Abstract
Background:
Patient reported outcome measures (PROMs) are becoming well recognized as an important component of health care outcomes and determinants of value in patient-centered care. Yet, there is emerging recognition that guidance is lacking in the utilization of PROMs in hip fracture patients. The aim of this study was to collect input from hip fracture patients and their health care advocates as proxies to identify outcomes that are important and to gain insight into which ones are of greatest importance.
Methods:
A cross-section of patients aged 65 and older treated for hip fractures at a single level 1 trauma center within the previous 3 to 9 months was identified. Semistructured telephone interviews of patients and/or health care proxies were performed in 2 phases: (1) concept identification and conceptual framework development and (2) item generation and assessment of relative importance of health care outcomes. Each phase was completed by separate patient cohorts.
Results:
Sixty-four interviews were completed. Eighteen interviews with 13 patients and 5 proxies were completed for framework development. Forty-six interviews with 33 patients and 13 proxies were completed for the assessment of relative importance. Care team and communication were reported as important in hip fracture patients. Physical outcomes were ranked as most important by only 9% of respondents. “Having confidence that I/my loved one received the best care possible” was perceived as very important by 98% of respondents and “Having access to the surgeon” was perceived as very important by 76% of the respondents.
Conclusions:
In our study, communication between patients and care providers as well as collaboration among patients’ care providers ranked as the most important postoperative preferences in our cohort. Notably, physical outcomes were ranked as most important by only 9% of respondents.
Keywords: patient reported outcome measures (PROMs), hip fracture, qualitative research methods, semistructured interviews, orthopedic outcomes
Introduction
The number of elderly adults in the United States is steeply rising. In 2014, individuals aged 65 and older represented 14.5% of the US population. By 2040, this number is expected to increase to 21.7% of the population.1 This surge in the number of older individuals will impact many health care specialties, but its effect on the practice of orthopedic surgery will be profound. It is estimated that 1 of every 3 elderly individuals will sustain a fall each year. Falls are responsible for 95% of hip fractures.2,3 Currently, over 300 000 elderly people are hospitalized annually for hip fractures.4,5 As the elderly population increases, the number of hip fractures will also rise.1,6,7
Patient reported outcome measures (PROMs) are becoming well recognized as an important component of health care outcomes and determinants of value in patient-centered care. However, there is emerging recognition that guidance is lacking in the utilization of PROMs in hip fracture patients.8,9 In addition, very little work has been accomplished to understand patient priorities in outcomes following hip fracture care. Most research regarding the identification of patient priorities in hip fracture care and recovery (largely accomplished outside of the United States) points to the need for consideration of the complexity of the patient’s medical and cognitive status.8,10-14 Further, there is great variation in the patient demographics of those experiencing and recovering from hip fracture, which further complicates the identification of a single set of priorities for all hip fracture patients and points to the need to understand how best to incorporate health care proxies.15-17
Given the growing incidence of hip fractures, the known variation in physiological and neurological wellness in this population,15 and the lack of knowledge regarding patient priorities during recovery from hip fracture, we sought to gather pilot data on the priorities of patients who have sustained hip fractures. To ensure assessment of priorities of patients with potentially a greater number of medical comorbidities, including cognitive impairment, data from health care advocates or proxies were also sought. The primary goal of our work was to determine and rank outcome priorities in a small cohort of hip fracture patients.
Methods
All patients aged 65 and older and treated for hip fractures at our institution are entered into a hip fracture registry. Following institutional review board approval, this registry was utilized to identify patients who had sustained an isolated low-energy hip fracture in the previous 3 to 9 months. A cross-sectional study design consisting of semistructured interviews of patients or proxies was executed. Chart reviews were performed via the electronic medical record to ascertain whether each patient was an independent decision maker or whether the patient had a health care agent. During the standard care delivery process, health care agents were identified as proxies when the patient was unable to advocate for himself/herself secondary to dementia, Alzheimer disease, or memory loss, or when a physician-documented inability to make independent health care decisions was identified. Responses were obtained directly from the patients themselves whenever possible. However, the inclusion of proxies allowed identification of priorities for patients with cognitive deficits. Exclusions to study participation were non-English speaking patients or patients with a diagnosis of cognitive impairment with no health care proxy named in the electronic medical record.
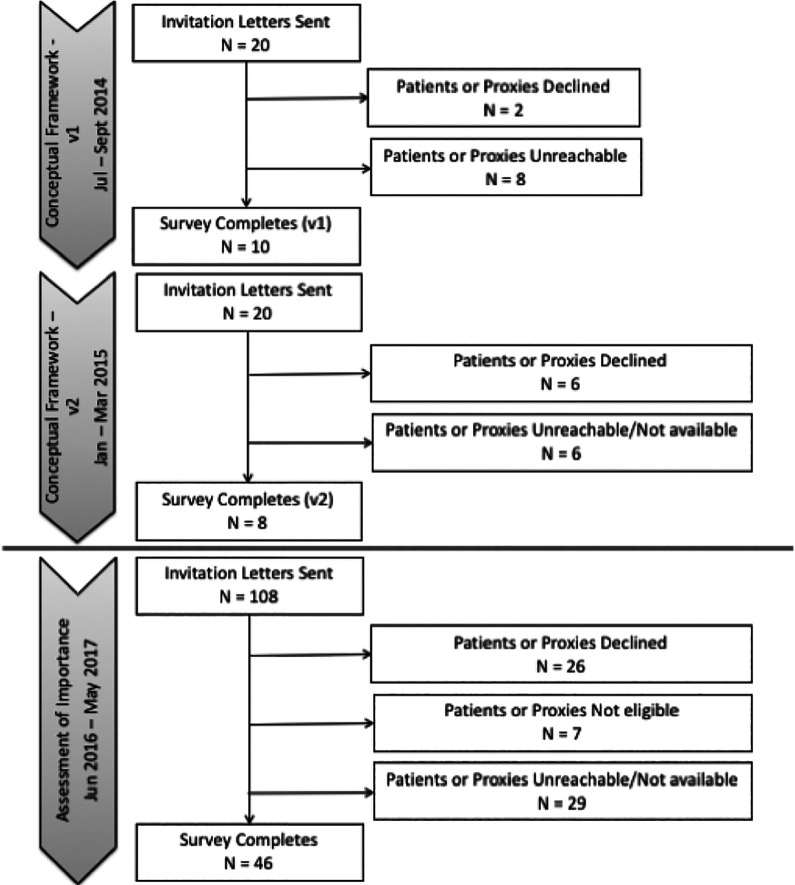
The study was conducted at Regions Hospital, a large urban, community hospital, which also serves as the region’s level 1 trauma center. All data were collected by Health Partners Institute and documented in research electronic data capture (REDCap) system.18 Two phases of the study were undertaken: (1) concept identification and conceptual framework development and (2) item generation and assessment of relative importance of health care outcomes. Each phase was completed by separate patient cohorts (Figure 1).
Figure 1.
A flow diagram illustrating the process of patient invitation and enrollment, including those who were excluded or declined participation.
Phase 1: Concept Identification and Conceptual Framework Development
To identify important outcomes following hip fracture, we conducted in-depth semistructured interviews with patients and/or their proxies. (Appendix 1A) Invitation letters were sent to identified patients (or health care agents) to explain the purpose of the study and to invite them to participate. Prospective respondents were given the option to either participate or opt-out of the study. If they did not opt out, patients (or health care agents) were contacted 1 week later by a trained interviewer. Semistructured telephone interviews were conducted and the patients’ responses were recorded. Interviewers asked open-ended questions relating to the patient’s experience during their recent hip fracture treatment.
The semistructured telephone interview scripts were adapted based upon initial results to include questions about functional outcomes. These questions were fielded with an additional group of patients and health care agents (Appendix 1B).
Upon completion of semistructured interviews, responses were distilled into themes, and a set of declarative statements was produced. These were reviewed by all project team members for face validity and further categorized into themes for group analysis. The resulting thematic report was used as the basis for the conceptual framework leading to item generation.
Phase 2: Item Generation and Assessment of Relative Importance of Health Care Outcomes
In the second phase, a telephone-based interview survey was then designed to assess the relative importance of the patient-centered components of orthopedic care and outcomes. Questionnaire items were generated using the thematic report summarizing prior interview data. Best practices for question writing and survey development were used.19 Upon completion of the draft instrument, it was reviewed for face validity by a panel of content experts including an orthopedic surgeon, a hospitalist, a clinical research director, and survey methodologists not directly involved in the questionnaire development.20
Steps were taken to minimize the cognitive load on participants by limiting each section to no more than 5 declarative statements. To avoid ceiling effects in outcomes reported as important, respondents were asked to further rank their “very” and “somewhat” important statements. The interview script was crafted to facilitate patient understanding. Two separate scripts were created and tailored for either patients or proxies.
A priori we sought to obtain 50 consents and completed surveys. The same invitation and contact protocol used in phase 1 was employed. Preliminary invitation letters were sent to inform as well as to provide the opt-out option. Up to 10 contact attempts from interviewers were made to patients who did not opt out. During interviews, patients were asked to rate the importance of each declarative statement on a scale of 4 options: very important, somewhat important, somewhat not important, or not at all important. After a relative importance had been recorded for each declarative statement in a section, the interviewer repeated the items that had been identified as very or somewhat important, and the participant was then asked to quantitatively rank the top 2 most important health care components in the given section. At the conclusion of the interview, participants were then asked to quantitatively rank each of the 6 sections based on their overall relative importance.
All telephone encounters concluded with the EQ-5D-3L questionnaire and the visual analogue scale (VAS) for pain assessments to describe the study cohort of hip fracture patients.21 Proxies were asked to respond/provide information relative to the patient.
Results
A total of 148 eligible patients and/or proxies were contacted and 64 interviews were completed with a 43% response rate. Eighteen interviews with 13 patients and 5 proxies were completed for framework development. Forty-six interviews with 33 patients and 13 proxies were completed for the assessment of relative importance. Figure 1 describes the project flow and subject recruitment process. Demographics for the full cohort, including 46 females and 18 males, are given in Table 1.
Table 1.
Demographics of Hip Fracture Patients Included in Self-reported and Proxy-Reported Results.
| All | Patients | Proxies | |
|---|---|---|---|
| Framework Development Survey, v1 | N = 10 | N = 8 | N = 2 |
| M: F | 4:6 | 3:5 | 1:1 |
| Mean age (SD) | 79.6 (7.0) | 78.3 (7.1) | 85.0 (4.2) |
| Mean EQ5-D (SD) | .70 (.18) | .76 (.08) | .47 (.31) |
| Mean VAS (SD) | 68.8 (31.6) | 72.9 (32.3) | 52.5 (31.8) |
| Framework Development Survey, v2 | N = 8 | N= 5 | N = 3 |
| M: F | 3:5 | 1:4 | 2:1 |
| Mean age (SD) | 81.6 (10.8) | 76.6 (9.2) | 90.0 (8.5) |
| Mean EQ5-D (SD) | .71 (.16) | .80 (.05) | .56 (.17) |
| Mean VAS (SD) | 55.6 (17.4) | 65.0 (12.2) | 40.0 (13.2) |
| Assessment of importance | N = 46 | N = 33 | N = 13 |
| M: F | 10:36 | 7:26 | 3:10 |
| Mean age (SD) | 78.9 (7.7) | 77.5 (7.1) | 82.4 (8.3) |
| Mean EQ5-D (SD) | .73 (.22) | .78 (.18) | .59 (.28) |
| Mean VAS (SD) | 75.3 (19.8) | 77.2 (19.0) | 68.3 (22.5) |
Abbreviations: F, female; M, male; SD, standard deviation.
Phase 1: Concept Identification and Conceptual Framework Development
Enrollment for this phase occurred from May 2014 through June 2015. An iterative process was utilized in the generation of the conceptual framework, and 2 versions were required before thematic saturation was thought to be achieved by the team and content experts (see Appendix 1A and B).
Upon completion of semistructured interviews, the text from each recorded call was coded and placed into a matrix (MSExcel, Microsoft Corp). Next, interview responses were studied, organized into categories, concepts were distilled, and themes were grouped. Results were finally reviewed by the full team to ensure that all categories, concepts, and themes were appropriately represented from the data set. This work resulted in identifying the following themes: People, Communication, Coordination, Physical outcomes, Feelings, and Expectations during transition from the hospital. Example quotes from the respondents include the following:
“Went pretty well, it was new to me…They got me up really well the first time. Wish they would have done more treatment.” (ie. physical therapy) (Patient ID #52, Q2, 89 y.o., F)
“…I am more interested in them being interested in me than in what is going on around me…” (Patient ID #34, Q7, 85 y.o., M)
“The thing that scared me the most and the thing that I ended up liking the most was helping to overcome my fear. Going up and down the stairs. The persistence, help you gain the trust.” (Patient ID #51, Q7, 72 y.o., M)
A set of declarative statements that represented the concepts acquired above was produced. These statements were secondarily reviewed and further categorized into themes for group analysis. The research team reviewed the set of declarative statements for face validity. The resulting thematic report was used as the basis for the conceptual framework leading to item generation (phase 2).
Phase 2: Item Generation and Assessment of Relative Importance of Health Care Outcomes
Based upon the result from the previous phase, the final survey included the 6 categories: People, Communication, Coordination, Physical outcomes, Feelings, and Expectations during transition from the hospital. A series of declarative statements related to each category was developed and utilized in a telephone survey for this second phase (Appendix 2). Enrollment for this phase of the project occurred from June 2016 through May 2017.
Analysis of the results from this portion of the project included a direct rating of the percentage of responses for “very important” and (95% CI) regarding each declarative statement within each category. These were then ranked by highest percentage.
Within the category of People, the statement “Having confidence that I received the best possible care” was ranked #1 overall, and independently with patients and proxies with 98% overall, 97% of patients and 100% of proxies responding with “very important.”
Within the category of Communication, the statement “Getting all questions answered” was ranked #1 overall, and independently with patients (94% and 94%, respectively), while proxies rank this statement as #2 with 92% with “very important.” In the Communication category, the statement which resulted in the #1 ranking by proxies was “Having the care team explain things in language that is understandable,” with 100% stating that this was “very important.”
Within the category of Coordination, the statement “Feeling like all members of the care team are on the same page” was ranked #1 overall, and independently with patients and proxies with 84% overall, 84% of patients and 85% of proxies responding with “very important.”
Within the category of Feelings, the statement “Feeling like my wishes (wishes of the patient) are being heard” was ranked #1 overall, and independently with proxies (78% and 92%, respectively), while patients ranked this statement as #2 with 73% stating “very important.” In this category of Feelings, the statement which resulted in the #1 ranking by patients was “Feeling like the care team understands the impact of this event in my life,” with 76% stating that this was “very important.”
Within the category of Physical Outcomes, the statement “Avoiding complications after fracture treatment” was ranked #1 overall, and independently with patients (93% and 94%, respectively), while proxies ranked this statement as #2 with 92% stating “very important.” In this category of Physical Outcomes, the statement which resulted in the #1 ranking by proxies was “Having the care team set and explain realistic goals for my physical outcomes,” with 100% stating that this was “very important.”
Finally, for the category of Expectations, the statement “Being connected with resources such as equipment, home modifications, rehabilitation, or support for daily activities after leaving the hospital” was ranked #1 overall, and by patients and proxies independently (78%, 75%, and 85%, respectively.)
After a relative importance had been recorded for each declarative statement in a section, the interviewer repeated the items that had been identified as very or somewhat important, and the participant was then asked to quantitatively rank the top 2 most important health care components in the given section. All results for percentages and confidence intervals of patients and proxies responding “very important” are given in Table 2.
Table 2.
Results of Rating and Ranking in the Assessment of Relative Importance.
| Overall | Patient | Agent | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 46 | Rank | n = 33 | Rank | n = 13 | Rank | |||||
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | |||||
| People | Rating: “very important” vs other | |||||||||
| Team | 28 | 62.2 (46.5-76.2) | 21 | 65.6 (46.8-81.4) | 7 | 53.8 (25.1-80.8) | ||||
| Surgeon | 35 | 76.1 (61.2-87.4) | 2 | 26 | 78.8 (61.1-91.0) | 2 | 9 | 69.2 (38.6-90.9) | 2 | |
| Hospitalist | 32 | 69.6 (54.3-82.3) | 24 | 72.7 (54.4-86.7) | 8 | 61.5 (31.6-86.1) | ||||
| Decisions | 33 | 71.7 (56.5-84.0) | 25 | 75.8 (57.7-88.9) | 8 | 61.5 (31.6-86.1) | ||||
| Best care | 45 | 97.8 (88.5-99.9) | 1 | 32 | 97.0 (84.2-99.9) | 1 | 13 | 100.0 (75.3-100.0) | 1 | |
| Ranking: “most” or “second most important” vs other | ||||||||||
| Team | 28 | 71.8 (55.1-85.0) | 19 | 70.4 (49.8-86.3) | 9 | 75.0 (42.8-94.5) | ||||
| Surgeon | 38 | 86.4 (72.7-94.8) | 2 | 27 | 84.4 (67.2-94.7) | 2 | 11 | 91.7 (61.5-99.8) | 2 | |
| Hospitalist | 22 | 56.4 (39.6-72.2) | 16 | 59.3 (38.8-77.6) | 6 | 50.0 (21.1-78.9) | ||||
| Decisions | 30 | 76.9 (60.7-88.9) | 23 | 82.1 (63.1-93.9) | 7 | 63.6 (30.8-89.1) | ||||
| Best care | 42 | 91.3 (79.2-97.6) | 1 | 30 | 90.9 (75.7-98.1) | 1 | 12 | 92.3 (64.0-99.8) | 1 | |
| Communication | Rating: “very important” vs other | |||||||||
| Why | 25 | 54.3 (39.0-69.1) | 18 | 54.5 (36.4-71.9) | 7 | 53.8 (25.1-80.8) | ||||
| Risk | 33 | 71.7 (56.5-84.0) | 23 | 69.7 (51.3-84.4) | 10 | 76.9 (46.2-95.0) | ||||
| Information | 33 | 73.3 (58.2-85.4) | 24 | 75.0 (56.6-88.5) | 9 | 69.2 (38.6-90.9) | ||||
| Explain | 43 | 93.5 (82.1-98.6) | 2 | 30 | 90.9 (75.7-98.1) | 2 | 13 | 100.0 (75.3-100.0) | 1 | |
| Questions | 43 | 93.5 (82.1-98.6) | 1 | 31 | 93.9 (79.8-99.3) | 1 | 12 | 92.3 (64.0-99.8) | 2 | |
| Ranking: “most” or “second most important” vs other | ||||||||||
| Why | 28 | 70.0 (53.5-83.4) | 20 | 74.1 (53.7-88.9) | 8 | 61.5 (31.6-86.1) | ||||
| Risk | 36 | 83.7 (69.3-93.2) | 1 | 28 | 90.3 (74.3-98.0) | 1 | 8 | 66.7 (34.9-90.1) | ||
| Information | 31 | 75.6 (59.7-87.6) | 20 | 71.4 (51.3-86.8) | 11 | 84.6 (54.6-98.1) | 2 | |||
| Explain | 35 | 83.3 (68.6-93.0) | 2 | 23 | 76.7 (57.7-90.1) | 12 | 100.0 (75.3-100.0) | 1 | ||
| Questions | 35 | 81.4 (66.6-91.6) | 25 | 80.6 (62.5-92.6) | 2 | 10 | 83.3 (51.6-97.9) | |||
| Coordination | Rating: “very important” vs other | |||||||||
| All | 32 | 69.6 (54.3-82.3) | 23 | 69.7 (51.3-84.4) | 9 | 69.2 (38.6-90.9) | ||||
| Wait | 18 | 39.1 (25.1-54.6) | 13 | 39.4 (22.9-57.9) | 5 | 38.5 (13.9-68.4) | ||||
| Page | 37 | 84.1 (69.9-93.4) | 1 | 26 | 83.9 (66.3-94.6) | 1 | 11 | 84.6 (54.6-98.1) | 1 | |
| No doc | 37 | 80.4 (66.1-90.6) | 2 | 27 | 81.8 (64.5-93.0) | 2 | 10 | 76.9 (46.2-95.0) | 2 | |
| Ranking: “most” or “second most important” vs other | ||||||||||
| All | 35 | 81.4 (66.6-91.6) | 2 | 24 | 77.4 (58.9-90.4) | 2 | 11 | 91.7 (61.5-99.8) | 2 | |
| Wait | 29 | 70.7 (54.5-83.9) | 20 | 69.0 (49.2-84.7) | 9 | 75.0 (42.8-94.5) | ||||
| Page | 34 | 81.0 (65.9-91.4) | 2 | 23 | 76.7 (57.7-90.1) | 2 | 11 | 91.7 (61.5-99.8) | 2 | |
| No doc | 40 | 90.9 (78.3-97.5) | 1 | 29 | 90.6 (75.0-98.0) | 1 | 11 | 91.7 (61.5-99.8) | 1 | |
| Feelings | Rating: “very important” vs other | |||||||||
| Care | 32 | 69.6 (54.3-82.3) | 22 | 66.7 (48.2-82.0) | 10 | 76.9 (46.2-95.0) | 2 | |||
| Attention | 32 | 69.6 (54.3-82.3) | 22 | 66.7 (48.2-82.0) | 10 | 76.9 (46.2-95.0) | ||||
| Wishes | 36 | 78.3 (63.6-89.1) | 1 | 24 | 72.7 (54.5-86.7) | 2 | 12 | 92.3 (64.0-99.8) | 1 | |
| Impact | 32 | 69.6 (54.3-82.3) | 2 | 25 | 75.8 (57.7-88.9) | 1 | 7 | 53.8 (25.1-80.8) | ||
| Ranking: “most” or “second most important” vs other | ||||||||||
| Care | 35 | 83.3 (68.6-93.0) | 2 | 26 | 89.7 (72.7-97.8) | 2 | 9 | 69.2 (38.6-90.9) | ||
| Attention | 30 | 81.1 (64.8-92.0) | 20 | 76.9 (56.4-91.0) | 10 | 90.9 (58.7-99.8) | 2 | |||
| Wishes | 37 | 90.2 (76.9-97.3) | 1 | 26 | 89.7 (72.7-97.8) | 1 | 11 | 91.7 (61.5-99.8) | 1 | |
| Impact | 31 | 81.6 (65.7-92.3) | 21 | 80.8 (60.7-93.5) | 10 | 83.3 (51.6-97.9) | ||||
| Physical outcomes | Rating: “very important” vs other | |||||||||
| Goals | 35 | 77.8 (62.9-88.8) | 22 | 68.8 (50.0-83.9) | 13 | 100.0 (75.3-100.0) | 1 | |||
| Complications | 42 | 93.3 (81.7-98.6) | 1 | 30 | 93.8 (79.2-99.2) | 1 | 12 | 92.3 (64.0-99.8) | 2 | |
| Pain | 36 | 80.0 (65.4-90.4) | 2 | 26 | 81.3 (63.6-92.8) | 10 | 76.9 (46.2-95.0) | |||
| Activity | 30 | 68.2 (52.4-81.4) | 26 | 83.9 (66.3-94.6) | 2 | 4 | 30.8 (9.1-61.4) | |||
| Ranking: “most” or “second most important” vs other | ||||||||||
| Goals | 35 | 87.5 (73.2-95.8) | 2 | 23 | 82.1 (63.1-93.9) | 12 | 100.0 (75.3-100.0) | 2 | ||
| Complications | 40 | 88.9 (76.0-96.3) | 1 | 27 | 84.4 (67.2-94.7) | 1 | 13 | 100.0 (75.3-100.0) | 1 | |
| Pain | 35 | 83.3 (68.6-93.0) | 24 | 82.8 (64.2-94.2) | 2 | 11 | 84.6 (54.6-98.1) | |||
| Activity | 24 | 66.7 (49.0-81.4) | 19 | 73.1 (52.2-88.4) | 5 | 50.0 (18.7-81.3) | ||||
| Expectations during transition | Rating: “very important” vs other | |||||||||
| Next | 35 | 76.1 (61.2-87.4) | 2 | 24 | 72.7 (54.5-86.7) | 2 | 11 | 84.6 (54.6-98.1) | 2 | |
| Resources | 35 | 77.8 (62.9-88.8) | 1 | 24 | 75.0 (56.6-88.5) | 1 | 11 | 84.6 (54.6-98.1) | 1 | |
| Transfer | 27 | 61.4 (45.5-75.6) | 22 | 71.0 (52.0-85.8) | 5 | 38.5 (13.9-68.4) | ||||
| Function | 32 | 71.1 (55.7-83.6) | 23 | 71.9 (53.3-86.3) | 9 | 69.2 (38.6-90.9) | ||||
| Function 2 | 32 | 72.7 (57.2-85.0) | 25 | 80.6 (62.5-92.6) | 7 | 53.8 (25.1-80.8) | ||||
| Ranking: “most” or “second most important” vs other | ||||||||||
| Next | 38 | 88.4 (74.9-96.1) | 1 | 25 | 83.3 (65.3-94.4) | 1 | 13 | 100.0 (75.3-100.0) | 1 | |
| Resources | 34 | 85.0 (70.2-94.3) | 2 | 23 | 79.3 (60.3-92.0) | 2 | 11 | 100.0 (75.3-100.0) | 2 | |
| Transfer | 21 | 61.8 (43.6-77.8) | 16 | 64.0 (42.5-82.0) | 5 | 55.6 (21.2-86.3) | ||||
| Function | 31 | 77.5 (61.6-89.2) | 22 | 78.6 (59.1-91.7) | 9 | 75.0 (42.8-94.5) | ||||
| Function 2 | 28 | 73.7 (56.9-86.6) | 19 | 70.4 (49.8-86.3) | 9 | 81.8 (48.2-97.7) | ||||
| Overall | Ranking: “most” or “second most important” vs other | |||||||||
| Team | 36 | 80.0 (65.4-90.4) | 1 | 29 | 90.6 (75.0-98.0) | 1 | 7 | 53.8 (25.1-80.8) | 1 | |
| Communicate | 30 | 66.7 (51.0-80.0) | 2 | 20 | 62.5 (43.7-78.9) | 2 | 10 | 76.9 (46.2-95.0) | 2 | |
| Coordinate | 3 | 7.1 (1.5-19.5) | 1 | 3.3 (0.1-17.2) | 2 | 16.7 (2.1-48.4) | ||||
| Feelings | 3 | 7.1 (1.5-19.5) | 3 | 10.0 (2.1-26.5%) | 0 | 0 .0 (0.0-26.5) | ||||
| Physical | 11 | 26.8 (14.2-42.9) | 8 | 27.6 (12.7-47.2) | 3 | 25.0 (5.5-57.2) | ||||
| Expectations | 6 | 14.6 (5.6-29.2) | 2 | 7.1 (0.9-23.5) | 4 | 30.8 (9.1-61.4) | ||||
At the conclusion of the interview, participants were asked to quantitatively rank each of the 6 sections based on their overall relative importance. Figure 2 depicts the percentage of patients/proxies who ranked each category as either “most important” or “second most important” overall. Care team and communication were reported as important in hip fracture patients. Physical outcomes were ranked as most important by only 9% of respondents. The relative importance within the Care Team category: “Having confidence that I/my loved one received the best care possible” was perceived as very important by 98% of respondents and “Having access to the surgeon” was perceived as very important by 76% of the respondents.
Figure 2.
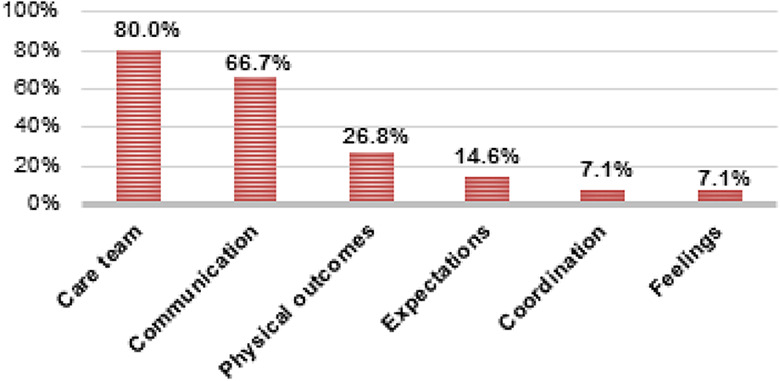
A bar chart demonstrating the percentage of patients ranking each outcome category as either “most important” or “second most important” overall.
Discussion
There exist today many instruments to assess physical function,22,23 hip-specific function,24-26 and quality of life in hip fracture patients.27,28 While most of these require direct patient reporting, none have been designed specifically for the hip fracture patient population, nor take into consideration patient preferences for outcomes on which to report.10 This omission is even more acutely true in the frailer, elderly patients, who have historically been broadly excluded from hip fracture trials and clinical outcomes research on the topic.16,17
Recent systematic reviews have assessed the quality of PROMs used in hip fracture care. Haywood et al29 reviewed and summarized the acceptability of 28 PROMs and concluded that there was only minimal evidence supporting the use of only a few measures, and most measures currently utilized have very limited relevance to this patient population.29 In addition, PROMs do not necessarily address the patient’s own priorities. Patient involvement in PROM development, evaluation, or implementation in hip fracture outcomes has not been reported.10,30,31 Current and future research priorities around PROMs in hip fracture patients must seek to understand which outcomes matter most to the patients themselves. In addition, due to the wide variation in health status at baseline in hip fracture patients, this work must also determine how best to appropriately incorporate proxy or health care advocate completion.16,17
Our study sought to conduct interviews to determine outcome priorities of hip fracture patients. This work identified the following themes: People, Communication, Coordination, Physical outcomes, Feelings, and Expectations during transition from the hospital. Sims-Gould et al described the expectations of a cohort of 48 patients who were within a year of hip fracture.32 By employing a semistructured format and a mixed-method study design similar to our own, they determined that, in this community dwelling, cognitively sound population, managing expectations, focusing on physical activity, and maintaining optimism during recovery were the most important themes.
We also worked to understand the rank order of importance of identified priorities in a second cohort of hip fracture patients. Care team and communication were reported as important in hip fracture patients, including the relative importance within the Care Team category: “Having confidence that I/my loved one received the best care possible” was perceived as very important by 98% of respondents and “Having access to the surgeon” was perceived as very important by 76% of the respondents. Physical outcomes were ranked as most important by only 9% of respondents, including subcategories of goals for physical outcomes, avoiding complications, avoiding ongoing pain, and recovery of prefracture activities.
Prior authors have hypothesized that outcomes important to younger, more healthy and independent patients, might be different from those important to a person who perceives themselves as nearing the end of life. Griffiths et al10 and others have not been able to identify a PROM specific to the assessment of hip fracture patient nor any robust evidence of the quality and acceptability of nonhip fracture specific PROMs used for hip fracture patients.29,33 These authors conclude that clarity in which outcomes of health care are considered most relevant to hip fracture patients do not currently exist, and it is unlikely that a single PROM could be developed for the entire spectrum of patients experiencing hip fracture. Therefore, our work in understanding relative importance could lead to important development of appropriate PROMs for this patient population.
Limitations in our study can be identified. We have only included a small sample of hip fracture patients, though our response rates (64 of 148, 43%) are similar to Griffiths et al (31 of 62, 50%).10 We also included patients who were 3 to 9 months posthip fracture in each phase of the study. Selection of this time point is in range with other qualitative research reports in this patient population10,32 and allows sufficient time for adequate recovery in the immediate postoperative period, though the impact of memory recall at this time point is unknown. In addition, this pilot work did not allow the possibility to compare and analyze patient and proxy responses, and prior work in a similar population does indicate some limitations to proxy responses, specifically in patients having dementia or cognitive impairment.34 By attempting to include all patients or their proxies, regardless of cognition status, our work is susceptible to underreporting of pain or its importance. Though this limitation is unable to be resolved within the scope of this work, our findings of importance in physical outcomes, including pain, being ranked as most important by only 9% of respondents, aligns with the results of Griffiths et al,10 who reported that pain was “not considered a major problem.” Finally, the methods of survey development tailored to the geriatric population must be further explored and perfected, but our study is unique step in this important direction.
In our study, communication between patients and care providers as well as collaboration among patients’ care providers ranked as the most important postoperative preferences in our cohort. Additionally, physical outcomes were ranked as most important by only 9% of respondents. This preliminary work and findings can promote future research in geriatric orthopedic outcomes and serve as the foundation for the development of a validated measure of patient-preferred outcomes in elderly hip fracture patients to be used at a national scale. This work may also be used to evaluate the relative value of innovative care models that are designed to improve more than traditional functional outcomes.
Appendix 1
-
Open-ended questions asked during telephone survey, v1.
To begin with, can you confirm that you were treated for hip fracture at Regions Hospital within the last year?
Thinking back to your overall experience and care that you received as a result of your hip fracture, what can you tell me about how things went?
Now, thinking specifically about the care that you received while you were in the hospital. What can you tell me about how things went?
Now, thinking specifically about the care that you continued to receive after you were in the hospital. What can you tell me about how things went?
We are also interested in your thoughts about your relationships with your health care providers. What aspects of these relationships (if any) were important in forming your thoughts about your overall experience? Note: We are interested in qualities of communication and relationships, not information about a specific person.
Thinking about the overall experience that you had, would you recommend Regions to a friend or family member with the same medical needs? What factors or parts of your experience would lead you to make or not to make this recommendation?
What else can you tell me about your overall experience? Were there other aspects to the care that you received that impacted your overall thoughts about the experience?
-
Open-ended questions asked during telephone survey, v2.
To begin with, can you confirm that you were treated for hip fracture at Regions Hospital within the last year?
Thinking back to your overall experience and care that you received as a result of your hip fracture, what can you tell me about how things went?
We are interested in knowing more about what you were hoping to get out of your surgery. Thinking back to before your surgery, what were you hoping for as a result? What did you think would be the best possible result of the surgery?
In addition to the outcomes we just talked about, was there anything else that you were hoping to result from the surgery?
Thinking about how you are now as a result of the surgery, what can you do (or not do) that makes you think that the surgery was or was not a success?
Is there anything else about what happened to you as a result of the surgery that you think it would be important for us to know as we try to understand what is important to patients like you?
Appendix 2
Categories and Statements of Importance: Six categories of care, each containing no more than 5 declarative statements
-
○ People
▪ Knowing who is on my care team
▪ Having access to the surgeon
▪ Having access to the hospitalist
▪ Having the care team include me in decision-making
▪ Having confidence that I received the best possible care
-
○ Communication
▪ Understanding why things like tests and blood draws happen during the hospital stay
▪ Having the care team explain the risks and benefits of pain medication
▪ Having the care team communicate information about things like discharge planning, equipment, and home modifications
▪ Having the care team explain things in language that is understandable
▪ Getting all questions answered
-
○ Coordination
▪ Coordination in all aspects of the hospital stay, such as doctor consultations, showers and personal care, tests, and x-rays
▪ Not having to wait for activities to occur, such as doctor consultations, showers and personal care, tests, and x-rays
▪ Feeling like all members of the care team are on the same page
▪ Being able to get information I need even when the doctor is not available
-
○ Feelings
▪ Feeling like the care team cares about me and my family
▪ Feeling like the care team pays enough attention to me
▪ Feeling like my wishes are being heard
▪ Feeling like the care team understands the impact of this event in my life
-
○ Physical outcomes
▪ Having the care team set and explain realistic goals for my physical outcomes
▪ Avoiding complications after fracture treatment
▪ Avoiding ongoing pain after fracture treatment
▪ Being able to do all of the activities that I could do before fracture treatment
-
○ Expectations
▪ Having confidence in the next steps in care after leaving the hospital
▪ Being connected with resources such as equipment, home modifications, rehabilitation, or support for daily activities after leaving the hospital
▪ Understanding why I am transferred to the nursing care facility (will also have a Not Applicable option)
▪ Being prepared for my level of functioning immediately after fracture treatment
▪ Being prepared for my level of functioning after I recover from the fracture
– Patients were asked both to assess the relative importance of each statement and rank the top 2 most important statements in each category.
– Relative importance was assessed as either “very important, somewhat important, somewhat not important, or not at all important.”
– Patients were then asked to rank each of the 6 categories in order of importance.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded a Clinical Research Committee grant through the Department of Orthopaedic Surgery, University of Minnesota.
ORCID iDs: Naomi Turner  https://orcid.org/0000-0002-4775-3822
https://orcid.org/0000-0002-4775-3822
Julie A. Switzer  https://orcid.org/0000-0002-4834-1643
https://orcid.org/0000-0002-4834-1643
References
- 1. Administration for Community Living, Administration on Aging. 2017 Profile of Older Americans; 2018:4 Accessed August 10, 2020 https://www.acl.gov/aging-and-disability-in-america/data-and-research/profile-older-americans
- 2. Hayes WC, Myers ER, Morris JN, Gerhart TN, Yett HS, Lipsitz LA. Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcif Tissue Int. 1993;52(3):192–198. [DOI] [PubMed] [Google Scholar]
- 3. Parkkari J, Kannus P, Palvanen M, et al. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int. 1999;65(3):183–187. [DOI] [PubMed] [Google Scholar]
- 4. Weiss AJ, Barrett ML, Andrews RM. Trends and projections in U.S. hospital costs by patient age, 2003–2013: statistical brief #176 In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2006. Accessed August 10, 2020 http://www.ncbi.nlm.nih.gov/books/NBK242376/ [PubMed] [Google Scholar]
- 5. HCUPnet. HCUPnet. 2016. Accessed August 10, 2020 https://hcupnet.ahrq.gov
- 6. Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States. United States Census Bureau; 2014:28. [Google Scholar]
- 7. Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Mineraz Res. 2007;22(3):465–475. doi:10.1359/jbmr.061113 [DOI] [PubMed] [Google Scholar]
- 8. Liem IS, Kammerlander C, Suhm N, et al. Identifying a standard set of outcome parameters for the evaluation of orthogeriatric co-management for hip fractures. Injury. 2013;44(11):1403–1412. doi:10.1016/j.injury.2013.06.018 [DOI] [PubMed] [Google Scholar]
- 9. Haywood KL, Griffin XL, Achten J, Costa ML. Developing a core outcome set for hip fracture trials. The Bone & Joint J. 2014;96-B(8):1016–1023. doi:10.1302/0301-620X.96B8.33766 [DOI] [PubMed] [Google Scholar]
- 10. Griffiths F, Mason V, Boardman F, et al. Evaluating recovery following hip fracture: a qualitative interview study of what is important to patients. BMJ Open. 2015;5(1):e005406–e005406. doi:10.1136/bmjopen-2014-005406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Currie C. Hip fracture audit: creating a ‘critical mass of expertise and enthusiasm for hip fracture care’? Injury. 2018;49(8):1418–1423. doi:10.1016/j.injury.2018.06.025 [DOI] [PubMed] [Google Scholar]
- 12. Johansen A, Golding D, Brent L, et al. Using national hip fracture registries and audit databases to develop an international perspective. Injury. 2017;48(10):2174–2179. doi:10.1016/j.injury.2017.08.001 [DOI] [PubMed] [Google Scholar]
- 13. Stott-Eveneshen S, Sims-Gould J, McAllister MM, et al. Reflections on hip fracture recovery from older adults enrolled in a clinical trial. Gerontol Geriatr Med. 2017;3:233372141769766 doi:10.1177/2333721417697663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Langford D, Edwards N, Gray SM, Fleig L, Ashe MC. “Life goes on.” Everyday tasks, coping self-efficacy, and independence: exploring older adults’ recovery from hip fracture. Qual Health Res. 2018;28(8):1255–1266. doi:10.1177/1049732318755675 [DOI] [PubMed] [Google Scholar]
- 15. Penrod JD, Litke A, Hawkes WG, et al. Heterogeneity in hip fracture patients: age, functional status, and comorbidity. J Am Geriatri Soc. 2007;55(3):407–413. doi:10.1111/j.1532-5415.2007.01078.x [DOI] [PubMed] [Google Scholar]
- 16. Mundi S, Chaudhry H, Bhandari M. Systematic review on the inclusion of patients with cognitive impairment in hip fracture trials: a missed opportunity? Can J Surg. 2014;57(4):E141–E145. doi:10.1503/cjs.023413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hebert-Davies J, Laflamme G-Y, Rouleau D. Bias towards dementia: are hip fracture trials excluding too many patients? A systematic review. Injury. 2012;43(12):1978–1984. doi:10.1016/j.injury.2012.08.061 [DOI] [PubMed] [Google Scholar]
- 18. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Informat. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Improving Survey Questions. SAGE Publications Inc. Published August 19, 2018. Accessed August 10, 2020 https://us.sagepub.com/en-us/nam/improving-survey-questions/book4994
- 20. Groves RM, Jr FJF, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Survey Methodology. 2 ed Wiley; 2009. [Google Scholar]
- 21. Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72. doi:10.1016/0168-8510(96)00822-6 [DOI] [PubMed] [Google Scholar]
- 22. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. MD State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 23. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–919. doi:10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- 24. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 25. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 26. Klässbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis outcome score an extension of the Western Ontario and McMaster Universities Osteoarthritis index. Scandinavian J Rheumatol. 2003;32(1):46–51. doi:10.1080/03009740310000409 [DOI] [PubMed] [Google Scholar]
- 27. Parsons N, Griffin XL, Achten J, Costa ML. Outcome assessment after hip fracture: is EQ-5D the answer? Bone Joint Res. 2014;3(3):69–75. doi:10.1302/2046-3758.33.2000250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McHorney CA. Measuring and monitoring general health status in elderly persons: practical and methodological issues in using the SF-36 health survey. Gerontologist. 1996;36(5):571–583. [DOI] [PubMed] [Google Scholar]
- 29. Haywood KL, Brett J, Tutton E, Staniszewska S. Patient-reported outcome measures in older people with hip fracture: a systematic review of quality and acceptability. Qual Life Res. 2017;26(4):799–812. doi:10.1007/s11136-016-1424-1 [DOI] [PubMed] [Google Scholar]
- 30. Bruun-Olsen V, Bergland A, Heiberg KE. “I struggle to count my blessings”: recovery after hip fracture from the patients’ perspective. BMC Geriatrics. 2018;18(1):18 doi:10.1186/s12877-018-0716-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jensen CM, Smith AC, Overgaard S, Wiil UK, Clemensen J. “If only had I known”: a qualitative study investigating a treatment of patients with a hip fracture with short time stay in hospital. Int J Qual Stud Health Well-being. 2017;12(1):1307061 doi:10.1080/17482631.2017.1307061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sims-Gould J, Stott-Eveneshen S, Fleig L, McAllister M, Ashe MC. Patient perspectives on engagement in recovery after hip fracture: a qualitative study. J Aging Res. 2017;2017 doi:10.1155/2017/2171865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Auais M, French SD, Beaupre L, Giangregorio L, Magaziner J. Identifying research priorities around psycho-cognitive and social factors for recovery from hip fractures: an international decision-making process. Injury. 2018;49(8):1466–1472. doi:10.1016/j.injury.2018.04.017 [DOI] [PubMed] [Google Scholar]
- 34. Boyer F, Novella J-L, Morrone I, Jolly D, Blanchard F. Agreement between dementia patient report and proxy reports using the Nottingham health profile. Int J Geriatric Psychiatry. 2004;19(11):1026–1034. doi:10.1002/gps.1191 [DOI] [PubMed] [Google Scholar]