endolaser, and gas tamponade versus vitrectomy alone for serous macular detachment associated with optic disc pit. Am J Ophthalmol 2015; 160: 779–785. [DOI] [PubMed] [Google Scholar]
- 14. Fantaguzzi PM, Vasco A. Vitrectomy and silicone oil tamponade for serous macular detachment associated with an optic disk pit. Eur J Ophthalmol 2006; 16: 330–334. [DOI] [PubMed] [Google Scholar]
- 15. Rayat JS, Rudnisky CJ, Waite C, et al. Long-term outcomes for optic disk pit maculopathy after vitrectomy. Retina 2015; 35: 2011–2017. [DOI] [PubMed] [Google Scholar]
- 16. Akça Bayar S, Sarıgül Sezenöz A, Yaman Pınarcı E, et al. Spontaneous regression of optic disc pit maculopathy in a six-year-old child. Turk J Ophthalmol 2017; 47: 56–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yuen CH, Kaye SB. Spontaneous resolution of serous maculopathy associated with optic disc pit in a child: a case report. J AAPOS 2002; 6: 330–331. [DOI] [PubMed] [Google Scholar]
- 18. Parikakis EA, Chatziralli IP, Peponis VG, et al. Spontaneous resolution of long-standing macular detachment due to optic disc pit with significant visual improvement. Case Rep Ophthalmol 2014; 5: 104–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gupta RR, Choudhry N. Spontaneous resolution of optic disc pit maculopathy after posterior vitreous detachment. Can J Ophthalmol 2016; 51: e24–e27. [DOI] [PubMed] [Google Scholar]


